Abstract
Introduction:Recent models of psychosis implicate stressful events in its etiology. However, while evidence has accumulated for childhood trauma, the role of adult life events has received less attention. Therefore, a review of the existing literature on the relationship between life events and onset of psychotic disorder/experiences is timely. Methods: A search was conducted using PsychInfo, Medline, Embase, and Web of Science to identify studies of life events and the onset of psychosis or psychotic experiences within the general population. Given previous methodological concerns, this review included a novel quality assessment tool and focused on findings from the most robust studies. A meta-analysis was performed on a subgroup of 13 studies. Results: Sixteen studies published between 1968 and 2012 were included. Of these, 14 reported positive associations between exposure to adult life events and subsequent onset of psychotic disorder/experiences. The meta-analysis yielded an overall weighted OR of 3.19 (95% CI 2.15–4.75). However, many studies were limited by small sample sizes and the use of checklist measures of life events, with no consideration of contextual influences on the meaning and interpretation of events. Conclusions: Few studies have assessed the role of adult life events in the onset of psychosis. There was some evidence that reported exposure to adult life events was associated with increased risk of psychotic disorder and subclinical psychotic experiences. However, the methodological quality of the majority of studies was low, which urges caution in interpreting the results and points toward a need for more methodologically robust studies.
Key words: psychosis, life events, review, stress, etiology
Introduction
Recent models of psychosis implicate social adversity, broadly defined, in its etiology.1,2 However, while evidence has accumulated for childhood trauma,3,4 the role of adult life events has received less attention. Life events are situations or occurrences that bring about a positive or negative change in personal circumstances and/or involve an element of threat (examples provided in onlinesupplementary material 1). As a basis for further research, it is important to evaluate existing research on life events and psychosis, both in terms of substantive findings and methodological issues. This review focuses on the impact of adult life events on risk of both onset of psychotic disorder and subclinical psychotic experiences in general population samples.
A recent review by Fallon5 evaluated studies that used semi-structured interview measures to assess exposure to life events in psychosis patients. Because the literature in this area is still fairly small, a more extensive, systematic, and updated review of the literature was considered to be the most appropriate strategy to better understand the association between adult life events and psychosis. Given previous concerns about the methodological quality of studies of life events and psychosis,5 a quality assessment tool was devised to evaluate the selected studies. This review focuses on the most robust studies.
Methods
A systematic search of relevant databases was conducted using predefined search terms (see onlinesupplementary material 2). Studies were included if (a) they assessed life events in adulthood, (b) the individuals were over 16 years, (c) the individuals had a first episode of psychosis or subclinical psychotic experiences, and (d) they were published in English in peer-reviewed journals. Studies were excluded if (a) they assessed childhood events only and (b) no distinction was made between childhood and adulthood in timing of exposure. Adulthood was defined as aged 17 years. Each study was assessed using a quality assessment tool (see onlinesupplementary material 3). A cutoff score of at least 10 out of 14 (over 70%) was chosen to select the more “methodologically robust” studies. Although this may be arbitrary and risks leaving out any study that scores high on some and low on other criteria, it does ensure consideration of only the most consistently robust studies.
Results
Sixteen studies published between 1968 and 2012 met the inclusion criteria (supplementary material 4), a surprisingly small number. Eleven were studies of clinical samples (6 of first-episode cases and 5 of mixed first- and non-first-episode cases) and 5 of general population samples (tables 1–3). Fourteen studies reported a positive association between adult life events and onset of psychotic disorder or occurrence of subclinical experiences. Within the clinical studies, cases with psychosis were over 2 times6 to 8 times7 more likely to report life events compared with controls in the period leading up to onset. In the general population studies, those with psychotic experiences (vs those without) were between 2 times8 and 7 times9 more likely to report recent life events.
Table 1.
Studies Investigating the Associations Between Adult Life Events and Psychosis in First-Episode Samples
| Authors, Location | Design | Sample | Measure of Life Events | Life Events Period | Measure of Psychosis | Main Findings | Quality Score |
|---|---|---|---|---|---|---|---|
| Day et al (1987),21 WHO international study | Within-patient | 386 cases with psychosis | WHO Life Events Schedule (WHO LES 1978, unpublished) | 3 months prior to onset of psychosis | ICD-9 diagnoses (including PSE and CATEGO, where possible) | Number of patients reporting life events 3 months prior to onset ranged from 21% to 87% | 9 |
| Gureje and Adewunmi (1988),10 Nigeria | Case-control | 42 cases with psychosis and 50 population controls | Paykel’s life events checklist (Paykel et al 1969) | 6 months prior to onset (cases) or interview (controls) | Research Diagnostic Criteria (Spitzer et al 1975) for schizophrenia | Life event 1 month prior to onset/interview: cases: 7%, controls: 24% (χ 2 = 8.26, P < .01) | 10 |
| Chakraborty et al (2007),22 India | Between-patient | 18 cases with acute and transient psychotic disorder, and 20 control patients with mania | Presumptive Stressful Life Events Scale (Singh et al 1984) | Lifetime and within 6 months prior to onset (cases) or interview (manic patients) | Consensus decision and ICD-10 criteria | Mean number of negative life events 2 weeks prior to onset/interview: cases: 0.72 (SD 0.95), manic patients: 0.20 (SD 0.52) (U = 110.0, P = .013) | 7 |
| Faravelli et al (2007),11 Italy | Case-control | 9 cases with psychosis and 123 population controls | LEDS (Brown and Harris, 1989)23 | 1 year prior to onset (cases) or interview (controls) | Florence Psychiatric Interview (Faravelli et al 2001), which produced Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV) diagnoses | Severe life events 1 year prior to onset/interview: cases: 3 (33%), controls: 15 (12%) (OR 3.2, 95% CI 0.7–15.5, not significant) | 10 |
| Raune et al (2009),6 United Kingdom | Within-patient cluster design (with case-control comparisons) | 41cases with psychosis and 548 population controls | LEDS | 1 year prior to onset (cases) or interview (controls) | ICD-10 diagnosis of psychosis (from SCAN) | Moderate to severe independent life event 3 months prior to onset: cases: 14 (34.1%), controls: 42 (13.5%) (OR = 5.0, 95% CI 2.4–10.7) | 11 |
| Mondelli et al (2010),18 United Kingdom | Case-control | 50 cases with psychosis and 36 population controls | Brief Life Events Questionnaire (Brugha and Cragg, 1990) | 6 months prior to onset (cases) or interview (controls) | ICD-10 and DSM-IV criteria for psychosis using the Operational Criteria (OPCRIT) (McGuffin et al 1991) | Number of life events in previous 6 months: cases: 2.3 (SD 0.3), controls: 0.7 (SD 0.2) (t = −4.8, df (1, 81), P < .001) | 5 |
Note: CATEGO, Categorical assessment of psychiatric disorder; ICD, International Classification of Diseases; PSE, Present State Examination; LEDS, Life Events and Difficulties Schedule; SCAN, Schedules for Clinical Assessment in Neuropsychiatry.
Table 3.
Studies Investigating the Associations Between Adult Life Events and Psychosis Experiences in General Population Samples
| Authors, Location | Design | Sample | Measure of Life Events | Life Events Period | Measure of Psychotic Experiences | Main Findings | Quality Score |
|---|---|---|---|---|---|---|---|
| Vinokur and Selzer (1975),24 United States | Cross sectional | 1059 male subjects | Social Readjustment Rating Scale (Holmes & Rahe 1967) | 1 year prior to interview | Paranoid thinking assessed using a self-report questionnaire | Positive correlation between life events and self-reported paranoid thinking (r = .33, P < .01) | 2 |
| Johns et al (2004),8 United Kingdom | Cross sectional | Random sample of 8520 adults. 478 (5.5%) reported >1 psychotic symptoms in the past year | LTE | 6 months prior to interview | Psychosis Screening Questionnaire (PSQ; Bebbington and Nayani 1995) | Life event in past 6 months: yes: 2136 (25%), no: 6384 (75%) (OR 2.20, 95% CI 1.82–2.66, P < .001) | 9 |
| Jenkins et al (2010),9 Tanzania | Cross sectional | Random sample of 899 adults. 35 (3.9%) reported >1 psychotic symptoms in the past year | Life events checklist, based on the LTE (Jenkins et al 1997 a/b) | 6 months prior to interview | PSQ | 2 or more life events in past 6 months: yes: 117 (13%), no: 782 (87%) (OR 7.45, 95% CI 3.42–16.21, P < .001) | 9 |
| van Nierop et al (2012),20 the Netherlands | Cross sectional | Random sample of 6646 adults. 1078 (16%) endorsed >1 lifetime psychotic experience | LTE | 1 year prior to interview | Composite International Diagnostic Interview (CIDI; Kessler and Ustun 2004) | Negative life events in past year: psychotic experiences group: 249 (66%), controls: 2541 (48%) (RR 2.07, 95% CI 1.66–2.57, P < .001) | 7 |
| Lataster et al (2012),15 the Netherlands | Cross sectional | Random sample of 1722 young adults. 170 (9.9%) endorsed >1 lifetime psychotic experience | Munich Interview for the Assessment of Life Events and Conditions (MEL; Maier-Diewald et al 1983) | An average of 3.6 years prior to interview | CIDI | Mean number of negative life events: psychotic experiences group: 7.49, controls: 5.98 (t = −4.17, df (1, 1720), P < .001) | 12 |
Note: RR, relative risk.
Table 2.
Studies Investigating the Associations Between Adult Life Events and Psychosis in Mixed Onset and Relapse Samples
| Authors, Location | Design | Sample | Measure of Life Events | Life Events Period | Measure of Psychosis | Main Findings | Quality Score |
|---|---|---|---|---|---|---|---|
| Brown and Birley (1968),12 United Kingdom | Case-control | 50 cases with psychosis and 325 population controls | Early version of the Life Events and Difficulties Schedule (LEDS) | 13 weeks before onset (cases) or interview (controls) | Present State Examination (PSE; Wing et al 1967) | Independent life event in 3 weeks pre-onset or interview: cases: 46%, controls: 14% (P < .001). | 11 |
| Canton and Fraccon (1985),7 Italy | Case-control | 54 cases with schizophrenia, recent onset (n = 24), chronic (n = 30), and 54 control subjects | Paykel’s Interview for Recent Life Events (Paykel and Mangen 1980) | 6 months preceding hospital admission (cases) or interview (controls) | Diagnostic and Statistical Manual of Mental Disorders, Third Edition (DSM-III) diagnosis of schizophrenia | Exposure to >2 life events 6 months prior to psychosis/interview: cases: 33 (61%), controls: 4 (7%) (P < .001). | 9 |
| Al Khani et al (1986),19 Saudi Arabia | Case-control | 48 cases with schizophrenia, first episode (n = 21), previous episodes (n = 27), and 62 population controls | WHO LES | 1 year prior to onset/relapse (cases) and interview (controls) | Arabic version of PSE and Categorical assessment of psychiatric disorder (CATEGO) | Life event in 6 months prior to psychotic episode/interview: cases: 88%, controls: 71% (not significant; precise P not reported) | 9 |
| Dohrenwend et al (1987),13 United States | Case-control | 66 cases with schizophrenic disorder (21 first onset) and 197 population controls | Psychiatric Epidemiology Research Interview (PERI; Dohrenwend et al 1978) | 1 year prior to onset/relapse (cases) and interview (controls) | DSM-III diagnoses | Mean number of “non-fateful” life event in 1 year prior to psychotic episode/interview: cases: 0.89; controls: 0.25 (P < .001) | 12 |
| Bebbington et al (1993),14 United Kingdom | Case-control | 97 cases with psychosis and 207 population controls | LEDS | 6 months prior to onset (cases) or interview (controls) | DSM-III diagnoses | Severe life events 3 months prior to onset/interview: cases: 27 (52%), controls: 21 (10%) (χ 2 = 69.05, P < .001) | 12 |
The picture is the same when only those studies6,10–15 that received a quality score of 10 or above (n = 7) are considered, ie, 6 studies6,11–15 reported some evidence that the number and/or severity of events was associated with around a 3- to 5-fold increased risk of psychosis.
Timing
The majority of these more robust studies found life events were elevated prior to onset of psychosis, with the time period under consideration ranging between 3 months12 and 3.6 years.15 The seminal article of Brown and Birley,12 eg, found life events were increased in the 3-week period pre-onset of psychotic symptoms. The sample, however, was small (n = 50, 13 of whom were non-first-episode), and no subsequent studies have reported similar findings. Later studies suggest that life events may exert their influence over a longer period. For example, 2 studies11,13 of disorder found life events were around 2–3 times higher in cases compared with controls across a 1-year period. Further, a general population study15 of 1722 young adults found that exposure to life events over the previous 3 years was associated with an increased risk of psychotic experiences.
Severity and Type
Some studies assessed other contextual elements of events, such as their severity and type. In a study of 97 cases (35 first episode) and 207 controls, Bebbington et al14 found that moderate and severe life events (vs mild) were higher in the 3-month period pre-onset in patients with schizophrenia (ie, 52% cases with moderate/severe events vs 10% controls).
More specifically, using a sample of 41 first-onset patients, Raune et al6 found that intrusive events, such as a physical assault or invasive operation, were more likely to be associated with an increased risk of psychosis and were most common in the 3 months pre-onset (ie, 34% cases vs 3% controls). However, for these analyses, the control sample was taken from 2 studies16,17 conducted 20 years previously.
Others have found evidence for specific effects for certain types of events. Dohrenwend et al,13 eg, in a sample of 66 schizophrenia cases (21 first onset) and 197 population-based controls, found physical illness and injury (akin to intrusive events) were around 2 times more common in cases than controls.
Independence of Events
One way of clarifying the causal relationship between events and onset is to distinguish events that are independent of emerging symptoms, eg, death of a close relative, from those which may be influenced by mental state, eg, interpersonal conflict.
Five of the more robust studies6,11–14 distinguished between possibly dependent and independent events. For example, Brown and Birley12 found 46% of cases were exposed to recent independent events compared with 14% of controls. More recent research suggests similar conclusions.6,11,14 Raune et al,6 eg, found that almost all cases (95%) experienced a life event 1 year prior to the development of symptoms, and that in 76%, these event(s) were independent. These authors also found that cases were 2 times more likely to report independent life events in the 3 months pre-onset than controls (34% cases vs 14% controls).
In contrast, Dohrenwend et al13 did not find any increase in independent events prior to onset. However, they did find a higher number of “non-fateful” events (a similar concept to dependent events, ie, events that are influenced by prior mental state and personality characteristics, such as relationship difficulties) in the year prior to onset.
Meta-analysis
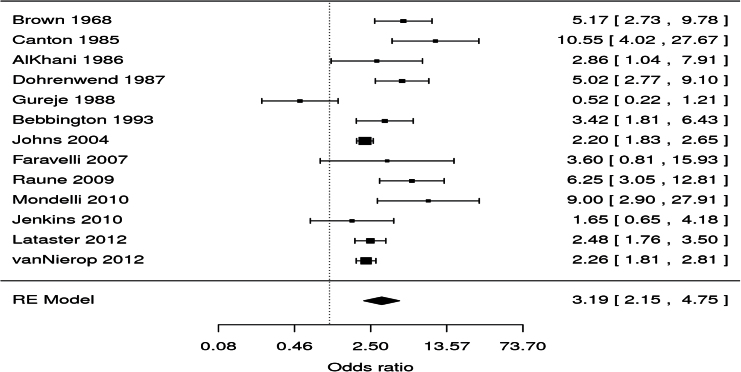
Additionally, we carried out a meta-analysis of a subset of 13 studies in which the number exposed and not exposed to life events had been reported7–9,10,11–15,18–20 (see onlinesupplementary material 5 for more detail).
The meta-analysis yielded an overall weighted OR of 3.19 (95% CI 2.15–4.75), which suggests that individuals with psychotic disorder/experiences are roughly 3 times more likely than controls to be exposed to recent life events (figure 1). The OR from the clinical samples6–8,10–14,18,19 are higher than the general population studies,9,15,20 but this was not statistically significant. There is substantial heterogeneity between studies (Higgins’ I 2 = 87.27% [95% CI 70.34%–96.36%]). The heterogeneity was not removed by meta-regression using any of the 4 possible moderators (year of publication, life events period, quality score, and type of sample, ie, clinical or general population), possibly due to rather restricted variability on all of them.
Fig. 1.
Forest plot for the meta-analysis examining the overall association between recent life events and psychosis.
Methodological Issues
Across all studies, there were a number of common methodological issues that merit specific consideration. First, the majority of studies were cross sectional, introducing potential recall bias and limiting inferences concerning direction of causation. In relation to psychotic disorder, it is difficult to envisage longitudinal studies being feasible, given the low incidence of disorders. Consequently, efforts to minimize recall bias and carefully date exposure to events and onset of disorder are essential but were rarely made.
Further, not all the studies in this review included a comparison group, and, of the 10 that did,6,7,10–14,18,19,22 not all drew controls from the same populations as cases. Bias in selection of comparison group(s), therefore, cannot be excluded.
Within the clinical studies, causal interpretations are limited by the small number of first-episode only samples and by the failure of papers based on mixed samples to report findings specifically for first-episode cases. This noted, both types of study in the main reported positive associations. It is clear that more first-episode studies are needed, which utilize appropriate control groups and objective ratings of the impact of events.
Differences in life events measurement make comparisons between studies difficult and this may account for some of the variations in findings. Instruments to assess life events generally fall into 2 categories: checklist or semi-structured interview. The Life Events and Difficulties Schedule23 (LEDS) is considered the gold standard as it takes account of context, eg, timing, severity, and independence of events. It is, however, time consuming to administer and rate. Of the studies reviewed, 4 used checklists8,9,20,24, 2 used a checklist that was interviewer administered10,18, and 10 used semi-structured interviews,6,7,11–15,19,21,22 of which 46,11,12,14 used the LEDS.23 Of these latter studies, 3 studies6,12,14 found positive associations between recent life events and psychosis onset.
Where the severity of life events was evaluated, this was mainly determined using objective criteria and not based on subjective appraisals. This is because subjective perceptions of severity may be affected by mood and mental state, which would then risk confusing exposure and outcome and make it impossible to distinguish cause and effect.
Although most of the assessments of life events used in the reviewed studies do enquire about positive events, only one of the studies drew a distinction between positive (desirable) and negative (undesirable) events in their analyses,22 finding associations only for negative events and psychosis. No study specifically discussed the valence of events in relation to psychosis onset.
Finally, adjustment for potential confounders was inconsistent. Where adjustments were made, the majority controlled for age, gender, and ethnicity, with some controlling for a wider range of factors, such as urbanicity, education, IQ, substance use, comorbid neurosis,8 and past year cannabis use.9 No study adjusted for childhood adversity.
Discussion
There were 3 main findings: (a) the literature on adult life events and psychosis onset is surprisingly small (only 16 studies spread over 44 years); (b) most studies suggest the number of events prior to onset is higher (compared with a comparison group) in those with psychosis or psychotic experiences, with our meta-analysis suggesting around a 3-fold increased odds of life events in the period prior to psychosis onset; and (c) more tentatively, there are some indications that intrusive events may be particularly relevant to the development of psychosis. These findings noted that much of the existing research is methodologically limited, and this necessarily urges caution in drawing any inferences about the etiological role of life events in psychosis.
Life Events and Psychosis
Interest in the role of life events in the onset of psychosis has fluctuated in the time since Brown and Birley’s seminal study.12 In recent years, there has been a resurgence of interest in the role of social factors in psychosis etiology. Within this context, it is important to revisit the question of whether exposure to proximal stressors (ie, life events) increases risk of psychosis. The literature is suggestive but too weak to permit firm conclusions.
The suggestion that life events may increase risk is nonetheless strengthened by the emergence of plausible mechanisms that may account for how exposure to external stressors can impact on individuals in ways that increase risk for psychosis. For example, drawing from cognitive models of psychosis, it is possible that exposure to, say, threatening and intrusive events influence how individuals appraise their social worlds, perhaps leading to hostile perceptions of the external world.1 Repeated exposure may contribute to pushing some along a continuum from suspiciousness to paranoia to persecutory delusions. More biologically, there is now evidence of hypothalamic-pituitary-adrenal (HPA) axis dysregulation in psychosis. Stress-induced dysregulation of the HPA axis may subsequently give rise to increased dopamine receptor densities and dopamine release,25 mirroring dopaminergic abnormalities commonly thought to be present in psychosis. The association between adult life events and psychosis may also be influenced by genetic susceptibility, be it as a result of an underlying variation in DNA sequence or because of epigenetic variation in gene expression.
In sum, there is evidence to suggest adult life events may be relevant to the onset of psychosis for some, and there are plausible mechanisms through which such exposures may work. However, the existing literature is disparate and methodologically weak. To more fully understand the nature of the link, if any, between life events and psychosis, there is a need for a new generation of studies that pay close attention to careful assessment of events, that include robust comparison groups, and that seek to minimize the inherent recall and selection biases. Exposure and responses to life events are potentially modifiable, and a better understanding of how they impact on risk of psychosis may inform strategies for prevention and early intervention.
Supplementary Material
Supplementary material is available at http://schizophre niabulletin.oxfordjournals.org.
Funding
Wellcome Trust (WT087417); the European Union (European Community’s Seventh Framework Program [HEALTH-F2-2009–241909]: Project EU-GEI); and the UK Department of Health via the National Institute for Health Research (NIHR) Specialist Biomedical Research Centre for Mental Health award to the South London and Maudsley NHS Foundation Trust (SLaM) and the Institute of Psychiatry, King’s College London. Economic and Social Research Council PhD studentship (to S.B.); UK Medical Research Council Population Health Scientist award (G1002366 to H.L.F.).
Supplementary Material
Acknowledgments
We would like to thank Professors Paul Bebbington, Bruce Dohrenwend, Tom Craig, and Inez Myin-Germeys for their assistance with searching for additional studies. We also thank Assistant Professor Johan Lataster for providing additional data and clarification. All authors declare that they have no conflicts of interest in relation to the subject of this study.
References
- 1. Garety PA, Kuipers E, Fowler D, Freeman D, Bebbington PE. A cognitive model of the positive symptoms of psychosis. Psychol Med. 2001;31:189–195 [DOI] [PubMed] [Google Scholar]
- 2. Selten JP, Cantor-Graae E. Social defeat: risk factor for schizophrenia? Br J Psychiatry. 2005;187:101–102 [DOI] [PubMed] [Google Scholar]
- 3. Morgan C, Fisher H. Environment and schizophrenia: environmental factors in schizophrenia: childhood trauma—a critical review. Schizophr Bull. 2007;33:3–10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Varese F, Smeets F, Drukker M, et al. Childhood adversities increase the risk of psychosis: a meta-analysis of patient-control, prospective- and cross-sectional cohort studies. Schizophr Bull. 2012;38:661–671 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Fallon P. Life events; their role in onset and relapse in psychosis, research utilizing semi-structured interview methods: a literature review. J Psychiatr Ment Health Nurs. 2008;15:386–392 [DOI] [PubMed] [Google Scholar]
- 6. Raune D, Kuipers E, Bebbington P. Stressful and intrusive life events preceding first episode psychosis. Epidemiol Psichiatr Soc. 2009;18:221–228 [PubMed] [Google Scholar]
- 7. Canton G, Fraccon IG. Life events and schizophrenia. A replication. Acta Psychiatr Scand. 1985;71:211–216 [DOI] [PubMed] [Google Scholar]
- 8. Johns LC, Cannon M, Singleton N, et al. Prevalence and correlates of self-reported psychotic symptoms in the British population. Br J Psychiatry. 2004;185:298–305 [DOI] [PubMed] [Google Scholar]
- 9. Jenkins R, Mbatia J, Singleton N, White B. Prevalence of psychotic symptoms and their risk factors in urban Tanzania. Int J Environ Res Public Health. 2010;7:2514–2525 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Gureje O, Adewunmi A. Life events and schizophrenia in Nigerians. A controlled investigation. Br J Psychiatry. 1988;153:367–375 [DOI] [PubMed] [Google Scholar]
- 11. Faravelli C, Catena M, Scarpato A, Ricca V. Epidemiology of life events: life events and psychiatric disorders in the Sesto Fiorentino study. Psychother Psychosom. 2007;76:361–368 [DOI] [PubMed] [Google Scholar]
- 12. Brown GW, Birley JL. Crises and life changes and the onset of schizophrenia. J Health Soc Behav. 1968;9:203–214 [PubMed] [Google Scholar]
- 13. Dohrenwend BP, Levav I, Shrout PE, Link BG, Skodol AE, Martin JL. Life stress and psychopathology: progress on research begun with Barbara Snell Dohrenwend. Am J Community Psychol. 1987;15:677–715 [DOI] [PubMed] [Google Scholar]
- 14. Bebbington P, Wilkins S, Jones P, et al. Life events and psychosis. Initial results from the Camberwell Collaborative Psychosis Study. Br J Psychiatry. 1993;162:72–79 [DOI] [PubMed] [Google Scholar]
- 15. Lataster J, Myin-Germeys I, Lieb R, Wittchen HU, van Os J. Adversity and psychosis: a 10-year prospective study investigating synergism between early and recent adversity in psychosis. Acta Psychiatr Scand. 2012;125:388–399 [DOI] [PubMed] [Google Scholar]
- 16. Bebbington PE, Tennant C, Hurry J. Adversity and the nature of psychiatric disorder in the community. J Affect Disord. 1981;3:345–366 [DOI] [PubMed] [Google Scholar]
- 17. Harris T. Recent developments in the study of life events in relation to psychiatric and physical disorders.In: Cooper B, ed. Psychiatric Epidemiology. London: England: Croom-Helm; 1987. 81–103 [Google Scholar]
- 18. Mondelli V, Dazzan P, Hepgul N, et al. Abnormal cortisol levels during the day and cortisol awakening response in first-episode psychosis: the role of stress and of antipsychotic treatment. Schizophr Res. 2010;116:234–242 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Al Khani MA, Bebbington PE, Watson JP, House F. Life events and schizophrenia: a Saudi Arabian Study. Br J Psychiatry. 1986;148:12–22 [DOI] [PubMed] [Google Scholar]
- 20. van Nierop M, van Os J, Gunther N, et al. Phenotypically continuous with clinical psychosis, discontinuous in need for care: evidence for an extended psychosis phenotype. Schizophr Bull. 2012;38:231–238 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Day R, Nielsen JA, Korten A, et al. Stressful life events preceding the acute onset of schizophrenia: a cross-national study from the World Health Organization. Cult Med Psychiatry. 1987;11:123–205 [DOI] [PubMed] [Google Scholar]
- 22. Chakraborty R, Chatterjee A, Choudhary S, Singh AR, Chakraborty PK. Life events in acute and transient psychosis—a comparison with mania. . Ger J Psychiatry. 2007;10:36–40 [Google Scholar]
- 23. Brown GW, Harris TO. Life Events and Illness. New York: NY: Guilford Press; 1989 [Google Scholar]
- 24. Vinokur A, Selzer ML. Desirable versus undesirable life events: their relationship to stress and mental distress. J Pers Soc Psychol. 1975;32:329–337 [DOI] [PubMed] [Google Scholar]
- 25. Walker EF, Diforio D. Schizophrenia: a neural diathesis-stress model. Psychol Rev. 1997;104:667–685 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.