Abstract
Health care spending has risen steadily in most countries, becoming a concern for decision-makers worldwide. Commentators often point to new medical technology as the key driver for burgeoning expenditures. This paper critically appraises this conjecture, based on an analysis of the existing literature, with the aim of offering a more detailed and considered analysis of this relationship. Several databases were searched to identify relevant literature. Various categories of studies (eg, multivariate and cost-effectiveness analyses) were included to cover different perspectives, methodological approaches, and issues regarding the link between medical technology and costs. Selected articles were reviewed and relevant information was extracted into a standardized template and analyzed for key cross-cutting themes, ie, impact of technology on costs, factors influencing this relationship, and methodological challenges in measuring such linkages. A total of 86 studies were reviewed. The analysis suggests that the relationship between medical technology and spending is complex and often conflicting. Findings were frequently contingent on varying factors, such as the availability of other interventions, patient population, and the methodological approach employed. Moreover, the impact of technology on costs differed across technologies, in that some (eg, cancer drugs, invasive medical devices) had significant financial implications, while others were cost-neutral or cost-saving. In light of these issues, we argue that decision-makers and other commentators should extend their focus beyond costs solely to include consideration of whether medical technology results in better value in health care and broader socioeconomic benefits.
Keywords: medical technology, health expenditure, health policy, costs
Introduction
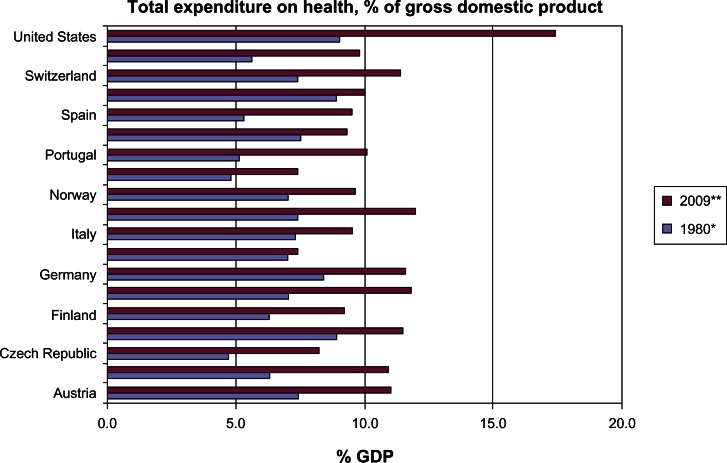
Health care spending has risen at rates greater than gross domestic product in most OECD countries. In 2009, average health spending reached 9.5% of gross domestic product, up from 8.8% in 20081 (Figure 1). During the same time period, average per capita spending increased by an average of 3.8% in 2008 and 3.5% in 2009, with public spending on health growing at an even faster rate of 4.8% and 4.1%, respectively.1 For most countries, rising health expenditure is considered an enduring challenge and one that requires a complex balancing act between cost control, affordable and equitable access to beneficial treatments, and support for innovation.
Figure 1.
Total expenditure on health as a percentage of gross domestic product (GDP) (1980–2009).
Notes: *All data from 1980 except for Czech Republic (1990), Hungary (1991), Italy (1998), Poland (1990), and Slovenia (1995); **all data from 2009, except for Portugal (2008).
OECD Health Data 2011.1
A number of factors have been identified as contributors to spending growth, including the ageing of populations, increased public demand and expectations, personal income growth, rising prices of physician and hospital services (eg, labor costs), and inefficiencies in the organization and payment of care. For example, the growth in life expectancy has had an obvious yet gradual impact on the demand for health care. Although the use of care depends ultimately on the health status of a person and not necessarily on their age cohort(s), elderly people use health care more often and more intensively than younger populations, with a high proportion of costs garnered at the end of life.2 Longer life spans, in concert with an increase in unhealthy lifestyles, have also contributed to an increased prevalence of disease, particularly chronic conditions such as obesity, diabetes, and cancer. Greater prevalence of chronic conditions are likely to increase spending both through an increase in treated prevalence (ie, number of cases treated) and the cost of treatment (ie, spending per case).
However, analysts often point to advances in medical technology and their diffusion across health systems as the principal driver for burgeoning expenditures.3–10 This paper critically examines this conjecture, based on an analysis of a broad range of existing evidence on the relationship between medical technology diffusion and health expenditure. We strive to focus on medical devices, given the gap in the literature on their role in health expenditures, which has predominantly centered on pharmaceuticals, and because the sector has grown considerably in recent years. Not only are there substantially more medical technologies on the market, but they have grown increasingly sophisticated.
The paper is structured as follows. We first outline the methods used to review the literature, followed by a summary of the available evidence. The paper then discusses the complexities inherent to ascertaining the impact of technology on spending, including some of the methodological challenges associated with demonstrating and quantifying this link. Based on the analysis, we close by arguing that while the impact of medical technology on rising costs is an important concern and area of inquiry, attention should also be focused on exploring whether investments in medical technology result in better value, as measured by therapeutic benefit, cost-effectiveness, and other important outcomes (eg, quality of life, improved productivity) in health care, and under which conditions technologies allow for the most effective and efficient use of available health care resources. We offer some general suggestions for what might be done to support this end.
Materials and methods
A literature review was conducted to explore the current evidence base on the relationship between medical technology and health care expenditures. Unlike previous studies in this area, we considered a wide range of literature to ensure adequate coverage of different methodological approaches and ideological perspectives for assessing this relationship. The categories of literature included in the search and review included general and descriptive analyses, policy analyses, literature reviews, multivariate analyses, cost-effectiveness analyses, and cost impact studies of specific technologies. Table 1 presents and describes the various study types included in the review.
Table 1.
Types of studies included in the review
| Study type | Definition |
|---|---|
| General and descriptive analyses | Generally provide an in depth analysis of the main variables or factors affecting health expenditures. Some of these studies take a broad approach examining a range of variables, while others focus on a particular issue, such as medical technology, on spending. Furthermore, studies vary in whether they examine national-level expenditures or take a narrower approach by assessing hospital spending. Most of these studies are qualitative. |
| Policy analyses | Evaluate the impact of different policy interventions (eg, managed care, changes to hospital organization or services) and their impact on health expenditures, as well as on mediating factors, such as technology diffusion. Other policy studies consider the implications of high expenditures associated with a particular cost driver (eg, aging, technological advancement). Analyses can be either qualitative or quantitative in nature. |
| Literature reviews | Assess the current literature on the impact of a particular factor or a broad array of factors on health expenditures. This category includes systematic reviews and general literature reviews. |
| Econometric analyses | Typically entails multivariate studies, which examine multiple variables and their effects (and interrelationships) on health expenditures. These studies employ three methodological approaches most frequently, including the “residual” approach, the “proxy” approach, and case studies of specific technologies. The residual approach measures the impact of certain demographic and economic factors (eg, population aging) known to affect health expenditures and then attributes the unexplained portion of spending growth to medical technology. The proxy approach is an indirect method, which employs a measurable proxy indicator for technological change (eg, spending on research and development, time, patents) to explain health care spending trends. The case study approach examines how a specific technology and the associated changes in clinical practice affect spending on specific types of patients, conditions, or settings. |
| Cost-effectiveness analyses | Assess the cost and clinical benefits of a given technology. Such studies seek to ascertain the value for money of a particular intervention. This approach often entails combining clinical benefit with quality of life in a single generic measure of health gain, the quality-adjusted life year, in a cost-utility analysis. |
| Cost impact studies | Evaluate the impact of specific technologies or policies on costs, either at one point in time or over time. |
Key databases, including PubMed, EMBASE, MEDLINE, and EconLit, were searched to identify relevant literature. The search terms employed to identify relevant literature included “technolog* AND (expenditure OR cost) AND (health OR healthcare)”, and “medical AND technolog* AND (expenditure OR cost)”.
To identify relevant cost-effectiveness analyses across all medical technologies would be a considerable task. Therefore, we took advantage of two previously completed systematic reviews of economic evaluations of medical devices in the cardiology and orthopedic sectors, the two most significant markets for therapeutic devices.11 In these reviews, we used the National Health Service Economic Evaluation Database12 for the searches, which contains structured reviews (abstracts) of full economic evaluations of health care treatments and programs. In these two previously conducted studies, we employed the following search terms “cardiology”, “cardiac rhythm management”, “cardiovascular”, “coronary stents”, “cardiac resychronization”, “implantable cardioverter defibrillators”, “orthopaedic”, “hip”, “knee”, “shoulder”, “ankle”, “elbow”, “arthroplasty”, and “joint”.
All the relevant abstracts were reviewed, from both the general literature review and the review of National Health Service Economic Evaluation Database. Duplicate and irrelevant abstracts were identified and eliminated. Selected articles were reviewed according to a data extraction form, developed in Microsoft Excel, to standardize the review and facilitate subsequent analysis of the collated information. The categories of information extraction included: basic bibliographic information; publication year; literature type (eg, descriptive analysis); study aims; technologies studied; study setting; methods employed; outcomes across health, costs/expenditures, and cost-effectiveness; and, stated conclusions and implications of the study. The information extracted was then analyzed for key themes across the domains interest (ie, impact of medical technology on costs or spending and factors influencing this relationship, and the methodological challenges noted in measuring such linkages).
A total of 86 studies were included in the review (Appendix 1). Table 2 provides a summary of general study details. The majority (52%) of studies were more qualitative in nature (eg, descriptive and policy analyses, literature reviews), followed by cost-effectiveness (40%) and multivariate (24%) analyses. In addition, the bulk of studies were published within the last ten years (77%) and focused on the US (52%). With the exception of cost-effectiveness and cost impact studies examining specific medical devices, most studies (52%) examined medical technology in general, which in some cases included some combination of drugs, devices, diagnostics, or procedures.
Table 2.
Characteristics of the reviewed literature
| Study characteristics | |||
|---|---|---|---|
| Type of study | Number | Year | Number |
|
| |||
| General/descriptive analysis | 12 | 1980–1985 | 1 |
| Policy analysis | 8 | 1986–1990 | 2 |
| Literature review | 4 | 1991–1995 | 5 |
| Multivariate analysis | 21 | 1996–2000 | 12 |
| Cost-effectiveness analysis | 34 | 2001–2005 | 37 |
| Cost impact study | 7 | 2006–2010 | 29 |
| Technology studied | Number | Study setting | Number |
|
| |||
| General health technology | 27 | US | 45 |
| Specific medical devices | 41 | Europe | 21 |
| Specific drugs | 3 | OECD | 5 |
| Combination of specific drugs, devices, and/or services | 7 | Canada | 5 |
| Other* | 8 | Other** | 10 |
Notes:
Articles that focused on cost containment policy effects and general economic trends;
articles that did not focus on any one country, or did not specify.
Results
Although technological innovation is of great significance in health care13,14 and has been claimed to be a key driver of health spending, the review highlighted that research measuring the potential contributions of medical technology to rising health care costs has been relatively sparse. One possible reason for this neglect, and the predominant reliance on more descriptive or qualitative analyses among available studies, is that technology itself and its possible implications on health expenditures are insufficiently understood. Other reasons center on the often limited data available to explore this relationship and the complexities of measuring such associations, which we discuss further below.
The available evidence that does exist suggests that, in general, new medical technology is an important determinant in rising health care expenditures. Of the studies reviewed that attempted to quantify this relationship, mainly econometric studies, the overall impact (ie, proportion of the cost increase) ranges from approximately 25% to 75%, averaging at about 50%7,9,10,14–19 (Table 3).
Table 3.
Contributions of selected factors to growth in health care spending
| Di Matteo15 | Jones16 | Pricewaterhouse Coopers7 | Smith et al19 | Peden and Freeland17 | Cutler9 | Newhouse10 | |
|---|---|---|---|---|---|---|---|
| Life expectancy/aging | ∼9% | * | 15%** | 2% | 6%–7% | 2% | 2% |
| Administrative costs | * | * | 15%*** | 3%–10% | * | 13% | * |
| Changes in financing | * | * | * | 10% | 4%–5% | 10% | 10% |
| Personal income growth | 9%–20% | * | * | 11%–18% | 14%–18% | 5% | <23% |
| Health care prices | * | * | 18% | 11%–22% | * | 19% | * |
| Technology | ∼65% | 50%–75% | 25% | 38%–62% | 70%–75% | 49% | >65% |
Notes:
Not estimated;
included aging, but also “front page treatments” (ie, media coverage drives demand for expensive treatment), increased preventive and diagnostic activity, and consumers moving away from less expensive managed care products;
included government mandates (including new mandated benefits) and federal and state regulatory requirements.
While much of the quantitative evidence indeed substantiated the cost-increasing effect of new technology overall, the broader spectrum of evidence (eg, cost-effectiveness studies, descriptive analyses) suggests that the relationship between technological advances and health care expenditure is not straightforward or static. Rather, it should be understood as being complex, with a wide range of potential intervening factors that change and shift the dynamic of the association, depending on the particular circumstances.
For example, this relationship often differed across technologies, with some exerting more upward pressure on health care expenditure than others. Of 16 diseases (and subgroups) studied by Scitovski20 in a case study, new technology decreased costs in eight cases, increased costs in seven, and in one case had neutral effects. The use of “low-tech” technologies such as electrocardiography, laboratory tests, and x-rays stabilized or increased costs at a moderate pace, while the use of complex or sophisticated technologies and procedures such as cesarean section, new treatment modalities for breast cancer, and coronary bypass surgery substantially increased costs. In another case study, Bryan et al21 found that technology that introduces computer-based information networks for imaging archiving increased annual hospital costs by 1.8%. A Congressional Budget Office6 review of the available economic literature highlighted particular areas of technology advancement that has been accompanied by more spending, including revascularization for coronary artery disease, diagnostic imaging, and joint replacement.
Whether a particular technology increases or decreases costs depends on whether a given technology: substitutes for an existing service; expands the number of treatable conditions, in that it allows providers to treat conditions they previously could not treat or could not treat effectively or aggressively; intensifies level of use of the technology for the same condition; impacts the delivery of care (eg, improves the capacity of the system to treat more patients); broadens the definition of diseases; and extends life, for which each patient bears (or induces) additional years of health care consumption.6,17,22–25
For instance, with regards to increasing the indications and applications of the innovations, the initial use of imaging diagnostics (eg, x-rays, computed tomography, magnetic resonance) was initially targeted to specific organs and functions, but their application has extended to almost every part of the human body, resulting in increased spending.26 Further, some new technologies may allow lower unit costs (ie, treatment becomes cheaper) or cause less discomfort or complications, thereby offering the potential for cost savings. However, these benefits may lead to increased provision of services to persons who, without the new technology, may not have undergone a particular treatment. Therefore, when the cost savings per case are offset by the increased number of procedures, these technologies will result in increased costs in the aggregate, but will almost certainly also increase the total benefits from the care provided. Chernew et al27 found this was the case with regard to introduction of laparoscopic techniques at the beginning of the 1990s in the US. Of course, new technology can also help extend life (in patients with life-threatening or chronic conditions), which may result in higher spending due to extended years of health care utilization. However, in parallel, a given technology may also allow individuals to live those additional years with greater quality of life or in an improved health state, which could bring potential cost-savings and/or broader social benefits.
In contrast, those technologies that have a substitutive effect, thereby reducing treatment with older technology, eg, use of percutaneous transluminal coronary angioplasty (PTCA) and coronary artery bypass grafting (CABG), may facilitate reductions in spending, even if treatment expansion follows.25,26 For example, PTCA outcomes improved through the introduction of coronary stents, leading to reduced occurrence of restenosis, heart attacks, emergency CABG, and mortality. Consequently, the procedures had become highly substitutable with CABG and for patients with severe coronary artery disease. While the growth of PTCA resulted in higher costs, this has been offset over time by the substitution of PTCA for CABG. Therefore, by metrics of costs, the diffusion of some new technologies can increase spending rapidly at first as it treats those who went without, and less rapidly over time as technology substitutes for more expensive existing treatments.28,29
Moreover, the impact of technology on costs varies depending on the circumstances (eg, patient population, placement in treatment pathway) within which a given therapy is used. For example, several cost-effectiveness analyses on drug-eluting stents have demonstrated that use of these devices increased per patient treatment costs compared with standard balloon angioplasty.30–32 However, if used in medium-risk to high-risk patients, drug-eluting stents could be cost-neutral31,32 or even cost-saving.30
There are also organizational, economic, and social considerations that influence the link between new technology and spending and arguably interplay with the aforementioned factors. For example, impacts on costs may be affected by how the technology is administered or impacts the delivery of care, because some innovations may lead to an increased use of medical personnel, material supplies, or training, particularly if they employ a new technique or procedure, while others may reduce staff or time requirements or shift care to less costly settings of care (eg, inpatient to outpatient).33,34 In particular, some technologies may improve the efficiency of care delivery by reducing procedure time, length of stay, or number of hospitalizations, thereby increasing the capacity of the hospital to treat additional patients. Overall costs may rise as a result, but such outlays will likely result in improved health outcomes for a greater number of patients.
Finally, technological advancements may generate consumer demand for care (and, perhaps more intense, costly services, even if not cost-effective), as well as the demand for insurance.17,27,35,36 At the same time, expanding insurance provides increased incentives to develop new technologies.22 Some analysts maintain that such incentives contribute to long-term growth in expenditure, because the development costs of these products must be recouped by industry (leading to higher prices).6 Although much of this evidence originates from the US, Barros and Martinez-Giralt37 also found that payment systems affect the rate of technology adoption and utilization in European systems. National procurement policies and practices may also influence their diffusion into the health system and the costs associated with adoption. For example, use of more centralized purchasing strategies (eg, local or regional procurement consortiums) or value-based purchasing in Europe and elsewhere, where payment is directly linked to the quality and efficiency of a new technology, may reduce spending.38,39
In relation to this point, there are important differences between countries and their respective health systems that influence the adoption and diffusion of new technologies. For instance, technological change often results from incentives in the health care system. Given that incentive structures differ across countries, technology influences spending differently across jurisdictions.40 Lambooij et al41 assert that lower resourced countries encourage diffusion of innovations that enhance efficiency, whereas better resourced jurisdictions encourage diffusion of complex, expensive technologies.
Discussion
The results of our review suggest that medical technology does have a significant role in health care expenditures, albeit a dynamic and complex one. However, there are limitations to the methodological approaches used in the available published literature, which introduce challenges to arriving at a clear assessment of such dynamics. For example, in terms of quantifying this link, the residual approach4,10,17 can yield a reasonable indirect approximation of how medical technology relates to long-term growth in total health expenditure, but it can be sensitive to assumptions regarding the effects of other related factors (eg, personal income, health insurance coverage, technology development) and the dynamics between them.6,18 This frequently leads to an overestimation of the effect of technology on spending. Another common method, ie, the proxy approach,14,15 is only as good as the proxy indicator used to assimilate the impact of technology on spending. The use of time as a proxy measure for technological change, for example, not only captures such changes, but may also encapsulate variations in policy, patient experiences, preference, and expenditures.15
Another method, ie, the case study approach,25,26 is useful to explain the impact of certain medical technologies on health care costs, but there are problems of sampling and it is difficult to generalize to an aggregate or national level.6,19 Consequently, most analysts using this approach have focused on the most significant conditions (eg, prevalent, contributing to high levels of mortality or disability), such as heart disease. These technical issues also characterize cost-effectiveness and cost impact analyses.42–45
In addition to the limitations noted with individual approaches, there are technical issues shared across the various methods. Firstly, the results are frequently based on aggregate level data that are often subject to potential endogeneity and omit variable bias.46 Secondly, as intimated above, several of these methods can depend on relatively simplified models dealing with highly complicated and interrelated parameters16 and can only arrive at conclusions about the collective effect of technology on health care spending, not on the contributions of specific technologies. Different types of technologies (eg, drugs versus medical devices) arguably impact health spending differently, particularly in terms of the associated changes in clinical practice that follow their adoption. For example, a recent study47 estimated that medical devices account for a relatively small share of national health expenditures (3%–5%), which have risen only slightly over the last 20 years, ie, a trend different from that of pharmaceuticals. Thirdly, across both quantitative and qualitative approaches, capturing the economic (and social) complexities surrounding the use of technology can be challenging, because it generally necessitates a complete understanding of the manner and magnitude of change in the clinical management pathway associated with treatment and follow-up. This process can occur over extended periods of time, and can have varying resource costs that can be both easy and difficult to measure.48
Available studies are often focused on a narrow time window and the specific duration of the life cycle for a technology. Therefore, results from studies with longer or different time periods could vary. For instance, the price of medical technologies generally decreases over time, which would not be captured in shorter-term studies or those that happen to examine a given technology(s) close to initial launch. similarly, technological advances occur simultaneously with changes in other factors that affect health care spending, such as personal income and health financing systems, which make it difficult to identify causality reliably, and exactly how technology itself affects spending growth. Finally, current methods cannot effectively demonstrate the cost impact that would result if availability of technology were reduced or eliminated. In the short-term, cost-savings may be achieved, while limited access to technology may result in higher costs in the long term due to the presence of disease that was not adequately treated owing to reliance on older, less-effective technologies or a complete lack of viable treatment alternatives.
Therefore, while examining the role of medical technology in rising health expenditures is indeed an important area of inquiry, it is largely an incomplete exercise, due to some of the noted methodological issues, and also because most new technological innovations are cost-increasing. Even if a given technology increases costs, it may increase benefits by an even greater amount. In addition, the same technology, applied in different settings, or in different groups of patients, could be cost-effective in some instances and not in others. Consequently, alongside simply examining costs, it is perhaps more productive to assess whether the additional benefits resulting from the use of the technology justify any increase in costs and under which circumstances technologies deliver greater value in health care. That is, are the resulting spending levels reflected in more effective, cost-effective, and higher quality health care?
Several studies from the review indicate that, on average, increases in spending as a result of technological advances have provided reasonable value. For example, Cutler et al49 found that from 1960 to 2000, average life expectancy increased by 7 years, 3.5 years of which were attributable to improvements in health care. Comparing the value of a year of life (anywhere from $50,000 to $200,000) with the finding that each year of increased life expectancy cost about $19,900 in health spending, they conclude that the increased spending, on average, had been a worthwhile investment. similar conclusions were arrived at by Cutler and McClellan25 and Skinner et al50 in examining technological innovation in cardiac care. The former, for example, demonstrated that the use of new technology helped to increase the average coronary patient’s life expectancy by one year (valued at $70,000 per case), while treatment costs increased $10,000 per case (4.2% per year), for a net benefit of $60,000 per case. In addition, as previously discussed, cost-effectiveness analyses of particular medical devices demonstrate value for money (as measured by cost per quality-adjusted life year) and in some limited cases, cost savings.30,31,42,51–53 On a broader level, Fuchs and Sox54 surveyed physician perceptions of the importance of and value brought by various areas of technological innovation, with magnetic resonance imaging and computed tomographic scanning, angiotensin-converting enzyme inhibitors, balloon angioplasty, statins, and mammography all rated highly.
Before concluding, it is important to note a few limitations to this study. Firstly, while we strove to select and review only studies focused on medical technology, some studies, particularly certain types of econometric studies, looked at technology collectively. Therefore, for those studies, we were unable to distinguish the relative contribution of different types of technology (eg, drugs versus devices) to the proportion of spending attributed to technological innovation. Secondly, we focused our review of cost-effectiveness studies only on selected cardiology and orthopedic devices. Nevertheless, these particular sectors are arguably important markets and those most likely to have a cost impact.
Conclusion
Major technological advances in medical science have allowed health care providers to diagnose and treat illnesses in ways that were previously impossible. In general, such developments have tended to increase health care spending, which has been seen as an important policy concern, especially considering ever-limited health care budgets.
However, examining the link between medical technology and health expenditures is only one part of the picture. In order to understand better the dynamics between innovation and spending, it is important to assess whether and under what circumstances do investments in medical technology result in better value in health care. As Cutler and McClellan25 assert, “it does not necessarily follow that technology change is therefore bad … costs of technology need to be compared with benefits before welfare statements can be made”. Given the current global economic situation, it is ever more important to ensure that we are attaining good value for money from the technologies developed.
To be sure, the question of whether medical technologies result in added value to the health care system is, of course, also difficult to answer. It depends on our ability to determine the value of output from the health services sector, and placing a value on longer or better quality of life is difficult to appraise. As a starting point, much more comparative research is needed to understand better which technologies work best and are most cost-effective, and under what circumstances. Indeed, as previously discussed, some of the cost-increasing effects of technology arise from inappropriate use, where new treatments are offered to patients for whom there is none to little clinical benefit. Current efforts to support comparative effectiveness research in the US and health technology assessment in Europe and elsewhere may help to foster these aims. However, it is important to note that medical technologies introduce unique technical challenges to health technology assessment or comparative effectiveness research, so assessment methods should adequately account for or be developed to accommodate such aspects.55 Moreover, in addressing questions of value, such research should strive, where possible, to assess a broad range of potential benefits beyond clinical or therapeutic benefit, including value for money, higher quality of care, improved quality of life, greater efficiency in care delivery (eg, reduced length of stay, shifting care from inpatient to outpatient settings), and enhanced ability to work or return to work.
If the evidence generated from such research is to have an impact on health care spending, it should be used to inform policy and practice. As such, comparative effectiveness research and health technology assessment should be used to help reward and support the introduction of technologies into practice that confer therapeutic benefit and reasonable value for money, either through use in coverage and payment policies, insurance benefit design, or practice guidelines. Conversely, use of low-value interventions should be disincentivized through disinvestment or limitation on their use. Such strategies should be coupled with a greater emphasis on evidence-based delivery of care (eg, aligning appropriate financial incentives for providers and consumers), which might further reduce expenditure levels if such incentives support greater use of cost-effective services.6 However, in parallel, it will be important to monitor carefully the impact of such policy levers in order to ascertain the best way to control costs without denying the benefits of new innovation. In addition, such measures need to be coupled with other policies and practices to address some of the other drivers of health spending, including initiatives to support healthy aging and improve coordination of care for the chronically ill. Finally, given our ever-limited health care resources, it would be prudent to debate the opportunity costs of funding new (and increasingly expensive) technologies. Even in cases where medical technologies are cost-effective, available resources may be better allocated to other equally or more cost-effective investments outside of the health care sector, such as the environment or education.
Appendix 1
Studies reviewed
- Aidelsburger P, Grabein K, Klauss V, Wasem J. Cost-effectiveness of cardiac resynchronization therapy in combination with an implantable cardioverter defibrillator (CRT-D) for the treatment of chronic heart failure from a German health care system perspective. Clin Res Cardiol. 2002;97:89–97. doi: 10.1007/s00392-007-0586-9. [DOI] [PubMed] [Google Scholar]
- Baker L, Spetz J. Managed Care and Medical Technology Growth. 1999 National Bureau of Economic Research Working Paper Series, No 6894. Available from: http://www.nber.org/chapters/c9845.pdf. Accessed March 17, 2013. [Google Scholar]
- Baker LC. Managed care and technology adoption in health care: evidence from magnetic resonance imaging. J Health Econ. 2001;20:395–421. doi: 10.1016/s0167-6296(01)00072-8. [DOI] [PubMed] [Google Scholar]
- Baker L, Birnbaum H, Geppert J, Mishol D, Moyneur E. The relationship between technology availability and health care spending. Health Aff (Millwood) 2003;(Suppl Web Exclusives):W3-537–51. doi: 10.1377/hlthaff.w3.537. [DOI] [PubMed] [Google Scholar]
- Bakhai A, Stone GW, Grines CL, et al. Cost-effectiveness of coronary stenting and abciximab for patients with acute myocardial infarction: results from the CADILLAC (Controlled Abciximab and Device Investigation to Lower Late Angioplasty Complications) Trial. Circulation. 2003;108:2857–2863. doi: 10.1161/01.CIR.0000103121.26241.FA. [DOI] [PubMed] [Google Scholar]
- Banz K. Cardiac resynchronization therapy (CRT) in heart failure: a model to assess the economic value of this new medical technology. Value Health. 2005;8:128–139. doi: 10.1111/j.1524-4733.2005.03092.x. [DOI] [PubMed] [Google Scholar]
- Bagust A, Grayson AD, Palmer ND, Perry RA, Walley T. Cost-effectiveness of drug eluting coronary artery stenting in a UK setting: cost-utility study. Heart. 2006;92:68–74. doi: 10.1136/hrt.2004.053850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barros P, Martinez-Giralt X. Technological Adoption in Health Care. CEPR Discussion Papers 7558, CEPR. Discussion Papers; 2009. Available from: http://ideas.repec.org/p/unl/unlfep/wp545.html. Accessed March 17, 2013.
- Bentkover JD, Stewert EJ, Ignaszewski A, Lepage S, Liu P, Cooper J. New technologies and potential cost savings related to morbidity and mortality reduction in Class III/IV heart failure patients in Canada. Int J Cardiol. 2003;88:33–41. doi: 10.1016/s0167-5273(02)00378-9. [DOI] [PubMed] [Google Scholar]
- Bodenheimer T. High and rising health care costs. Part 2: technologic innovation. Ann Intern Med. 2005;142:932–937. doi: 10.7326/0003-4819-142-11-200506070-00012. [DOI] [PubMed] [Google Scholar]
- Bozic KJ, Morshed S, Silverstein MD, Rubash HE, Kahn JG. Use of cost-effectiveness analysis to evaluate new technologies in orthopaedics: the case of alternative bearing surfaces in total hip arthroplasty. J Bone Joint Surg Am. 2006;88:706–714. doi: 10.2106/JBJS.E.00614. [DOI] [PubMed] [Google Scholar]
- Brunner-La Rocca HP, Kaiser C, Berheim A, et al. Cost-effectiveness of drug-eluting stents in patients at high or low risk of major cardiac events in the Basel Stent KostenEffektivitäts Trial (BASKET): an 18-month analysis. Lancet. 2007;370:155–159. doi: 10.1016/S0140-6736(07)61660-2. [DOI] [PubMed] [Google Scholar]
- Bryan S, Buxton M, Brenna E. Estimating the impact of a diffuse technology on the running costs of a hospital. Int J Technol Assess. 2000;16:787–798. doi: 10.1017/s0266462300102065. [DOI] [PubMed] [Google Scholar]
- Busse R. Expenditure on health care in the EU: making projections for the future based on the past. Eur J Health Econ. 2001;2:158–161. [Google Scholar]
- Calvert MJ, Freemantle N, Yao G, et al. Cost-effectiveness of cardiac resynchronization therapy: results from the CARE-HF trial. Eur Heart J. 2005;26:2681–2688. doi: 10.1093/eurheartj/ehi662. [DOI] [PubMed] [Google Scholar]
- Caro J, Ward A, Moller J. Modelling the health benefits and economic implications of implanting dual-chamber vs single-chamber ventricular pacemakers in the UK. Europace. 2006;8:449–455. doi: 10.1093/europace/eul042. [DOI] [PubMed] [Google Scholar]
- Chen L, Hay JW. Cost-effectiveness of primary implanted cardioverter defibrillator for sudden death prevention in congestive heart failure. Cardiovasc Drugs Ther. 2004;18:161–170. doi: 10.1023/B:CARD.0000029034.65769.f7. [DOI] [PubMed] [Google Scholar]
- Chernew M, Hirth RA, Sonnad SS, Ermann R, Fenrick AM. Managed care, medical technology, and health care cost growth: A review of the evidence. Med Care Res Rev. 1998;55:259–288. doi: 10.1177/107755879805500301. [DOI] [PubMed] [Google Scholar]
- Chernew M, Fenrick AM, Hirth RA. Managed care and medical technology: implications for cost growth. Health Aff (Millwood) 1997;16:196–206. doi: 10.1377/hlthaff.16.2.196. [DOI] [PubMed] [Google Scholar]
- Clemente J, Marcuello C, Montanes A, Pueyo F. On the international stability of health care expenditure functions: are government and private functions similar? J Health Econ. 2004;23:589–613. doi: 10.1016/j.jhealeco.2003.08.007. [DOI] [PubMed] [Google Scholar]
- Cohen DJ, Murphy SA, Baim DS, et al. Cost-effectiveness of distal embolic protection for patients undergoing percutaneous intervention of saphenous vein bypass graft (results from the SAFER trial) J Am Coll Cardiol. 2004;44:1801–1808. doi: 10.1016/j.jacc.2004.05.086. [DOI] [PubMed] [Google Scholar]
- Cowie MR, Marshall D, Drummond M. Lifetime cost-effectiveness of prophylactic implantation of a cardioverter defibrillator in patients with reduced left ventricular systolic function: results of Markov modelling in a European population. Europace. 2009;11:716–726. doi: 10.1093/europace/eup068. [DOI] [PubMed] [Google Scholar]
- Cutler DM, Huckman RS. Technological development and medical productivity: the diffusion of angioplasty in New York state. J Health Econ. 2003;22:187–217. doi: 10.1016/S0167-6296(02)00125-X. [DOI] [PubMed] [Google Scholar]
- Cutler DM, McClellan M. Is technological change in medicine worth it? Health Aff (Millwood) 2001;20:11–29. doi: 10.1377/hlthaff.20.5.11. [DOI] [PubMed] [Google Scholar]
- Cutler DM, McClellan M. The Determinants of Technological Change in Heart Attack Treatment. NBER Working Paper No 5751; 1996. Available from: http://ideas.repec.org/p/nbr/nberwo/5751.html. Accessed March 17, 2013.
- Cutler DM. The lifetime costs and benefits of medical technology. J Health Econ. 2007;26:1081–1100. doi: 10.1016/j.jhealeco.2007.09.003. [DOI] [PubMed] [Google Scholar]
- Cutler DM. Technology, Health Costs, and the NIH, Harvard University and the National Bureau of Economic Research. Paper prepared for the National Institutes of Health Economics Roundtable on Biomedical Research; September 1995. [Google Scholar]
- Di Matteo L. What drives provincial health expenditure? Canadian Tax Journal. 2004;52:1102. [Google Scholar]
- Di Matteo L. The macro determinants of health expenditure in the United States and Canada: assessing the impact of income, age distribution and time. Health Policy. 2005;71:23–42. doi: 10.1016/j.healthpol.2004.05.007. [DOI] [PubMed] [Google Scholar]
- Dybczak K, Przywara B. The Role of Technology on Health Care Expenditure on the EU European Economy – Economic Paper 400. Brussels, Belgium: Directorate General for Economic and Monetary Affairs, European Commission; 2010. Available from: http://ec.europa.eu/economy_finance/publications/economic_paper/2010/ecp400_en.htm. [Google Scholar]
- Ekman M, Sjogren I, James S. Cost-effectiveness of the Taxus paclitaxel-eluting stent in the Swedish healthcare system. Scand Cardiovasc J. 2006;40:17–24. doi: 10.1080/14017430500296323. [DOI] [PubMed] [Google Scholar]
- Filion KB, Roy AM, Baboushkin ET, Rinfret S, Eisenberg MJ. Cost-effectiveness of drug-eluting stents including the economic impact of late stent thrombosis. Am J Cardiol. 2006;103:338–344. doi: 10.1016/j.amjcard.2008.09.086. [DOI] [PubMed] [Google Scholar]
- Fuchs VR. Health care for the elderly: how much? Who will pay for it? Health Aff (Millwood) 1999;18:11–21. doi: 10.1377/hlthaff.18.1.11. [DOI] [PubMed] [Google Scholar]
- Fuchs VR, Sox HR. Physicians’ views of the relative importance of thirty medical innovations. Health Aff (Millwood) 2001;20:30–42. doi: 10.1377/hlthaff.20.5.30. [DOI] [PubMed] [Google Scholar]
- Gandjour A, Weylan EJ. Cost-effectiveness of preventing fractures by hip protectors in elderly institutionalized patients in Germany. Value Health. 2008;11:1088–1095. doi: 10.1111/j.1524-4733.2008.00393.x. [DOI] [PubMed] [Google Scholar]
- Givon U, Ginsberg GM, Horoszowski H, Shemer J. Cost-utility analysis of total hip anthroplasties. Technology assessment of surgical procedures by mailed questionnaires. Int J Technol Assess. 1998;14:735–742. doi: 10.1017/s0266462300012046. [DOI] [PubMed] [Google Scholar]
- Goetghebeur MM, Forrest S, Hay JW. Understanding the underlying drivers of inpatient cost growth: a literature review. Am J Manag Care. 2003;9(Spec No 1):SP3–SP12. [PubMed] [Google Scholar]
- Goyen M, Debatin J. Healthcare costs for new technologies. Eur J Nucl Med Mol Imaging. 2009;36:139–143. doi: 10.1007/s00259-008-0975-y. [DOI] [PubMed] [Google Scholar]
- Greenberg D, Rosenfield K, Garcia LA, et al. In-hospital costs of self-expanding Nitinol Stent Implantation vs. Balloon Angioplasty in the Femoropopliteal Artery (The VascuCoil Trial) J Vasc Interv Radiol. 2004;15:1065–1069. doi: 10.1097/01.RVI.0000136293.18041.88. [DOI] [PubMed] [Google Scholar]
- Grignon M. McMaster University; 2005. Aging, Health and Aggregate Medical Care Spending in France. Department of Economics Working Papers 2005–05. Available from: http://www.econbiz.de/en/search/detailed-view/doc/all/Aging,%20Health%20and%20Aggregate%20Medical%20Care%20Spending%20in%20France/10005635244/?no_cache=1. Accessed March 17, 2013. [Google Scholar]
- Hall RE, Jones CI. The Value of Life and the Rise in Health Spending. 2004 National Bureau of Economic Research Working Paper Series, No 10737. Available from: http://qje.oxfordjournals.org/content/122/1/39.short. Accessed March 17, 2013. [Google Scholar]
- Hay JW. Hospital cost drivers: an evaluation of 1998–2001 state-level data. Am J Manag Care. 2003;9:SP13–SP24. [PubMed] [Google Scholar]
- Hillman BJ. Government health policy and the diffusion of new medical devices. Health Serv Res. 1986;21:681–711. [PMC free article] [PubMed] [Google Scholar]
- Holahan J, Dor A, Zuckerman S. Understanding the recent growth in Medicare physician expenditures. JAMA. 1990;263:1658–1661. [PubMed] [Google Scholar]
- Honkanen LA, Mushlin AI, Lachs M, Schackman BR. Can hip protector use cost effectively prevent fractures in community-dwelling geriatric populations? J Am Geriatr Soc. 2006;54:1658–1665. doi: 10.1111/j.1532-5415.2006.00939.x. [DOI] [PubMed] [Google Scholar]
- Huber M, Orosze E. Health expenditure trends in OECD countries, 1990–2001. Health Care Financ Rev. 2003;25:1–22. [PMC free article] [PubMed] [Google Scholar]
- Jones CI. Why have Health Expenditures as a Share of GDP Risen So Much? National Bureau of Economic Research Working Paper Series, No 9325; 2002. Available from: http://www.stanford.edu/~chadj/health300.pdf. Accessed March 17, 2013. [Google Scholar]
- Kaiser C, Brunner-La Rocca HP, Buser PT, et al. Incremental cost-effectiveness of drug-eluting stents compared with a third-generation bare-metal stent in a real-world setting: randomised Basel Stent Kosten Effekivitats Trial (BASKET) Lancet. 2005;366:921–929. doi: 10.1016/S0140-6736(05)67221-2. [DOI] [PubMed] [Google Scholar]
- Koenig L, Siegel JM, Dobson A, Hearle K, Ho S, Rudowitz R. Drivers of healthcare expenditures associated with physician services. Am J Manag Care. 2003;9(Spec No 1):SP34–SP42. [PubMed] [Google Scholar]
- Kuukasjarvi P, Rasanen P, Malmivaara A, Aronen P, Sintonen H. Economic evaluation of drug-eluting stents: a systematic literature review and model-based cost-utility analysis. Int J Technol Assess. 2007;23:473–479. doi: 10.1017/S0266462307070560. [DOI] [PubMed] [Google Scholar]
- Lord SJ, Howard K, Allen F, et al. A systematic review and economic analysis of drug-eluting coronary stents available in Australia. Med J Aust. 2005;183:464–471. doi: 10.5694/j.1326-5377.2005.tb07124.x. [DOI] [PubMed] [Google Scholar]
- March LM, Barcinilla AL, Cross MJ, et al. Costs and outcomes of total hip and knee joint replacement for rheumatoid arthritis. Clin Rheumatol. 2008;27:1235–1242. doi: 10.1007/s10067-008-0891-3. [DOI] [PubMed] [Google Scholar]
- Marinelli M, Soccetti A, Panfoli N, de Palma L. Cost-effectiveness of cemented versus cementless total hip anthroplasty. A Markov decision analysis based on implant cost. J Orthop Traumatol. 2008;9:23–28. doi: 10.1007/s10195-008-0100-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martin S, Rice N, Smith PC. Does health care spending improve health outcomes? Evidence from English programme budgeting data. J Health Econ. 2008;27:826–842. doi: 10.1016/j.jhealeco.2007.12.002. [DOI] [PubMed] [Google Scholar]
- Mas N, Seinfield J. Is managed care restraining the adoption of technology by hospitals? J Health Econ. 2008;27:1026–1045. doi: 10.1016/j.jhealeco.2008.02.009. [DOI] [PubMed] [Google Scholar]
- Mattijs S, Lambooji PE, Westert GP. Diffusion of innovations in health care: does the structural context determine its direction? Int J Technol Assess. 2010;26:415–420. doi: 10.1017/S0266462310001017. [DOI] [PubMed] [Google Scholar]
- McClellan M, Newhouse JP. The marginal cost-effectiveness of medical technology: a panel instrumental-variables approach. J Econom. 1997;77:39–64. [Google Scholar]
- McKenzie L, Vale L, Stearns S. Metal on metal hip resurfacing arthroplasty. An economic analysis. Eur J Health Econ. 2003;4:122–129. doi: 10.1007/s10198-002-0158-x. [DOI] [PubMed] [Google Scholar]
- Mitton CR, Rose MS, Kohman ML, Sheldon RS. Cost-utility analysis of pacemakers for the treatment of vasovagal syncope. Am J Cardiol. 1999;84:1356–1359. doi: 10.1016/s0002-9149(99)00574-3. [DOI] [PubMed] [Google Scholar]
- Nichol G, Kaul P, Huszti E, et al. Cost-effectiveness of cardiac resynchronization therapy in patients with symptomatic heart failure. Ann Intern Med. 2004;141:343–351. doi: 10.7326/0003-4819-141-5-200409070-00102. [DOI] [PubMed] [Google Scholar]
- Newhouse J. Medical care costs: how much welfare loss? J Econ Perspect. 1992;6:3–21. doi: 10.1257/jep.6.3.3. [DOI] [PubMed] [Google Scholar]
- Neyt M, Thiry N, Rameekers D, Van Brabandt H. Cost-effectiveness of implantable cardioverter defibrillators for primary prevention in a Belgian context. Appl Health Econ Health Policy. 2008;6:67–80. doi: 10.2165/00148365-200806010-00006. [DOI] [PubMed] [Google Scholar]
- Okunade AA, Murthy VNR. Technology as a major driver of health care costs: a cointegration analysis of the Newhouse conjecture. J Health Econ. 2002;21:147–159. doi: 10.1016/s0167-6296(01)00122-9. [DOI] [PubMed] [Google Scholar]
- Oliveira Martins J, De La Maisonneuve C. The Drivers of Public Expenditure on Health and Long-Term Care: An Integrated Approach. 2006 Available from: http://ssrn.com/abstract=917782. Accessed March 17, 2013. [Google Scholar]
- Owens DK, Sanders GD, Harris RA, et al. Cost-effectiveness of implantable cardioverter defibrillators relative to amiodarone for prevention of sudden cardiac death. Ann Intern Med. 1997;126:1–12. doi: 10.7326/0003-4819-126-1-199701010-00001. [DOI] [PubMed] [Google Scholar]
- Packer C, Simpson S, Stevens A. International diffusion of new health technologies: a ten-country analysis of six health technologies. Int J Technol Assess. 2006;22:419–428. doi: 10.1017/S0266462306051336. [DOI] [PubMed] [Google Scholar]
- Pammolli F, Riccaboni M, Oglialoro C, et al. Medical Devices Competitiveness and Impact on Public Health Expenditure. Bruxelles, Belgium: Enterprise Directorate-General, European Commission; 2005. Available from: http://ideas.repec.org/p/pra/mprapa/16021.html. [Google Scholar]
- Peden EA, Freeland MS. A historical analysis of medical spending growth, 1960–1993. Health Aff (Millwood) 1995;14:235–247. doi: 10.1377/hlthaff.14.2.235. [DOI] [PubMed] [Google Scholar]
- Peden EA, Freeland MS. Insurance effects on US medical spending (1960–1993) Health Econ. 1998;7:671–687. doi: 10.1002/(sici)1099-1050(199812)7:8<671::aid-hec379>3.0.co;2-9. [DOI] [PubMed] [Google Scholar]
- PricewaterhouseCoopers The Factors Fueling Risking Healthcare Costs. 2002 Report prepared for the American Association of Health Plans. Available from: http://heartland.org/sites/all/modules/custom/heartland_migration/files/pdfs/14621.pdf. Accessed March 15, 2013. [Google Scholar]
- Rettig RA. Medical innovation duels cost containment. Health Aff (Millwood) 1994;13:7–27. doi: 10.1377/hlthaff.13.3.7. [DOI] [PubMed] [Google Scholar]
- Sanders GD, Hlatky MA, Owens DK. Cost-effectiveness of implantable cardioverter defibrillators. N Engl J Med. 2005;353:1471–1480. doi: 10.1056/NEJMsa051989. [DOI] [PubMed] [Google Scholar]
- Sanders GD, Hlatky MA, Every NR, et al. Potential cost-effectiveness of prophylactic use of the implantable cardiovascular defibrillator or amiodarone after myocardial infarction. Ann Intern Med. 2001;135:870–883. doi: 10.7326/0003-4819-135-10-200111200-00007. [DOI] [PubMed] [Google Scholar]
- Sanders GD, Hlatky MA, Owens DK. Special report: cost-effectiveness of implantable cardioverter defibrillators in a MADIT-II population. Technology Evaluation Center Assessment Program Report. 2004;19(3) [PubMed] [Google Scholar]
- Sharples LD, Dryer M, Cafferty F, et al. Cost-effectiveness of ventricular assist device use in the United Kingdom: Results from the evaluation of Ventricular Assist Device Programme in the UK (EVAD-UK) J Heart Lung Transplant. 2006;25:1336–1343. doi: 10.1016/j.healun.2006.09.011. [DOI] [PubMed] [Google Scholar]
- Schreyogg J, Baumler M, Busse R. Balancing adoption and affordability of medical devices in Europe. Health Policy. 2009;92:218–224. doi: 10.1016/j.healthpol.2009.03.016. [DOI] [PubMed] [Google Scholar]
- Segui-Gomez M, Keuffel E, Frick KD. Cost and effectiveness of hip protectors among the elderly. Int J Technol Assess. 2002;18:55–66. [PubMed] [Google Scholar]
- Shrive FM, Manns BJ, Galbraith PD, et al. Economic evaluation of sirolimus-eluting stents. Can Med Assoc J. 2005;172:345–351. doi: 10.1503/cmaj.1041062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singh S, Sun H, Anis AH. Cost-effectiveness of hip protectors in the prevention of osteoporosis related hip fractures in elderly nursing home residents. J Rheumatol. 2004;31:1607–1613. [PubMed] [Google Scholar]
- Skinner J, Staiger D. Technology Diffusion and Productivity Growth in Health Care. doi: 10.1162/REST_a_00535. National Bureau of Economic Research Working Paper Series, No 14865; 2009. Available from: http://www.dartmouth.edu/~jskinner/documents/SkinnerStaigerw14865_000.pdf. Accessed March 17, 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith SD, Heffler SK, Freeland MS. The Impact of Technological Change on Health Care Cost Increases: An Evaluation of the Literature. Health Care Financing Administration Working Paper; 2000. Available from: http://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/NationalHealthExpendData/downloads/tech_2000_0810.pdf. [Google Scholar]
- Von Hout BA, Serruys PW, Lemos PA, et al. One-year cost-effectiveness of sirolimus eluting stents compared with bare metal stents in the treatment of single native de novo coronary lesions: an analysis from the Ravel trial. Heart. 2005;91:507–512. doi: 10.1136/hrt.2004.034454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weisbrod BA. The health care quadrilemma: an essay on technological change, insurance, quality of care and cost containment. J Econ Lit. 1991;29:523–532. [Google Scholar]
- Yao G, Freemantle N, Calvert MJ, et al. The long-term cost-effectiveness of cardiac resynchronization therapy with or without an implantable cardioverter defibrillator. Eur Heart J. 2007;28:42–51. doi: 10.1093/eurheartj/ehl382. [DOI] [PubMed] [Google Scholar]
- Yock CA, Boothroyd DB, Owens DK, Garber AM, Hlatky MA. Cost-effectiveness of bypass surgery vs stenting in patients with multivessel coronary artery disease. Am J Med. 2003;115:382–389. doi: 10.1016/s0002-9343(03)00296-1. [DOI] [PubMed] [Google Scholar]
- You JJ, Woo A, Dennis TK, et al. Life expectancy gains and cost-effectiveness of implantable cardioverter defibrillators for the primary prevention of sudden cardiac death in patients with hypertrophic cardiomyopathy. Am Heart J. 2007;145:899–907. doi: 10.1016/j.ahj.2007.06.026. [DOI] [PubMed] [Google Scholar]
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Organisation for Economic Co-operation and Development . OECD Health Data 2011. Paris, France: Organisation for Economic Co-operation and Development; 2011. Available from http://www.oecd.org/health/health-systems/healthataglance2011.htm. [Google Scholar]
- 2.Lubitz JD, Riley GF. Trends in Medicare payments in the last year of life. N Engl J Med. 1993;328:1092–1096. doi: 10.1056/NEJM199304153281506. [DOI] [PubMed] [Google Scholar]
- 3.Organisation for Economic Co-operation and Development . OECD Health at a Glance: Europe 2010. Paris, France: Organisation for Economic Co-operation and Development; 2010. [Google Scholar]
- 4.Organisation for Economic Co-operation and Development Projecting OECD Health and Long Term Care Expenditures: What are the Main Drivers? Organisation for Economic Co-operation and Development Economic Department Working Paper, No 477; 2006. Available from: http://www.oecd.org/tax/public-finance/36085940.pdf. Accessed March 15, 2013.
- 5.Centers for Disease Control and Prevention . Health, United States, 2009 with Special Feature on Medical Technology. US Department of Health and Human Services; Hyattsville, MD: 2009. Available from: http://www.cdc.gov/nchs/data/hus/hus09.pdf. Accessed March 15, 2013. [Google Scholar]
- 6.Congressional Budget Office . Technological Change and The Growth of Health Care Spending. Congressional Budget Office. Washington, DC: Congressional Budget Office; 2008. [Google Scholar]
- 7.PricewaterhouseCoopers The Factors Fueling Risking Healthcare Costs. 2002. Report prepared for the American Association of Health Plans. Available from: http://heartland.org/sites/all/modules/custom/heartland_migration/files/pdfs/14621.pdf. Accessed March 15, 2013.
- 8.Fuchs VR. Economics, values, and health care reform. Am Econ Rev. 1996;86(1):1–24. [PubMed] [Google Scholar]
- 9.Cutler DM. Technology, Health Costs, and the NIH, Harvard University and the National Bureau of Economic Research. Paper prepared for the National Institutes of Health Economics Roundtable on Biomedical Research; September 1995. [Google Scholar]
- 10.Newhouse J. Medical care costs: How much welfare loss? J Econ Perspect. 1992;6:3–21. doi: 10.1257/jep.6.3.3. [DOI] [PubMed] [Google Scholar]
- 11.Sorenson C, Drummond M. The socio-economic value of orthopaedic devices: Evidence and methodological challenges. Orthopedic Research and Reviews. 2012;4:87–96. [Google Scholar]
- 12.Centre for Review and Dissemination . Abstractors Guide for NHS EED. York, UK: Centre for Review and Dissemination; 2009. Available from: http://ospguides.ovid.com/OSPguides/cleeddb.htm. [Google Scholar]
- 13.Berndt ER, Cutler DM, Frank RG, Griliches Z, Newhouse JP, Triplett JE. Medical care prices and output. In: Culyer AJ, Newhouse JP, editors. Handbook of Health Economics, Volume 1A. Amsterdam, The Netherlands: Elsevier; 2000. [Google Scholar]
- 14.Okunade AA, Murthy VNR. Technology as a major driver of health care costs: a cointegration analysis of the Newhouse conjecture. J Health Econ. 2002;21:147–159. doi: 10.1016/s0167-6296(01)00122-9. [DOI] [PubMed] [Google Scholar]
- 15.Di Matteo L. The macro determinants of health expenditure in the United States and Canada: assessing the impact of income, age distribution and time. Health Policy. 2005;71:23–42. doi: 10.1016/j.healthpol.2004.05.007. [DOI] [PubMed] [Google Scholar]
- 16.Jones CI. Why have Health Expenditures as a Share of GDP Risen So Much? 2002. National Bureau of Economic Research Working Paper Series, No 9325. Available from: http://ideas.repec.org/p/nbr/nberwo/9325.html. Accessed March 15, 2013.
- 17.Peden EA, Freeland MS. A historical analysis of medical spending growth, 1960–1993. Health Affairs. 1995;14:235–247. doi: 10.1377/hlthaff.14.2.235. [DOI] [PubMed] [Google Scholar]
- 18.Dybczak K, Przywara B. The Role of Technology on Health Care Expenditure on the EU European Economy – Economic Paper 400. Brussels, Belgium: Directorate General for Economic and Monetary Affairs, European Commission; 2010. Available from: http://ec.europa.eu/economy_finance/publications/economic_paper/2010/ecp400_en.htm. [Google Scholar]
- 19.Smith SD, Heffler SK, Freeland MS. The Impact of Technological Change on Health Care Cost Increases: An Evaluation of the Literature. 2000. Health Care Financing Administration Working Paper. Available from: http://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/NationalHealthExpendData/downloads/tech_2000_0810.pdf.
- 20.Scitovski AA. Changes in the cost of treatment of selected illnesses, 1971–1981. Med Care. 1985;23:1345–1357. doi: 10.1097/00005650-198512000-00004. [DOI] [PubMed] [Google Scholar]
- 21.Bryan S, Buxton M, Brenna E. Estimating the impact of a diffuse technology on the running costs of a hospital. Int J Technol Assess. 2000;16:787–798. doi: 10.1017/s0266462300102065. [DOI] [PubMed] [Google Scholar]
- 22.Weisbrod BA. The health care quadrilemma: an essay on technological change, insurance, quality of care and cost containment. J Econ Lit. 1991;29:523–532. [Google Scholar]
- 23.Rettig RA. Medical innovation duels cost containment. Health Aff (Millwood) 1994;13:7–27. doi: 10.1377/hlthaff.13.3.7. [DOI] [PubMed] [Google Scholar]
- 24.Fuchs VR. Health care for the elderly: how much? Who will pay for it? Health Aff (Millwood) 1999;18:11–21. doi: 10.1377/hlthaff.18.1.11. [DOI] [PubMed] [Google Scholar]
- 25.Cutler DM, McClellan M. Is technological change in medicine worth it? Health Aff (Millwood) 2001;20:11–29. doi: 10.1377/hlthaff.20.5.11. [DOI] [PubMed] [Google Scholar]
- 26.Baker LC. Managed care and technology adoption in health care: evidence from magnetic resonance imaging. J Health Econ. 2001;20:395–421. doi: 10.1016/s0167-6296(01)00072-8. [DOI] [PubMed] [Google Scholar]
- 27.Chernew M, Fendrick AM, Hirth RA. Managed care and medical technology: implications for cost growth. Health Aff (Millwood) 1997;16:196–206. doi: 10.1377/hlthaff.16.2.196. [DOI] [PubMed] [Google Scholar]
- 28.Cutler DM, Huckman RS. Technological development and medical productivity: the diffusion of angioplasty in New York state. J Health Econ. 2003;22:187–217. doi: 10.1016/S0167-6296(02)00125-X. [DOI] [PubMed] [Google Scholar]
- 29.Martin S, Rice N, Smith PC. Does health care spending improve health outcomes? Evidence from English programme budgeting data. J Health Econ. 2008;27:826–842. doi: 10.1016/j.jhealeco.2007.12.002. [DOI] [PubMed] [Google Scholar]
- 30.Greenberg D, Rosenfield K, Garcia LA, et al. In-hospital costs of self-expanding nitinol stent implantation vs. balloon angioplasty in the femoropopliteal artery (The VascuCoil Trial) J Vasc Interv Radiol. 2004;15:1065–1069. doi: 10.1097/01.RVI.0000136293.18041.88. [DOI] [PubMed] [Google Scholar]
- 31.Von Hout BA, Serruys PW, Lemos PA, et al. One-year cost-effectiveness of sirolimus eluting stents compared with bare metal stents in the treatment of single native de novo coronary lesions: an analysis from the Ravel trial. Heart. 2005;91:507–512. doi: 10.1136/hrt.2004.034454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bagust A, Grayson AD, Palmer ND, Perry RA, Walley T. Cost-effectiveness of drug eluting coronary artery stenting in a UK setting: cost-utility study. Heart. 2006;92:68–74. doi: 10.1136/hrt.2004.053850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Blank J, Vogelaar I. Specifying technical change: a research on the nature of technical change in Dutch hospital industry. Q Rev Econ Finance. 2004;44:448–463. [Google Scholar]
- 34.Bradley TB, Kominski GF. Contributions of case mix and intensity change to hospital cost increases. Health Care Financ Rev. 1992;14:151–163. [PMC free article] [PubMed] [Google Scholar]
- 35.Mas N, Seinfeld J. Is managed care restraining the adoption of technology by hospitals? J Health Econ. 2008;27:1026–1045. doi: 10.1016/j.jhealeco.2008.02.009. [DOI] [PubMed] [Google Scholar]
- 36.Cutler DM, McClellan M. The determinants of technological change in heart attack treatment. 1996. NBER Working Paper No 5751. Available from: http://ideas.repec.org/p/nbr/nberwo/5751.html. Accessed March 17, 2013.
- 37.Barros P, Martinez-Giralt X. Technological Adoption in Health Care. 2009. CEPR Discussion Papers 7558. Available from: http://ideas.repec.org/p/unl/unlfep/wp545.html. Accessed March 17, 2013.
- 38.Sorenson C, Kanavos P. Medical technology procurement in Europe: a cross-country comparison of current practice and policy. Health Policy. 2011;100:43–50. doi: 10.1016/j.healthpol.2010.08.001. [DOI] [PubMed] [Google Scholar]
- 39.Obremskey WT, Dail T, Jahangir AA. Value-based purchasing of medical devices. Clin Orthop Relat Res. 2012;470:1054–1064. doi: 10.1007/s11999-011-2147-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Cutler DM. The lifetime costs and benefits of medical technology. J Health Econ. 2007;26:1081–1100. doi: 10.1016/j.jhealeco.2007.09.003. [DOI] [PubMed] [Google Scholar]
- 41.Lambooij MS, Engelfriet P, Westert GP. Diffusion of innovations in health care: does the structural context determine its direction? Int J Technol Assess. 2010;26:415–420. doi: 10.1017/S0266462310001017. [DOI] [PubMed] [Google Scholar]
- 42.March LM, Barcinilla AL, Cross MJ, et al. Costs and outcomes of total hip and knee joint replacement for rheumatoid arthritis. Clin Rheumatol. 2008;27:1235–1242. doi: 10.1007/s10067-008-0891-3. [DOI] [PubMed] [Google Scholar]
- 43.Marinelli M, Soccetti A, Panfoli N, de Palma L. Cost-effectiveness of cemented versus cementless total hip anthroplasty. A Markov decision analysis based on implant cost. J Orthop Traumatol. 2008;9:23–28. doi: 10.1007/s10195-008-0100-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Banz K. Cardiac resynchronization therapy (CRT) in heart failure: a model to assess the economic value of this new medical technology. Value Health. 2005;8:128–139. doi: 10.1111/j.1524-4733.2005.03092.x. [DOI] [PubMed] [Google Scholar]
- 45.Brunner-La Rocca HP, Kaiser C, Bernheim A, et al. Cost-effectiveness of drug-eluting stents in patients at high or low risk of major cardiac events in the Basel Stent KostenEff Ektivitäts Trial (BASKET): an 18-month analysis. Lancet. 2007;370:155–159. doi: 10.1016/S0140-6736(07)61660-2. [DOI] [PubMed] [Google Scholar]
- 46.Hay JW. Hospital cost drivers: an evaluation of 1998–2001 state-level data. Am J Manag Care. 2003;9:SP13–SP24. [PubMed] [Google Scholar]
- 47.Donavan GD, King G. Advanced Medical Technology Association; 2011. Estimates of Medical Device Spending in the United States. Available from: www.amsa.org/.../king_paper_medical_device_spending.sflb.ashx. [Google Scholar]
- 48.Luce BR, Elixhauser A. Estimating costs in the economic evaluation of medical technologies. Int J Technol Assess. 1990;6:57–75. doi: 10.1017/s026646230000893x. [DOI] [PubMed] [Google Scholar]
- 49.Cutler DM, Rosen AB, Vijan S. The value of medical spending in the United States, 1960–2000. N Engl J Med. 2006;355:920–927. doi: 10.1056/NEJMsa054744. [DOI] [PubMed] [Google Scholar]
- 50.Skinner J, Staiger D. Technology Diffusion and Productivity Growth in Health Care. 2009. National Bureau of Economic Research Working Paper Series, No 14865. Available from: http://www.dartmouth.edu/~jskinner/documents/SkinnerStaigerw14865_000.pdf. Accessed March 17, 2013. [DOI] [PMC free article] [PubMed]
- 51.Bozic KJ, Morshed S, Silverstein MD, Rubash HE, Kahn JG. Use of cost-effectiveness analysis to evaluate new technologies in orthopaedics: the case of alternative bearing surfaces in total hip arthroplasty. J Bone Joint Surg Am. 2006;88:706–714. doi: 10.2106/JBJS.E.00614. [DOI] [PubMed] [Google Scholar]
- 52.Singh S, Sun H, Anis AH. Cost-effectiveness of hip protectors in the prevention of osteoporosis related hip fractures in elderly nursing home residents. J Rheumatol. 2004;31:1607–1613. [PubMed] [Google Scholar]
- 53.Segui-Gomez M, Keuffel E, Frick KD. Cost and effectiveness of hip protectors among the elderly. Int J Technol Assess. 2002;18:55–66. [PubMed] [Google Scholar]
- 54.Fuchs VR, Sox HC. Physicians’ views of the relative importance of thirty medical innovations. Health Aff (Millwood) 2001;20:30–42. doi: 10.1377/hlthaff.20.5.30. [DOI] [PubMed] [Google Scholar]
- 55.Sorenson C, Tarricone R, Siebert M, Drummond M. Applying health economics for policy decision making: how much do devices differ from drugs? Europace. 2011;13(Suppl 2):ii54–ii58. doi: 10.1093/europace/eur089. [DOI] [PubMed] [Google Scholar]