Abstract
Background
Adverse respiratory effects in children with asthma are associated with exposures to nitrogen dioxide (NO2). Levels indoors can be much higher than outdoors. Primary indoor sources of NO2 are gas stoves, which are used for cooking by one-third of US households. We investigated effects of indoor NO2 exposure on asthma severity among an ethnically and economically diverse sample of children, controlling for season and indoor allergen exposure.
Methods
Children aged 5–10 years with active asthma (n=1,342), were recruited through schools in urban and suburban Connecticut and Massachusetts (2006–2009) for a prospective, year-long study with seasonal measurements of NO2 and asthma severity. Exposure to NO2 was measured passively for four, month-long, periods with Palmes tubes. Asthma morbidity was concurrently measured by a severity score and frequency of wheeze, night symptoms and use of rescue medication. We used adjusted, hierarchical ordered logistic regression models to examine associations between household NO2 exposure and health outcomes.
Results
Every 5 ppb increase in NO2 exposure above a threshold of 6 ppb was associated with a dose-dependent increase in risk of higher asthma severity score (odds ratio= 1.37 [95% confidence interval= 1.01 – 1.89]), wheeze (1.49 [1.09 – 2.03]), night symptoms (1.52 [1.16 – 2.00]) and rescue medication use (1.78 [1.33 – 2.38]).
Conclusions
Asthmatic children exposed to NO2 indoors, at levels well below the US Environmental Protection Agency outdoor standard (53 ppb), are at risk for increased asthma morbidity. Risks are not confined to inner-city children, but occur at NO2 concentrations common in urban and suburban homes.
Exposure to nitrogen dioxide (NO2), a byproduct of combustion and a respiratory irritant,1,2 can occur both indoors and outdoors. Gas appliances such as gas cooking stoves are primary sources indoors, where children spend large amounts of time. Gas stoves are used by approximately 39% of US households.3 Indoor levels where NO2 sources are present can be much higher than outdoors, where the primary source of NO2 is traffic. Exposure to NO2 continues to be a public health concern, especially with regard to the respiratory health of children with asthma.
A randomized controlled trial conducted in Australia has provided compelling evidence for an association between indoor NO2 exposure and adverse respiratory outcomes among children with asthma.4 The study, which involved replacing unflued gas heaters in selected schools with flued or electric heat, found improved average asthma morbidity over a 12-week period among students in the intervention schools. Two recent reviews of indoor environmental influences on asthma in children included NO2 as an important potential trigger of asthma morbidity.5,6 Both reviews summarized key studies dating back to the 1980’s and concluded that there is limited but suggestive evidence of associations between indoor NO2 exposure and asthma morbidity in children. Asthma morbidity measures used in studies of NO2 exposure include number of symptom-days or nights (wheeze, persistent cough, shortness of breath, chest tightness), frequency of rescue medication use, peak expiratory flow (PEF), upper and lower respiratory tract symptoms, limited speech, and forced expiratory volume (FEV).4,7–11 Many of these outcomes (especially symptoms and medication use) have limitations because they tend to be associated with access to healthcare and other socioeconomic factors. Confounding by these factors may account for some of the persistent inconsistency of asthma morbidity associations in the indoor NO2-exposure literature.
We previously conducted a study of 728 asthmatic children and associations of symptoms with measured indoor NO2,7 and found increased risks of wheeze and chest tightness associated with increased levels of NO2. Risks were confined, however, to children living in multifamily homes, a study characteristic associated with lower socioeconomic status, higher proportion of gas stove use and smaller proportion of asthma maintenance medication use. Analysis was based on a single NO2 measurement per child and did not account for other important factors such as atopic status or indoor allergen exposure.
The current analysis characterizes the relationship between measured indoor NO2 and concurrent asthma severity in a repeated measures analysis of a diverse population while considering some common mediating factors such as atopy, allergen exposure, seasonality, and socioeconomic status.
Methods
Participants
The Study of Traffic, Air quality and Respiratory health (STAR) was a prospective, one-year follow-up study of school-aged children with asthma. From 2006 through 2009, the study enrolled 1,401 children recruited through flyers distributed to schools in 23 cities and towns with gas lines in Connecticut and western Massachusetts. Volunteer families contacted the office and were screened (n = 2,175) via telephone. Eligible children (n = 1,642) were age 5–10 years, had a caregiver who spoke English and had active asthma defined as two or more of the following: physician diagnosis; asthma symptoms within the past 12 months (wheeze, persistent cough, chest tightness, shortness of breath); use of prescription asthma medication within the past 12 months (short-acting rescue medications and maintenance medications including inhaled steroids, systemic steroids, cromolyn, leukotriene inhibitors). The race/ethnicity distribution of children enrolled (i.e., those who completed a home interview and provided a blood sample) was similar to that of the towns where the children resided. Children (n = 1,342) who had complete information for health outcome measures and successful concurrent monitoring of indoor NO2 were included in this analysis.
Data collection
At the time of enrollment, a research assistant visited the home, obtained consent, and interviewed the mother or primary caregiver (respondent) to obtain demographic data (age, sex, race/ethnicity, mother’s education) and medical history of the child. The research assistant also observed and recorded housing type (single- or multi-family) and cooking appliance (gas or electric) of the enrollment residence. The mother was given a calendar to record daily symptoms and medication use.
At the end of each of the four, month-long monitoring periods, a research assistant phoned the respondent to obtain reports of daily symptoms and medication use and data on smoking in the home during the monitoring period. Sampling seasons were defined by winter and summer solstice and vernal and autumnal equinox. The midpoint of the observation period was used to assign the observation to a season.
At the end of one year, an exit interview was conducted via telephone. At this time a detailed address history was collected and the respondent provided housing characteristics such as housing type and type of cooking stove in each residence during the study. Housing type was later confirmed for all addresses with publicly available tax-assessor records.
Nitrogen dioxide (NO2) measurement
At the enrollment visit, the research assistant placed passive monitors (Palmes tubes)12 to measure NO2 in rooms where the child spent the most time awake (dayroom) and asleep (bedroom). After one month, the respondent was contacted via telephone and instructed to cap the NO2 monitors and return them in a pre-paid mailing envelope provided. Additional monitors were sent at three-month intervals for repeat sampling.
Palmes tubes were analyzed for NO2 concentration.12 Duplicate samples and field blanks were used for quality control. Regression analysis of duplicate samples (n=183) produced an adjusted R2 = 0.91 with a slope = 0.96 and intercept = 0.84. Coefficients of variation for the dayroom, dayroom duplicates, bedroom, and bedroom duplicates were 95.3, 94.5, 120.4 and 116.8 respectively. Dayroom and bedroom concentrations of NO2 were highly correlated (r = 0.89). In the present analysis, indoor NO2 concentrations are defined as the average of the two indoor measurements per home for each monitoring period. Measurements matching monitoring periods with complete health data were used for analysis (n = 4,499). Quintile concentration boundaries (in ppb) were ≤ 4.02, > 4.02 – 6.02, 6.03 – 8.88, 8.89 – 14.32, > 14.32.
Environmental sampling and allergy testing
At the enrollment visit, the research assistant collected dust from the main living area for measurement of common allergens, using a protocol described previously.7,13,14 Dust samples were assayed by enzyme-linked immunosorbent assay (ELISA) for detectable levels of dust mite allergens (Der p 1 ≥ 0.10 μg/g and Der f 1 ≥ 0.10 μg/g), cat allergen (Fel d 1 ≥ 0.12 μg/g), dog allergen (Can f 1 ≥ 0.12 μg/g) and cockroach allergen (Bla g 1 ≥ 0.60 U/g).
Using blood samples collected at the time of enrollment, serum for allergy testing was analyzed using the UniCAP system to determine total IgE and specific sensitivity to a panel of ten allergens. Atopy was defined as a sensitivity to any of the specific allergens, or as total IgE exceeding age-adjusted levels.15 For each allergen (Der p 1, Der f 1, Can f 1, Fel d 1, Bla g 1) a binary variable was used that included allergen-specific sensitization and allergen-specific exposure14: for this analysis “1” indicated a specific sensitivity and detectable allergen in the home, “0” indicated no sensitization to the specific allergen or no detectable allergen in the home.
Asthma severity
An asthma severity score based on the Global Initiative for Asthma guidelines16 was constructed for each observation period. The score was composed of two components: a symptom step and a medication step. We defined symptom steps as (0) no symptoms, (1) 1 – 3 symptom days and 0 –2 nights OR 0 days and any nights, (2) 4 – 19 symptom days OR 1 – 3 symptom days and 3 or more nights, (3) 20 or more symptom days OR 4 – 19 days and 5 or more nights, (4) more than 20 symptom days AND 10 or more nights. Medication steps were defined as (0) no asthma medication use, (1) rescue medication use only, (2) use of one controller medication (3) simultaneous use of two controller medications, (4) simultaneous use of three or more controller medications.
Symptom and medication steps were combined to determine overall asthma severity for each child in each monitoring period. A composite severity score of 0 was possible only if no symptoms were experienced and no asthma medication was used (symptom and medication step combination of (0, 0)). A score of 1 (“mild transient”) was assigned for symptom and medication step combinations of (1, 1), (0, 1) or (1, 0) respectively. A score of 2 (“mild persistent”) was assigned for symptom and medication step combinations of (2, 0), (2, 1), (0, 2) or (1, 2) respectively. Symptom and medications step combinations of (3, 0), (3, 1), (2, 2), (0, 3), (1, 3), respectively, were assigned a score of 3 (“moderate persistent”). Finally, a score of 4 (“severe persistent”) was assigned if either the symptom or medication step was a 4 OR with symptom and medication step combinations of (3, 2), (3, 3), (2, 3). (See Figure 1 in the paper by Gent et al., 201214)
Additional outcomes of interest included frequency of wheeze, night symptoms and use of rescue medication. For analysis, we classified these into categories corresponding to symptom steps for the severity score: “0,” “1 – 3,” “4 – 19,” and “more than 19” days per month.
Statistical analysis
Descriptive statistics and unadjusted associations between health outcomes, quintiles of NO2 exposure, and covariates were computed with SAS version 9.2 (Cary, NC). We examined both unadjusted and adjusted associations with ordered logistic regression (proportional odds model). The proportional odds assumption for all outcomes was tested using NLMIXED in SAS in unadjusted models with quintiles of NO2 exposure.
To allow for repeated measures of the health outcomes and exposure, we used a hierarchical ordered logistic model with a random term for subject. We assumed a normal distribution with unknown variance for subject effects. Associations between health outcomes and NO2 exposures, both unadjusted and adjusted for covariates, were examined using a Bayesian approach with a Markov Chain Monte Carlo strategy implemented in OpenBUGS.17 Bayesian estimates of model parameters were obtained by drawing samples from the posterior distribution using uninformative prior distributions (normal with mean zero and precision 1.0×10−6) for model parameters in the linear predictor, flat priors with ordered ranges for the ordinal parameters, and a gamma prior (with shape = 0.001 and scale = 0.001) specified for precision for the random-subject effect. Estimates for final models were based on a sample of 10,000 iterations with thinning of 20 following burn-in of 20,000 iterations.
Initially, unadjusted models were constructed with exposure represented as quintiles of NO2 concentration. We explored the shape of the exposure-response relationships between health outcomes and NO2 using a natural spline function of the natural log (ln) of NO2 18 specifying 5 knots (at NO2 concentrations representing the 10th, 25th, 50th, 75th and 95th percentiles of the distribution). Posterior means at exposure levels corresponding to the knots indicated that a threshold model would fit the data well and that the threshold was near the boundary of the second and third quintile of the NO2 distribution. Thus, in adjusted models we combined the bottom two exposure quintiles. Linear trends above the threshold were examined in a fully adjusted model using ln NO2 concentration as a continuous variable. Adjusted models for asthma severity score included age, sex, atopy, season of monitoring, race/ethnicity, mother’s education, smoking in the home and all five variables for combined specific sensitization and exposure to indoor allergens (Der p 1, Der f 1, Fel d 1, Can f 1 Bla g 1). Models for wheeze, night symptoms and rescue medication included age, sex, atopy, season of monitoring, and all five variables for combined specific sensitization and exposure to indoor allergens (Der p 1, Der f 1, Fel d 1, Can f 1 Bla g 1), as well as maintenance medication use (which represents a critical aspect of disease severity not included in these outcome measures). Due to co-linearity with maintenance medication use, race/ethnicity, mother’s education, and smoking in the home were excluded from models for wheeze, night symptoms and rescue medication.
Results
Each monitoring period was four weeks long, and all symptom and medication-use day counts were standardized to 28 days. The mean monitoring length was 33 (SD=7) days; median= 30 days; mode= 28 days. This analysis used NO2 concentrations and health outcomes measured concurrently during 4,499 monitoring period observations contributed by 1,342 subjects. Of these, 870 (65%) subjects contributed complete asthma symptom, medication use and concurrently measured indoor NO2 data for all monitoring periods; 202 (15%), 143 (11%), and 127 (9%) contributed data for 3, 2 or 1 monitoring periods, respectively. Out of 4,499 monitoring periods, 1,163 (26%) took place in summer, 1,092 (24%) in fall, 1,117 (25%) in winter, and 1,127 (25%) in spring.
Table 1 describes the enrollment characteristics of the study population. Just over half of children were age 5 – 7 years (52%) and male (59%). Two-thirds of the population were considered atopic (66%) and used maintenance medication at some point during the year of follow-up (66%). The population was 40% white, 19% African American, and 36% Hispanic. Only 16% of mothers had less than a high school education, while 29% were college graduates. At the time of enrollment, 10% of respondents reported having a smoker in their home. For four of the five allergens, less than one-third of the population was both sensitized and exposed (Der p 1 26%, Der f 1 29%, Fel d 1 29%, Can f 1 27%). Only 7% of children were both sensitized and exposed to cockroach (Bla g 1).
Table 1.
Characteristics of 1,342 asthmatic children enrolled from Connecticut and Massachusetts, 2006–2009.
| Enrollment Characteristics | (n=1342) No. (%) |
|---|---|
| Age (yrs) | |
| 5 – 7 | 703 (52) |
| 8 – 10 | 639 (48) |
| Sex | |
| Boys | 786 (59) |
| Girls | 556 (41) |
| Atopica | |
| No | 451 (34) |
| Yes | 886 (66) |
| Maintenance medication useb | |
| No | 460 (34) |
| Yes | 882 (66) |
| Race/Ethnicity | |
| White | 538 (40) |
| African American | 260 (19) |
| Hispanic | 477 (36) |
| Mixed, Other | 67 (5) |
| Mother’s education (yrs) | |
| < 12 | 219 (16) |
| 12 – 15 | 729 (55) |
| ≥ 16 | 393 (29) |
| Smoking in the home | |
| No | 1199 (90) |
| Yes | 136 (10) |
| Allergens: Combined exposure sensitization status | |
| Dust mites | |
| Der p 1 (μg/g) | |
| < 0.10 or allergy absent | 964 (74) |
| ≥ 0.10 and allergy present | 345 (26) |
| Der f 1 (μg/g) | |
| < 0.10 or allergy absent | 919 (71) |
| ≥ 0.10 and allergy present | 380 (29) |
| Pets | |
| Fel d 1 (μg/g) | |
| < 0.12 or allergy absent | 934 (71) |
| ≥ 0.12 and allergy present | 376 (29) |
| Can f 1 (μg/g) | |
| < 0.12 or allergy absent | 952 (73) |
| ≥ 0.12 and allergy present | 360 (27) |
| Cockroach | |
| Bla g 1 (U/g) | |
| < 0.60 or allergy absent | 1210 (93) |
| ≥ 0.60 and allergy present | 89 (7) |
General atopy defined as a positive response to any of the panel of allergens tested, or total IgE response above age-adjusted levels.
Use of any maintenance medications during any of the four, month-long, monitoring periods during the year-long study.
The mean daily indoor NO2 level over all observations was 10.6 (SD=9.4) ppb, with interquartile range 4.5 – 12.5 ppb. Table 2 shows the distribution of all indoor NO2 measurements (by quintile) over subject characteristics. White respondents were predominantly in the lower exposure quintiles, while African American and Hispanic families fell in the higher quintiles. Among women who did not complete high school, 7% are in the lowest exposure categories, while 37% are in the highest exposure categories. Among women who completed college, the distribution is reversed. Non-smokers were distributed fairly evenly across exposure quintiles while smokers were more often in the heavily exposed category. Indoor NO2 measurements in the highest concentration quintile are most likely in the winter and least likely in the summer. For allergens Der p 1, Der f 1, Can f 1, and Fel d 1 17% of observations contributed by sensitized and exposed respondents fall into the highest NO2 exposure categories compared with 34% of those contributed by respondents sensitized and exposed to Bla g 1.
Table 2.
Distribution of subject characteristics for quintiles of indoor nitrogen dioxide (NO2).
| Characteristic | Observations (n=4499) No. | NO2 Exposure Quintile (ppb)a
|
||||
|---|---|---|---|---|---|---|
| ≤ 4.02 (n=899) | > 4.02 – 6.02 (n=900) | > 6.02 – 8.88 (n=900) | > 8.88–14.32 (n=900) | > 14.32 (n=900) | ||
| % | % | % | % | % | ||
| Age (yrs) | ||||||
| 5 – 7 | 2345 | 21 | 21 | 20 | 19 | 19 |
| 8 – 10 | 2154 | 18 | 19 | 21 | 21 | 21 |
| Sex | ||||||
| Boys | 2665 | 20 | 21 | 20 | 20 | 19 |
| Girls | 1834 | 20 | 19 | 20 | 20 | 21 |
| Atopic | ||||||
| No | 1490 | 20 | 19 | 18 | 20 | 23 |
| Yes | 2990 | 20 | 20 | 21 | 20 | 19 |
| Race/Ethnicity | ||||||
| White | 1963 | 31 | 26 | 20 | 15 | 8 |
| African American | 817 | 10 | 15 | 20 | 23 | 32 |
| Hispanic | 1490 | 11 | 15 | 21 | 23 | 30 |
| Mixed, Other | 229 | 15 | 18 | 17 | 28 | 22 |
| Mother’s education (yrs) | ||||||
| < 12 | 685 | 7 | 12 | 19 | 25 | 37 |
| 12 – 15 | 2363 | 16 | 18 | 21 | 22 | 23 |
| ≥ 16 | 1448 | 33 | 27 | 19 | 14 | 7 |
| Smoking in the home | ||||||
| No | 4114 | 21 | 20 | 20 | 20 | 19 |
| Yes | 365 | 7 | 16 | 17 | 23 | 37 |
| Season | ||||||
| Summer | 1163 | 18 | 21 | 24 | 23 | 14 |
| Fall | 1092 | 25 | 20 | 17 | 18 | 20 |
| Winter | 1117 | 20 | 18 | 19 | 19 | 24 |
| Spring | 1127 | 17 | 21 | 20 | 20 | 22 |
| Allergens: Combined exposure sensitization status | ||||||
| Dust mites | ||||||
| Der p 1 (μg/g) | ||||||
| < 0.10 or allergy absent | 3206 | 20 | 19 | 20 | 20 | 21 |
| ≥ 0.10 and allergy present | 1177 | 20 | 22 | 21 | 20 | 17 |
| Der f 1 (μg/g) | ||||||
| < 0.10 or allergy absent | 3055 | 18 | 20 | 20 | 19 | 23 |
| ≥ 0.10 and allergy present | 1291 | 23 | 20 | 21 | 21 | 15 |
| Pets | ||||||
| Fel d 1 (μg/g) | ||||||
| < 0.12 or allergy absent | 3084 | 18 | 20 | 20 | 20 | 22 |
| ≥ 0.12 and allergy present | 1299 | 22 | 20 | 20 | 21 | 17 |
| Can f 1 (μg/g) | ||||||
| < 0.12 or allergy absent | 3133 | 19 | 19 | 20 | 20 | 22 |
| ≥ 0.12 and allergy present | 1256 | 22 | 22 | 21 | 19 | 16 |
| Cockroach | ||||||
| Bla g 1 (U/g) | ||||||
| < 0.60 or allergy absent | 4063 | 21 | 20 | 20 | 20 | 19 |
| ≥ 0.60 and allergy present | 279 | 7 | 15 | 20 | 24 | 34 |
Four, month-long integrated NO2 samples were collected in each study subject’s home, one sample per season.
Table 3 shows the distribution of asthma severity scores across subject characteristics. The most common level of symptoms was mild persistent (25%), and the least common was mild transient (10%). Atopic children were slightly less likely to be categorized as having no symptoms or medications during a monitoring period than non-atopic participants, but were no more likely to be categorized as severe. There were minor differences by ethnicity. Asthma severity scores were generally lower in the summer months and higher in the fall. Children who were both sensitized and exposed to Der p 1, Der f 1, Fel d 1, and Can f 1 were less likely to be in the severity score category 0 than non-sensitized or unexposed children.
Table 3.
Distribution of subject characteristics by asthma severity score.
| Characteristic | Observations (n=4499) No. | Asthma Severity Scorea
|
||||
|---|---|---|---|---|---|---|
| None (n=1087) | Mild Transient (n=431) | Mild Persistent (n=1133) | Moderate Persistent (n=952) | Severe Persistent (n=896) | ||
| % | % | % | % | % | ||
| Age (yrs) | ||||||
| 5 – 7 | 2345 | 26 | 9 | 23 | 21 | 21 |
| 8 – 10 | 2154 | 22 | 11 | 28 | 21 | 18 |
| Sex | ||||||
| Boys | 2665 | 25 | 9 | 24 | 22 | 20 |
| Girls | 1834 | 23 | 10 | 27 | 20 | 20 |
| Atopic | ||||||
| No | 1490 | 28 | 9 | 24 | 19 | 20 |
| Yes | 2990 | 22 | 10 | 26 | 22 | 20 |
| Race/Ethnicity | ||||||
| White | 1963 | 23 | 8 | 26 | 24 | 19 |
| African American | 817 | 25 | 13 | 25 | 19 | 18 |
| Hispanic | 1490 | 26 | 10 | 23 | 19 | 22 |
| Mixed, Other | 229 | 17 | 5 | 28 | 25 | 25 |
| Mother’s education (yrs) | ||||||
| < 12 | 685 | 24 | 11 | 23 | 19 | 23 |
| 12 – 15 | 2363 | 25 | 10 | 25 | 20 | 20 |
| ≥ 16 | 1448 | 22 | 8 | 27 | 25 | 18 |
| Smoking in the home | ||||||
| No | 4114 | 24 | 10 | 25 | 21 | 20 |
| Yes | 365 | 22 | 13 | 28 | 20 | 17 |
| Season | ||||||
| Summer | 1163 | 31 | 10 | 27 | 18 | 14 |
| Fall | 1092 | 21 | 9 | 23 | 23 | 24 |
| Winter | 1117 | 22 | 9 | 26 | 22 | 21 |
| Spring | 1127 | 22 | 11 | 25 | 21 | 21 |
| Allergens: Combined exposure sensitization status | ||||||
| Dust mites | ||||||
| Der p 1 (μg/g) | ||||||
| < 0.10 or allergy absent | 3206 | 26 | 9 | 25 | 20 | 20 |
| ≥ 0.10 and allergy present | 1177 | 20 | 10 | 25 | 25 | 20 |
| Der f 1 (μg/g) | ||||||
| < 0.10 or allergy absent | 3055 | 26 | 9 | 24 | 21 | 20 |
| ≥ 0.10 and allergy present | 1291 | 20 | 10 | 28 | 23 | 19 |
| Pets | ||||||
| Fel d 1 (μg/g) | ||||||
| < 0.12 or allergy absent | 3084 | 27 | 9 | 24 | 20 | 20 |
| ≥ 0.12 and allergy present | 1299 | 19 | 10 | 27 | 24 | 20 |
| Can f 1 (μg/g) | ||||||
| < 0.12 or allergy absent | 3133 | 26 | 9 | 25 | 20 | 20 |
| ≥ 0.12 and allergy present | 1256 | 19 | 10 | 27 | 25 | 19 |
| Cockroach | ||||||
| Bla g 1 (U/g) | ||||||
| < 0.60 or allergy absent | 4063 | 25 | 9 | 25 | 21 | 20 |
| ≥ 0.60 and allergy present | 279 | 24 | 13 | 26 | 15 | 22 |
Health data (asthma severity score based on symptoms and medication use) were collected during four, month-long monitoring periods, one per season.
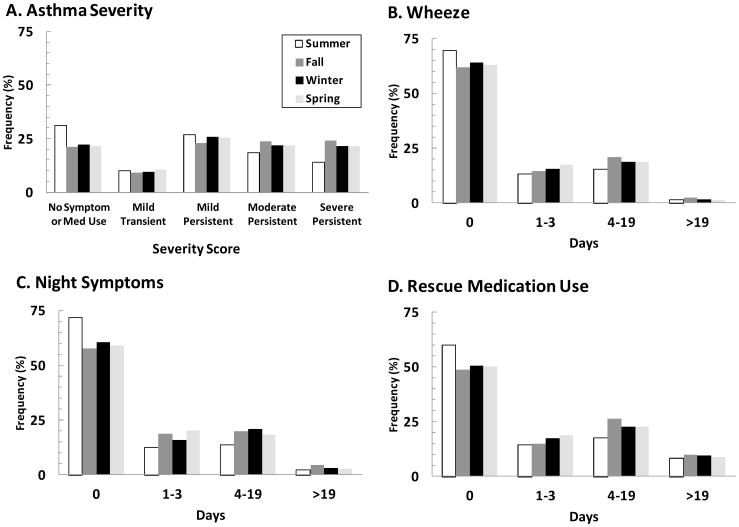
Figure 1 displays the seasonal distributions of health outcomes. A comparison of Figure 1A with Figures 1B, 1C and 1D reveals a flat distribution of scores across asthma severity categories compared with the skewed distributions for categorized days of wheeze and night symptoms and somewhat less skewed distribution for rescue medication use. In general, summer is the season with lowest asthma severity (for all outcomes).
Figure 1.
Distribution of health outcomes: observations by season of monitoring for asthma severity score (A), days of wheeze (B), night symptoms (C) and rescue medication use (D).
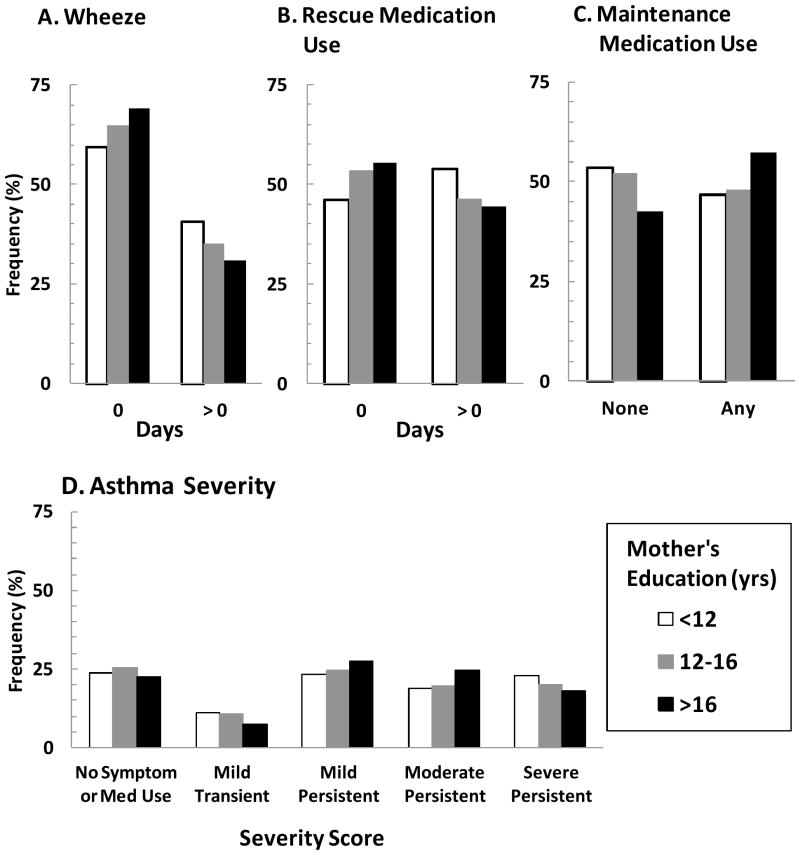
Figure 2 shows distributions of asthma severity score, wheeze and both rescue and maintenance medication use stratified by mother’s education. The distributions for wheeze (Fig. 2A) and rescue medications (Fig. 2B) are similar: subjects whose mother did not complete high school were more likely to report wheeze (41%) and rescue medication use (54%) compared with children of mothers who completed high school (wheeze 35%, rescue medication use 46%) or college (wheeze 31%, rescue medication 45%). However, children of mothers who completed college were more likely (58%) to report use of maintenance medication compared with children of mothers who did not complete high school (46%) or college (47%) (Fig. 2C). Figure 2D shows that the asthma severity score, which incorporates both symptoms and medication use, is not associated with mother’s education. Due to collinearity between maintenance medication and all socioeconomic variables, models for wheeze, night symptoms and rescue medication included maintenance medication use (an important indicator of disease status), but did not include race/ethnicity, mother’s education, or smoking in the home.
Figure 2.
Distribution of any wheeze (A), rescue medication use (B), maintenance medication use (C) and asthma severity score (D): observations for all monitoring periods by mother’s education level.
The proportional odds assumption was satisfied for all outcomes in unadjusted models using quintiles of NO2 exposure. Table 4 presents the results of Bayesian cumulative logistic regression models of associations between health outcomes and NO2 exposure. In unadjusted models, compared with the lowest quintile of exposure (Table 4, unadjusted Model 1), the odds ratios for severity score imply a protective effect for exposure to NO2 levels in the second two quintiles and an increased risk for exposure in the higher quintiles. A similar pattern is seen for night symptoms and rescue medication use and suggests a threshold for health effect. Unadjusted models using the combined lowest two quintiles as the reference group are shown in Table 4, unadjusted Model 2.
Table 4.
Results from ordered logistic regression modelsa of unadjusted and adjusted associations between exposure to indoor NO2 (nitrogen dioxide) and risk of increased asthma severity (asthma severity score, wheeze, night symptoms and rescue medication use).
| NO2 exposure ppbc | Health outcomesb
|
|||||||
|---|---|---|---|---|---|---|---|---|
| Asthma Severity Score | Wheeze | Night Symptoms | Rescue Medication Use | |||||
|
|
|
|
||||||
| OR | (95% CI) | OR | (95% CI) | OR | (95% CI) | OR | (95% CI) | |
| Unadjusted | ||||||||
| Model 1 | ||||||||
| 0 – ≤ 4.00d | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| 4.00 – ≤ 6.02 | 0.83 | (0.67 – 1.03) | 1.05 | (0.81 – 1.36) | 0.89 | (0.71 – 1.12) | 0.92 | (0.73 – 1.16) |
| 6.02 – ≤ 8.88 | 0.89 | (0.70 – 1.12) | 1.08 | (0.81 – 1.43) | 1.08 | (0.84 – 1.37) | 1.09 | (0.85 – 1.40) |
| 8.88 – ≤ 14.30 | 1.04 | (0.81 – 1.34) | 1.31 | (0.98 – 1.75) | 1.20 | (0.94 – 1.54) | 1.21 | (0.94 – 1.59) |
| > 14.30 | 1.21 | (0.92 – 1.59) | 1.38 | (1.02 – 1.87) | 1.40 | (1.09 – 1.81) | 1.53 | (1.16 – 2.02) |
| Model 2 | ||||||||
| 0 – ≤ 6.02d | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| 6.02 – ≤ 8.88 | 1.00 | (0.82 – 1.21) | 1.04 | (0.83 – 1.31) | 1.15 | (0.94 – 1.41) | 1.17 | (0.93 – 1.42) |
| 8.88 – ≤ 14.30 | 1.16 | (0.94 – 1.44) | 1.27 | (1.00 – 1.63) | 1.28 | (1.03 – 1.59) | 1.27 | (1.02 – 1.61) |
| > 14.30 | 1.34 | (1.06 – 1.71) | 1.34 | (1.03 – 1.73) | 1.49 | (1.18 – 1.87) | 1.61 | (1.25 – 2.06) |
| Adjustede | ||||||||
| ≤ 6.02 d | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| 6.02 – ≤ 8.88 | 1.15 | (0.94 – 1.42) | 1.15 | (0.90 – 1.45) | 1.36 | (1.09 – 1.68) | 1.29 | (1.04 – 1.60) |
| 8.88 – ≤ 14.30 | 1.31 | (1.04 – 1.66) | 1.44 | (1.11 – 1.86) | 1.41 | (1.12 – 1.78) | 1.43 | (1.12 – 1.81) |
| > 14.30 | 1.43 | (1.08 – 1.88) | 1.53 | (1.16 – 2.02) | 1.59 | (1.24 – 2.01) | 1.74 | (1.34 – 2.26) |
| Threshold modelf | 1.37 | (1.01 – 1.89) | 1.49 | (1.09 – 2.03) | 1.52 | (1.16 – 2.00) | 1.78 | (1.33 – 2.38) |
To allow for repeated health outcome measures from each monitoring period, hierarchical mixed models with a random term for subject were used.
Asthma severity score has 5 levels: 0 (no symptoms, no medication use), 1 (mild transient), 2 (mild persistent), 3 (moderate persistent), 4 (severe persistent). Health outcomes wheeze, night symptoms, and rescue medication use have 4 levels: 0 (no days of symptoms/medication use), 1 (1 – 3 days), 2 (4 – 19 days), 3 (> 19 days).
Exposure to quintiles of NO2 (ppb) were compared to the lowest quintile (for unadjusted Model 1) or threshold value (≤ 6.02 ppb, combined first and second quintiles, for unadjusted Model 2 and adjusted model). Separate models were run for each health outcome.
Reference category.
Model for asthma severity score adjusted for: age, sex, general atopy, season, specific sensitization and exposure to five indoor allergens (Der p 1, Der f 1, Fel d 1, Can f 1, Bla g 1), race/ethnicity, mother’s education, smoking in the home. Models for wheeze, night symptoms and rescue medication use were adjusted for: age, sex, general atopy, season, specific sensitization and exposure to five indoor allergens (Der p 1, Der f 1, Fel d 1, Can f 1, Bla g 1), maintenance medication use. Because of colinearity with maintenance medication use, socioeconomic status variables (race/ethnicity, mother’s education, smoking in the home) were not included for these three outcomes.
Linear trend of exposure-response relationship with the exposure as a continuous variable representing ln NO2 values greater than the threshold (6.02 ppb). Odds ratios given as a 1.6 increase ln NO2 concentration (5-fold increase in NO2).
OR indicates odds ratio; CI, confidence interval.
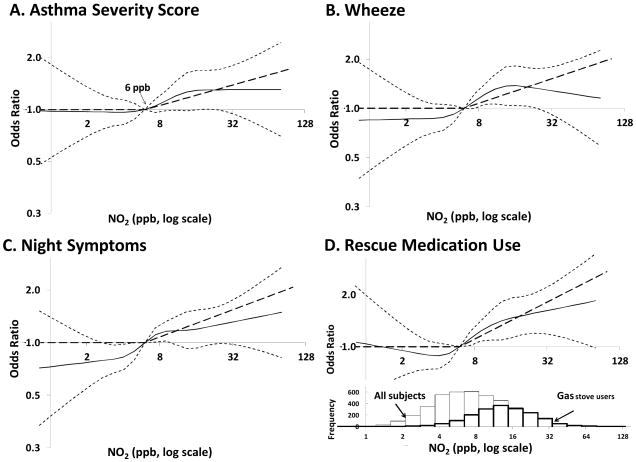
Figure 3 illustrates, for fully adjusted models, the exposure-response relationships between NO2 and health outcomes using a constrained, natural spline function of ln NO2 and 95% confidence limits, as well as threshold functions for each outcome. In adjusted models of NO2 exposure as quintiles (Table 4), levels greater than 14.3 ppb compared with the reference level (≤ 6 ppb, the threshold value) resulted in an increased risk of a one-level increase in asthma severity score (OR= 1.43 [95% CI= 1.08 – 1.88]). These same exposures were also associated with increased risks of wheeze (1.53 [1.16 – 2.02]), night symptoms (1.59 [1.24 – 2.01]) and rescue medication use (1.74 [1.34 – 2.26]). In the fully adjusted threshold models, every 5-ppb increase in NO2 exposure above 6 ppb was associated with a dose-dependent increase in asthma severity score (1.37 [1.01 – 1.89]) as well as asthma morbidity measured by wheeze (1.49 [1.09 – 2.03]), night symptoms (1.52 [1.16 – 2.00]) and rescue medication use (1.78 [1.33 – 2.38]).
Figure 3.
Exposure-response relationships between health outcome and NO2 (log concentration as a continuous variable) illustrated with constrained, natural spline functions (solid lines) with 95% confidence limits (small dashed lines) and threshold function (bold dashed line) from fully adjusted, hierarchical ordered logistic regression models for asthma severity score (A), wheeze (B), night symptoms (C), and rescue medication use (D). Also shown is a histogram of NO2 levels measured in subjects’ homes (panel D) for all observations (thin border) and observations taken in homes of gas stove users (bold border).
Discussion
In this study of school-aged children we observed an association of increasing NO2 concentration in the home with asthma severity assessed by a 5-level score, as well as with asthma morbidity measured by days of wheeze, night symptoms and rescue medication use. Analyses were based on repeated measures of both NO2 and asthma outcomes controlling for atopic status and common household allergen exposures.
These associations are consistent with findings in the literature suggesting an association between NO2 exposure at both relatively low and high levels, and increased asthma severity and morbidity.4,7,9–11,19 The mean indoor NO2 level over all 4,499 observations was 10.6 (SD=9.4) ppb and was 15.6 (10.4) ppb among observations from homes with gas stoves. Figure 3D (rescue medication use) displays a histogram of NO2 levels measured in all subjects’ homes as well as in homes with gas stoves. In our previous study, the mean indoor NO2 for all observations was 14.5 (SD=15.2) ppb and was 25.8 (SD=18.1) ppb in homes with gas stoves.
Figure 1 in that publication7 describes the distribution of NO2 with respect to both stove type and housing type. The lower NO2 levels in our current study reflects the expanded use of high-efficiency gas appliances, which can reduce residential gas usage by up to 30 percent.20 Differences among studies in NO2 distributions also can be attributed to variations in recruitment strategies. We enrolled both urban and suburban children residing in homes with either electric or gas stoves, and found a wide distribution of household NO2 exposures.
In our previous study of children with asthma,7 indoor NO2 was associated with respiratory symptoms but only among children in multifamily housing (an indicator of lower socioeconomic status). To compare the two studies, we explored associations between housing type and respiratory symptoms in the current study and found that children living in multifamily housing were 75% more likely to wheeze, 68% more likely to have night symptoms, and twice as likely to use rescue medication (data not shown). However, we did not find a differential effect of housing type on the asthma severity score.
An important confounder of the association of indoor NO2 exposure with asthma morbidity is socioeconomic status. Higher NO2 concentrations were found in homes of minority children and children whose mothers reported the fewest years of education (Table 2). These children also reported less use of maintenance medication (Fig. 2). Three of our four outcome measures (frequency of wheeze, night symptoms and rescue medication use) represent only part of a child’s disease status. For example, a child reporting no wheeze who is not also taking controller medication will have less severe asthma than a child with no wheeze who is taking maintenance medication. In order to control for this aspect of disease severity (which is not included in the outcome measure), we included maintenance medication use as a covariate in models exploring associations between symptoms and NO2 exposure. Because use of maintenance medication is also associated with socioeconomic status, we did not include additional socioeconomic-status variables in the adjusted models for these outcomes. When these additional variables are added, the odds ratios for the association with NO2 exposure are attenuated and the confidence intervals widen (for wheeze, OR= 1.03 [95% CI= 0.75 – 1.42]; night symptoms 1.16 [0.87 – 1.54]; and rescue medication use 1.24 [0.91 – 1.68]).
A strength of our study is that one of our outcome measures, the asthma severity score, incorporates both symptom frequency and medication use. The asthma severity score is not associated with the socioeconomic status variables (Table 3) included as covariates in adjusted models.
In the Inner City Asthma Study10 among non-atopic children, those with high NO2 exposure were more likely to have more than four symptom days in a two-week period, and more likely to have peak flow values < 80% of predicted values. That study found no association between NO2 exposure and symptoms or peak flow among atopic children. In our study, atopic children were no less likely to experience an increased risk of asthma morbidity associated with increased NO2 than their non-atopic counterparts. This finding is in agreement with the Baltimore Indoor Environment Study of Asthma in Kids,9 whichfound that atopy did not modify the association between NO2 and asthma symptoms.
Strengths of the current study include large sample size, seasonal repeated measurements of NO2 concurrent with measurements of asthma symptoms and medication use and an asthma severity score not associated with socioeconomic variables. Associations between NO2 and asthma were consistent across all outcome measures. Allergy testing and household-allergen sampling at the time of enrollment permitted inclusion of additional important household asthma triggers.14 In addition, the hierarchical analysis permitted estimates of associations between, rather than within, subjects, across homes with different levels of exposure.
The focus of our analysis was on the health effects of indoor exposure to NO2 measured with passive monitors placed in a child’s home where they spend the major portion of their time. One limitation of the passive monitoring method is that it results in an integrated average NO2 concentration and does not allow for measurement of peak exposures. Sources of NO2 were not part of the statistical model, and in homes without indoor sources (such as gas appliances), the only source of NO2 would be outside the residence. The current study included passive monitors placed outside of the residence.21 It remains for future analyses to model the complex relationship between outdoor and indoor levels of NO2 and health effects. For example, when outdoor levels are added as a variable to the adjusted, threshold model for asthma severity score (bottom of Table 4), the odds ratio for indoor NO2 exposure became 1.21 (0.88 – 1.67) and 1.31 (0.95 – 1.83) for outdoor NO2 exposure. One could argue that indoor levels of NO2 already account for a child’s home exposure to outdoor NO2 and adding NO2 concentrations measured outside of a residence results in overcontrolling for indoor levels. An alternative model might be one that adds only “residual” amounts above what is measured indoors. In this alternative model, where only “extra” NO2 not accounted for in the indoor measurement is added, the odds ratio for indoor NO2 exposure on the asthma severity score is 1.52 (1.06 – 2.18), and the odds ratio for outdoor NO2 exposures is 1.20 (0.98 – 1.46). The child’s exposure away from home was not assessed either through personal monitoring or by taking measurements in other environments such as school. We would not expect children to be exposed to sources of NO2 (e.g. gas stoves, unvented gas heaters) in schools or other non-residential environments in our study area. Other limitations include the lack of biological measures of asthma (e.g., peak flow or spirometric measures) and lack of control for viral respiratory illness (another known trigger of asthma exacerbations with possible potentiating effects on NO2 exposure in asthmatic children8).
Our results contribute to a growing body of literature associating low levels of NO2 exposure with adverse respiratory outcomes in asthmatic children. Further, the apparent threshold for these effects in asthmatic children (6 ppb indoors) was comparable to the 10th percentile of mean levels measured outdoors22 – far below the US EPA 53 ppb standard – and with increasing risk of adverse respiratory morbidity above that level.
Acknowledgments
Source of Funding: This work was funded by the NIH National Institutes of Environmental Health Sciences grant ES05410 (Brian P. Leaderer, PI; brian.leaderer@yale.edu).
We gratefully acknowledge Rashele Yarborough and the staff of the Center for Perinatal, Pediatric and Environmental Epidemiology for their contributions to the collection and analysis of study data.
Footnotes
Conflicts of Interest: The authors have no conflicts of interest.
Contributor Information
Kathleen Belanger, Email: kathleen.belanger@yale.edu, Center for Perinatal, Pediatric and Environmental Epidemiology, Yale University School of Public Health, New Haven, CT.
Theodore R. Holford, Email: theodore.holford@yale.edu, Yale University School of Public Health, New Haven, CT
Janneane F. Gent, Email: janneane.gent@yale.edu, Center for Perinatal, Pediatric and Environmental Epidemiology, Yale University School of Public Health, New Haven, CT
Melissa E. Hill, Email: melissa.hill@yale.edu, Center for Perinatal, Pediatric and Environmental Epidemiology, Yale University School of Public Health, New Haven, CT
Julie M. Kezik, Email: julie.kezik@yale.edu, Center for Perinatal, Pediatric and Environmental Epidemiology, Yale University School of Public Health, New Haven, CT
Brian P. Leaderer, Email: brian.leaderer@yale.edu, Center for Perinatal, Pediatric and Environmental Epidemiology, Yale University School of Public Health, New Haven, CT
References
- 1.Utell M, Frampton MW. Oxides of nitrogen. In: Roth RA, editor. Comprehensive Toxicology: Oxides of Nitrogen. Cambridge, UK: Cambridge University Press; 1997. pp. 303–312. [Google Scholar]
- 2.Samet JM, Utell MJ. The risk of nitrogen dioxide: what have we learned from epidemiological and clinical studies? Toxicol Ind Health. 1990;6:247–262. [PubMed] [Google Scholar]
- 3.US Department of Housing and Urban Development and US Census Bureau. [Accessed on 4/1/2011];American Housing Survey for the United States. 2009 http://www.census.gov/prod/2011pubs/h150-09.pdf.
- 4.Pilotto LS, Nitschke M, Smith BJ, Pisaniello D, Ruffin RE, McElroy HJ, Martin J, Hiller JE. Randomized controlled trial of unflued gas heater replacement on respiratory health of asthmatic schoolchildren. Int J Epidemiol. 2004;33:208–14. doi: 10.1093/ije/dyh018. [DOI] [PubMed] [Google Scholar]
- 5.Breysse PN, Diette GB, Matsui EC, Butz AM, Hansel NN, McCormack MC. Indoor air pollution and asthma in children. Proc Am Thorac Soc. 2010;7:102–106. doi: 10.1513/pats.200908-083RM. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sharma HP, Hansel NN, Matsui EC, Diette GB, Eggleston P, Breysse PN. Indoor environmental influences on children’s asthma. Pediatr Clin North Am. 2007;54:103–120. doi: 10.1016/j.pcl.2006.11.007. [DOI] [PubMed] [Google Scholar]
- 7.Belanger K, Gent JF, Triche EW, Bracken MB, Leaderer BP. Association of indoor nitrogen dioxide exposure with respiratory symptoms in children with asthma. Am J Respir Crit Care Med. 2006;173:297–303. doi: 10.1164/rccm.200408-1123OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chauhan AJ, Inskip HM, Linaker CH, Smith S, Schreiber J, Johnston SL, Holgate ST. Personal exposure to nitrogen dioxide (NO2) and the severity of virus-induced asthma in children. Lancet. 2003;361:1939–44. doi: 10.1016/S0140-6736(03)13582-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hansel NN, Breysse PN, McCormack MC, Matsui EC, Curtin-Brosnan J, Williams DL, Moore JL, Cuhran JL, Diette GB. A longitudinal study of indoor nitrogen dioxide levels and respiratory symptoms in inner-city children with asthma. Environ Health Perspect. 2008;116:1428–32. doi: 10.1289/ehp.11349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kattan M, Gergen PJ, Eggleston P, Visness CM, Mitchell HE. Health effects of indoor nitrogen dioxide and passive smoking on urban asthmatic children. J Allergy Clin Immunol. 2007;120:618–24. doi: 10.1016/j.jaci.2007.05.014. [DOI] [PubMed] [Google Scholar]
- 11.Gillespie-Bennett J, Pierse N, Wickens K, Crane J, Howden-Chapman P. The respiratory health effects of nitrogen dioxide in children with asthma. Eur Respir J. 2011;38:303–309. doi: 10.1183/09031936.00115409. [DOI] [PubMed] [Google Scholar]
- 12.Palmes ED, Gunnison AF, DiMattio J, Tomczyk C. Personal sampler for nitrogen dioxide. Am Ind Hyg Assoc J. 1976;37:570–7. doi: 10.1080/0002889768507522. [DOI] [PubMed] [Google Scholar]
- 13.Gent JF, Belanger K, Triche EW, Bracken MB, Beckett WS, Leaderer BP. Association of pediatric asthma severity with exposure to common household dust allergens. Environ Res. 2009;109:768–774. doi: 10.1016/j.envres.2009.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gent JF, Kezik JM, Hill ME, Tsai E, Li D-W, Leaderer BP. Household mold and dust allergens: Exposure, sensitization, and childhood asthma morbidity. Environ Res. 2012 doi: 10.1016/j.envres.2012.07.005. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mayo Clinic. [Accessed on 4/5/2011];Immunoglobulin E (IgE), Serum. 2006 http://mayomedicallaboratories.com/test-catalog/pring.pht?unit_code=8159.
- 16.US Department of Health and Human Services. [Accessed on 1/1/2011];Global Initiative for Asthma: Global Strategy for Asthma Management and Prevention. 2002 http://www.ginasthma.org/Guidelines/guidelines-2002-original%3a-workshop-report%2c-global-strategy-for-asthma-management-and-prevention.html.
- 17.MRC Biostatistics Unit. [Accessed on 06/08/11];The BUGS Project. http://www.mrc-bsu.cam.ac.uk/bugs.
- 18.Durrleman S, Simon R. Flexible regression models with cubic splines. Stat Med. 1989;8:551–61. doi: 10.1002/sim.4780080504. [DOI] [PubMed] [Google Scholar]
- 19.Nitschke M, Pilotto LS, Attewell RG, Smith BJ, Pisaniello D, Martin J. A cohort study of indoor nitrogen dioxide and house dust mite exposure in asthmatic children. J Occup Environ Med. 2006;48:462–469. doi: 10.1097/01.jom.0000215802.43229.62. [DOI] [PubMed] [Google Scholar]
- 20.The American Gas Association. [Accessed on 7/15/2012];2012 http://www.aga.org/our-issues/energyefficiency/Pages/NaturalGasUtilitiesandTheirCustomers.aspx.
- 21.Skene KJ, Gent JF, McKay LA, Belanger K, Leaderer BP, Holford TR. Modeling effects of traffic and landscape characteristics on ambient nitrogen dioxide levels in Connecticut. Atmos Environ. 2010;44:5156–5164. doi: 10.1016/j.atmosenv.2010.08.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.US EPA. [Accessed on 4/1/2011];Air Trends. 2009 http://www.epa.gov.airtrends/nitrogen.html.