Abstract
Recruiting research participants based on genetic information generated about them in a prior study is a potentially powerful way to study the functional significance of human genetic variation. However, it also presents significant ethical challenges that, to date, have received only minimal consideration. We convened a multi-disciplinary workshop to discuss key issues relevant to the conduct and oversight of genotype-driven recruitment and to translate those considerations into practical policy recommendations. Workshop participants were invited from around the U.S., and included genomic researchers and study coordinators, research participants, clinicians, bioethics scholars, experts in human research protections, and government representatives. Discussion was directed by experienced facilitators and informed by empirical data collected in a national survey of IRB chairs and in-depth interviews with research participants in studies where genotype-driven recontact occurred. A high degree of consensus was attained on the resulting 7 recommendations, which cover informed consent disclosures and choices, the process for how and by whom participants are recontacted, the disclosure of individual genetic research results, and the importance of tailoring approaches based on specific contextual factors. These recommendations are intended to represent a balanced approach—protecting research participants, yet avoiding overly restrictive policies that hinder advancement on important scientific questions.
Keywords: Ethics, research recruitment, informed consent, disclosure of research results, human genetic variation
Introduction
Translating advances in genomics into robust knowledge about the structure and function of the human genome represents an unprecedented opportunity for understanding health and disease (Green and Guyer 2011). Genotype-driven research recruitment is a potentially powerful tool for facilitating this translation (McGuire and McGuire 2008). Using this approach, investigators search genomic data generated about participants in an existing study population to identify those who possess a gene variant of interest, and then contact them to invite their participation in further research to better understand the functional significance of that variant (Beskow et al. 2010).
This kind of “recruitment by genotype” eliminates the expensive and time-consuming step of screening new populations to find individuals who have the variant of interest (Chulada et al. 2008). However, it also presents ethical challenges. When genetic information generated in one study is used as the basis for identifying and contacting participants about further research, concerns more commonly associated with participation in genetic research are shifted to the recruitment phase (Beskow et al. 2010). A central issue is the disclosure to research participants of their individual genetic results from the first study as part of the recruitment process for the second. There is a fundamental tension between disclosing genetic research results that may be unwanted and/or preliminary and easily misinterpreted, and leaving prospective participants uninformed about the purposes of the second study and why they are eligible to participate (Beskow et al. 2010).
To date, there has been only minimal consideration of the ethical issues associated with recontacting participants for the purpose of additional research recruitment and with genotype-driven recruitment in particular. We therefore convened a multi-disciplinary workshop to formulate recommendations to help investigators and institutional review boards (IRBs) identify balanced approaches—those that protect research participants, yet avoid overly restrictive policies that limit opportunities for those who would like to participate and that hinder advancement on important scientific questions.
Workshop Overview
We held a 1.5-day workshop in May 2011 at Duke University to discuss key issues relevant to the conduct and oversight of genotype-driven recruitment and to translate those considerations into practical policy recommendations. This discussion was informed by empirical data collected through a national survey of IRB chairs (Beskow et al. in press) and in-depth interviews with research participants in six studies where genotype-driven recontact occurred (Beskow et al. 2011; Cadigan et al. 2011; Namey and Beskow 2011; Tabor et al. 2011). A wide range of stakeholders were represented at the workshop, including researchers, study coordinators, and participants from the six studies, as well as bioethics scholars, IRB leaders, other genomic and biobank researchers, clinicians, and federal officials engaged in issues related to human subjects research (see Acknowledgements).
The workshop began with brief presentations of the empirical data, followed by discussions aimed at initiating reflection on four major topics (Table 1). We had identified and outlined these topics in a framing document that was circulated prior to the workshop. Each topic discussion started with a diverse panel of workshop participants (e.g., a researcher, clinician, IRB member, and research participant), who commented briefly on the topic from their perspective. These comments were followed by large-group discussion directed by experienced facilitators. The second day began with a synthesis of the first day's discussion, followed by further discussion of the major topics. We returned to points of potential disagreement with the aim of reaching consensus among a majority of the group. Discussion continued on each topic until no disagreement was voiced in response to facilitators' summary of the group's position (including minority opinions where applicable).
Table 1. Workshop Discussion Framework.
| Topic Area | Overarching Discussion Question | Primary Ethical Concerns |
|---|---|---|
| 1. Recruitment for Additional Genetic Research (“Recontact”) | When is it acceptable or not acceptable to recontact genetic research participants for recruitment into additional genetic research? |
|
|
| ||
| 2. Disclosure of Results in the Process of Genotype Driven Recruitment | When is it acceptable or not acceptable to disclose individual genetic research results from the first study during the process of genotype-driven recruitment for further research? |
|
|
| ||
| 3. Identifying Best Practices for the Process of Genotype-Driven Recruitment | Moving forward, what approaches to genotype-driven recruitment are optimal to respect and protect participants, minimize ethical dilemmas, and facilitate recruitment into beneficial research? |
|
|
| ||
| 4. Genotype-Driven Recruitment: Special Complexities | How does genotype-driven recruitment either attenuate or amplify obligations to return genetic research results? |
|
The discussion was documented through audio-recording and detailed note-taking for use in preparing this report. We invited all workshop participants to comment on an early draft, and later circulated a revised version with a request for participants to let us know whether they generally agreed with the recommendations. One participant was constrained from expressing a formal opinion due to her governmental position; among the 36 remaining participants, 33 affirmed their agreement.
Recommendations
Recommendation 1. Researchers should disclose the possibility of future contact for further research recruitment during the informed consent process for the initial study
Contact for the purpose of recruitment to additional research will occur with increasing frequency, even in cases where researchers do not necessarily anticipate such contact.
For prospective participants, advance notice about this possibility is a demonstration of respect; for some, such disclosures may be important to inform their decision about current research participation (Beskow et al. 2011). Although studies have found that participants often do not remember information disclosed during the consent process (Prentice et al. 2007) poor recall is a separate issue that is not unique to genotype-driven recruitment. It should be addressed in other ways, rather than serving as a justification for not providing appropriate disclosures. When genotype-driven recruitment is specifically anticipated, it is a good idea to communicate this to prospective participants in simple language; otherwise, somewhat less detailed disclosures about the bases for future research recruitment may suffice (Box 1).
In the case of currently existing consent forms, silence regarding the possibility of recontact for the purpose of research recruitment should not automatically rule out such contact. Contacting individuals without advance notice to ask about their interest in further research participation may be contrary to their preferences, but does not necessarily result in harm (Beskow et al. 2006). They can choose to not respond, express disinterest at the outset, or learn more about the research and then decide whether to take part (Beskow et al. 2004). Thus, although up front disclosure about future research contact is highly preferable, lack of such disclosure during the consent process for already ongoing research should not inevitably foreclose the possibility (Beskow et al. in press).
Consent forms that directly state or imply that contact for recruitment will not occur are more concerning. These kinds of statements should be avoided unless there is a specific reason to include them, e.g., in situations where researchers are willing to rule out future contact and making this promise aids recruitment. Workshop participants agreed that, when such statements have been included, there should be a strong presumption they will be honored. A minority felt that further contact might still be permitted in limited situations, based on compelling scientific justification and the use of a carefully designed approach.
Recommendation 2. Researchers should consider offering participants a choice at the time of initial consent about future contact for further research recruitment
Giving participants a choice about whether researchers can contact them for recruitment to additional research is not ethically required. For some studies, contact about additional research is central to the research design and thus cannot be optional. However, when feasible to do so, offering a choice at the time of initial consent would enable prospective participants who do not want such contact to opt out and yet still participate in the immediate study (Beskow et al. 2011).
Several ethical and logistical concerns have been raised about offering choices on consent forms in general (Ram 2008), including whether participants can be given enough information to make an informed selection at the time of initial consent (Beskow and Burke 2010). However, willingness to be contacted about future research can be presented as a simple binary (yes/no) choice about which we believe participants can be given enough information—assuming that the options and their implications are adequately explained.
If choices about future research contact are offered during the initial consent process, systems must be in place to ensure that each participant's decisions are tracked and honored (http://biospecimens.cancer.gov/bestpractices/2011-NCIBestPractices.pdf). If choices are not offered, researchers should be prepared to follow wishes that are expressed later, e.g., if a participant responds to contact about additional research by stating the desire to opt-out of any more contact.
Recommendation 3. Contact about additional research should be made by a person or entity known to the participant
Genotype-driven recruitment could be undertaken by investigators who want to recontact selected participants in their own studies about additional research (Beskow et al. 2010). However, investigators other than those who originally interacted with the participants may also seek to use genotype-driven recontact.
Prospective participants should not be left wondering how investigators obtained information about them (Beskow et al. 2004). It is therefore preferable that initial contact about further research be made by a trusted intermediary—either the original research team or the entity through which the person was originally recruited.
We recognize that this recommendation would pose non-trivial challenges if genotype-driven recruitment was permitted based on searches across multiple data sets stored in centralized repositories (such as the National Institutes of Health's database of Genotypes and Phenotypes, dbGaP (http://gwas.nih.gov/02dr2.html). McGuire and McGuire (2008) have suggested that using data shared through centralized repositories for such recruitment could maximize the utility of the massive amounts of information generated in genomic studies. Our recommendation, however, would not create additional barriers given that database users currently have no access to identifying information without working through the original investigators. Even if these databases were re-structured to allow more direct access (a topic not discussed at our workshop), close control and monitoring of recontacts would be vital to promote participant trust and long-term sustainability. At a minimum, recontact must include a clear explanation of how and where those conducting the new study obtained prospective participants' names—ideally referencing a source that is readily recognizable to participants. This process would be vastly enhanced by comprehensive efforts to educate research participants and the public about large-scale data sharing.
Recommendation 4. The process for contacting participants about additional research should be designed based on a range of considerations related to the research team and study question
The logistical process by which participants are contacted about additional research should be designed based on a range of contextual considerations. Factors that might warrant a more cautious approach include:
Research conducted by different investigators than those who originally interacted with participants;
Research focused on a different medical condition than the one for which participants were originally recruited; and/or
Research focused on a potentially sensitive or stigmatizing issue (even if this issue is the same as that originally under study, some participants may be averse to being asked repeatedly, or by different investigators, about a difficult subject).
These factors do not necessarily preclude recontact, but may favor a more conservative process, such as requiring an opt-in approach (i.e., the research team talks about the study with only those people who, in response to an initial letter, opt in to learning more) rather than allowing an opt-out approach (i.e., the research team follows up with all prospective participants except those who respond to an initial letter by opting out of further communication).
One situation that may preclude contact about additional research is that in which individuals who are eligible for a genotype-driven study never provided informed consent for genomic research. For example, research using biospecimens left over from a clinical procedure sometimes proceeds based on the protocol being exempt from human subjects regulations or with a waiver of the requirement to obtain informed consent (45 CFR §46.101(b)(4), 45 CFR §46.116(d)).
Workshop participants agreed that contacting individuals who may have no awareness of having been involved in research, based on something learned from that research, is fraught with difficulty. It may be perceived as an invasion of privacy and undermine trust in research and in the health care entity that collected the specimens. A minority, however, felt that such contact may be acceptable in rare cases. Moving forward with genotype-driven recruitment in such circumstances would require thorough consideration of the importance of the scientific questions and the unique nature of the study population, as well as the development and close oversight of an exacting approach.
It is important to distinguish between ‘never having provided informed consent’ and much current biobanking research where participants do provide informed consent for the storage and research use of their biospecimens and data (even though they do not provide specific consent for each subsequent use of their stored materials). In the latter instance, individuals can be informed during the initial consent process about the possibility of future contact.
Recommendation 5. Thresholds established for the return of individual genetic research results in general should not be used for decision-making about return of results in the context of genotype-driven recruitment
The general topic of return of individual results to participants in genomic research is the subject of vigorous ongoing debate. Opinions range widely from the view that such results should seldom if ever be offered (Meltzer 2006; Miller et al. 2008; Parker 2006) to the view that they should be offered routinely (Fernandez 2008; Kohane and Taylor 2010; Shalowitz and Miller 2005). National entities have issued guidelines placing the bar for disclosure at clinical validity and utility (Fabsitz et al. 2010; NBAC 1999), i.e., results should be offered only when a proven therapeutic or preventive intervention is available. Many consent forms for genomic research contain statements either conforming to this high bar or simply noting that no individual results will be returned.
Decisions about return of results in the context of genotype-driven recruitment should not be bound by these kinds of consent disclosures. Such statements reflect thresholds established for offering research results for the participant's personal or health-related benefit. In contrast, offering individual results during the process of genotype-driven recruitment is motivated by the need to ethically achieve a scientific goal. These are fundamentally different objectives.
Clinical validity and utility is a standard that would rarely be met in the context of genotype-driven recruitment, where further research is needed specifically because more must be learned to decipher the meaning of genetic research results in terms of risk, inheritance, diagnosis, prognosis, and treatment (Beskow et al. 2010). If this threshold were automatically applied, it would nearly always result in the need to obfuscate the purpose of the follow-up study and the reason why certain participants are being recontacted. A lower threshold—allowing for more preliminary results to be offered—should be considered for decision-making with regard to genotype-driven recruitment.
Recommendation 6. In most cases, individual genetic research results should be offered in the context of genotype-driven recruitment. A careful series of steps should be used both to avoid leaving prospective participants uninformed about the purpose of the study and to maximize their right not to know unwanted genetic information
Because of the ethical importance of avoiding deception when explaining the purpose of a genotype-driven study and why prospective participants are eligible, we believe it will be appropriate to offer individual genetic research results in most cases. It is crucial, however, that information be carefully and incrementally revealed in order to preserve prospective participants' right not to know unwanted genetic results (Andorno 2004; Laurie 1999). Specifically, enough information must be given to enable individuals to decide whether to learn more about the research, without disclosing or implying their results prior to their agreement to receive such information.
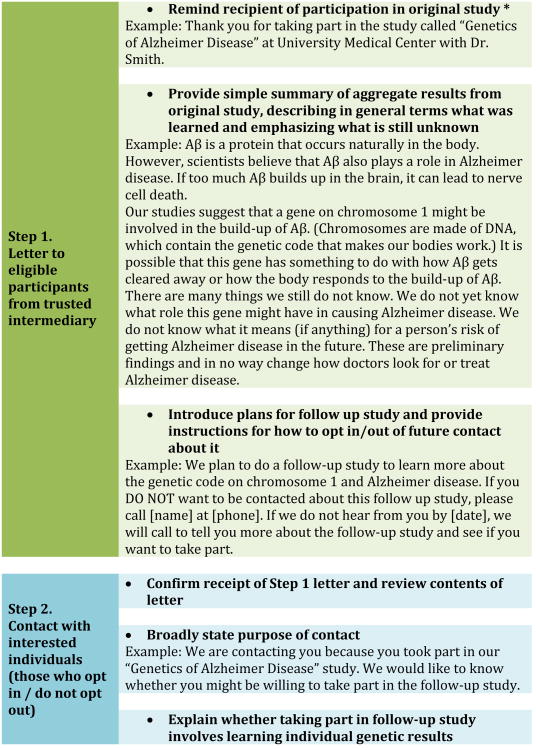
Figure 1 depicts one such approach. A key starting component for many studies will be the communication of aggregate results in clear lay language, conveying the nature and limitations of the original research findings. The description of the follow-up study should be given at a general enough level that prospective participants can understand the broad premise of the study, but cannot directly infer their individual status with regard to genetic inclusion criteria. At each stage, the information previously discussed should be reviewed and the prospective participant's desire to proceed confirmed. It is critical that people understand the tenuousness of the results they receive, and the use of well-trained research staff is essential.
Figure 1. Sample Approach to Genotype-Driven Recontact and Recruitment.
* In a biobank context, this point could be expanded to include (a) a reminder of biobank participation, and (b) a brief description of the specific study, e.g., “One of the studies researchers did with the stored samples and data was to look for links between X and Y.”
Readability characteristics: STEP 1 - Flesch-Kincaid grade level 7.3, Flesch-Kincaid reading ease 73, passive sentences 7%; STEP 2 (vary depending on which bulleted sentence is used) - Flesch-Kincaid grade level 7.7-8.8, Flesch-Kincaid reading ease 62-71, passive sentences 0%; STEP 3 - Flesch-Kincaid grade level 9.2, Flesch-Kincaid reading ease 60, passive sentences 0%
Our recommendation that individual results should generally be offered in the context of genotype-driven recruitment is not intended to suggest that they must be offered in every instance. For each study, arguments both for and against offering results will have to be considered (see Recommendation 7). In addition, the decision to receive results must be made by the potential recipient. Researchers and IRBs should determine in advance whether individuals who do not want to know their results can still participate in a genotype-driven study. Some individuals may wish to contribute to scientific advancement on the study question without knowing their status; if this is deemed acceptable from an ethical and scientific perspective, processes must be in place to avoid inadvertent disclosure during the course of the study.
The role of the Clinical Laboratory Improvement Amendments (CLIA) in the disclosure of research results is an important topic but our workshop was not constituted to meaningfully address this regulatory issue. CLIA certification is required of laboratories that report patient-specific results “for the purpose of providing information for the diagnosis, prevention, treatment of disease, or impairment of, or assessment of health” (https://www.cms.gov/CLIA/). Discussion continues regarding whether research labs that are not CLIA certified can disclose any information to participants (Fabsitz et al. 2010; Wolf et al. 2012; Wolf et al. 2008). However, we believe the explicit motivation for offering results in the context of genotype-driven recruitment—to achieve a scientific goal in an ethical manner, not for the participant's health-related benefit—is highly pertinent to this issue and merits further exploration.
Recommendation 7. For each study, appropriate approaches to genotype-driven recontact and the disclosure of individual genetic research results should be determined by researchers in consultation with their IRB
Empirical research suggests there is unlikely to be a “one-size-fits-all” solution, but rather several ethically acceptable approaches to genotype-driven recruitment depending on context (Beskow et al. 2011; Beskow et al. in press). For each study, the logistical process of recontact and the decision about whether to offer individual genetic results should be determined by researchers in consultation with their IRBs. Several factors, in addition to those already discussed, should be considered, including:
The nature of the researcher-participant relationship, including the frequency and duration of interactions, the longevity of the relationship, and whether the researcher is also the participants' physician or is part of the entity that provides participants' health care (Beskow and Burke 2010)
The nature of the research findings, including whether they are related to the etiology of an already-diagnosed condition (Namey and Beskow 2011) or suggest something about future risk or prognosis (per Recommendation 6, thresholds of validity and utility may be lower than those recommended for the return of results in general, but the research findings' certainty and usefulness (or lack thereof) should be considered when designing appropriate approaches to genotype-driven recruitment)
The nature of the study population, including whether or not participants have been diagnosed with the condition under study (Cadigan et al. 2011), whether participants are minors (Tabor et al. 2011), and issues related to cognitive, social, psychological, or economic vulnerabilities (Beskow and Burke 2010)
The nature of the follow-up study design, including plans to recruit family members (Beskow et al. 2004; Beskow et al. 2010; Hull et al. 2004)
In particular, investigators and IRBs should be aware of the range of expectations and assumptions that prospective participants may hold with regard to the meaning and usefulness of genetic information, and tailor their plans accordingly (Cadigan et al. 2011; Namey and Beskow 2011; Tabor et al. 2011). For instance, participants who have a condition without clear etiology may expect that genetic research results will reveal the cause of their illness (Namey and Beskow 2011). With awareness of the potential for this kind of over-interpretation, investigators can devise approaches to genotype-driven recruitment that include easy-to-understand explanations of the state of genomic science in their area of research, what the results of a particular study do and do not mean, and what they hope to learn with further study. There are several resources for identifying likely expectations among the target study population, including clinicians who regularly treat patients with the condition under study, disease advocacy organizations, or even a simple focus group of potential participants (Namey and Beskow 2011).
Conclusion and Future Directions
In their vision for the future of genomic research and the path toward genomic medicine, Green and colleagues stated (Green and Guyer 2011),
…large-scale genomic studies alone will not be sufficient for gaining a fundamental understanding of biology. Most of the data analysis and interpretation will actually come from individual research efforts. Indeed, a primary motivation for the development of genomics … has been to generate data catalogues and technological tools that empower individual investigators to pursue more effective hypothesis-driven research. (p.207)
Genotype-driven recruitment is a potentially powerful approach to such research—a means to advance the pace of research on the functional significance of human genetic variation and speed progress toward the ultimate goal of benefitting human health (McGuire and McGuire 2008). At the same time, this kind of recruitment raises concerns because the potential harms associated with the use and disclosure of genetic information are linked to the offer to participate in research.
Our recommendations address some issues that are generic with respect to recontacting participants about additional research as well as special issues that arise in genotype-driven recruitment. They are based in part on empirical data and should themselves be the subject of additional research. They are also based on current regulations for the protection of human research participants, which may undergo significant change (Emanuel and Menikoff 2011). As the landscape continues to evolve, it will be important to examine awareness and uptake of these recommendations, and to assess the outcomes of their implementation in terms of the impact on research participants and on rates of participation in scientifically valuable research.
Supplementary Material
Acknowledgments
Workshop participants (in addition to named authors): Georgia M. Alexander+, Research Participant; John H. Alexander, MD, MHS+, Duke Clinical Research Institute; Tracy Brazg, MSW, MPH*+, Seattle Children's Research Institute; Goldie S. Byrd, PhD, North Carolina Agricultural & State University; R. Jean Cadigan, PhD*+, University of North Carolina at Chapel Hill; Patricia Chulada, PhD, MHS+, National Institute of Environmental Health Sciences; Ellen Wright Clayton, MD, JD+, Vanderbilt University; Alexandra Cooper, PhD*+, Duke Social Science Research Institute; Julia Crouch, MPH*+, Seattle Children's Research Institute; Lauren A. Dame, JD, MPH+, Duke Institute for Genome Sciences & Policy; Douglas S. Diekema, MD, MPH+, Seattle Children's Research Institute; David G. Forster, JD, MA, CIP+, Western Institutional Review Board; Debbie Frisbee+, Research Participant; David B. Goldstein, PhD, Duke University; Gail E. Henderson, PhD*+, University of North Carolina at Chapel Hill; Sherri Holmes, Research Participant; Julie Kaneshiro, MA^, U.S. Department of Health and Human Services; John M. Kessler, PharmD+, Duke University; Clara Lajonchere, PhD+, Autism Speaks; Kristen N. Linney, RN+, Duke University; Sean McGuire, MD, PhD+, Baylor College of Medicine; Amy L. McGuire, JD, PhD+, Baylor College of Medicine; Marsha Michie, PhD*+, University of North Carolina at Chapel Hill; Janet Miller, JD, PhD+, Autism Genetic Resource Exchange; P. Pearl O'Rourke, MD+, Partners HealthCare; Jeffrey Peppercorn, MD, MPH+, Duke University Medical Center; Rodney A. Radtke, MD+, Duke University Medical Center; Laura Lyman Rodriguez, PhD+, National Human Genome Research Institute; Monica Samsky+, Research Participant; Maureen E. Smith, MS, CGC+, Northwestern University; Holly Tabor, PhD*+, Seattle Children's Research Institute
*Member of research team for RC1HG005787, “Ethical Approaches to Genotype-Driven Research Recruitment”
+Affirmed general agreement with these recommendations (in personal capacity, not as institutional representative)
^Constrained from formally expressing an opinion due to governmental position
Thanks to Devon Check for her assistance in organizing the workshop that led to these recommendations.
Funding source: The project described was supported by Award Number RC1HG005787 from the National Human Genome Research Institute. Support was also provided by UL1RR025014 from the National Center for Research Resources. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Public database ascension numbers: Not applicable
References
- Andorno R. The right not to know: an autonomy based approach. J Med Ethics. 2004;30:435–9. doi: 10.1136/jme.2002.001578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beskow LM, Botkin JR, Daly M, Juengst ET, Lehmann LS, Merz JF, Pentz R, Press NA, Ross LF, Sugarman J, Susswein LR, Terry SF, Austin MA, Burke W. Ethical issues in identifying and recruiting participants for familial genetic research. Am J Med Genet A. 2004;130A:424–31. doi: 10.1002/ajmg.a.30234. [DOI] [PubMed] [Google Scholar]
- Beskow LM, Burke W. Offering individual genetic research results: context matters. Sci Transl Med. 2010;2:38cm20. doi: 10.1126/scitranslmed.3000952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beskow LM, Linney KN, Radtke RA, Heinzen EL, Goldstein DB. Ethical challenges in genotype-driven research recruitment. Genome Res. 2010;20:705–9. doi: 10.1101/gr.104455.109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beskow LM, Namey EE, Cadigan RJ, Brazg T, Crouch J, Henderson GE, Michie M, Nelson DK, Tabor HK, Wilfond BS. Research participants' perspectives on genotype-driven research recruitment. J Empir Res Hum Res Ethics. 2011;6:3–20. doi: 10.1525/jer.2011.6.4.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beskow LM, Namey EE, Miller PR, Nelson DK, Cooper A. IRB. IRB chairs' perspectives on genotype-driven research recruitment. in press. [PMC free article] [PubMed] [Google Scholar]
- Beskow LM, Sandler RS, Weinberger M. Research recruitment through US central cancer registries: balancing privacy and scientific issues. Am J Public Health. 2006;96:1920–6. doi: 10.2105/AJPH.2004.061556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cadigan RJ, Michie M, Henderson G, Davis AM, Beskow LM. The meaning of genetic research results: reflections from individuals with and without a known genetic disorder. J Empir Res Hum Res Ethics. 2011;6:30–40. doi: 10.1525/jer.2011.6.4.30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chulada PC, Vahdat HL, Sharp RR, DeLozier TC, Watkins PB, Pusek SN, Blackshear PJ. The Environmental Polymorphisms Registry: a DNA resource to study genetic susceptibility loci. Hum Genet. 2008;123:207–14. doi: 10.1007/s00439-007-0457-5. [DOI] [PubMed] [Google Scholar]
- Emanuel EJ, Menikoff J. Reforming the regulations governing research with human subjects. N Engl J Med. 2011;365:1145–50. doi: 10.1056/NEJMsb1106942. [DOI] [PubMed] [Google Scholar]
- Fabsitz RR, McGuire A, Sharp RR, Puggal M, Beskow LM, Biesecker LG, Bookman E, Burke W, Burchard EG, Church G, Clayton EW, Eckfeldt JH, Fernandez CV, Fisher R, Fullerton SM, Gabriel S, Gachupin F, James C, Jarvik GP, Kittles R, Leib JR, O'Donnell C, O'Rourke PP, Rodriguez LL, Schully SD, Shuldiner AR, Sze RK, Thakuria JV, Wolf SM, Burke GL. Ethical and practical guidelines for reporting genetic research results to study participants: updated guidelines from a National Heart, Lung, and Blood Institute working group. Circ Cardiovasc Genet. 2010;3:574–80. doi: 10.1161/CIRCGENETICS.110.958827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fernandez C. Public expectations for return of results--time to stop being paternalistic? Am J Bioeth. 2008;8:46–8. doi: 10.1080/15265160802513127. [DOI] [PubMed] [Google Scholar]
- Green ED, Guyer MS. Charting a course for genomic medicine from base pairs to bedside. Nature. 2011;470:204–13. doi: 10.1038/nature09764. [DOI] [PubMed] [Google Scholar]
- Hull SC, Glanz K, Steffen A, Wilfond BS. Recruitment approaches for family studies: attitudes of index patients and their relatives. IRB. 2004;26:12–7. [PMC free article] [PubMed] [Google Scholar]
- Kohane IS, Taylor PL. Multidimensional results reporting to participants in genomic studies: getting it right. Sci Transl Med. 2010;2:37cm19. doi: 10.1126/scitranslmed.3000809. [DOI] [PubMed] [Google Scholar]
- Laurie GT. In defence of ignorance: genetic information and the right not to know. Eur J Health Law. 1999;6:119–32. doi: 10.1163/15718099920522730. [DOI] [PubMed] [Google Scholar]
- McGuire SE, McGuire AL. Don't throw the baby out with the bathwater: enabling a bottom-up approach in genome-wide association studies. Genome Res. 2008;18:1683–5. doi: 10.1101/gr.083584.108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meltzer LA. Undesirable implications of disclosing individual genetic results to research participants. Am J Bioeth. 2006;6:28–30. doi: 10.1080/15265160600935811. [DOI] [PubMed] [Google Scholar]
- Miller FA, Christensen R, Giacomini M, Robert JS. Duty to disclose what? Querying the putative obligation to return research results to participants. J Med Ethics. 2008;34:210–3. doi: 10.1136/jme.2006.020289. [DOI] [PubMed] [Google Scholar]
- Namey EE, Beskow LM. Epilepsy patient-participants and genetic research results as “answers”. J Empir Res Hum Res Ethics. 2011;6:21–9. doi: 10.1525/jer.2011.6.4.21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Bioethics Advisory Commission. Research Involving Human Biological Materials: Ethical Issues and Policy Guidance. Vol. 1. US Government Printing Office; Rockville, MD: 1999. [Google Scholar]
- Parker LS. Rethinking respect for persons enrolled in research. ASBH Exchange. 2006;9:1,6–7. [Google Scholar]
- Prentice KJ, Appelbaum PS, Conley RR, Carpenter WT. Maintaining informed consent validity during lengthy research protocols. IRB. 2007;29:1–6. [PubMed] [Google Scholar]
- Ram N. Tiered consent and the tyranny of choice. Jurimetrics. 2008;48:253–284. [Google Scholar]
- Shalowitz DI, Miller FG. Disclosing individual results of clinical research: implications of respect for participants. JAMA. 2005;294:737–40. doi: 10.1001/jama.294.6.737. [DOI] [PubMed] [Google Scholar]
- Tabor HK, Brazg T, Crouch J, Namey EE, Fullerton SM, Beskow LM, Wilfond BS. Parent perspectives on pediatric genetic research and implications for genotype-driven research recruitment. J Empir Res Hum Res Ethics. 2011;6:41–52. doi: 10.1525/jer.2011.6.4.41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolf SM, Crock BN, Van Ness B, Lawrenz F, Kahn JP, Beskow LM, Cho MK, Christman MF, Green RC, Hall R, Illes J, Keane M, Knoppers BM, Koenig BA, Kohane IS, Leroy B, Maschke KJ, McGeveran W, Ossorio P, Parker LS, Petersen GM, Richardson HS, Scott JA, Terry SF, Wilfond BS, Wolf WA. Managing incidental findings and research results in genomic research involving biobanks and archived data sets. Genet Med. 2012;14:361–84. doi: 10.1038/gim.2012.23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolf SM, Lawrenz FP, Nelson CA, Kahn JP, Cho MK, Clayton EW, Fletcher JG, Georgieff MK, Hammerschmidt D, Hudson K, Illes J, Kapur V, Keane MA, Koenig BA, Leroy BS, McFarland EG, Paradise J, Parker LS, Terry SF, Van Ness B, Wilfond BS. Managing incidental findings in human subjects research: analysis and recommendations. J Law Med Ethics. 2008;36211:219–48. doi: 10.1111/j.1748-720X.2008.00266.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.