Abstract
Cerebral air embolism during pleural lavage is a rare, but potentially fatal complication. We present a case of severe cerebral air embolism that developed during pleural lavage for empyema and was successfully treated by therapeutic hypothermia. A 77-year old male patient with empyema developed severe cerebral air embolism during pleural lavage via a chest tube. Cranial computed tomography and cranial magnetic resonance imaging showed many small bubbles and widespread infarction in the territory of the right middle cerebral artery. The patient received therapeutic hypothermia maintained at 33°C for 24 h and could leave the hospital without delayed sequelae.
Keywords: Cerebral air embolism, Pleural lavage, Empyema, Therapeutic hypothermia
CASE SUMMARY
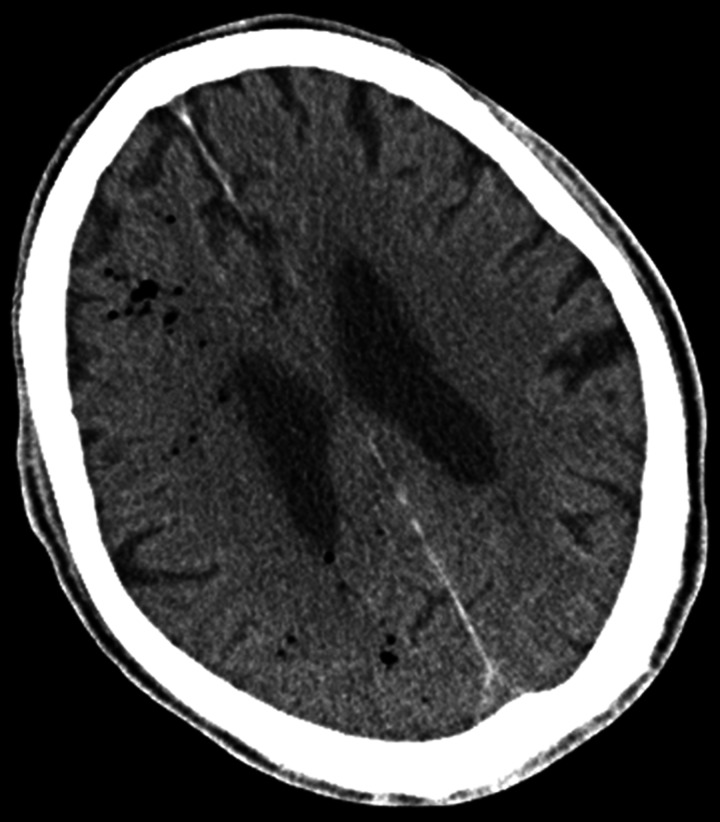
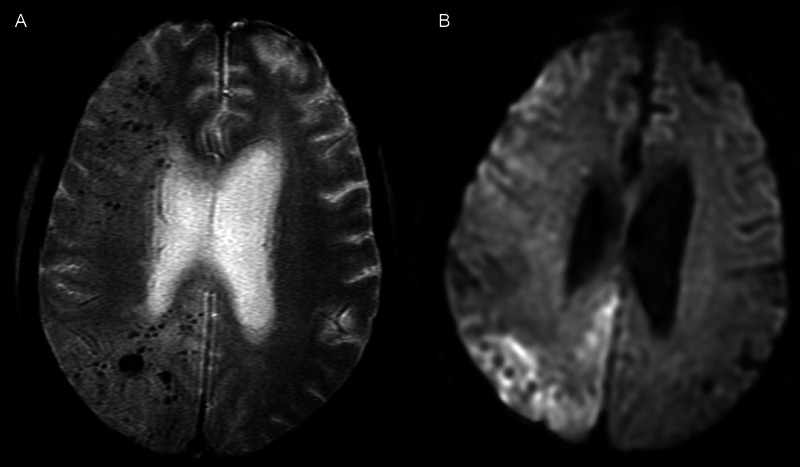
A 77-year old man with thoracic oesophageal cancer underwent subtotal oesophagectomy and reconstruction of the gastric tube via the post-sternal route with cervical anastomosis by right thoracolaparotomy. One year after surgery, he presented with prolonged fever and dyspnoea. Chest computed tomography (CT) revealed right pleural effusion surrounded by thickened pleura, and he was diagnosed with empyema. He underwent chest tube drainage and was referred to our hospital. The inflammatory reaction did not improve despite antibiotic treatment and chest tube drainage. Therefore, pleural lavage was started, with a natural drip of 500 ml physiological saline via the chest tube. The patient coughed soon after starting the lavage and presented with deteriorating consciousness and paralysis on the left side with conjugate deviation to the right upper side. The Glasgow Coma Scale was E4V5M6 and the National Institute of Health Stroke Scale was 20. Since cerebral infarction was suspected, brain CT and magnetic resonance imaging (MRI) scans were performed immediately. Brain CT images showed air inflow in the territory of the right middle cerebral artery (Fig. 1). T2 star images showed a large amount of air inflow in the territory of the right middle cerebral artery (Fig. 2A). Brain MRI diffusion-weighted images showed a widespread high intensity in the right cerebrum (Fig. 2B). Soon after the MRI scan, he presented with a convulsion and lost consciousness. Tracheal intubation was performed and he was transferred to the intensive care unit. Therapeutic hypothermia was initiated using a cooling blanket and was maintained at 33°C under sufficient sedation for 24 h. Though the air had disappeared on brain CT 24 h after the onset, a widespread low-density area was observed in the territory of the right middle cerebral artery. Transthoracic echocardiography did not reveal a right-to-left shunt. Open-window thoracotomy and tracheotomy were performed on Day 15 after the stroke onset. Intermittent convulsions gradually disappeared, his level of consciousness improved, and light persistent paralysis on the left side improved completely with rehabilitation. Since the empyema cavity was purified, thoracoplasty was performed on Day 93. The patient was discharged from the hospital on Day 127.
Figure 1:
Brain CT image at the stroke onset shows air inflow in the territory of the right middle cerebral artery.
Figure 2:
(A) T2 star magnetic resonance image at the stroke onset shows a large amount of air inflow in the territory of the right middle cerebral artery. (B) Brain diffusion-weighted magnetic resonance image at the stroke onset shows a widespread high intensity in the territory of the right middle cerebral artery.
DISCUSSION
Air embolism occurs rarely, and there has been no previous report of cerebral air embolism during pleural lavage with saline for empyema, although 2 cases of cerebral air embolism have been reported during pleural lavage with a fibrinolytic agent [1].
Two mechanisms have been suggested for the occurrence of cerebral air embolism [1, 2]. Possible mechanisms for the influx of air into the systemic circulation include the following: first, communication between the bronchus, bronchiole or air space and pulmonary vein. Secondly, communication between the pulmonary vein and atmosphere. In addition, increases in airway pressure caused by a cough, the Valsalva manoeuvre, or positive pressure ventilation increases the risk of cerebral air embolism [2]. The mechanism in this case is considered to be that of the elevated intrapleural pressure due to lavage and coughing causing air to enter the peripheral pulmonary veins exposed on the surface of the empyema cavity.
Hyperbaric oxygen treatment has been reported as a useful treatment for air embolism [1, 2]. Hyperbaric oxygen treatment, in which the patient is placed under high air pressure, is effective in shrinking intravascular air bubbles. It has also been reported that hyperbaric oxygen treatment increases the partial pressure of oxygen in the blood, raising the amount of dissolved oxygen and increasing oxygen transport to tissues surrounding the site of infarction by mechanisms other than oxygen transport by haemoglobin, thus protecting nerve cells and preventing cerebral oedema.
In the present case, although many small air bubbles had spread widely in the territory of the right middle cerebral artery and had caused widespread cerebral infarction, the patient could leave the hospital without cerebral infarction sequelae. This indicates that therapeutic hypothermia might improve the neurological outcome of the patient. Therapeutic hypothermia is usually adopted to prevent post-resuscitation encephalopathy after cardiac arrest and neonatal hypoxic encephalopathy, as well as for cranial trauma, and it has been reported to have a cerebroprotective effect [3]. Schwab reported that surface cooling methods reduced brain oedema, leading to reduction in intracranial pressure after a stroke [4].
In the present case, air disappeared and a widespread low-density area was observed in the territory of the right middle cerebral artery on brain CT 24 h after the stroke onset. These findings indicate that ischaemia/reperfusion injury due to cerebral air embolism occurs in a short period, and neuroprotection during this period is critical. Theoretically, neuroprotection by therapeutic hypothermia was considered to be effective during the period of ischaemia/reperfusion injury in this case.
The mechanisms underlying the beneficial properties of hypothermia therapy are multifactorial and include reductions in the cerebral metabolism of glucose and oxygen consumption; pathways mediating the accumulation of excite-toxic neurotransmitters, intracellular acidosis and the influx of intracellular calcium and oxygen free radical production; alterations in the expression of cold shock proteins; reductions in brain oedema; minimizing the risk of thrombosis and reducing the risk of epileptic activities through electrical stabilizing properties [5].
In conclusion, a patient who developed severe cerebral air embolism during pleural lavage was treated with therapeutic hypothermia. In spite of the widespread cerebral infarction after the stroke onset, the patient could leave the hospital without cerebral infarction sequelae. Although neuroprotection by therapeutic hypothermia is considered to be effective during the period of ischaemia/reperfusion injury caused by cerebral air embolism, further evaluations are needed for confirmation.
Conflict of interest: none declared.
REFERENCES
- 1.Schneider F, Lion R, Kummerlen C, Ducrocq X, Tempé JD. Neurological complications and pleural lavage with a fibrinolytic agent. A two-case report. Intensive Care Med. 2000;26:995–7. doi: 10.1007/s001340051293. [DOI] [PubMed] [Google Scholar]
- 2.Um SJ, Lee SK, Yang DK, Son C, Kim KN, Lee KN, et al. Four cases of a cerebral air embolism complicating a percutaneous transthoracic needle biopsy. Korean J Radiol. 2009;10:81–4. doi: 10.3348/kjr.2009.10.1.81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bernard SA, Gray TW, Buist MD, Jones BM, Silvester W, Gutteridge G, et al. Treatment of comatose survivors of out-of-hospital cardiac arrest with induced hypothermia. N Engl J Med. 2002;346:557–63. doi: 10.1056/NEJMoa003289. [DOI] [PubMed] [Google Scholar]
- 4.Schwab S, Schwarz S, Spranger M, Keller E, Bertram M, Hacke W. Moderate hypothermia in the treatment of patients with severe middle cerebral artery infarction. Stroke. 1998;29:2461–6. doi: 10.1161/01.str.29.12.2461. [DOI] [PubMed] [Google Scholar]
- 5.Delhaye C, Mahmoudi M, Waksman R. Hypothermia therapy: neurological and cardiac benefits. J Am Coll Cardiol. 2012;59:197–210. doi: 10.1016/j.jacc.2011.06.077. [DOI] [PubMed] [Google Scholar]