Abstract
OBJECTIVES
Deep sternal wound infections are significant and severe complications following cardiac surgery and substantially influence perioperative morbidity and mortality. We present the experience of our department using two different surgical treatments over a three-year period.
METHODS
Between January 2009 and December 2011, a total of 3274 cardiac procedures with complete median sternotomy were performed in our department. In 94 patients (3%), a deep sternal wound infection occurred, including sternal instability with consecutive surgical treatment. The patients either received wound debridement with sternum refixation and suction-irrigation drainage (SID; n = 72) or sternum refixation only (RF; n = 22) if there was sternal instability with limited signs of infection. SID was routinely installed for 7 days: the irrigation solution contained neomycin. In all cases, swabs were taken and analysed. The different methods were evaluated in respect of their clinical outcomes.
RESULTS
The success rate—defined as single, uncomplicated procedure—of the SID treatment was 74%, compared with 59% of the isolated sternum refixation. Complications included continuous infection, recurrence of sternal instability and wound necrosis. Eighty-eight percent of the swabs in the SID group were positive, compared with 32% in the sternal refixation only group. The dominating pathogenic germs were coagulase-negative staphylococci and staphylococcus aureus. Mortality was 10% for the SID group and 5% for the RF group.
CONCLUSIONS
Contrary to accepted opinion, the suction-irrigation drainage is an appropriate therapy for deep sternal wound infections. Nevertheless, deep sternal wound infections after cardiac surgery remain severe complications and are related to increased morbidity and mortality.
Keywords: Deep sternal wound infection, Suction-irrigation drainage, Wound closure
INTRODUCTION
Post-sternotomy wound infections are a common and severe complication following cardiac surgery, with a reported incidence of up to 8% [1–3]. Deep sternal wound infections (DSWI), including sternal osteomyelitis and mediastinitis, are associated with significant morbidity and mortality rates up to 30% [1–3]. This frequently leads to prolonged hospital stay and the need for repeated surgical procedures, as well as extensive treatment costs.
A wide variety of treatment modalities for DSWI have been developed in the recent years, ranging from simple surgical revision to extensive reconstructive plastic surgery, but there is still lack of consensus among surgeons regarding optimal management of post-sternotomy osteomyelitis, mostly due to the fact that scientific evidence for the superiority of certain procedures is inconsistent [2, 3].
The most common therapeutic procedures for DSWI are surgical debridement, followed either by immediate wound re-closure (with optional installation of a suction/irrigation system) or a vacuum-assisted closure (VAC) therapy. More complex surgical treatments include the use of omentum majus or pectoralis major muscle flaps for wound coverage [3, 4].
In recent years, a treatment algorithm including VAC therapy, eventually combined with omental or different muscular flaps, seems to be preferred by the majority of cardiac centres.
The aim of the present study was to critically evaluate the effectiveness of our department's therapeutic regimen, which is predominantly based on direct wound closure with or without a closed suction-irrigation system, and to compare results with published data concerning treatment modalities of deep sternal wound infections.
MATERIAL AND METHODS
Patient selection and data collection
Between January 2009 and December 2011 a total of 3274 cardiac procedures with complete median sternotomy were performed in our department. Data on all patients were prospectively collected and retrospectively analysed. According to the classification of El Oakley Wright, 94 cases of deep sternal wound infection could be identified, which amount to 2.9% of the study cohort [5]. Data on all patients affected by DSWI—including preoperative characteristics, type of cardiac surgery, intraoperative microbiological samples, postoperative course and therapy success rate—defined as single, uncomplicated procedure, were statistically analysed and compared between the two treatment groups and data published in literature.
Treatment algorithm and surgical technique
The standard approach for treatment of postoperative DSWI in our department is an extensive pre-sternal wound debridement with consecutive removal of all osteosyntetic material and resection of necrotic portions of the sternal bone. After cleansing the wound with an antimicrobial solution (Prontosan®, B. Braun, Melsungen, Germany) a suction-irrigation drainage is applied retrosternally. This consists of two jugularly placed 16 CH catheters for irrigation and two 32 CH chest tubes for mediastinal drainage. Finally, the sternum is rewired and the wound closed with single sutures (Figs 1 and 2). Continuous suction and irrigation (2400 ml/day) with diluted neomycine (1 g/1000 ml) is applied for 7 days postoperatively.
Figure 1:
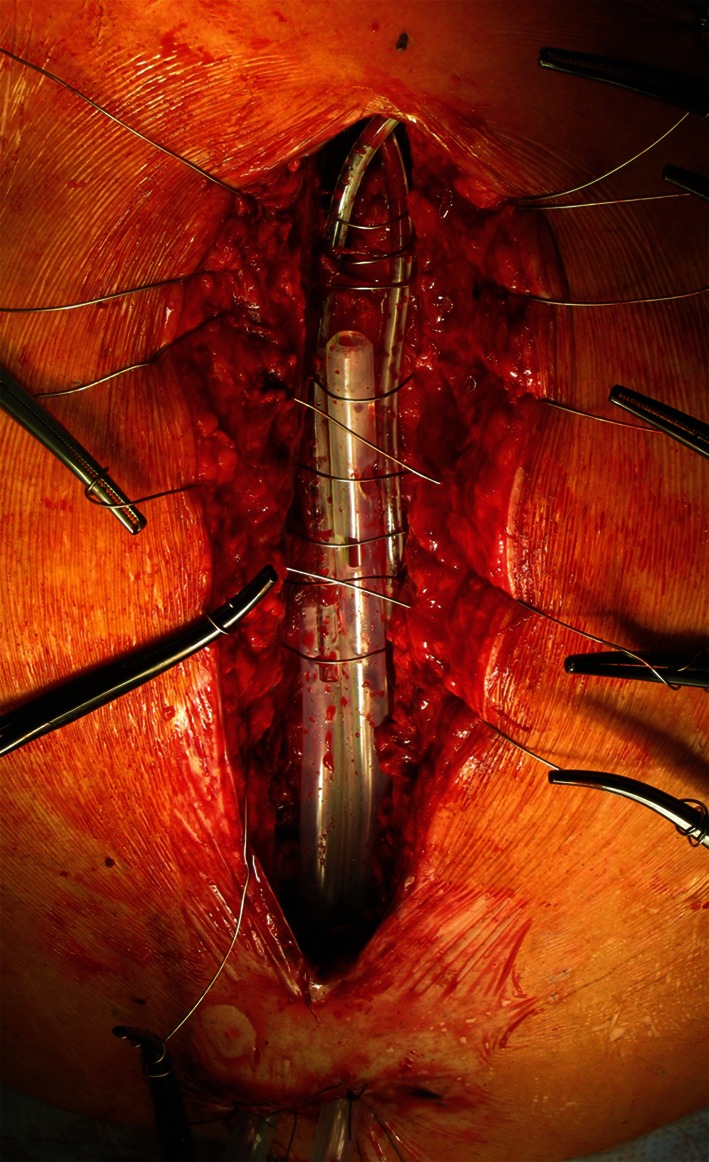
Insertion of the suction-irrigation drainage and sternal rewiring.
Figure 2:

Primary wound closure with single sutures.
Alternatively, in cases of sternal instability with limited signs of infection, the suction irrigation drainage may be spared.
Allocation to either treatment group was left to the surgeon's discretion in a non-randomized fashion. Intraoperative microbiological samples were obtained consecutively in all patients.
In cases of treatment failure with the need for further operative revisions, surgical approach depended on intraoperative findings. If enough vital sternal bone remained for rewiring, another SID was applied. In all other cases, definite wound closure was performed with omentum majus or pectoralis major muscle flaps. Temporary wound treatment with VAC therapy as preparation for soft tissue flap coverage was applied if necessary.
Statistical methods
Descriptive statistics are presented as mean ± standard deviation and as percentage for discrete variables. The statistical significances were determined using Student's unpaired t-test, Fisher's exact test, the chi-squared test or Mann-Whitney test as appropriate. Significance was assessed at a P-level less than 0.05.
Data were stored and analysed by the use of the software JMP® 8 (SAS Institute Inc. Cary, North Carolina, USA).
RESULTS
Of the 94 identified cases of deep sternal wound infection, 72 patients were treated with suction-irrigation drainage (SID) and 22 patients received sternum refixation only (RF). Preoperative characteristics, as well as the type of cardiac surgery of both groups are shown in Table 1. The distribution of the different cardiac procedures did not differ significantly between the groups. Regarding patient demographics of the study cohorts, two significant differences could be seen. Whereas the sternal refixation group contained significantly more male patients (P = 0.03), peripheral artery disease was significantly more frequent in the SID cohort (P = 0.01).
Table 1:
Preoperative characteristics and type of primary surgery
| Sternal refixation (n = 22) | Suction-irrigation drainage (n = 72) | P-value | |
|---|---|---|---|
| Age (years) | 73.7 ± 7.6 | 70.8 ± 7.8 | 0.09 |
| Sex (male) | 90.9% (n = 20) | 75% (n = 54) | 0.03 |
| Adipositas | 36.4% (n = 8) | 31.9% (n = 23) | 0.7 |
| Diabetes | 50.0% (n = 11) | 52.8% (n = 38) | 0.82 |
| Renal insufficiency | 22.7% (n = 5) | 20.8% (n = 15) | 0.85 |
| PAD | 9.1% (n = 2) | 34.7% (n = 25) | 0.01 |
| COPD | 31.8% (n = 7) | 29.2% (n = 25) | 0.81 |
| CABG | 63.6% (n = 14) | 63.9% (n = 46) | 0.98 |
| Aortic valve replacement | 9.1% (n = 2) | 12.5% (n = 9) | 0.65 |
| Mitral valve repair | 4.5% (n = 1) | 1.4% (n = 1) | 0.41 |
| Combined procedures | 18.2% (n = 4) | 22.2% (n = 16) | 0.5 |
| Other | 4.5% (n = 1) | 0% (n = 0) | 0.09 |
| Re-operations | 4.5% (n = 1) | 2.8% (n = 2) | 0.67 |
| Re-explorations | 4.5% (n = 1) | 2.8% (n = 2) | 0.25 |
PAD: peripheral artery disease; COPD: chronic obstructive pulmonary disease; CABG: coronary artery bypass grafting.
The time between primary cardiac surgery and occurrence or diagnosis of sternal instability with consecutive surgical treatment was 21.4 ± 16.6 days (median 16 days) in group 1 (SID) and 71.4 ± 102.3 days (median 18 days) in group 2. Although the delay between cardiac procedure and onset/detection of DSWI was longer in the RF group, it failed to reach a significant level (P > 0.76).
Concerning inflammatory parameters, C-reactive protein level was significantly higher in the SID cohort, compared with the RW group (CRP: 137.1 ± 99.2 vs 62.5 ± 55.6 mg/l; P < 0.001). The comparison of preoperative leukocyte counts before surgical revision revealed similar results (12.4 ± 8.7 vs 11.2 ± 4.0 tsd/µl, P = 0.97).
In the SID group, 86% of all swabs taken intraoperatively were positive (P > 0.001). In group 2, only 32% of the microbiological samples could provide pathological germs. Coagulase-negative staphylococci and s. aureus were the dominating germs (Table 2).
Table 2:
Distribution of pathological germs in intra-operative swabs
| Sternal re-fixation group | Suction-irrigation drainage group | P-value | |
|---|---|---|---|
| Staphylococcus aureus | 57.1% (n = 4) | 23.8% (n = 15) | 0.18 |
| MRSA | 0% | 9.5% (n = 6) | 0.19 |
| Coagulase-negative staphylococci | 28.6% (n = 2) | 25.4% (n = 16) | 0.83 |
| Enterococci | 0% | 9.3% (n = 5) | 0.24 |
| Enterobacteria | 0% | 3.2% (n = 2) | 0.46 |
| Klebsiella | 0% | 3.2% (n = 2) | 0.46 |
| Escherichia coli | 0% | 1.6% (n = 1) | 0.60 |
| Candida albicans | 14.3 (n = 1) | 3.2% (n = 2) | 0.33 |
MRSA: multi-resistant Staphylococcus aureus.
The success rate—defined as single, uncomplicated procedure—of the SID treatment was 74% (n = 53), compared with 60% (n = 13) of the isolated sternum refixation (P = 0.056). In all cases of treatment failure, a further surgical revision was performed. The different surgical procedures were as follows:
In the SID cohort, eight patients received a re-SID, six patients were treated with VAC therapy, three patients underwent—and in two cases wound closure was achieved with—an omentum majus flap combined with VAC therapy. A repeated therapy failure occurred in 26% (two re-SID, three VAC). All of these patients were finally treated successfully with either a pectoralis muscle flap (four patients) or VAC therapy (one patient).
In the RF group, repeated DSWI was treated in four cases with SID, two cases with a second rewiring and in another two cases pectoralis muscle flaps were carried out. VAC therapy was applied once. Success rate was 89%. One patient with a repeated sternum refixation (only) had to undergo a third surgical revision, receiving a pectoralis muscle flap.
The proportion of sterile microbiological samples in the treatment failure cohorts were 21% (SID; n = 4) and 44% (RW; n = 4), respectively.
Mortality rate of the SID group was 10%, compared with 5% in the RF group (P = 0.32). Mean hospital stay after occurrence of DSWI was 19.3 ± 16.7 days in the SID group and 14.4 ± 12.3 days in the RF group (P < 0.12).
DISCUSSION
During the last decade, treatment of deep sternal wound infections after cardiac surgery has diversified [2, 3]. However, a general consensus regarding the optimal therapy modality has not so far been achieved. Actual development seems to favour different variations of vacuum-assisted wound closure but evidence is weak and treatment algorithms of most cardiac centres are mainly experience-driven [2, 3].
In this paper we present our experience regarding postoperative wound healing strategy, which concentrates on primary rewiring and direct wound closure after extensive debridement, with optional use of a suction-irrigation system.
Our results show different outcomes concerning the two treatment approaches. Success rate of the RF-only group was only 59%. Only 30% of the intraoperative microbiological samples could identify pathological germs and preoperative C-reactive protein levels, as well as leukocyte counts, were only moderately elevated (62.5 ± 55.6 and 11.3 ± 4). This indicates a low bacterial load and a predominantly local inflammatory reaction. Considering the local process, achieved wound healing rate is not satisfactory, compared with our second treatment group as well as results of various surgical methods [1–3] already published. Mortality rate (5%) and mean treatment duration (14.3 ± 12.3 days) are acceptable, though. Even with simple means like closed vacuum drainage systems using Redon catheters, Vos et al. could recently demonstrate considerably improved primary wound healing rates [6]. As a consequence of reported results, sternal refixation on its own is stated to be outdated and is only used in carefully selected cases without local infection and very good vascularization of the tissue.
Looking at our SID cohort, results present quite differently. Primary wound healing without any further interventions was achieved in 74%, showing a better success rate than treatment with sternal rewiring alone, although significance was not reached, owing to a small sample number. Taking into account that 86% of all intraoperatively obtained swabs were positive and CRP levels were significantly higher than in the RW cohort (137.1 ± 99.2 vs 62.5 ± 55.6 mg/l, P < 0.001), treatment with a suction-irrigation drainage proved to be highly effective in a patient cohort suffering from severe inflammatory processes.
The fact that the mean hospital treatment duration was comparable between both groups (19.3 ± 16.8 vs 14.3 ± 12.3 days)—regardless of the different degrees of sternal infection—underlines the superior performance of the SID method compared with sternal rewiring alone. The mortality rate associated with the SID treatment was 10%.
Our results are in line with the findings of Merrill et al., who demonstrated, in a consecutive series of 40 patients, excellent therapeutic effectiveness and safety of the continuous suction-irrigation drainage in a closed chest [7]. Mortality of the study cohort was 0% and the primary wound healing rate was 95%. Treatment modalities and duration are comparable to our cohort.
Assmann et al. [8], in a retrospective analyses of 5232 patients reported in 2011 on their experience with VAC treatment, compared with primary rewiring (RW) and irrigation therapy. The VAC group showed a decreased length of hospital stay (45.6 ± 18.5 vs 55.2 ± 23.6 days) and reduced mortality (15 vs 26%). Nevertheless, 39% of the VAC patients received secondary rewiring and 12% complex tissue flap coverage after VAC therapy.
Segers et al. [9] also described the superior results of VAC therapy, compared with primary rewiring (RW) with closed drainage technique, regarding recurrence of mediastinitis. Patients with VAC had a 28% chance of therapy failure vs 59% in the RW group. Mean treatment duration was 22.8 days, compared with 16.5 in the RW cohort. Again, definite wound closure was achieved only by a second surgical procedure, including 29% of reconstructive surgery with muscle flaps. The interval between initial surgery and the onset of DSWI was 17.9 days (mean). This is comparable to our data, where the median surgery-to-infection period was 21.4 ± 16.8 days.
Berg et al. [10] compared a suction-irrigation drainage vs a closed vacuum drainage system using Redon drains. His results are favourable regarding the use of the vacuum drainage system when analysing treatment failure (52 vs 16%) and postoperative hospital stay (42 ± 21.9 vs 29 ± 26.0 days). Sjögren et al. [11] as well as Doss et al. [12] confirmed these findings despite using VAC treatment instead of a vacuum drainage system with Redon drains.
An important similarity of these three cited publications is the combination of a suction-irrigation drainage and an open pre-sternal soft tissue treatment. This definitely distinguishes our therapeutic regimen from these published treatment modalities and, therefore, unfavourable results regarding the success of SID treatment are hardly comparable to our presented data.
In conclusion, we can state that our presented results are promising and can easily bear comparison, in terms of mortality, success rates and treatment duration, to already published data of various surgical treatment options. A major benefit of the proposed treatment regimen is simultaneous rewiring and pre-sternal soft tissue closure after surgical debridement. This guarantees immediate postoperative thoracic stability, which is crucial for fast weaning from mechanical ventilation as well as patients' mobility. Equally important, there is not often a need for consecutive repeat surgical intervention for wound closure—which itself is associated with relevant morbidity and mortality—especially if reconstructive surgical approaches like soft tissue or muscle flaps are required.
In a meta-analysis of 16 publications, Van Wingerden et al. highlight outcomes of muscle and omental flaps [4]. The incidence of re-explorations for flap necrosis or recurrent infection was between 3 and 18%, with mortality rates up to 29%. Other severe complications like chronic chest wall pain, shoulder weakness or abdominal hernias, were reported with frequencies of up to 50, 30 and 5%, respectively.
In our patient cohort, soft tissue flap coverage after sternal rewiring was only necessary in eight cases (11%) proving a soft tissue sparing aspect of an SID with immediate wound closure even in cases of primary therapy failure.
In a recent publication, Rodriguez Cetina Biefer et al. showed that bacterial contamination at the time of wound closure does not influence the re-infection rate in cases of DSWI [13]. Furthermore, they reported that, in terms of treatment success, no difference was found between a VAC therapy with delayed wound closure or direct wound closure, but that the VAC group showed a significantly longer hospital stay.
All these findings support our management algorithm of DSWI, which is based primarily on sternal refixation with insertion of a suction-irrigation system and direct wound closure.
We are aware that this study suffers from some serious limitations. All possible drawbacks of a non-randomized, retrospective study design apply. Due to the fact that a third treatment group—using VAC therapy or similar techniques for wound closure—is missing, we can compare our results only to historical cohorts described in literature. Therefore, caution is advised in the interpretation of the data.
Nevertheless, we think that, in the light of the presented data, the suction-irrigation drainage is a promising alternative to more common treatment approaches of deep sternal wound infections, although randomized trials are necessary to confirm our findings.
Conflict of interest: none declared.
APPENDIX. CONFERENCE DISCUSSION
Dr P. Karunakara (Visakhapatnam, India): Regarding mortality, this is greater in the suction-irrigation group. Are you thinking that rewiring is a better option?
Dr Deschka: We think that suction-irrigation drainage is the better option.
Dr Karunakara: But the mortality you have shown is greater in the suction-irrigation group.
Dr Deschka: Yes, that is right. But if you look at the cases, the proportion of the more severe wound infections was higher in the suction-irrigation drainage group. So we think this explains the higher mortality rate to some extent and, moreover, the difference is not significant between the two groups regarding mortality.
Mr R. van Valen (Rotterdam, Netherlands): I found the period before presentation with this problem very long at a median of 100 days. In our clinic, most patients present with this problem within 7 to 14 days, and a lot of them have multiple fractures, and are not really suitable for rewiring. So how do you handle those patients?
Dr Deschka: In most cases, our patients present between one and two weeks after cardiac surgery. And that is right, sometimes there are multiple fractures. But we try, as long as there is some vital sternal bone, to refixate or rewire it, and in most of the cases, it works.
Mr van Valen: And do you use a plate material, such as that from Synthes?
Dr Deschka: No. We use normal sternal wires.
Dr L. Melly (Basel, Switzerland): Don't you think it is two different entities? Because in the first group where you use the drainage, the delay was about 20 days before the diagnosis and the other one was 70 days. Don't you think that in the second group there were more primary sternal instabilities that then ended up in a secondary sternal infection?
Dr Deschka: If you look at the median period, the two groups are quite similar. In the suction-irrigation drainage, the median delay is 16 days and 18 days in the sternal refixation group. This is quite a small sample number, and there are just some patients who presented after half a year with a mediastinal problem and, therefore, you have this little bit of a difference between the two cohorts. But I do not think that there is any difference.
Dr R. Deac (Targu-Mures, Romania): Dr Deschka, one small question. In the rewiring technique, are you using the same size wire or do you change it?
Dr Deschka: No. We use the same size wires as in the primary cardiac procedures.
REFERENCES
- 1.Borger MA, Rao V, Weisel RD, Ivanov J, Cohen G, Scully HE, et al. eep sternal wound infection: risk factors and outcomes. Ann Thorac Surg. 1998;65:1050–56. doi: 10.1016/s0003-4975(98)00063-0. [DOI] [PubMed] [Google Scholar]
- 2.Schimmer C, Sommer SP, Bensch M, Leyh R. Management of post-sternotomy mediastinitis: experience and results of different therapy modalities. Thorac Cardiov Surg. 2008;56:200–4. doi: 10.1055/s-2008-1038386. [DOI] [PubMed] [Google Scholar]
- 3.Singh K, Anderson E, Harper JG. Overview and management of sternal wound infection. Semin Plast Surg. 2011;25:25–33. doi: 10.1055/s-0031-1275168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Van Wingerden JJ, Lapid O, Boonstra PW, de Mol BAJM. Muscle flaps or omental flap in the management of deep sternal wound infection. Interact CardioVasc Thorac Surg. 2011;13:179–88. doi: 10.1510/icvts.2011.270652. [DOI] [PubMed] [Google Scholar]
- 5.El Oakley RM, Wright JE. Postoperative mediastinitis: classification and management. Ann Thorac Surg. 1996;61:1030–6. doi: 10.1016/0003-4975(95)01035-1. [DOI] [PubMed] [Google Scholar]
- 6.Vos RJ, Yilmaz A, Sonker U, Kelder JC, Kloppenburg GTL. Primary closure using Redon drains vs. vacuum-assisted closure in post-sternotomy mediastinitis. Eur J Cardiothorac Surg. 2012;42 doi: 10.1093/ejcts/ezs404. [DOI] [PubMed] [Google Scholar]
- 7.Merrill WH, Akhter SA, Wolf RK, Schneeberger EW, Flege JB. Simplified treatment of positive mediastinitis. Ann Thorac Surg. 2004;78:608–12. doi: 10.1016/j.athoracsur.2004.02.089. [DOI] [PubMed] [Google Scholar]
- 8.Assmann A, Boecken U, Feindt P, Schurr P, Akhyari P, Lichtenberg A. Vacuum-assisted wound closure is superior to primary rewiring in patients with deep sternal wound infection. Thorac Cardiovasc Surg. 2011;59:25–29. doi: 10.1055/s-0030-1250598. [DOI] [PubMed] [Google Scholar]
- 9.Segers P, de Jong AP, Kloek JJ, de Mol BAJM. Post-sternotomy mediastinitis: comparison of two treatment modalities. Interact CardioVasc Thorac Surg. 2005;4:555–60. doi: 10.1510/icvts.2005.112714. [DOI] [PubMed] [Google Scholar]
- 10.Berg HF, Brands GB, van Geldorp TR, Kluytmans-VandenBergh MFQ, Kluytmans JAJW. Comparison between closed drainage techniques for the treatment of postoperative mediastinitis. Ann Thorac Surg. 2000;70:924–29. doi: 10.1016/s0003-4975(00)01524-1. [DOI] [PubMed] [Google Scholar]
- 11.Sjögren J, Malmsjö M, Gustafsson R, Ingemansson R. Post-sternotomy mediastinitis: a review of conventional surgical treatments, vacuum-assisted closure therapy and presentation of the Lund University Hospital mediastinitis algorithm. Eur J Cardiothorac Surg. 2006;30:898–990. doi: 10.1016/j.ejcts.2006.09.020. [DOI] [PubMed] [Google Scholar]
- 12.Doss M, Martens S, Wood JP, Wolff JD, Baier C, Moritz A. Vacuum-assisted suction drainage versus conventional treatment in the management of post-sternotomy osteomyelitis. Eur J Cardiothorac Surg. 2002;22:934–38. doi: 10.1016/s1010-7940(02)00594-8. [DOI] [PubMed] [Google Scholar]
- 13.Rodriguez Cetina Biefer H, Sündermann SH, Emmert MY, Rancic Z, Salzberg SP, Grünenfelder J, et al. Negative microbiological results are not mandatory in deep sternal wound infections before wound closure. Eur J Cardiothorac Surg. 2012;42:306–10. doi: 10.1093/ejcts/ezr326. [DOI] [PubMed] [Google Scholar]


