Abstract
Background
Limited research exists on physician-delivered education interventions. We examined the feasibility and impact of an educational tool on facilitating physician-patient kidney disease communication.
Study Design
Pilot feasibility clinical trial with a historical control to examine effect size on patient knowledge and structured questions to elicit physician and patient feedback.
Setting & Participants
Adults with chronic kidney disease (CKD) stages 1–5, seen in nephrology clinic.
Intervention
One page educational worksheet, reviewed by physicians with patients.
Outcomes
Kidney knowledge between patient groups and provider/patient feedback.
Measurements
Patient kidney knowledge was measured using a previously validated questionnaire compared between patients receiving the intervention (April–October 2010) and a historical cohort (April–October 2009). Provider input was obtained using structured interviews. Patient input was obtained through survey questions. Patient characteristics were abstracted from the medical record.
Results
556 patients were included, with 401 patients in the historical cohort, and 155 receiving the intervention. Mean age was 57 ± 16 (SD) years, with 53% male, 81% White, and 78% CKD stages 3–5. Compared to the historical cohort, patients receiving the intervention had higher adjusted odds of knowing they had CKD (adjusted OR, 2.20; 95% CI, 1.16–4.17; p=0.01), knowing their kidney function (adjusted OR, 2.25; 95% CI, 1.27–3.97; p=0.005), and knowing their stage of CKD (adjusted OR, 3.22; 95% CI, 1.49–6.92; p=0.003). Physicians found the intervention tool easy and feasible to integrate into practice and 98% of patients who received the intervention recommended it for future use.
Limitations
Study design did not randomize patients for comparison and enrollment was performed in clinics at one center.
Conclusions
In this pilot study, a physician delivered education intervention was feasible to use in practice, and was associated with higher patient kidney disease knowledge. Further examination of physician delivered education interventions for increasing patient disease understanding should be tested through randomized trials.
Index Words: Chronic Kidney Disease, Patient Education, Education Intervention, Patient-centered care
Patient-centered care emphasizes a partnership between patients and providers to create an environment where patients gain information necessary to actively engage in decisions related to their own health.1 In patients with kidney disease, understanding of basic concepts about kidney function, symptoms of progressing disease, and one’s own disease status is unsatisfactory, even amongst those seeing nephrologists.2 Low patient kidney knowledge is associated with worse clinical outcomes, including less use of permanent dialysis access,3 and shorter times to dialysis initiation.4 Low knowledge is also associated with low mental health function—linked to both increased mortality and hospitalizations.5 Moreover, poor patient knowledge may prohibit optimal participation in shared decision-making in many areas critical to preventing disease progression and preparing for transition to renal replacement therapy.
Education interventions in patients initiating renal replacement therapy increase patient knowledge and improve clinical outcomes.6 But education intervention studies are lacking in earlier chronic kidney disease (CKD),7 perhaps where prevention and patient self-care efforts could have greatest impact. Additionally, although patients perceive physicians as their most influential source of health information,8 there is a paucity of research in kidney disease specifically examining physician-delivered education interventions.7 Whether such interventions are feasible in nephrology clinical practice, and their impact on patient outcomes, remain largely unknown.
The objective of this study was to test the feasibility and impact of a brief, physician-delivered, educational worksheet used to facilitate discussion with patients about their established CKD during nephrology visits. The worksheet focused on addressing gaps in patient knowledge, including patients’ understanding of their kidney function, monitoring and treatment. We hypothesized this educational intervention would increase patient knowledge compared to a historical cohort, and would be a well-received, efficient tool for providers.
METHODS
Study Design, Setting, and Participants
We enrolled patients using convenience sampling at one academic center who were ≥ 18 years of age and had established CKD per the National Kidney Foundation–Kidney Disease Outcomes Quality Initiative (NKF-KDOQI).9 This diagnosis was determined by medical record review of estimated glomerular filtration rate (eGFR), kidney imaging/related results (e.g. biopsy reports), and nephrology provider documentation. Patients had to understand and speak English, as our study was not designed to assess multi-lingual knowledge needs. Research staff read aloud the survey if needed (e.g. literacy concerns). Patients were excluded if they had not been seen in nephrology clinic at least once prior to enrollment (i.e. new patients), received dialysis or a kidney transplant, or had significant cognitive or vision impairment. There were nine nephrology clinics consisting of nine attending physicians and 16 nephrology fellows.
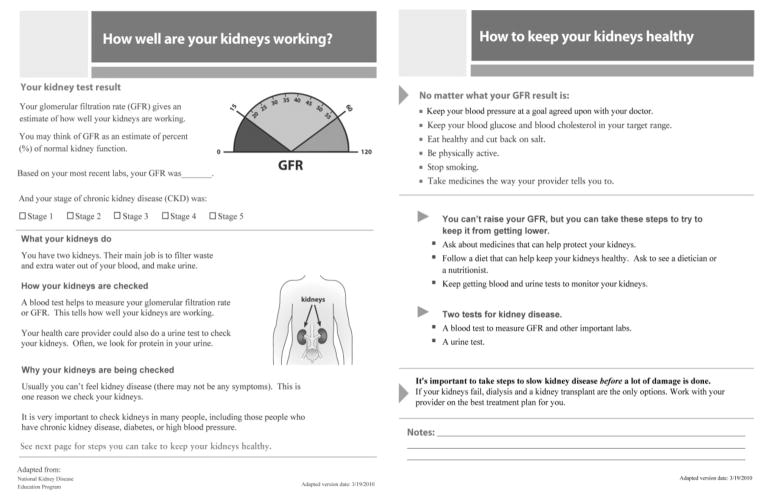
To examine the effect of the intervention we compared patient knowledge about kidney disease between patients who had received the educational intervention (April 2010 to October 2010) and a historical cohort (April 2009 to October 2009) (Figure 1). Patients who participated in the historical cohort were not eligible for enrollment in the intervention group. Provider and patient feedback to determine acceptability and usefulness of the intervention was assessed by structured interviews. Patients who received the intervention were asked if it was helpful and if they recommended it for use with others.
FIGURE 1.
STUDY DESIGN AND TIMELINE
The study was approved by the Vanderbilt Institutional Review Board. All subjects provided written informed consent and were offered small monetary compensation.
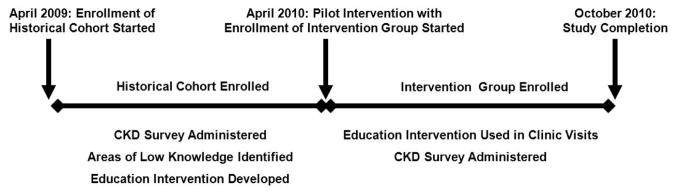
Educational Intervention
The one page intervention worksheet was delivered by physicians (nephrology fellows) during clinic visits. Providers attended a one-hour training session including information on clear communication principles,10 health literacy,11 and an orientation to using the customizable, interactive kidney-disease educational intervention worksheet. The worksheet was adapted from the National Kidney Disease Education Program resources (Figure 2)12, and was reviewed by nephrology physicians, and health communication experts to optimize its content for the intended target audience. The worksheet emphasized patient awareness of their CKD diagnosis, assessment of kidney function, and strategies for care. Intervention fidelity was evaluated by asking patients if the worksheet was used during their visit.
FIGURE 2. KIDNEY EDUCATION WORKSHEET (FRONT AND BACK).
Adapted from the National Kidney Disease Education Program12.
Outcomes
The primary outcome was kidney-specific knowledge determined by the validated Kidney Knowledge Survey (KiKS)2 (the survey itself is available as supplementary material for Wright et al2), with additional items specific to awareness. Outcomes were measured immediately after the clinic visit in both historical control and intervention groups. In addition to overall KiKS scores, individual items specifically addressed by the intervention were compared between study groups.
Additional measures obtained by patient self-report and medical record review included demographics, number of previous nephrology visits, stage of CKD, previous attendance in structured CKD education classes, whether the patient knew someone else with CKD, and health literacy (assessed using the Rapid Estimate of Adult Literacy in Medicine [REALM]).13 Stage of chronic kidney disease was determined using serum creatinine, estimated glomerular filtration rate (eGFR),14 urinary protein measurements, and imaging or related reports abstracted from the medical record.
Statistical Analyses
Sample size calculations used effect size estimates of differences between the historical cohort and the intervention group for the KiKS score. Estimates of 0.3–0.5 are generally considered to be conservative and we chose to use an effect size of 0.4.15 With 2-sided significance of 0.05, and power of 0.90, the study required at least 132 patients each in the historical cohort and intervention group to detect a difference of 0.4 in standard deviations of the mean KiKS score. This number was inflated by 10%–15% for potential dropouts.
Descriptive statistics were calculated as median and interquartile range (IQR) for continuous variables or frequency (%) for categorical variables. We examined the association of the intervention with proportions of patients correctly answering individual awareness and knowledge questionnaire items. Four patients (3%) in the intervention group did not receive the educational tool but were included in the analysis as an intention-to-treat. We performed complete case analysis excluding patients with missing values of knowledge of kidney function and CKD stage (25.2%), income (5%), and “know anyone with CKD” and health literacy (less than 0.5%). For analyses with kidney function and CKD stage as outcomes, 394 subjects were included. For analyses of the total score and all other individual items as outcomes, 521 subjects were included.
Unadjusted associations were analyzed using the Pearson chi-square test. Adjusted associations were analyzed using logistic regression with Huber-White robust sandwich estimator including supervising attending as a clustering variable.16 Each model adjusted for a priori defined covariates including patients’ age, sex, race, income, average eGFR, health literacy, number of doctor visits, and whether the patient knew anyone else with CKD. Average eGFR was estimated as the mean value of two measurements closest to the patient visit, but not exceeding one-year prior. For those patients with only one measurement, the single value was used as their eGFR. Findings with a 2-sided p-value <0.05 were considered statistically significant. All statistical calculations were performed using R statistical software version 2.12.0 (R Foundation for Statistical Computing).
Interviews of providers were transcribed verbatim and analyzed using manual statement counts with NVivo, a qualitative analysis software package. (NVivo, version 8, QSR International Pty Ltd)
RESULTS
Patient Characteristics
A total of 401 patients were enrolled in the historical cohort, and 155 received the intervention (Figure 3). Among all patients screened within the nephrology clinic, we did not track the number of patients excluded. We previously reported no differences in age and sex comparing patients who enrolled in the historical cohort (responders) versus those declined to participate (nonresponders).17 In comparing age and sex between responders and nonresponders in the intervention group, we found no differences in sex, but patients were of older age among the nonresponders (mean age of 62 [95% CI, 59–61] years versus 57 [95% CI, 54–59] years; p=0.004). Five patients withdrew from the historical cohort because of time constraints (2), feeling too ill (2), or not wanting to finish (1). Eleven withdrew from the intervention group because of time constraints (5), feeling too ill (3), declining to participate after enrollment (2), or administrative reasons (1).
FIGURE 3.
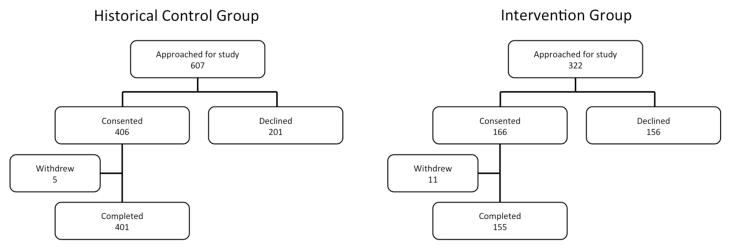
ENROLLMENT FLOW DIAGRAMS FOR THE HISTORICAL COHORT AND INTERVENTION GROUP
The mean age of the total study population (N=556) was 57 ± 16 (standard deviation) years. Fifty-three percent were male, 81% White, and 78% had CKD stages 3–5. There were no statistically significant differences in age, sex, race, educational attainment, estimated glomerular filtration rate (eGFR), previous participation in CKD education, health literacy, or income level between the historical cohort and intervention group (Table 1). Fewer participants in the intervention group had seen their kidney doctor 3 times or more in the past one year compared to those in the historical cohort (48% vs. 58%; p=0.04).
TABLE 1.
PARTICIPANT CHARACTERISTICS
| No. | Historical Cohort (n=401) | Intervention Group (n=155) | p-value | |
|---|---|---|---|---|
| Age (y) | 556 | 58 [46–68] | 58 [46–69] | 0.9 |
| Race | 556 | 0.08 | ||
| White | 333 (83) | 119 (77) | ||
| Non-white | 68 (17) | 36 (23) | ||
| Sex | 556 | 0.8 | ||
| Female | 188 (47) | 71 (46) | ||
| Male | 213 (53) | 84 (54) | ||
| Formal Education Attainment | 554 | 0.7 | ||
| < High School | 26 (6) | 11 (7) | ||
| ≥High School | 375 (94) | 142 (93) | ||
| REALM | 555 | 0.2 | ||
| <9th grade literacy | 71 (18) | 34 (22) | ||
| ≥9th grade literacy | 330 (82) | 120 (78) | ||
| eGFR (ml/min/1.73 m2) | 556 | 41 [28–57] | 38 [27–56] | 0.2 |
| Annual Income | 525 | 0.07 | ||
| <$25,000 | 71 (19) | 40 (28) | ||
| $25,000 – $55,000 | 128 (34) | 46 (32) | ||
| > $55,000 | 181 (48) | 59 (41) | ||
| No. of kidney doctor visits, past 1 y | 556 | 0.04 | ||
| <2 visits | 169 (42) | 80 (52) | ||
| ≥3 visits | 232 (58) | 75 (48) | ||
| Know someone else with CKD | 553 | 202 (51) | 82 (53) | 0.5 |
| Attended Previous CKD education class | 554 | 67 (17) | 21 (16) | 0.7 |
Note: Values for categorical variables are given as number (percentage); values for continuous variables, as median [interquartile range].
REALM, Rapid Estimate of Adult Literacy in Medicine; CKD, chronic kidney disease; eGFR, estimated glomerular filtration rate;
Patient Gaps in CKD Awareness and Knowledge
Findings from the CKD knowledge survey in the historical cohort have been previously reported.2,17 Areas where knowledge was poor included physiologic roles of the kidney, understanding symptoms of advanced disease, and nephrology-related terms. There were also gaps in patients’ understanding about their diagnosis, including the presence of decreased kidney function and its severity. Most participants in the intervention group recognized they had a problem with their kidneys (96%); however, fewer (78%) acknowledged their diagnosis of chronic kidney disease (Table 2). Even fewer were able to identify their stage of CKD or estimated level of kidney function.
TABLE 2.
UNADJUSTED AND ADJUSTED ANALYSES OF CORRECT AWARENESS AND KNOWLEDGE SURVEY QUESTIONS
| Survey Question | No. | Historical Cohort (n=401) | Intervention Group (n=155) | Unadjusted Analysis | Adjusted Analysis* | |||
|---|---|---|---|---|---|---|---|---|
| p-value | OR (95% CI) | p-value | aOR (95% CI) | p-value | ||||
| Awareness of kidney problem | 556 | 375 (94) | 149 (96) | 0.2 | 1.72 (0.62–4.79) | 0.3 | 3.01 (1.06–8.60) | 0.04 |
| Awareness of CKD diagnosis | 556 | 278 (69) | 121 (78) | 0.04 | 1.57 (1.19–2.09) | 0.002 | 2.20 (1.16–4.17) | 0.02 |
| Awareness of decreased kidney function | 556 | 307 (77) | 109 (70) | 0.1 | 0.73 (0.45–1.16) | 0.2 | 0.68 (0.49–0.94) | 0.02 |
| Aware of current estimate of kidney function | 416 | 149 (49)# | 74 (68)^ | <0.001 | 2.24 (1.45–3.47) | <0.001 | 2.25 (1.27–3.97) | 0.005 |
| Aware of stage of CKD | 416 | 110 (36)# | 71 (65)^ | <0.001 | 3.34 (1.68–6.66) | <0.001 | 3.22 (1.49–6.92) | 0.003 |
| Knowledge a person normally has 2 kidneys | 556 | 395 (99) | 155 (100) | 0.1 | 1553.39 (295.74–8159.28) | <0.001 | 1586.30 (187.41–13426.89) | <0.001 |
| Knowledge the kidneys make urine | 556 | 274 (68) | 124 (80) | 0.006 | 1.85 (1.28–2.67) | <0.001 | 1.68 (1.09–2.60) | 0.02 |
| Knowledge the kidneys clean blood | 556 | 353 (88) | 137 (88) | 0.9 | 1.03 (0.54–1.98) | 0.9 | 0.99 (0.55–1.79) | 0.9 |
| Knowledge of how kidney function is checked | 556 | 385 (96) | 151 (97) | 0.4 | 1.57 (0.34–7.23) | 0.6 | 1.63 (0.32–8.28) | 0.6 |
| Knowledge there may not be symptoms | 556 | 89 (22) | 44 (28) | 0.1 | 1.39 (0.85–2.27) | 0.2 | 1.61 (0.97–2.67) | 0.06 |
| Knowledge of what GFR stands for | 556 | 273 (68) | 131 (85) | <0.001 | 2.56 (1.69–3.87) | <0.001 | 4.90 (3.20–7.40) | <0.001 |
| Knowledge of stages of CKD | 556 | 374 (93) | 134 (86) | 0.01 | 0.46 (0.33–0.63) | <0.001 | 0.47 (0.29–0.74) | 0.001 |
| General KiKS | 556 | 68 [57 to 75] | 68 [57 to 75] | 0.8 | 0.010 [−0.021 to 0.041] | 0.5 | ||
Note: Unless otherwise indicated, values are given as number (percentage) or median [interquartile range].
Adjusted for age, sex, race, health literacy, income, number of provider visits, estimated GFR, health literacy and knowing someone else with CKD
n=307.
n=109
CKD, chronic kidney disease; GFR, glomerular filtration rate; OR, odds ratio; AOR, adjusted odds ratio; CI, confidence interval; KiKS, Kidney Knowledge Survey
Unadjusted and Adjusted Analyses
When compared to historical cohort participants, unadjusted analysis showed that a higher proportion of patients receiving the intervention were aware of their CKD diagnosis (78% vs. 69%; p=0.04), and correctly defined “GFR” (85% vs. 68%; p<0.001), their estimated kidney function category (68% vs. 49%; p<0.001), and their stage of CKD (65% vs. 36%; p<0.001). A higher proportion of patients in the historical cohort knew there were stages of CKD as compared to the intervention group (93% vs. 86%; p=0.01). There was no evidence of difference in overall kidney knowledge survey summary scores (KiKS) between the intervention group and the historical cohort (p= 0.8). (Table 2)
Adjusted analyses (Table 2) showed that, compared to the historical cohort, patients receiving the intervention had higher adjusted odds ratio (aOR) of knowing they had a kidney problem (aOR, 3.01; 95% CI, 1.06–8.60; p=0.04), knowing they had CKD (aOR, 2.20; 95% CI, 1.16–4.17; p=0.01), knowing their kidney function (aOR, 2.25; 95% CI, 1.27–3.97; p=0.005), knowing their stage of CKD (aOR, 3.22; 95% CI, 1.49–6.92; p=0.003), knowing the kidneys make urine (aOR, 1.68; 95% CI, 1.09–2.60; p=0.02), and knowing the term GFR (aOR, 4.90; 95% CI, 3.20–7.40; p<0.001). There was also a higher proportion who knew most people have two kidneys (AOR, 1,586.30; 95% CI, 187.41–13,426.89; p=<0.001), although very high odds ratios reflected that nearly all participants answered correctly. Interestingly, patients in the intervention group retained a lower odds (aOR, 0.47; 95% CI, 0.29–0.74; p=0.001) of knowing there were stages of CKD compared to the historical cohort, as well as a lower odds of reporting they had “decreased kidney function” (aOR, 0.68; 95% CI, 0.49–0.94; p=0.02). No clinically significant evidence of differences by literacy level were observed in this study.
Educational Intervention Feasibility
Among intervention participants, 66% percent deemed the worksheet extremely helpful, and 98% recommended its use. We performed structured interviews with seven (47%) nephrology fellows who delivered the intervention. Question topics and selected verbatim responses are shown in Table 3. The interview questions are provided as online supplemental material (Item S1). Fellows’ mean age was 31 ± 2 years, and two (29%) were female. They perceived the kidney education worksheet as useful, including important content and visual aids to confer information. The worksheet was efficient and required only 1–2 minutes to administer. They suggested the worksheet was valuable to facilitate discussions not only during nephrology visits, but with potential applicability in primary care. Concerns were redundancy in some of the talking points, and the flow of information.
TABLE 3.
PHYSICIAN PERCEPTIONS OF USING THE EDUCATION WORKSHEET IN PRACTICE
| Question Topic Area | No. of statements | Representative Comments |
|---|---|---|
| Perception of usefulness | 20 |
“I think it’s very helpful. The amount of information on the sheet is brief and to the point”---PFG1 “It reminded me as a physician to do some basic education with each of the patients”---PFG1 “I think the one thing I liked the most was the GFR visual aid … Being able to show patients [GFR) on a scale I thought really helps” PFG5 |
| Benefits to using | 47 |
“I had more than one patient … who when I informed them of their GFR, which I’m pretty sure I informed them before, it was a revelation. They had no idea that this is their percent kidney function. I suspect that’s because those individuals were more visual learners than audio, and seeing something really made it click” PFG1 “It added another way for me as a provider to educate patients … not everyone learns in the same way … having something concrete and short with bright colors is nice” PFG1 “It didn’t take time away [from clinic) at all” PFG1 “[Time spent on it with each patient) was 1–2 minutes” PFG4 “It reminds the physician of all the high points that they need to communicate to the patients and also allows the patient to read something and gives them a visual way of learning as well as an auditory way of learning as you speak to them.” PFG2 |
| Barriers/concerns to using | 26 |
“On the second page it says ‘take medicines the way your provider tells you to’ … I almost felt like that was a little too paternalistic” PFG1 “The order of the information made it difficult for me to get through. … I thought it would make more sense to explain [what the kidneys did) first. “ PFG2 “The actual [GFR) diagram is not proportional … if the patient is looking at [it) they may think that there is an equal chance of [GFR) being in green as the red and that most people are in the yellow.” PFG2 “One patient interpreted the [GFR diagram) like an odometer. Her mind set was that ‘where the numbers are lower … it is safer’. So you have to make sure your patient understands what your goal of the schematic is.” PFG2 |
| How worksheet was used | 19 |
“I focused on different parts [of the worksheet) for different patients.” PFG1 “I think the words ‘chronic kidney disease’ are important because patients need to understand that they have a chronic disease and that it’s relating to their kidneys. I say percent kidney function … instead of saying GFR.” PFG5 |
| Recommend ations for future | 32 |
“This is a very brief, succinct overview of a large, complicated disease process … any provider would be able to use it” PFG1 “I would distribute them to nephrologists and allow them to use their own and make it an option for primary care providers as well.” PFG1 “I think it is probably a good idea at every clinic visit to go over where a patient’s GFR is and where it has been … help them understand about the possibility of needing renal replacement therapy in the future.” PFG2 “I think it would be especially useful for the internal medicine division to have something like this. Especially for patients who had not been referred to nephrology yet.” PFG5 |
GFR, glomerular filtration rate; PFG,
DISCUSSION
In this pilot study, we showed that a brief, physician-delivered education intervention is feasible to apply in an outpatient nephrology practice, and is associated with increased patient knowledge about CKD. Patients who received the educational intervention had greater awareness and knowledge about kidney disease when compared to a historical cohort. Specifically, they were more likely to know they had a kidney problem, recognize their diagnosis of CKD, accurately report its severity, and have a better understanding of kidney actions and commonly used kidney-related medical terms.
The findings of our study have important implications. The educational intervention was estimated to take approximately 1–2 minutes, easy to administer, did not interfere with routine clinic visits, and was an acceptable adjunct to physician-patient CKD communication. Physicians perceived it as a useful tool to confer important health information to patients, and patients overwhelmingly reported the intervention was helpful to their own understanding. Our intervention facilitated patient-provider communication and addressed some of the barriers patients face in gaining disease information, which may be particularly helpful as research indicates often patients feel they do not even know what questions to ask providers to improve their knowledge.18
Great emphasis has been placed on the importance of program development to enhance identification, awareness, and subsequent treatment of CKD.19,20 In the U.S., there is support for Medicare patients with advanced CKD to participate in specific kidney disease patient education in either individual or group sessions.21 However, the execution of group kidney patient education sessions may be challenging in some settings due to staffing and availability of resources, whereas tools such as the one used in this study can be easily obtained and implemented by individual providers. To our knowledge, this is one of the few studies demonstrating greater patient kidney knowledge using a simple, time-efficient, physician-delivered tool.
Interventions aimed to optimize patient health-related knowledge and subsequent self-care behaviors are often developed after years of multi-phased research, including iterative steps by which interventions are tested and refined over time.22–24 As a recent review points out, the National Institutes of Health outlines phases for development of interventions which include conceptualization, standardization, and piloting. Additionally it recommends that intervention studies first include assessments of the acceptability of intervention delivery in practice, along with determination of feasibility of recruiting study participants. It suggests that data found from pilot work is necessary to inform the development of larger scale, definitive trials.25 Accordingly, the results of our study should be considered preliminary and should pave the way for more rigorously designed trials to test the true efficacy of this educational intervention.
An appealing aspect of our study was that both patients and physicians felt the educational intervention was feasible and should be considered for future use. Patients may have felt the worksheet was helpful because it presented fundamental concepts about kidney disease following clear communication and plain language principles.10 It also included simple graphics to describe information in a complementary visual, non-verbal format. Online tools using simplified graphics to educate women on breast cancer treatment and risks not only increase patient understanding but are perceived as more effective than complex verbal communication and displays.26 This likely also applies in kidney disease, as even the diagnosis is at times an abstract concept due to its frequent lack of symptoms.27
Use of the educational worksheet also may have facilitated more effective communication and rapport building between patients and their physician. Observational data indicate that patients’ assessments of a physician’s trustworthiness and expertise are directly related to how patients process information about their care,28 and this may have contributed to the overwhelmingly positive feedback patients had about the intervention.
We did have unexpected findings. Patients in the intervention group were less aware about their “decreased kidney function” compared to the historical cohort, despite the fact that more patients in the intervention group correctly reported their CKD stage and eGFR. Qualitative research indicates patients may passively accept health information, without clarifying its meaning,29 which could have occurred within our intervention group. In addition, health literacy may have played a role. Although it did not meet statistical significance, a higher proportion of patients in the intervention group were assessed at a lower literacy level. There is often no plain language equivalent for the term ‘function’,30,31 and patients may identify more with an individualized and specific numerical representation of their disease.
Another unexpected finding was that patient knowledge about stages of CKD was lower in the intervention group compared to the historical cohort, although overall both are high and the absolute differences are modest. The reason for higher knowledge about the stages in the historical cohort is not clear, especially since more people in the intervention group were able to identify their own stage of CKD. Similar to the term “function”, we suspect this may reflect patient confusion regarding the definition of CKD staging and its meaning. Debate exists within the nephrology community about perceived ‘pros’ and ‘cons’ of the staging definition and its use in clinical practice and there have been calls for its revision.32 As kidney specialists, providers delivering the intervention in this study were likely aware of this debate, and subsequent communication with patients on this aspect of kidney education could have been limited as a result. In addition, the historical cohort had areas of high knowledge and despite some additional improvements seen in the intervention group, there are still areas where knowledge was not advanced. Thus, important opportunities may still exist to refine the intervention and its delivery for higher impact.
Another interesting finding is that summary scores of kidney knowledge from KiKS were not different between the study groups. The KiKS included many topics not specifically addressed by the education intervention--for example, additional questions about physiologic kidney functions, health implications of CKD, and symptoms observed in advanced disease. In addition, guided by findings in the historical cohort, we identified a significant opportunity to improve patients’ awareness and understanding of their own CKD diagnosis, with some questions not specifically assessed in KiKS. A more comprehensive educational program may be more effective in modifying patients’ overall kidney knowledge.
There are several limitations of this study. First, the design was a pilot and used a comparison of patient kidney knowledge between an intervention group and a historical cohort.. Thus, there may be patient, provider or other external characteristics that affect patient knowledge that are not accounted for in our analysis. However, in this study there were few differences in measured patient characteristics between groups, and there was no specific change in the continuity clinics during the study duration. Additionally, patient knowledge was higher in the intervention group despite the fact that patients in this group had seen their providers less often in the past year than those in the historical cohort. A second limitation is that patients were all enrolled from clinics at one academic center. Thus, our findings may not be generalizable to other patient populations or practice settings. However, in examining our patient demographics, they are similar to those seen in the U.S. non–dialysis-dependent CKD population,33 supporting applicability of our findings to U.S. patients with CKD. Also, patient knowledge was assessed after clinic appointments. Whether this represents newly acquired knowledge during the visit, higher kidney knowledge prior to the visit, or whether this level of kidney knowledge was retained over time remain unknown. For some findings we observed high adjusted odds ratios, although the unadjusted proportions do not reflect the same magnitude and the two groups are well balanced across the adjusted variables. One of the reasons why some adjusted odds ratios are higher than unadjusted might be a mathematical property of the odds ratio, called uncollapsability. This property may lead to a situation when adjusting for a covariate causes the odds ratio to change away from the null, and the greater the association, the greater the change in the adjusted odds ratio, even when the covariate is perfectly balanced between exposure categories.34 A final point is that both groups were enrolled using convenience sampling, and not randomized. Nonresponders were older compared to participants in the intervention group. Studies in hypertension reveal patients who do not attend educational sessions are more likely to be older,35 although when older patients do participate, benefits in both knowledge and health measures are observed.36 Therefore, although there were age differences between responders and nonresponders, it is not clear how this may have affected our results.
There are important implications of our research. A one page, physician-delivered tool can be used to facilitate effective disease communication in non–dialysis-dependent CKD. Awareness of CKD, whereby a patient recognizes that they indeed have the condition, is low in the general population,37 and also low among those at-risk in screening programs.38 Low kidney disease awareness and knowledge pose significant barriers to optimal clinical outcomes as unaware patients are not likely to seek care until late in the course of disease.39,40 Efficiency of administration of the educational intervention, and positive reception by both providers and patients, is encouraging of its use in practice, to improve these areas of low patient knowledge. Importantly, our findings suggest feasibility for development of more rigorous studies and larger trials, including those performed in other practice settings such as primary care--where the majority of patients with non–dialysis-dependent CKD receive care.41
In conclusion, our pilot study revealed that a brief education intervention, easily integrated into clinical practice, was perceived as a useful adjunct to existing CKD related communication and was associated with higher patient disease understanding and knowledge about fundamental kidney disease concepts. Further evaluation of its utility and impact using larger, randomized trial study design is needed to establish the long-term efficacy of this tool, particularly as it relates to patient clinical outcomes.
Supplementary Material
Acknowledgments
This work was presented in abstract form at the National Kidney Disease Education Program Coordinating Panel Meeting and the American Society of Nephrology’s Kidney Week meeting in Philadelphia, November 8–13, 2011.
Support: This work was supported in part by T32 DK007569 and a Clinical Scientist in Nephrology Fellowship Grant from the American Kidney Fund (Dr Wright Nunes). Additional support was provided by the National Institute of Diabetes and Digestive and Kidney Diseases by awards K23DK080952 and K23DK080952-02S1 (Dr Cavanaugh), K24DK77875 and P60DK020593 (Dr Elasy), and K24DK062849 (Dr Ikizler). Dr. Cavanaugh is also supported by the American Society of Nephrology Carl W. Gottschalk Research Scholar Grant. The funding agencies did not have a role in the design, conduct, or reporting of the study.
Footnotes
Financial Disclosure: The authors declare that they have no other relevant financial interests.
Item S1: Structured interview questions for physicians regarding the education worksheet intervention.
Note: The supplementary material accompanying this article (doi:_______) is available at www.ajkd.org
Descriptive Text for Online Delivery
Hyperlink: Supplementary Item S1 (PDF)
About: Structured interview questions for physicians regarding the education worksheet intervention.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Delivery CotNQRoHC, Services BoHC. Envisioning the National Health Care Quality Report. The National Academies Press; 2001. [PubMed] [Google Scholar]
- 2.Wright JA, Wallston KA, Elasy TA, Ikizler TA, Cavanaugh KL. Development and results of a kidney disease knowledge survey given to patients with CKD. Am J Kidney Dis. 2011;57(3):387–395. doi: 10.1053/j.ajkd.2010.09.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cavanaugh KL, Wingard RL, Hakim RM, Elasy TA, Ikizler TA. Patient dialysis knowledge is associated with permanent arteriovenous access use in chronic hemodialysis. Clin J Am Soc Nephrol. 2009;4(5):950–956. doi: 10.2215/CJN.04580908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Devins GM, Mendelssohn DC, Barre PE, Binik YM. Predialysis psychoeducational intervention and coping styles influence time to dialysis in chronic kidney disease. Am J Kidney Dis. 2003;42(4):693–703. doi: 10.1016/s0272-6386(03)00835-7. [DOI] [PubMed] [Google Scholar]
- 5.Curtin RB, Sitter DC, Schatell D, Chewning BA. Self-management, knowledge, and functioning and well-being of patients on hemodialysis. Nephrol Nurs J. 2004;31(4):378–386. 396. quiz 387. [PubMed] [Google Scholar]
- 6.Devins GM, Mendelssohn DC, Barre PE, Taub K, Binik YM. Predialysis psychoeducational intervention extends survival in CKD: a 20-year follow-up. Am J Kidney Dis. 2005;46(6):1088–1098. doi: 10.1053/j.ajkd.2005.08.017. [DOI] [PubMed] [Google Scholar]
- 7.Mason J, Khunti K, Stone M, Farooqi A, Carr S. Educational interventions in kidney disease care: a systematic review of randomized trials. Am J Kidney Dis. 2008;51(6):933–951. doi: 10.1053/j.ajkd.2008.01.024. [DOI] [PubMed] [Google Scholar]
- 8.Couper MP, Singer E, Levin CA, Fowler FJ, Jr, Fagerlin A, Zikmund-Fisher BJ. Use of the Internet and ratings of information sources for medical decisions: results from the DECISIONS survey. Med Decis Making. 2010;30(5 Suppl):106S–114S. doi: 10.1177/0272989X10377661. [DOI] [PubMed] [Google Scholar]
- 9.National Kidney Foundation. KDOQI Clinical Practice Guidelines and Clinical Practice Recommendations for Diabetes and Chronic Kidney Disease. Am J Kidney Dis. 2007;49(2 Suppl 2):S12–154. doi: 10.1053/j.ajkd.2006.12.005. [DOI] [PubMed] [Google Scholar]
- 10.Schillinger D, Piette J, Grumbach K, et al. Closing the loop: physician communication with diabetic patients who have low health literacy. Arch Intern Med. 2003;163(1):83–90. doi: 10.1001/archinte.163.1.83. [DOI] [PubMed] [Google Scholar]
- 11.Pignone M, DeWalt DA, Sheridan S, Berkman N, Lohr KN. Interventions to improve health outcomes for patients with low literacy. A systematic review. J Gen Intern Med. 2005;20(2):185–192. doi: 10.1111/j.1525-1497.2005.40208.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.National Institutes of Health. Publication Number 08-6220. 2008. National Kidney Disease Education Program: How Well Are Your Kidneys Working? [Google Scholar]
- 13.Davis TC, Long SW, Jackson RH, et al. Rapid estimate of adult literacy in medicine: a shortened screening instrument. Fam Med. 1993;25(6):391–395. [PubMed] [Google Scholar]
- 14.Levey AS, Coresh J, Balk E, et al. National Kidney Foundation practice guidelines for chronic kidney disease: evaluation, classification, and stratification. Ann Intern Med. 2003;139(2):137–147. doi: 10.7326/0003-4819-139-2-200307150-00013. [DOI] [PubMed] [Google Scholar]
- 15.Cohen J. A power primer. Psychol Bull. 1992;112(1):155–159. doi: 10.1037//0033-2909.112.1.155. [DOI] [PubMed] [Google Scholar]
- 16.Williams RL. A note on robust variance estimation for cluster-correlated data. Biometrics. 2000;56(2):645–646. doi: 10.1111/j.0006-341x.2000.00645.x. [DOI] [PubMed] [Google Scholar]
- 17.Wright Nunes JA, Wallston KA, Eden SK, Shintani AK, Ikizler TA, Cavanaugh KL. Associations among perceived and objective disease knowledge and satisfaction with physician communication in patients with chronic kidney disease. Kidney Int. 2011;80(12):1344–1351. doi: 10.1038/ki.2011.240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rantanen M, Kallio T, Johansson K, Salantera S, Virtanen H, Leino-Kilpi H. Knowledge expectations of patients on dialysis treatment. Nephrol Nurs J. 2008;35(3):249–255. quiz 256. [PubMed] [Google Scholar]
- 19.Narva AS, Briggs M. The National Kidney Disease Education Program: improving understanding, detection, and management of CKD. Am J Kidney Dis. 2009;53(3 Suppl 3):S115–120. doi: 10.1053/j.ajkd.2008.05.038. [DOI] [PubMed] [Google Scholar]
- 20.Collins AJ, Gilbertson DT, Snyder JJ, Chen SC, Foley RN. Chronic kidney disease awareness, screening and prevention: rationale for the design of a public education program. Nephrology (Carlton) 2010;15 (Suppl 2):37–42. doi: 10.1111/j.1440-1797.2010.01312.x. [DOI] [PubMed] [Google Scholar]
- 21.Young HN, Chan MR, Yevzlin AS, Becker BN. The rationale, implementation, and effect of the Medicare CKD education benefit. Am J Kidney Dis. 2011;57(3):381–386. doi: 10.1053/j.ajkd.2010.10.056. [DOI] [PubMed] [Google Scholar]
- 22.Harris KJ, Catley D, Good GE, Cronk NJ, Harrar S, Williams KB. Motivational interviewing for smoking cessation in college students: a group randomized controlled trial. Prev Med. 2010;51(5):387–393. doi: 10.1016/j.ypmed.2010.08.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Petersen CB, Severin M, Hansen AW, Curtis T, Gronbaek M, Tolstrup JS. A population-based randomized controlled trial of the effect of combining a pedometer with an intervention toolkit on physical activity among individuals with low levels of physical activity or fitness. Prev Med. 2012;54(2):125–130. doi: 10.1016/j.ypmed.2011.12.012. [DOI] [PubMed] [Google Scholar]
- 24.Wilson DB, Jones RM, McClish D, Westerberg AL, Danish S. Fruit and vegetable intake among rural youth following a school-based randomized controlled trial. Prev Med. 2012;54(2):150–156. doi: 10.1016/j.ypmed.2011.11.005. [DOI] [PubMed] [Google Scholar]
- 25.Jago R, Sebire S. Publishing pilot and feasibility evaluations of behavioural interventions: Implications for Preventive Medicine. Prev Med. 2012 doi: 10.1016/j.ypmed.2012.07.005. [DOI] [PubMed] [Google Scholar]
- 26.Zikmund-Fisher BJ, Fagerlin A, Ubel PA. Improving understanding of adjuvant therapy options by using simpler risk graphics. Cancer. 2008;113(12):3382–3390. doi: 10.1002/cncr.23959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Jennette CE, Vupputuri S, Hogan SL, Shoham DA, Falk RJ, Harward DH. Community perspectives on kidney disease and health promotion from at-risk populations in rural North Carolina, USA. Rural Remote Health. 2010;10(2):1388. [PubMed] [Google Scholar]
- 28.Ledford CJ, Villagran MM, Kreps GL, et al. “Practicing medicine”: patient perceptions of physician communication and the process of prescription. Patient Educ Couns. 2010;80(3):384–392. doi: 10.1016/j.pec.2010.06.033. [DOI] [PubMed] [Google Scholar]
- 29.Bonner A, Lloyd A. Exploring the information practices of people with end-stage kidney disease. J Ren Care. 2012;38(3):124–130. doi: 10.1111/j.1755-6686.2012.00258.x. [DOI] [PubMed] [Google Scholar]
- 30.University of Michigan Library. M Library Plain Language Dictionary. Regents University of Michigan; 2012. [Accessed December 18]. http://lib.umich.edu. [Google Scholar]
- 31.Department of Health and Human Services, National Center for Health Marketing, Centers for Disease Control and Prevention. Publication #07-151(NE)/092607. 2007. Plain Language Thesaurus for Health Communications. [Google Scholar]
- 32.Bauer C, Melamed ML, Hostetter TH. Staging of chronic kidney disease: time for a course correction. J Am Soc Nephrol. 2008;19(5):844–846. doi: 10.1681/ASN.2008010110. [DOI] [PubMed] [Google Scholar]
- 33.U.S. Renal Data System. USRDS 2010 Annual Report: Atlas of Chronic Kidney Disease and End-Stage Renal Disease in the United States. National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases; Bethesda, MD: 2010. [Google Scholar]
- 34.Hauck WW, Neuhaus JM, Kalbfleisch JD, Anderson S. A consequence of omitted covariates when estimating odds ratios. J Clin Epidemiol. 1991;44(1):77–81. doi: 10.1016/0895-4356(91)90203-l. [DOI] [PubMed] [Google Scholar]
- 35.Byrne J, Khunti K, Stone M, Farooqi A, Carr S. Feasibility of a structured group education session to improve self-management of blood pressure in people with chronic kidney disease: an open randomised pilot trial. BMJ Open. 2011;1(2):e000381. doi: 10.1136/bmjopen-2011-000381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Yen M, Huang JJ, Teng HL. Education for patients with chronic kidney disease in Taiwan: a prospective repeated measures study. J Clin Nurs. 2008;17(21):2927–2934. doi: 10.1111/j.1365-2702.2008.02348.x. [DOI] [PubMed] [Google Scholar]
- 37.Nickolas TL, Frisch GD, Opotowsky AR, Arons R, Radhakrishnan J. Awareness of kidney disease in the US population: findings from the National Health and Nutrition Examination Survey (NHANES) 1999 to 2000. Am J Kidney Dis. 2004;44(2):185–197. doi: 10.1053/j.ajkd.2004.04.023. [DOI] [PubMed] [Google Scholar]
- 38.Stevens LA, Li S, Kurella Tamura M, et al. Comparison of the CKD Epidemiology Collaboration (CKD-EPI) and Modification of Diet in Renal Disease (MDRD) study equations: risk factors for and complications of CKD and mortality in the Kidney Early Evaluation Program (KEEP) Am J Kidney Dis. 2011;57(3 Suppl 2):S9–16. doi: 10.1053/j.ajkd.2010.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Pereira BJ. Optimization of pre-ESRD care: the key to improved dialysis outcomes. Kidney Int. 2000;57(1):351–365. doi: 10.1046/j.1523-1755.2000.00840.x. [DOI] [PubMed] [Google Scholar]
- 40.Shah A, Fried LF, Chen SC, et al. Associations between access to care and awareness of CKD. Am J Kidney Dis. 2012;59(3 Suppl 2):S16–23. doi: 10.1053/j.ajkd.2011.10.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Patwardhan MB, Samsa GP, Matchar DB, Haley WE. Advanced chronic kidney disease practice patterns among nephrologists and non-nephrologists: a database analysis. Clin J Am Soc Nephrol. 2007;2(2):277–283. doi: 10.2215/CJN.02600706. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.