Abstract
Objective
Successful resuscitation from cardiac arrest requires the delivery of high-quality chest compressions, encompassing parameters such as adequate rate, depth, and full recoil between compressions. The lack of compression recoil (“leaning” or “incomplete recoil”) has been shown to adversely affect hemodynamics in experimental arrest models, but the prevalence of leaning during actual resuscitation is poorly understood. We hypothesized that leaning varies across resuscitation events, possibly due to rescuer and/or patient characteristics and may worsen over time from rescuer fatigue during continuous chest compressions.
Methods
This was an observational clinical cohort study at one academic medical center. Data were collected from adult in-hospital and Emergency Department arrest events using monitor/defibrillators that record chest compression characteristics and provide real-time feedback.
Results
We analyzed 112,569 chest compressions from 108 arrest episodes from 5/2007 to 2/2009. Leaning was present in 98/108 (91%) cases; 12% of all compressions exhibited leaning. Leaning varied widely across cases: 41/108 (38%) of arrest episodes exhibited <5% leaning yet 20/108 (19%) demonstrated >20% compression leaning. When evaluating blocks of continuous compressions (>120 sec), only 4/33 (12%) had an increase in leaning over time and 29/33 (88%) showed a decrease (p<0.001).
Conclusions
Chest compression leaning was common during resuscitation care and exhibited a wide distribution, with most leaning within a subset of resuscitations. Leaning decreased over time during continuous chest compression blocks, suggesting that either leaning may not be a function of rescuer fatiguing, or that it may have been mitigated by automated feedback provided during resuscitation episodes.
Keywords: cardiopulmonary resuscitation, cardiac arrest, sudden death, chest compression, quality of care
1. Introduction
Despite the life-saving potential of well-performed cardiopulmonary resuscitation (CPR), clinical investigations have revealed suboptimal CPR quality during resuscitation efforts for both in-hospital and out-of-hospital cardiac arrest. Multiple parameters of CPR quality such as the rate and depth of chest compressions, ventilation rate, and pauses in CPR delivery, have been shown to frequently deviate from the consensus resuscitation guideline recommendations during actual performance.1–4
Chest compression leaning (or “incomplete recoil”) occurs when a rescuer does not completely release downward force from the chest wall after a chest compression (see Fig. 1), with or without lifting hands off the chest between compressions. Both the American Heart Association and European Resuscitation Council guidelines recommend complete chest wall decompression during CPR.5–6 Animal data have shown the resulting residual force from leaning to negatively affect hemodynamics by decreasing coronary and cerebral pressures.7–8 Chest compressions circulate blood in part by creating negative intrathoracic pressure during the upstroke of the compression, thereby facilitating venous return through a “bellows” action (chest volume expansion). Leaning may prevent or reduce the negative intrathoracic pressure during the release portion of chest compressions, thereby impeding blood flow and reducing the effectiveness of CPR.7–8
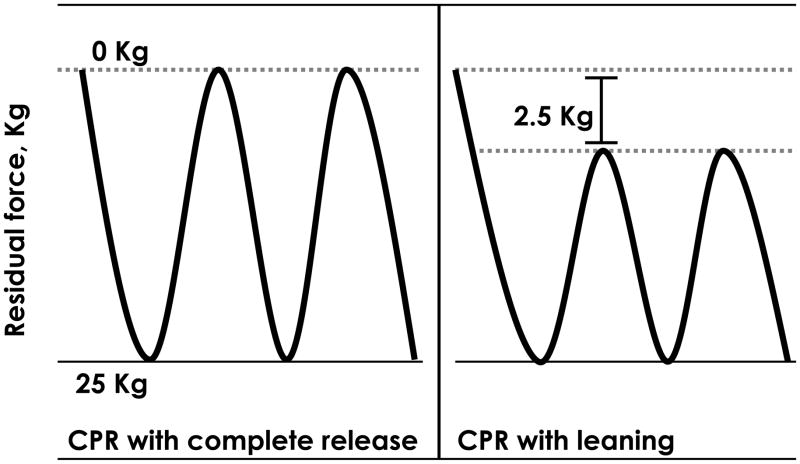
Figure 1.
Schematic of chest compression delivery. The chest compression waveform on the left represents high quality compressions with no residual force (complete release). The waveform on the right shows compressions with a residual force of 2.5 kg, defined in this investigation as the threshold for leaning.
A small number of investigations have documented the presence of leaning during adult out-of-hospital and Emergency Department cardiac arrest resuscitations.9–11 Additionally, a study of in-hospital pediatric resuscitation revealed a high prevalence of leaning during CPR.12 The frequency and characteristics of leaning during adult inhospital CPR remain unknown. It is also unclear whether rescuer and/or patient factors affect rescuer leaning, whether it worsens with fatigue during CPR delivery, or if it is minimized by real-time, automated CPR feedback. We performed the current investigation in an effort to address these questions.
2. Methods
This was an observational, clinical cohort study of adult in-hospital cardiac arrest events occurring at one hospital using CPR-sensing monitor/defibrillators that provide real-time, audiovisual feedback. The Institutional Review Board of the Hospital of the University of Pennsylvania approved this study. All data were appropriately collected and de-identified in a manner compliant with the Health Insurance Portability and Accountability Act (HIPAA) regulations to ensure subject confidentiality.
2.1. Data collection
Clinical data, including patient demographics and event characteristics, were obtained from patient medical records and written resuscitation transcripts. Resuscitation performance and rhythm data were collected using a commercially available monitor/defibrillator with CPR-sensing and recording capabilities (MRx-QCPR, Philips Healthcare, Andover, MA). The device records compression rate, depth, force, and incomplete release (i.e., chest compression leaning) as well as other parameters of CPR performance. Additionally, the MRx-QCPR defibrillator provides real-time feedback, alerting rescuers by way of corrective voice and screen prompts when CPR parameters deviate significantly from consensus resuscitation guidelines. The version of MRx-QCPR used in this study displayed visual feedback information on the monitor display but not on the CPR sensing equipment itself.
2.2. Study site and subjects
This study took place at the Hospital of the University of Pennsylvania, a tertiary-care academic medical center. Data collection occurred within five areas of the hospital: the Emergency Department (ED), Medical Intensive Care Unit (MICU), Cardiac Care Unit (CCU), and two general medicine wards. All health care providers at the study location were instructed in the use of the MRx-QCPR system prior to the start of the study and received intermittent refresher training to ensure appropriate use of the devices. During the duration of data collection, all five hospital areas employed only MRx-QCPR defibrillators, with each location storing and using multiple MRx-QCPR devices.
We included for analysis all adults ( 18 years old) who suffered cardiac arrest between May 2007 and February 2009 for whom corresponding CPR data from an MRx-QCPR monitor/defibrillator were available. Cardiac arrests were excluded if the CPR recording sensor was not deployed or if chest compressions were not provided. The chest compression leaning analyses performed in this investigation have not been included in previous publications; however, other aspects of resuscitation care from an overlapping portion of our subject cohort have been reported elsewhere.13
2.3. Data analysis
Custom CPR analysis software designed specifically for the MRx-QCPR was used to graphically and numerically analyze CPR parameters (QCPR Review 2.1.0, Laerdal Medical Corporation, Stavanger, Norway). We performed additional statistical analysis using a spreadsheet application (Excel 2003, Microsoft Corp., Redmond, WA). Fisher’s Exact Test was employed for group comparisons. For quartile analyses, it was decided a priori to compare the lowest quartiles of chest compression rate and depth with the other three, and therefore the Bonferroni correction method was employed to establish a significance (alpha) threshold for the three resultant comparisons. That is, significance was defined in the quartile analyses as alpha = (0.05/3) = 0.016. In the comparison of leaning before and after feedback prompts, a paired T-test was used to test for significance.
This study defined leaning as the presence of a force of ≥2.5 kg at the point of minimum chest compression depth between two compressions during CPR delivery (see Fig. 1), which represented the monitor/defibrillator feedback cut-off for leaning as well. This threshold was based on definitions from prior clinical work9 and originally established in part based on two prior studies: Tomlinson et al. 8 found that on average, during adult CPR, rescuers provide chest compressions with a force of approximately 25–30 kg; and Zuercher et al. demonstrated in a piglet model of cardiac arrest that a leaning force equaling 10% of the maximum compression force resulted in clinically relevant negative hemodynamic effects.14 Conversely, complete release (lack of leaning) was defined as any residual force on the chest of <2.5 kg. Percent leaning was calculated for each case and for the entire chest compression cohort, defined as: (compressions with incomplete release / total compression count) × 100.
Typically, multiple health care providers perform chest compressions during any given in-hospital resuscitation event; rescuer switches and identities are typically not documented in cardiac arrest records. In order to examine potential differences between rescuers, the leaning percentage was calculated for the first segment of continuous chest compressions (“block”) from each cardiac arrest episode. A block was defined as a minimum of 30 sec of compressions without pauses, with a pause defined as an interruption in compressions >1 sec. This ensured the highly probable assessment of a single rescuer per block. This approach has been used in a prior investigation.13 Episodes lacking uninterrupted blocks with a duration of >30 sec were excluded from this analysis.
In an effort to examine the potential relationship between leaning and other CPR quality parameters, we compared leaning percentage against both chest compression rate and depth, grouped by quartiles. We performed additional comparisons between leaning and patient characteristics (height, weight, Body Mass Index (BMI), age, gender, race, initial rhythm) as well as between leaning and time of day for a given cardiac arrest (day defined as 0700–1900, night defined as 1900-0700). BMI, height, weight, and age were evaluated by quartile analyses.
We then sought to determine whether chest compression leaning was a function of rescuer fatiguing, in which case an increase in leaning percentage might be observed over time of continuous chest compression delivery by individual rescuers. In other words, this study focused on prolonged single-rescuer chest compression duration as a surrogate marker to evaluate potential fatigue during CPR delivery. Similar to the rescuer analysis, every ≥120 sec continuous chest compression block was analyzed – first by subdivision into 30 sec segments and then by calculating the leaning percentage for each segment. This time interval of 120 sec was chosen based on our prior work evaluating fatigue during actual in-hospital CPR.13 Time sequential segments were evaluated to assess for any change in leaning over time.
To determine the effect of real-time CPR audiovisual feedback on leaning, the instances of corrective feedback in each ≥ 120 sec block were evaluated. The defibrillator delivered corrective feedback messages in response to short runs of consecutive chest compressions exhibiting leaning, as specified by the 2.5 kg threshold. The leaning percentage in the 10 sec before and 10 sec after each instance of audio feedback was calculated. If additional feedback messages occurred within the latter 10 sec, the percent leaning was alternatively calculated between the first message to 10 sec after the final message in the sequence. In this fashion, the leaning percentage before and after corrective messages was then determined and quantified for all instances of such feedback.
3. Results
A total of 223 in-hospital cardiac arrest events took place during the study period, of which 112 events met eligibility criteria by virtue of occurring in the relevant clinical settings with a CPR-recording defibrillator available and CPR performed. After exclusion of four cases that did not have the recording sensor correctly applied, a total of 108 cardiac arrest resuscitations from 95 unique patients met final criteria for inclusion in this investigation. Of these events, 98/108 (91%) contained instances of chest compression leaning. The 108 resuscitation events included 112,569 chest compressions, with 13,270 of them exhibiting leaning (12% of total chest compressions). Patient demographics and resuscitation performance characteristics are shown in Tables 1 and 2, respectively.
Table 1.
Patient demographics and clinical resuscitation data
| Number of resuscitation episodes: | 108 |
| Number of unique patients: | 95 |
| Patient age (yrs), mean ± SD: | 58.3 ± 17.3 |
| Gender, n (%): | |
| Female | 42 (44) |
| Male | 50 (53) |
| Event location, n (%): | |
| ICU | 83 (77) |
| Non-ICU | 4 (4) |
| ED | 21 (19) |
| Initial arrest rhythm, n (%): | |
| VF/VT | 25 (23) |
| PEA | 56 (52) |
| Asystole | 23 (21) |
| Other/Unknown | 4 (4) |
| Time of event, n (%) | |
| 7:00 am – 6:59 pm | 60 (56) |
| 7:00 pm – 6:59 am | 48 (44) |
| ROSC, n (%): | 60 (56) |
| Survival to discharge, n (%): | 9 (10) |
The demographic data (aside from location and duration) from three patients were unobtainable. More cardiac arrest episodes than patients are represented because some patients experienced more than one arrest event. ICU, Intensive Care Unit; ED, Emergency Department; VF/VT, ventricular fibrillation/ventricular tachycardia; PEA, pulseless electrical activity; ROSC, return of spontaneous circulation.
Table 2.
CPR performance parameters during cardiac arrest episodes
| Initial five minutes of arrest episode (n=108) | Entire cardiac arrest episode (n=108) | |
|---|---|---|
| Chest compression data | ||
| Compression Rate /min | ||
| Mean (SD) | 107 (10) | 106 (7) |
| Cases with rate<80 (%) | 0 | 0 |
| Cases with rate<90 (%) | 4 | 3 |
| Cases with rate>110 (%) | 35 | 29 |
| Compression depth, mm | ||
| Mean (SD) | 48.7 (9.9) | 48.8 (9.0) |
| Cases w depth<38 mm (%) 13 | 8 | |
| Leaning percentage | ||
| Mean (SD) | 11 (14) | 10 (10) |
|
| ||
| Compression Interruption | ||
| No-flow fraction, mean (SD) | 0.3 (0.3) | 0.2 (0.2) |
| Time with no-flow fraction >0.20 (%) | 41 | 37 |
No-flow fraction is defined as the cumulative no-flow time (time without pulse or chest compressions) during a given resuscitation event, divided by the total time without a pulse during that same event. SD, standard deviation.
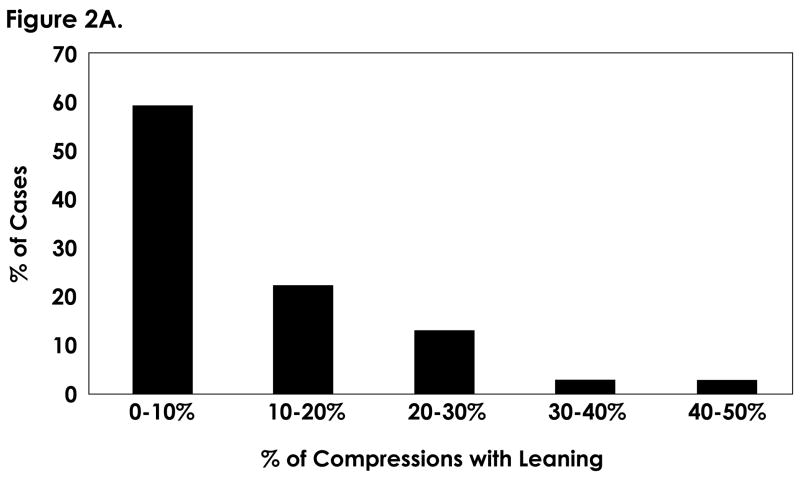
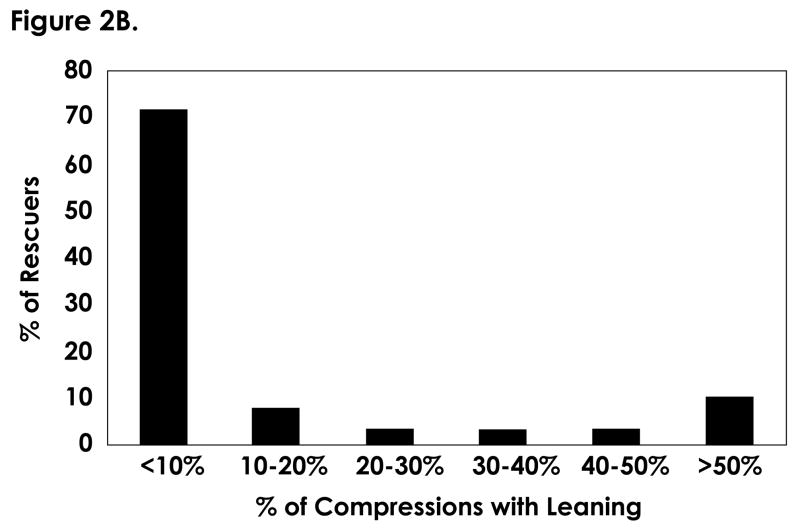
The prevalence of leaning across all cases and initial chest compressions blocks is shown in Fig. 2. While 41/108 (38%) cardiac arrest episodes exhibited <5% leaning, 20/108 (19%) exhibited more than 20 % leaning, demonstrating a relatively wide distribution of this phenomenon. The leaning distribution within the initial blocks qualitatively resemble the distribution from overall episodes, with 58/88 (66%) exhibiting less than 5% leaning and 18/88 (21%) exhibiting more than 20% leaning. Additionally, the leaning distribution did not differ significantly between event locations such as MICU vs. ED (data not shown).
Figure 2.
Distribution of chest compression leaning. Fig. 2A, leaning percentage among all cases. While most cases involve a low percentage of leaning, a wide distribution exists and 20/108 (19%) involve >20% leaning. Fig. 2B, leaning percentage among all rescuers. The two analyses reveal similar distributions.
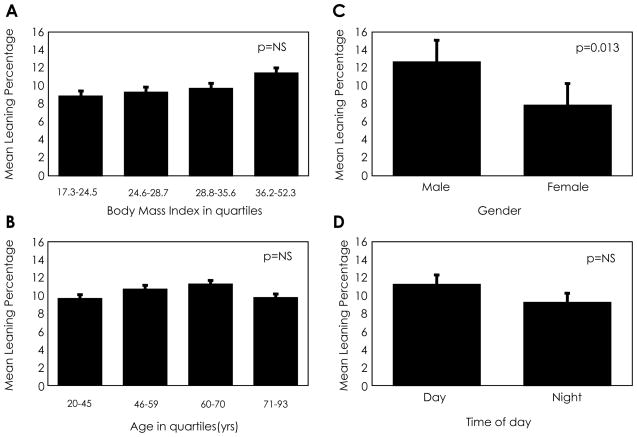
The quartile analyses comparing leaning with respect to chest compression rate and depth is shown in Table 3. Leaning percentage demonstrated a statistically significant difference when comparing the highest and lowest quartiles of compression rate (25.1% vs. 13.6%, p=0.012). Leaning did not have any significant relationship with depth by quartile analysis. Figure 3 shows relationships between leaning and other patient characteristics and external factors examined in this study. Leaning only significantly differed between patient genders, with male cardiac arrest victims receiving more leaning than females (p=0.013). Additionally, leaning did not show any significant relationship to initial rhythm, height, weight, or patient race (data not shown)
Table 3.
Quartile analyses comparing leaning against chest compression rate and depth
| Rate quartile (min−1) | Average leaning (%) | p-value |
|---|---|---|
| 1 (62–102) | 13.6 | |
| 2 (102–108) | 9.6 | |
| 3 (108–114) | 9.7 | |
| 4 (114–153) | 25.1 | 0.012 |
|
| ||
| Depth quartile (mm) | Average leaning (%) | |
|
| ||
| 1 (23–42) | 15.7 | |
| 2 (42–48) | 18.6 | |
| 3 (48–56) | 9.4 | |
| 4 (56–77) | 14.5 | NS |
P values represent comparisons between first and last quartile in each analysis.
NS, not significant.
Figure 3.
Leaning analyzed against patient and external factors. A, chest compression leaning analyzed by quartiles of cardiac arrest victim body-mass index (BMI); B, chest compression leaning by quartiles of cardiac arrest victim age; C, chest compression leaning by quartiles of cardiac arrest victim gender; D, chest compression leaning by event time of day. The only variable with a significant difference found was between gender of chest compression recipients (p=0.013).
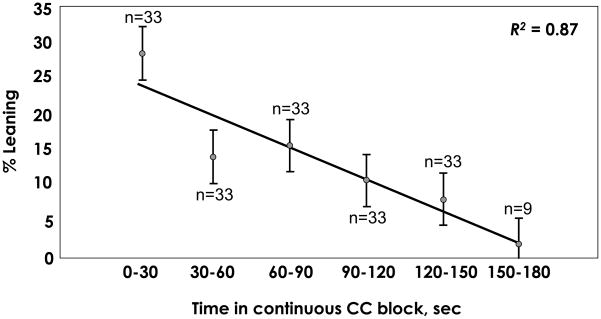
To address the question of whether chest compression leaning increases with rescuer fatigue, we identified and assessed continuous chest compression blocks for changes in leaning over time. Contrary to our hypothesis, we found that the leaning percentage as performed by a single rescuer decreased over time among 29/33 (88%) blocks of continuous chest compressions (and therefore rescuers). Figure 4 shows the average leaning percentage per each 30 sec segment of the continuous blocks with a best-fit curve (R2=0.87).
Figure 4.
Average decline in chest compression leaning percentage for the rescuers (n values shown for each epoch) who completed ≥120 sec continuous blocks of CPR, as measured by consecutive 30 sec segments. The regression coefficient is shown.
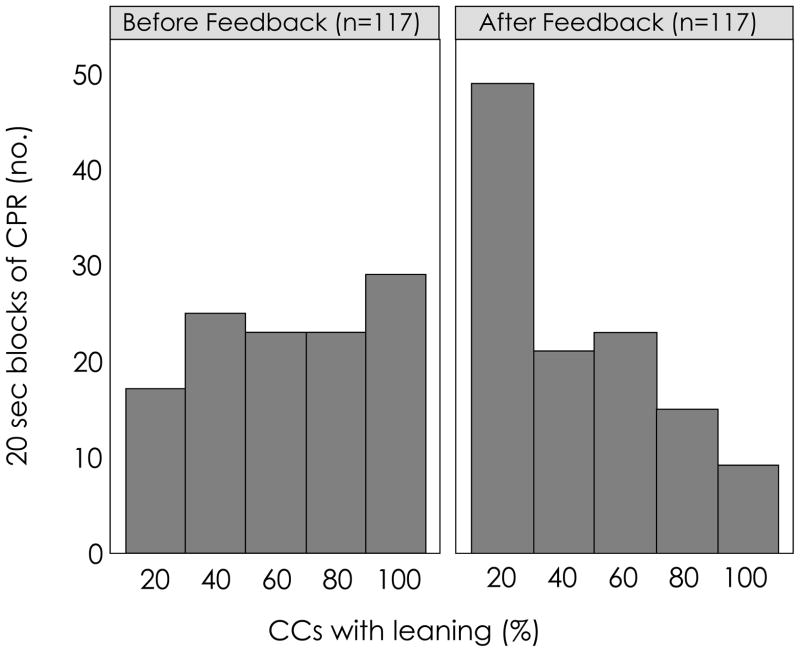
Of the 33 initial continuous chest compression blocks with a ≥ 120 sec duration, 25 contained a total of 117 corrective audio feedback, alerting rescuers to their leaning. Of the 8 blocks without leaning feedback messages, 8/8 (100%) had no more than one instance of leaning per 30 sec. Figure 5 shows a frequency distribution of leaning before and after feedback in these 117 instances of leaning corrective messages. We found that every rescuer reduced their leaning to some extent after verbal feedback. The reduction in leaning percentage after feedback prompting was statistically significant (56±28% vs. 35±27%, p<0.001).
Figure 5.
Frequency histogram of chest compression leaning percentage before and after feedback messages for 25 individual rescuers in 117 instances of feedback. Leaning frequency declined after corrective feedback messages were given (comparison of mean percentages: 56±28% vs. 35±27%, p<0.001).
4. Discussion
Our work has demonstrated that in-hospital CPR providers exhibit a wide range of leaning during chest compression delivery. In addition, the majority of in-hospital cardiac arrest resuscitations in our cohort (91%) demonstrated some degree of leaning. One other investigation has provided data on chest compression leaning from adult, hospital-based, cardiac arrest resuscitations.9 Our finding of 12% overall leaning percentage is similar to the 11% found in their study of CPR performance in an Austrian ED. It is unknown from their data whether leaning was evenly dispersed or concentrated by provider and event. In contrast, an evaluation of out-of-hospital CPR performance in Europe demonstrated no leaning in a cohort of 176 arrest events.2 However, this latter study set the leaning threshold at ≥ 4 kg, instead of the ≥ 2.5 kg level used in our analysis. The use of different techniques to measure leaning may also confound comparison between studies. For instance, while Losert et al.9 used a similar technology and software combination as the current investigation, Aufderheide et al. performed their measurements by way of direct observation and electronically measured airway pressures.11 This difficulty in comparison between studies suggests the need for future standardization of CPR performance definitions.
Laboratory investigations have suggested that leaning during chest compressions (using a threshold of residual leaning force equivalent to 10% of maximal compression force) decreases coronary and cerebral pressures, and that this effect remains in place for a significant period of time after the cessation of leaning.7–8 Therefore, even short periods of leaning during resuscitation may have deleterious effects on tissue perfusion during CPR and resuscitation outcomes.
While a majority of cardiac arrests events in this investigation contained small leaning percentages, many cases did contain a relatively large amount, with leaning affecting as many as 44% of chest compressions in a given episode. This suggests that the overall leaning percentage (12%) does not accurately represent the potential clinical impact on some cardiac arrest victims in our cohort. In an attempt to identify the cause of this wide variation, we found that leaning does not correlate with a set of patient characteristics or external factors other than patient gender, leaving the disparity unexplained by simple univariate analysis. However, it is important to note that CPR quality represents a complex measure with multiple interacting factors, such that any single parameter such as leaning is likely influenced by both other CPR performance and rescuer characteristics. A larger case sample size than contained in our cohort might allow for multivariate regression analysis to better evaluate these factors.
On the other hand, our analysis of initial blocks of chest compressions (representing individual CPR providers) suggests that the wide range of leaning might represent a rescuer-specific phenomenon. Reasons for possible differences between rescuer leaning behaviors remain unclear, but may be related to rescuer training and physical characteristics. An investigation of simulated CPR by Verplancke et al. illustrated that characteristics such as rescuer self-confidence, time from last training, and time from last resuscitation experience affected rescuer CPR quality.15 Further work is needed to examine the relationship between leaning and these factors as well as patient characteristics such as body habitus or chest compliance.
Our data also suggest that leaning may not increase over time when a single rescuer performs continuous chest compressions, contrary to our hypothesis that increasing leaning might represent a fatiguing phenomenon. As a note of caution, this is a small, potentially self-selected group of rescuers who performed chest compressions without pauses, and few continuous blocks were longer than two minutes in any case. Nevertheless, despite previous studies showing that a single rescuer’s CPR quality (e.g., compression depth) worsens over time, our current work indicates that increasing time in a block of continuous chest compressions actually negatively correlates with leaning, at least under conditions of CPR monitoring and corrective feedback.13,16–17 An investigation of CPR quality in pediatric resuscitation by Sutton et al. corroborates this finding of more frequent leaning at the beginning of a rescuer’s chest compression performance.18 Two hypotheses might explain this: one is that rescuers could require some time to establish correct chest compression performance, or alternatively, specific to our study site, perhaps rescuers simply responded to the real-time, automated feedback and corrected any chest compression leaning behavior. Prior work has established that real-time feedback modifies other CPR parameters.19–20 Our analysis found that rescuers exhibited less leaning after feedback messages, suggesting that it indeed may have played a role in decreasing leaning during chest compression delivery.
Limitations
It is important to note several limitations in our work. First, all of the resuscitation episodes analyzed in this study involved the use of a defibrillator that provided real-time, corrective feedback that may have influenced leaning behaviors. Also, the majority of the cardiac arrest events occurred in the critical care setting, where providers are arguably more experienced in cardiac arrest care than those on most general wards. Finally, the current investigators (and consequently staff at the study hospital) have focused for a number of years on improving hospital-wide cardiac arrest care through education and quality improvement activities.20 Taking these points together, our work likely underestimates the prevalence of leaning compared to other settings of CPR performance.
A second limitation is that our study was not powered to test the relationship between leaning and clinical outcomes. Given the multitude of patient and resuscitation quality factors that influence cardiac arrest outcome, such a relationship would require a much larger cohort. A third limitation lies in the choice of a chest compression leaning threshold of ≥2.5 kg. Despite being based upon animal models and prior clinical work, the quantitative effects of leaning on hemodynamics during clinical CPR are unknown. Further work correlating clinical hemodynamics and chest compression parameters such as leaning is required. Finally, we were unable to gather mattress characteristic data for the resuscitations; other work has demonstrated that mattresses deflection confounds CPR quality measurement.21–22 The effect of mattress compliance on chest compression leaning is unknown.
5. Conclusion
We found that chest compression leaning occurred in the vast majority of in-hospital cardiac arrest resuscitation episodes in our cohort (91%). We also found a broad distribution of leaning prevalence among cases and chest compression blocks, with most leaning coming from a subset of events. We also found that rescuers’ leaning frequency decreased as they provided chest compressions for increasing lengths of time. Rescuer response to automated, verbal feedback may explain this phenomenon. Future studies should build on these findings to determine whether patient or rescuer characteristics affect leaning, as such information could influence future CPR guidelines and training protocols. Leaning is one of a number of CPR parameters that potentially should be measured during investigations that report clinical CPR quality.23
Acknowledgments
We thank the resident physicians and inpatient nursing staff at the Hospital of the University of Pennsylvania for their involvement with our research and their efforts to provide excellent care to patients suffering cardiac arrest.
This study was partially funded by Philips Healthcare, which had no role in the design and conduct of the study, analysis of the findings, or the drafting of this manuscript. This work was also partially funded by a National Institutes of Health Career Development Award to Dr. Abella (NHLBI 5K23HL083082).
Footnotes
Conflict of interest
Drs. Becker and Abella have received honoraria and research funding from Philips Healthcare. Dr. Abella has additionally received honoraria from Medivance Corporation, and research funding from the American Heart Association. Dr. Becker has received research funding from Laerdal Medical Corporation.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Abella BS, Alvarado JP, Myklebust H, et al. Quality of cardiopulmonary resuscitation during in-hospital cardiac arrest. JAMA. 2005;293:305–10. doi: 10.1001/jama.293.3.305. [DOI] [PubMed] [Google Scholar]
- 2.Wik L, Kramer-Johansen J, Myklebust H, et al. Quality of cardiopulmonary resuscitation during out-of-hospital cardiac arrest. JAMA. 2005;293:299–304. doi: 10.1001/jama.293.3.299. [DOI] [PubMed] [Google Scholar]
- 3.Aufderheide TP, Sigurdsson G, Pirrallo RG, et al. Hyperventilation-induced hypotension during cardiopulmonary resuscitation. Circulation. 2004;109:1960–5. doi: 10.1161/01.CIR.0000126594.79136.61. [DOI] [PubMed] [Google Scholar]
- 4.Valenzuela TD, Kern KB, Clark LL, et al. Interruptions of chest compressions during emergency medical systems resuscitation. Circulation. 2005;112:1259–65. doi: 10.1161/CIRCULATIONAHA.105.537282. [DOI] [PubMed] [Google Scholar]
- 5.2005 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2005;112:IV1–203. doi: 10.1161/CIRCULATIONAHA.105.166550. [DOI] [PubMed] [Google Scholar]
- 6.Handley AJ, Koster R, Monsieurs K, Perkins GD, Davies S, Bossaert L. European Resuscitation Council guidelines for resuscitation 2005. Section 2. Adult basic life support and use of automated external defibrillators. Resuscitation. 2005;67 (Suppl 1):S7–23. doi: 10.1016/j.resuscitation.2005.10.007. [DOI] [PubMed] [Google Scholar]
- 7.Yannopoulos D, McKnite S, Aufderheide TP, et al. Effects of incomplete chest wall decompression during cardiopulmonary resuscitation on coronary and cerebral perfusion pressures in a porcine model of cardiac arrest. Resuscitation. 2005;64:363–72. doi: 10.1016/j.resuscitation.2004.10.009. [DOI] [PubMed] [Google Scholar]
- 8.Zuercher M, Hilwig RW, Ranger-Moore J, et al. Leaning during chest compressions impairs cardiac output and left ventricular myocardial blood flow in piglet cardiac arrest. Crit Care Med. 2010;38:1141–6. doi: 10.1097/CCM.0b013e3181ce1fe2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Losert H, Sterz F, Kohler K, et al. Quality of cardiopulmonary resuscitation among highly trained staff in an emergency department setting. Arch Intern Med. 2006;166:2375–80. doi: 10.1001/archinte.166.21.2375. [DOI] [PubMed] [Google Scholar]
- 10.Kramer-Johansen J, Myklebust H, Wik L, et al. Quality of out-of-hospital cardiopulmonary resuscitation with real time automated feedback: a prospective interventional study. Resuscitation. 2006;71:283–92. doi: 10.1016/j.resuscitation.2006.05.011. [DOI] [PubMed] [Google Scholar]
- 11.Aufderheide TP, Pirrallo RG, Yannopoulos D, et al. Incomplete chest wall decompression: a clinical evaluation of CPR performance by EMS personnel and assessment of alternative manual chest compression-decompression techniques. Resuscitation. 2005;64:353–62. doi: 10.1016/j.resuscitation.2004.10.007. [DOI] [PubMed] [Google Scholar]
- 12.Niles D, Nysaether J, Sutton R, et al. Leaning is common during in-hospital pediatric CPR, and decreased with automated corrective feedback. Resuscitation. 2009;80:553–7. doi: 10.1016/j.resuscitation.2009.02.012. [DOI] [PubMed] [Google Scholar]
- 13.Sugerman NT, Edelson DP, Leary M, et al. Rescuer fatigue during actual inhospital cardiopulmonary resuscitation with audiovisual feedback: a prospective multicenter study. Resuscitation. 2009;80:981–4. doi: 10.1016/j.resuscitation.2009.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tomlinson AE, Nysaether J, Kramer-Johansen J, Steen PA, Dorph E. Compression force-depth relationship during out-of-hospital cardiopulmonary resuscitation. Resuscitation. 2007;72:364–70. doi: 10.1016/j.resuscitation.2006.07.017. [DOI] [PubMed] [Google Scholar]
- 15.Verplancke T, De Paepe P, Calle PA, De Regge M, Van Maele G, Monsieurs KG. Determinants of the quality of basic life support by hospital nurses. Resuscitation. 2008;77:75–80. doi: 10.1016/j.resuscitation.2007.10.006. [DOI] [PubMed] [Google Scholar]
- 16.Ashton A, McCluskey A, Gwinnutt CL, Keenan AM. Effect of rescuer fatigue on performance of continuous external chest compressions over 3 min. Resuscitation. 2002;55:151–5. doi: 10.1016/s0300-9572(02)00168-5. [DOI] [PubMed] [Google Scholar]
- 17.Ochoa FJ, Ramalle-Gomara E, Lisa V, Saralegui I. The effect of rescuer fatigue on the quality of chest compressions. Resuscitation. 1998;37:149–52. doi: 10.1016/s0300-9572(98)00057-4. [DOI] [PubMed] [Google Scholar]
- 18.Sutton RM, Maltese MR, Niles D, et al. Quantitative analysis of chest compression interruptions during in-hospital resuscitation of older children and adolescents. Resuscitation. 2009;124:494–9. doi: 10.1016/j.resuscitation.2009.08.009. [DOI] [PubMed] [Google Scholar]
- 19.Abella BS, Edelson DP, Kim S, et al. CPR quality improvement during in-hospital cardiac arrest using a real-time audiovisual feedback system. Resuscitation. 2007;73(1):54–61. doi: 10.1016/j.resuscitation.2006.10.027. [DOI] [PubMed] [Google Scholar]
- 20.Edelson DP, Litzinger B, Arora V, et al. Improving in-hospital cardiac arrest process and outcomes with performance debriefing. Arch Intern Med. 2008;168:1063–9. doi: 10.1001/archinte.168.10.1063. [DOI] [PubMed] [Google Scholar]
- 21.Perkins GD, Kocierz L, Smith SC, McCulloch RA, Davies RP. Compression feedback devices over estimate chest compression depth when performed on a bed. Resuscitation. 2009;80:79–82. doi: 10.1016/j.resuscitation.2008.08.011. [DOI] [PubMed] [Google Scholar]
- 22.Nishisaki A, Nysaether J, Sutton R, et al. Effect of mattress deflection on CPR quality assessment for older children and adolescents. Resuscitation. 2009;80:540–5. doi: 10.1016/j.resuscitation.2009.02.006. [DOI] [PubMed] [Google Scholar]
- 23.Kramer-Johansen J, Edelson DP, Losert H, Kohler K, Abella BS. Uniform reporting of measured quality of cardiopulmonary resuscitation (CPR) Resuscitation. 2007;74:406–17. doi: 10.1016/j.resuscitation.2007.01.024. [DOI] [PubMed] [Google Scholar]