Summary
We reported the results of the endovascular treatment using Guglielmi detachable coil (GDC) for wide-necked aneurysms. Fourteen aneurysms were treated with remodeling technique. One aneurysm was performed endovascular treatment followed by partial neck clipping. The other was treated with scaffolding technique. All aneurysms could not be performed by conventional GDC treatment initially because of coil protrusion into the parent artery due to wide neck of these aneurysms.
These aneurysms sited at anterior circulation system in 10 cases, and at posterior circulation system in 6 cases. Immediately after the procedure, the obliteration rate could be obtained complete occlusion in 3 cases, >95% occlusion in 7 cases, >90% occlusion in 3 cases and < 90% occlusion in 3 cases. In 14 patients follow-up angiography or magnetic resonance image (MRI) was carried out. The angiographic follow-up period is range from 2 to 19 months (mean: 10 months).
The results of angiographical follow-up indicated increasing obliteration rate with all aneurysms except for 2 cases. In these 2 cases, the reembolization was needed for recanalization of the aneurysm. The clinical follow-up period is range form one to 26 months (mean: 15 months). There is no evidence of aneurysmal rupture and all cases have been survival without any permanent neurological deficits. The GDC treatment with additional technique (remodeling technique, combined neck-clipping and coiling therapy, scaffolding technique) provides safety and effectiveness, even if there are wide-necked aneurysms.
Key words: cerebral aneurysm, wide neck, GDC, embolization
Introduction
For the treatment of cerebral aneurysm the surgical clipping has been still gold standard. The surgical clipping, however, is not always the acceptable treatment for all cerebral aneurysms. In 1990 aneurysmal embolization using Guglielmi detachable coils (GDC) emerged as alternative therapy 1.
The several investigators reported the effectiveness to prevent subsequent bleeding and low morbidity and mortality 2-4. Especially in aneurysm with small neck GDC treatment could be achieved complete obliteration. But a wide neck has prevented achieving complete occlusion and an incomplete occlusion has brought some sequela such as recanalization, regrowth or rerupture of aneurysms5,6.
In order to solve this problem, some new methods have been developed. In this study, we evaluated effectiveness and safety of coil embolization for wide-necked aneurysms using remodeling technique, combined neck-clipping and coiling therapy, and scaffolding technique.
Clinical Material and Methods
Sixteen patients (12 female, 4 male; mean age, 55 years; range, 10 to 70 years) with 16 aneurysms underwent intraaneurysmal embolization using GDC. All aneurysms were wide necked aneurysms. Aneurysm with > 4 mm of neck or < 2 of sac/neck ratio was defined as wide-necked aneurysm. The size of aneurysm was small (< 12mm) in 11 aneurysms and large (> 12 mm) in 5 aneurysms. The size of neck was ranged from 2.7 to 12 mm. All aneurysms but one were unruptured aneurysms. The other one was a ruptured aneurysm that had recanalization due to coil compaction 9 months after first coil embolization using conventional technique. Ten aneurysms sited at anterior circulation, and 6 aneurysms in posterior circulation (table 1). Among 16 aneurysms, 14 aneurysms were treated with remodeling technique (figure 1). A large middle cerebral artery aneurysm was performed coil embolization after intentionally partial neck clipping (figures 2,3). The other aneurysm that sited at right vertebral artery was treated with scaffolding technique (figure 4). After aneurysmal neck was covered with gfx coronary stent entirely,GDCs were deposited into aneurysmal lumen via stent's strut without coil protrusion (figure 5). Angiography or magnetic resonance imaging was performed as the evaluation of embolized aneurysms at least on 6 months after embolization.
Table 1.
Site of aneurysms
| Parent artery | Treatment attempted |
Treatment completed |
|---|---|---|
| Anterior circulation | 10 | 10 |
| Internal carotid artery: | ||
| PCoA | 3 | 3 |
| SHA | 1 | 1 |
| OphA | 2 | 2 |
| Carotid cave | 3 | 3 |
| Middle cerebral artery: | ||
| Bifurcation | 1 | 1 |
| Posterior circulation | 6 | 6 |
| Basilar artery: | ||
| Termination | 3 | 3 |
| Vertebral artery: | ||
| PICA | 2 | 2 |
| Trunk | 1 | 1 |
| Total | 16 | 16 |
|
Pcom = posterior communicating artery; SHA = superior hypophysial artery; OphA = ophthalmic artery; PICA = pos- terior inferior cerebellar artery | ||
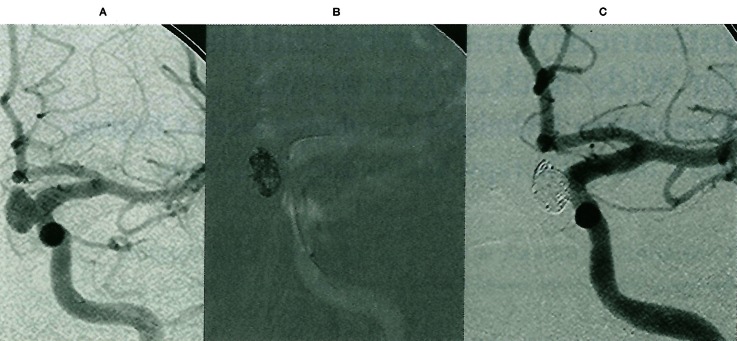
Figure 1.
GDC treatment using remodeling technique. A) Left carotid angiogram demonstrated ophthalmic aneurysm with wide neck. B) A microballoon catheter, was introduced into left internal carotid artery, was covered aneurysmal neck. C) On angiogram immediately after procedure, aneurysm was obliterated completely.
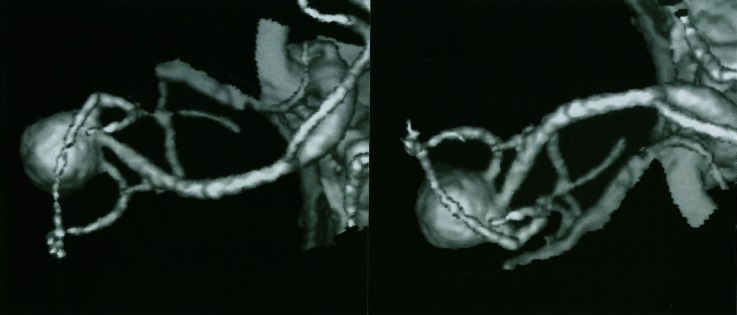
Figure 2.
Three dimensional CT angiography. Complex aneurysm with wide neck was demonstrated at right middle cerebral artery.
Figure 3.
GDC treatment followed neck clipping. A) Large complex aneurysm with wide neck was demonstrated. B) After neck clipping, aneurysm was still visualized. C) On angiogram immediately after embolization, >95% occlusion was achieved. D) Aneurysm was obliterated completely 6 months after embolization.
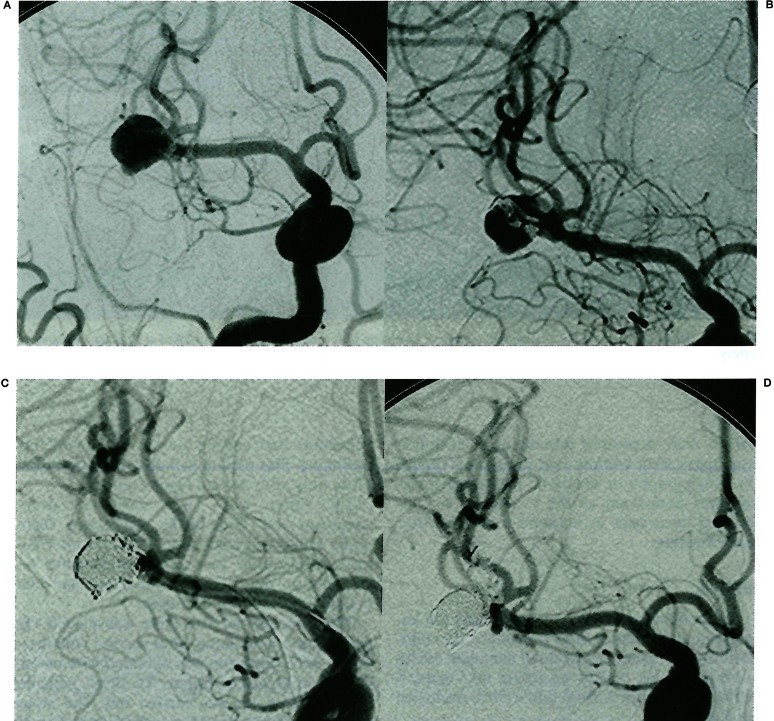
Figure 4.
Contrast enhanced CT scan. Partially thrombosed aneurysm was demonstrated in front of brain stem.
Figure 5.
GDC treatment using scaffolding technique. A) On right vertebral angiogram (AP view), irregular shaped aneurysm on right vertebral artery was revealed. B) A gfx stent could cover the aneurysmal neck entirely. C) On angiogram immediately after the procedure, near complete occlusion was achieved. D) AP view on skull XP was seen deposited coils and stent.
Results
All patients were treated successfully. On angiogram immediately after procedure, the obliteration rate could be obtained complete occlusion in 3 cases, > 95% occlusion in 7 cases, > 90% occlusion in 3 cases and < 90% occlusion in 3 cases.
There was no serious procedure-related morbidity and mortality. Though in a patient with IC-ophthalmic aneurysm treated with remodeling technique, mild hemiweakness was emerged during the procedure, she recovered fully within 5 days after the procedure. In 14 patients, follow-up angiogram was obtained.
The mean angiographic follow-up period was 12 months (range, 5 to 19 months). The obliteration rate was 100% in 5 cases, > 95% in 4 cases, > 90% in 3 cases, 70% in 2 cases. Two cases of 70% occlusion were large aneurysms. One with basilar trunk aneurysm was obtained 85% occlusion by mean of the first embolization using remodeling technique. For recanalization 14 months after first embolization, second embolization was carried out using remodeling technique. This patient gained >95% occlusion 17 months after second embolization.
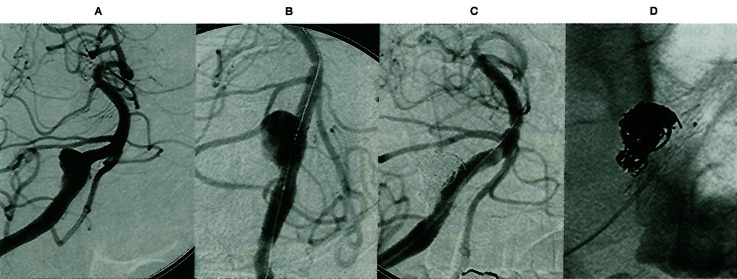
The other with large vertebral artery aneurysm was done using scaffolding technique. Follow-up angiogram 2 months after initial embolization was demonstrated the recanalization due to coil compaction and embedding of coils into thrombus.
Therefore second procedure was needed. On angiogram immediately after second embolization, >95% occlusion was obtained with patency of parent artery (figure 6). In all patients, clinical follow-up was carried out. The mean follow-up period was 15 months (range, 2 to 26 months). No incidence of subsequent aneurysmal bleeding and neurological deterioration was encountered during follow-up period.
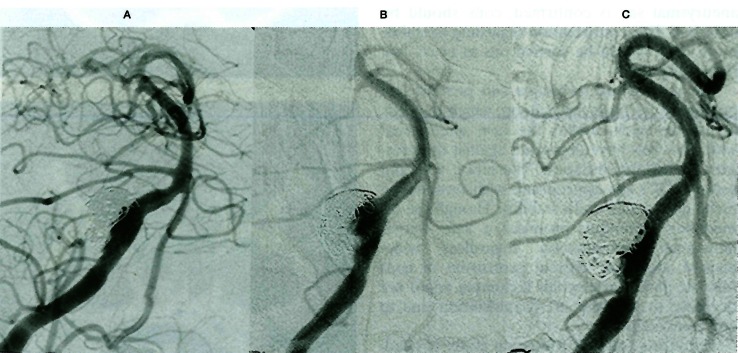
Figure 6.
GDC treatment using scaffolding technique. A) Two weeks follow-up angiogram demonstrated near complete occlusion. B) On follow-up angiogram 2 months after embolization, recanalization was recognized due to coil compaction and embedding of coils into thrombus. C) The near complete occlusion was obtained by second embolization.
Discussion
GDC treatment for wide-necked aneurysms
The neck clipping is still gold standard method for cerebral aneurysms. The endovascular treatments for poor surgical candidates using Guglielmie detachable coils were started in 19911. Now this method has been used widely all over the world. Many investigators have reported good results from follow-up studies, especially in small aneurysms with a smallneck 2-4. In contrast, large aneurysms with a wide neck continue to represent a challenge for most interventionalist5,6.
In wide-necked aneurysms, the detachable coils tend to protrude into the parent artery and this protrusion is likely to oppose dense packing.
The resulting loose packing may lead to a recanalization due to coil compaction. Therefore in endovascular treatment, the most limiting factor, which prevents complete occlusion and long-term stability of the coils, is wide neck. In this paper, coil embolization using three different techniques for wide-necked aneurysms was described.
Remodeling technique
The first report of remodeling technique, where each coil is placed within the aneurysmal lumen while a microballoon is kept inflated across the neck, described by Moret et Al7. Several investigators have reported on the effectiveness of this technique compared with thatof conventional embolization techniques in treating wide-necked aneurysms8,10. By use of the remodeling technique, the aneurysm can be packed densely at not only the body of the aneurysm but also the neck.
Therefore, this method can achieve safe “the endovascular trapping”, which both inflow zone and outflow zone are occluded. This dense coil packing leads to promote the thrombosis within the aneurysm, to make the faultless aneurysm obliteration and to prevent the recanalization by compaction. Because this technique requires transient obstruction of blood flow of parent artery, assessment about a collateral circulation before procedure and significant anticoagulant therapy during and after procedure are needed. After microballoon is deflated and stability of the coils within aneurysmal sac is confirmed, coils should be detached. This confirmation regarding to stability of coils should be carried out in every coil repeatedly.
The remodeling technique can prevent coil protrusion because the balloon, which deposits across the neck, makes the new aneurysmal wall. The coils have deposited against the pressure of balloon inflation. Therefore, soft and softer GDCs are appropriate with remodeling technique to gain coil's stability. Though the remodeling technique promises a safe intraaneurysmal embolization regardless wide-necked aneurysm without protrusion of coils into the parent artery, this technique could not decrease in the rate of recanalization due to coil compaction.
Therefore, prudent follow-up study is needed. We considered the embolization using this technique for wide-necked aneurysms with > 4 mm of neck and/or > 1 of sac/neck ratio.
Combined neck-clipping and coiling therapy
Wide-necked aneurysms pose the greatest technical difficulty for surgical clipping without complications. In our case, angiogram could not reveal a neck of aneurysm obviously (figure 3). Therefore, we selected surgical treatment initially. Then, we made a plan of endovascular treatment followed surgical treatment if complete neck clipping could not be achieved. In this case, complete neck clipping was abandoned because vascular stenosis was yielded at an origin of anterior branch of middle cerebralartery by slide of clip into side of parent artery. Incomplete neck clipping reduced the size of neck from 8 mm to 2 mm, whereby endovascular treatment 1 week after surgical treatmentcould be performed safely with near complete occlusion. Previous reports already referred endovascular coil embolization after surgical clipping 11-13.
Most of them reported endovascular treatment for incidentally residual aneurysms. In order to achieve effective occlusion of aneurysms using this technique, it is important that intentionally incomplete neck clipping is done in consideration of safe and easy endovascular procedure. We believed that this technique is suitable for wide-necked aneurysm with complex vascular anatomy, e.g. bifurcation of middle cerebral artery aneurysm or top of basilar artery aneurysm.
Scaffolding technique
Modality of endovascular treatment for large vertebral artery aneurysm is parent artery occlusion or intraaneurysmal embolization. In unilateral vertebral artery occlusion, rate of morbidity and mortality was reported about 7% 14. We explained the effectiveness and therisks of surgical treatment and endovascular treatment to patient and his family, and they chose the endovascular treatment using scaffolding technique. Advancement of intravascular stent technology permits the deposition into intracranial vessels15.
Recently some investigators reported successful embolization using scaffolding technique 16-18. We believed that indication of this technique is aneurysm with < 1 of sac/neck ratio. The past reports, however, long-term follow-up did not indicate. In large aneurysm with wide neck, recanalization due to coil compaction is encountered frequently. In this case, second embolization was needed for recanalization. Therefore, in the future it is necessary to evaluate this problem in this technique.
Conclusions
Though our experience is small series, endovascular treatment of cerebral aneurysms with wide-neck and bad shape using remodeling technique, combined operation and endovascular approach, scaffolding technique have proven safe and effective.
These techniques can contribute to extend the therapeutic spectrum of endovascular treatment with cerebral aneurysms, such as wide-necked and badly shaped aneurysms that could not achieve complete occlusion or fail the procedure using standard embolization procedure. These additional techniques must be chosen according to aneurysmal nature (site, size and shape) and patient's condition.
References
- 1.Guglielmi G, Viñuela F, et al. Electrothrombosis of saccular aneurysms via endovascular approach. Part 2: Preliminary clinical experience. J Neurosurg. 1991;75:8–14. doi: 10.3171/jns.1991.75.1.0008. [DOI] [PubMed] [Google Scholar]
- 2.Graves V, Strother C, et al. Early treatment of ruptured aneurysms with Guglielmi detachable coils: effect on subsequent bleeding. Neurosurgery. 1995;37:640–648. doi: 10.1227/00006123-199510000-00006. [DOI] [PubMed] [Google Scholar]
- 3.Pierot L, Boulin A, et al. Selective occlusion of basilar artery aneurysms using Controlled detachable coils: report of 35 cases. Neurosurgery. 1996;38:948–954. doi: 10.1097/00006123-199605000-00019. [DOI] [PubMed] [Google Scholar]
- 4.Malisch T, Guglielmi G, et al. Intracranial aneurysms treated with the Guglielmi detachable coil: midterm results in a consecutive series of 100 patients. J Neurosurg. 1997;87:176–183. doi: 10.3171/jns.1997.87.2.0176. [DOI] [PubMed] [Google Scholar]
- 5.Zubillaga A, Guglielmi G, et al. Endovascular occlusion of intracranial aneurysms with electrically detachable coils: correlation of aneurysm neck size and treatment results. Am J Neuroradiol. 1994;15:815–820. [PMC free article] [PubMed] [Google Scholar]
- 6.McDougall C, Halbach V, et al. Endovascular treatment of basilar tip aneurysms using electrolytically detachable coils. J Neurosurg. 1996;84:393–399. doi: 10.3171/jns.1996.84.3.0393. [DOI] [PubMed] [Google Scholar]
- 7.Moret J, Cognard C, et al. The “Remodelling Technique” in the treatment of wide neck intracranial aneurysms angiographic results and clinical follow-up in 56 cases. Interventional Neuroradiology. 1997;3:21–35. doi: 10.1177/159101999700300103. [DOI] [PubMed] [Google Scholar]
- 8.Levy D, Ku A. Balloon-assisted coil placement in widenecked aneurysms. J Neurosurg. 1997;86:724–727. doi: 10.3171/jns.1997.86.4.0724. [DOI] [PubMed] [Google Scholar]
- 9.Mericle R, Wakhloo A, et al. Temporary balloon protection as an adjunct to endosaccular coiling of widenecked cerebral aneurysms: technical note. Neurosurgery. 1997;41:975–978. doi: 10.1097/00006123-199710000-00045. [DOI] [PubMed] [Google Scholar]
- 10.Nakahara T, Kutsuna M, et al. Coil embolization of a large, wide-necked aneurysm using a double coil-delivered microcatheter technique in combination with a balloon-assisted technique. Neurol Res. 1999;21:324–326. doi: 10.1080/01616412.1999.11740939. [DOI] [PubMed] [Google Scholar]
- 11.Cekirge H, Islak C, et al. Endovascular coil embolization of residual or recurrent aneurysms after surgical clipping. Acta Radiol. 2000;41:111–115. doi: 10.1080/028418500127344957. [DOI] [PubMed] [Google Scholar]
- 12.Forsting M, Albert F, et al. Coil placement after clipping: endovascular treatment of incompletely clipped cerebral aneurysms. Report of two cases. J Neurosurg. 1996;85:966–969. doi: 10.3171/jns.1996.85.5.0966. [DOI] [PubMed] [Google Scholar]
- 13.Bavinzski G, Talazoglu V, et al. Coiling of recurrent and residual cerebral aneurysms unsuccessful clipping. Minim Invasive Neurosurg. 1999;42:22–26. doi: 10.1055/s-2008-1053363. [DOI] [PubMed] [Google Scholar]
- 14.Aymard A, Gobin Y, et al. Endovascular occlusion of vertebral arteries in the treatment of unclippable vertebrobasilar aneurysms. J Neurosurg. 1991;74:393–398. doi: 10.3171/jns.1991.74.3.0393. [DOI] [PubMed] [Google Scholar]
- 15.Nakahara T, Kurisu K, et al. Treatment of vertebral dissecting aneurysm with a balloon-expandable stent and Guglielmi detachable coils. Interventional Neuroradiology. 1999;5:171–177. doi: 10.1177/159101999900500211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mericle R, Lanzino G, et al. Stenting and secondary coiling of intracranial internal carotid artery aneurysm: technical case report. Neurosurgery. 1998;43:1229–1234. doi: 10.1097/00006123-199811000-00130. [DOI] [PubMed] [Google Scholar]
- 17.Lylyk P, Ceratto R, et al. Treatment of a vertebral dissecting aneurysm with stents and coils: technical case report. Neurosurgery. 1998;43:385–388. doi: 10.1097/00006123-199808000-00132. [DOI] [PubMed] [Google Scholar]
- 18.Sekhon L, Morgan M, et al. Combined endovascular stent implantation and endosaccular coil placement for the treatment of a wide-necked vertebral artery aneurysm: Technical case report. Neurosurgery. 1998;43:380–384. doi: 10.1097/00006123-199808000-00127. [DOI] [PubMed] [Google Scholar]