Abstract
Purpose
To describe the physical activity (PA) and sedentary behaviors of postpartum Latinas who are overweight or obese prior to initiating Madres para la Salud, a social-support mediated walking intervention to promote postpartum weight loss.
Methods
139 postpartum (13.6 ± 7.7 weeks since childbirth) women (age = 28.3 ± 5.6 years and BMI = 29.7 ± 3.5 kg.m2), recruited from Phoenix area Latino-serving organizations completed the Stanford Brief Activity Survey (SBAS) and concurrently wore an accelerometer (AG) and a pedometer for 7-days, and kept a PA record (PAR).
Results
Most were classified as inactive and lightly active on the SBAS (51% inactive, 37% light, 11% moderate). Most time was spent in sedentary (512.0 ± 169.9 min.d−1) and light-intensity PA (242.4 ± 51.4 min.d−1) with less time in moderate-intensity lifestyle (78.3 ± 39.9 min.d−1), moderate-intensity walking (16.6 ± 14.4 min.d−1), and vigorous-intensity PA (0.34 ± 1.5 min.d−1). Pedometer steps.d−1 were low (total = 4,973 ± 2,202 steps; aerobic = 412 ± 774 steps) with most participants rated as sedentary (61%) or low-active (28.1%). Consistent with objective PA measures, PARs showed more time spent in light-intensity PAs such as home care, cooking, child- and self care tasks, occupation, religious events, and watching television.
Conclusion
By and large, the postpartum Latinas enrolled spent most of their day in low-intensity activity levels with little time spent in health-enhancing PA levels/behaviors. This demographic should be the focus of PA interventions to increase PA to health enhancing levels.
Keywords: Exercise, Hispanics, Accelerometer, Physical Activity Record, Self Report Questionnaire, Pedometer
INTRODUCTION
Lifestyle behaviors associated with reduced risks for morbidity and mortality from chronic diseases include participating in regular physical activity (PA), maintaining normal values for blood lipids, blood pressure, and body weight, and not smoking [10, 15, 20]. Many women of Mexican ethnicity (referred to as Latinas) living in the U.S. have low levels of health-enhancing PA (48.2%) [45] and elevated rates of overweight and obesity (65.4%) [14] which put them at risk for type 2 diabetes and other chronic diseases. Additionally, decreases in aerobic fitness [43] and increases in depression [13] are observed during the postpartum period. While the national average for postpartum depression is 10–20%, researchers have found rates approaching 45% for Hispanic women living in the United States [9, 13].
Childbearing is a critical time in women’s developmental trajectory as it is a time when women may gain excessive weight [40]. Some data show that nearly 50% of U.S. women gained more than the recommended weight gain during pregnancy [40]. Failure to lose pregnancy weight following childbirth contributes to obesity in this subgroup, with subsequent impact on obesity-related risk and illness [17]. In 2009, the Institute of Medicine (IOM) [38] published new target gestational weight gain recommendations to address gestational weight gain based on pre pregnancy body mass. Women who begin pregnancy as “underweight” (BMI <18.5 kg/m2) are encouraged to gain between 28 and 40 lbs during pregnancy; women who are overweight (BMI 25.0–29.9 kg/m2) should restrict weight gain to between 15 and 25 lbs and obese women (BMI ≥30 kg/m2) should be encouraged to gain no more than 20 lbs over the 40 weeks of gestation (IOM, 2009). The IOM reported that the distribution of BMI among women of childbearing age had substantially increased in 2009 compared with the 1980s and that a greater proportion of women are entering pregnancy overweight or obese. Accordingly, the postpartum period is an opportune time for losing pregnancy associated weight gain to reduce the risks for obesity [47]. Regular PA with sufficient frequency and duration to accumulate at least 150 min.wk−1 (e.g., 30 min.d−1 and 5 d.wk−1) of moderate-intensity activity or at least 75 min.wk−1 (e.g., 25 min.d−1 and 3 d.wk−1) of vigorous-intensity activity can help to reduce weight following childbirth [18, 46].
Most studies reporting PA behaviors during postpartum have relied on the use of subjective methods to assess PA such as questionnaires, recalls, and records to assess the frequency, intensity, duration, and type of PA performed [6, 7, 12, 26, 47, 50]. Østbye et al. [35] used the 7-Day PA Recall survey [8] to evaluate predictors of postpartum weight loss among women enrolled in the Active Mothers Postpartum Study. In the same study, Durham et al. [12] reported overweight and obese mothers spent more time in sedentary and light activities and only 34% met national PA guidelines as compared with normal weight status mothers. Healthier eating and increased PA were significantly related with weight loss after controlling for all other predictors. Walker et al. [47] also used the 7-Day PA Recall in the Austin New Mothers Study to describe PA levels in low-income women for 12-months following childbirth. An overall profile of low PA was observed with most time spent in light intensity activity.
Few studies have used objective measures or a combination of objective and subjective methods to assess PA in postpartum women. Objective measures of PA include pedometers and accelerometers. Maturi et al. [32] used pedometers to encourage walking up to 10,000 steps in a clinical trial to promote pregnancy-related weight loss. Step counts increased from 3,249 to 9,960 steps in the intervention group with significant reductions in weight loss compared with an inactive control group. Montpetit et al. [33] used a PA questionnaire and pedometers in modeling factors that contributed to postpartum weight retention. Results showed PA was significantly associated with weight loss. No studies have reported using accelerometers to record PA levels during the postpartum. There is value in assessing PA behaviors using multiple assessment methods. Objective PA monitors provide information about the volume of activity performed such as steps walked or time spent in different intensities of movement. In particular, accelerometers capture the frequency, duration, and intensity of ambulatory activities as they are accumulated throughout the day. Subjective measures allow examination of the frequency and duration of types of activities performed. Such detail about PA behaviors allows interventionists to identify time spent in different types and intensities of activities in postpartum women and provide targeted strategies to increase PA that may be meaningful to study participants. This is of particular importance when designing culturally-appropriate PA interventions for ethnic subgroups.
The purpose of this report is to describe the baseline PA behaviors of sedentary, postpartum Latina women. PA was measured with objective measures of accelerometers and pedometers and with subjective measures of questionnaires and record books.
METHODS
Overview
In this paper, we describe the baseline PA levels of postpartum Latinas who were overweight or obese prior to initiating Madres para la Salud, a social-support mediated walking intervention to promote postpartum weight loss. One hundred thirty-nine Latinas (28.3 ± 5.6 years) volunteered for this study and were assessed at baseline for the PA levels prior to randomization into a control or intervention group. Detailed descriptions of the Madres para la Salud study design and measures is published elsewhere [24, 39].
Participants were recruited from a Spanish language radio station, public housing community Centers, word-of-mouth, flyers, and community organizations serving Latino residents in the greater Phoenix, Arizona area. Recruitment staff followed a systematic process in contacting agencies and inviting potential participants to participate that included reading a script to explain the study purpose, procedures, benefits and risks, and eligibility criteria. Eligibility criteria included (a) habitually sedentary as measured by the Stanford Brief Activity Survey (SBAS) (< 2.5 hours of moderate-intensity PA a week) but physically able to participate in moderate-intensity walking, (b) self-identified Latina, (c) 18 to 40 years of age, (d) 6-weeks to 6-months post childbirth, and (e) BMI of 25 to 35 kg/m2. Women interested in participation were scheduled for a screening visit. All participants read and signed an informed consent document approved by the Arizona State University IRB prior to participating in this study.
Physical Activity Assessment
Participants completed the SBAS, wore an ActiGraph GT3X accelerometer (AG) and an Omron HJ-720ITC pedometer (Omron) for seven days, and kept a PA record (PAR).
Stanford Brief Activity Survey (SBAS) was completed to classify the participants PA levels prior to study participation [42]. The SBAS is a quick screening tool to assess PA levels that takes little time to complete and does not rely on the recall of time spent in various types of PA. The SBAS rates occupational and leisure-time PA to compute a 5-point rating from inactive to very hard PA. The SBAS was self-completed in Spanish or English language as needed. Study investigators translated the SBAS into Spanish based on translation procedures outlined by Martinez et al.[28]. The validity evidence and test-retest reliability for the English language SBAS was determined in 1,010 adults (67.1% Caucasian) from the Atherosclerotic Disease Vascular Function and Genetic Epidemiology study, showing a strong, dose-response relation with the prevalence of metabolic syndrome and with factors associated with metabolic syndrome (e.g., minutes of moderate-intensity PA, energy expenditure, fasting glucose and insulin, triglycerides, HDL-C) (p < .01). Two-year test-retest reliability was r = 0.62 (p < .001) [41]. The validity evidence and test-retest reliability for the Spanish language SBAS was determined in a convenience sample of 37Mexican-American adults. The validity evidence against ActiGraph-determined time spent in moderate- and vigorous-intensity PA was r = 0.45 (p < .015). The one-week test-retest reliability was r = 0.62 (p < .01) [11].
Omron HJ-720ITC pedometers (Warminster, PA) were worn for seven days to identify the volume of walking during daily lifestyle behaviors. The Omron pedometer (Omron) is a small, lightweight electronic device worn on the waist that provides an objective, nonintrusive, validated estimate of walking levels in both healthy and overweight and obese adults [19, 21]. The Omron has acceptable validity evidence during prescribed walking speeds described as slow (2.0 mph), moderate (3.0 mph), and very brisk (4.0 mph) with an absolute percentage error [(pedometer steps – actual steps)/actual steps]×100 of 2.3% ± 2.8% across all walking speeds [21]. Test-retest reliability evidence across the three walking speeds is sufficient with a coefficient of variation ranging from 2.8% to 3.3% [21]. Participants were instructed to wear the Omron attached to their belt at the level of their waist, over their right hip, for seven days from the time they awoke until the time they went to bed. Prior to use, the monitors were initialized using a proprietary website. One week later, participants returned the monitor to the study manager who downloaded the data into a database. Data included total steps.d−1 and total steps.wk−1, moderate-intensity min.d−1 and min.wk−1 of walking at a cadence associated with moderate-intensity exercise (> 100 steps.min−1). To characterize PA levels with at least 80% reliability, Tudor-Locke et al.[44] have determined that subjects need to wear the pedometer continuously for 3–4 days to characterize moderate and vigorous activity patterns and for 7 days to characterize physical inactivity levels.
ActiGraph GT1M accelerometers (ActiGraph LLC, Pensacola, FL) were worn concurrently over the right hip with the Omron pedometer to obtain an objective measure of the time spent in ambulatory PA’s of different intensities. The ActiGraph is a small, battery operated electronic motion solid state sensor (micro-electro-mechanical systems) designed to measure the rate and magnitude of body movement in a vertical plane (accelerations). Output data are digitized at a rate of thirty times per second with intensity data recorded in one minute epochs (sampling interval). It is used to evaluate movement characteristics, validate PA questionnaires and quantify associations between PA levels and health outcomes [48]. The ActiGraph outputs data as counts per minute (cpm) that reflect: (a) the intensity of movement based on the frequency of acceleration deflections and (b) the duration of sustained period of the deflections. Cut-points developed from controlled laboratory experiments were used from the accelerometer counts per minute (cpm) data to estimate the minutes of activity at various intensity levels: sedentary (< 100 cpm) [31], light (100–759 cpm) and moderate-lifestyle activities (760–1951 cpm) [29], moderate-walking (1952–5725 cpm) and vigorous-intensity activities (> 5725 cpm) [16]. Count data were downloaded to an excel spreadsheet using ActiGraph 5.0 software and then translated into min.d−1 at the designated intensities using statistical program developed for SAS 9.2 (SAS, Cary, NC).
Participants were instructed to wear the ActiGraph for seven days. Each day they wore the monitor, participants were instructed to write the time they put the monitor on in the morning, when they took the monitor off before going to bed, and other times when they did not wear the monitor (e.g., bathing, swimming, etc.). The ActiGraph was programmed to capture accelerations at 60-second epochs beginning at midnight of the day the instrument was provided to the participant. The ActiGraph activity monitor data were directly downloaded into a computer as an electronic data file. To characterize activity levels with at least 80% reliability, Matthews et al. [30] determined that participants needed to wear the ActiGraph on a belt around the waist continuously for 3–4 days to characterize moderate- and vigorous-intensity movements and 7 days to characterize inactivity levels. Thus, 3–7 days of data with counts recorded for ≥10 h.d−1 were required for inclusion in the database. Prior to analyses, data for each subject was scanned and removed if (a) accelerometer data indicated ≤10 h.d−1 of movement counts, (b) < 3 days of recorded movement, and (c) there was no indication of PA on the activity calendar and movement counts on the ActiGraph. Nineteen participants did not have complete ActiGraph data that met the inclusion criteria, which gave us a compliance rate of 86% (see Table 2).
Table 2.
Baseline physical activity data for Madres para la Salud study participants (N=139)
| Variable | N | N (%) | Mean ± SD | Median (25th, 75th Quartiles) |
Minimum - Maximum |
|---|---|---|---|---|---|
| SBAS Category (%) | 139 | ||||
| Inactive | 72 (51.4) | ||||
| Light | 52 (37.1) | ||||
| Moderate | 15 (10.7) | ||||
| Hard | 0 (0) | ||||
| Very Hard | 0 (0) | ||||
| Pedometer | |||||
| Total steps.d−1 | 137a | 4,973 ± 2202 | 4,539 (3603, 6119) | 1,433 – 15,711 | |
| No. Steps > 100 steps.min−1 | 137 | 412b ± 774 | 0 (0, 573) | 0 – 5,014 | |
| Minutes spent walking >100 steps.min−1 | 137 | 4 ± 7 | 0 (0, 6) | 0 – 42 | |
| Pedometer Categories (steps.d−1) | 137 | ||||
| Sedentary (<5,000) | 83 (61.0) | ||||
| Low Active (5,000–7,499) | 39 (28.1) | ||||
| Somewhat active (7,500–9,999) | 11 (8.0) | ||||
| Active (10,000–12,499) | 2 (1.45) | ||||
| Highly active (>12,500) | 2 (1.45) | ||||
| ActiGraph Accelerometer (min.d−1) | 120c | ||||
| Sedentary (1–100 ctmd) | 512.0 ± 169.9 | 478.1 (407.4, 543.9) | 240.7 – 1061.2 | ||
| Light (101–759 ctm) | 242.4 ± 51.4 | 236.1 (205.3, 273.5) | 135.5 – 390.9 | ||
| Mod Lifestyle (760–1951 ctm) | 78.3 ± 39.9 | 75.6 (50.4, 98.2) | 13.2 – 317.3 | ||
| Mod Walking (1952–5724 ctm) | 16.7 ± 14.4 | 12.4 (5.7, 24.3) | 0.5 – 63.0 | ||
| Vigorous (≥5725 ctm) | 0.3 ± 1.5 | 0 (0, 0) | 0.0 – 10.9 |
Physical activity records (PAR) were maintained to identify the type, frequency, duration, and intensity of activities performed during the same period when the pedometers and accelerometers were worn. Two versions of PA records were maintained: a 7-day PAR (PAR-7) kept by participants (n = 88; 66%) and a 3-day PA (PAR-3) administered to participants by the study staff as a recall instrument (n = 46; 34%). The PAR was used to identify daily activity and inactivity patterns of study participants. Used previously in the Cross Cultural Activity Participation Study with minority women, the PAR-7 requires participants to (a) record the time of day they start an activity (e.g., 7 am), (b) write a description of the activity (e.g., feeding baby), (c) indicate their body position while performing the activity (reclining, sitting, standing, walking), (d) indicate their perceived intensity of the activity (light, moderate, vigorous), and (e) identify the purpose of the activity (e.g., self-care, child-care, household chores, inactivity, walking, transportation, occupation, etc.) [4]. The categories used to identify the purpose of the activity are those listed in the 2011 Compendium of Physical Activities (Compendium) [3]. Participants entered activities into the PAR-7 from the time they awoke to the time they went to bed. A typical day of recording produced from 60 to 100 activities recorded. Data were entered in either English (n = 72; 54%) or Spanish (n = 62; 46%) based on the participant’s preferred language.
Some participants found the PAR-7 too time consuming to complete which resulted in low compliance for completing the records. Because of this, we determined that a simpler method that would yield similar information about the primary types and intensities of PA’s performed during the day and that would allow us to identify the same movement types recorded in the PAR-7. The PAR-3 was modeled after the children’s 3-day PA Recall (3DPAR) developed by Pate et al. [36] that has respondents identify their primary activity performed every 30 minutes. Instead of having a pre-determined list of activities for respondents as used in the 3DPAR, participants indicated the primary activity performed during 30 minute periods, such as cooking, watching television, child care, driving a car, etc. Similar to the PAR-7, for each activity listed, participants indicated their body position during the activity, their perceived effort, and identified the purpose of the activity performed. Comparison of the versions is presented in the results section of this paper.
PA records were coded by bilingual study staff by using the written information about the type, intensity, and purpose of the activities performed to assign a 5-digit activity code from the 2011 Compendium [3]. The time each activity was started, codes for the body position, perceived intensity, and the 5-digit code were recorded into an Excel spread sheet. The data were scored using a SAS 9.2 program written for this study that outputs results as min.d−1 and MET-min.d−1 for total activity, activity by intensity levels, and activity by categories of activities. The term MET stands for metabolic equivalent which is defined as the activity metabolic rate divided by the resting metabolic rate [22]. The MET levels presented in the 2011 Compendium define the resting metabolic rate (1 MET) = 3.5 ml.kg−1.min−1. MET intensity categories are defined as sedentary (1.0–1.5), light (1.6–2.9), moderate (3.0–5.9), and vigorous (≤ 6.0).
Statistical Analyses
Data were analyzed using SAS 9.2 (SAS Inc, Cary, NC). Means and standard deviations were computed for continuous data. Percentages were computed for nominal and ordinal data t-tests were used to compare the min.d−1 between the PAR-3 and PAR-7 and between the PAR completed in English and Spanish languages. The Satterthwaite approximation for degrees of freedom was used to assess equality of variances between the groups.
RESULTS
Table 1 shows descriptive data for the study participants. Employment levels were low (n = 33, 23.7%) and few participants had higher than a high school education (20%). Most earned less than $30,000 per year and were married or living together. The number of children in the home ranged from 1 to 12 with the average of 3 children.
Table 1.
Baseline descriptive data for Madres para la Salud study participants (N=139)
| Variable | Sample N |
N (%) | Mean ± SD | Minimum - Maximum |
|---|---|---|---|---|
| Age (yr) | 139 | 28.3 ± 5.6 | 18 – 39 | |
| BMI (kg/htm2)a | 139 | 29.7 ± 3.5 | 23.4 – 41.5 | |
| Baseline weight (lbs) | 139 | 161.6 ± 21.8 | 119–221.8 | |
| Education (%) | 139 | |||
| None | 1 (0.7) | |||
| Elementary | 28 (20.1) | |||
| Some High School | 21 (15.1) | |||
| High School | 61 (43.9) | |||
| Some College | 18 (12.9) | |||
| College Graduate | 10 (7.2) | |||
| Employment (%) | 139 | |||
| Never Employed | 25 (17.9) | |||
| Unemployed | 81 (57.9) | |||
| Part-Time Job | 18 (12.9) | |||
| Full-Time Job | 15 (10.7) | |||
| Marital Status (%) | 139 | |||
| Single | 14 (10.1) | |||
| Married | 63(45.3) | |||
| Divorced/Separated | 4 (2.9) | |||
| Living Together | 58 (41.7) | |||
| Incomeb | 136 | |||
| 0–10,000 | 31 (22.3) | |||
| 10,000–19,999 | 65 (46.8) | |||
| 20,000–29,999 | 21 (15.1) | |||
| 30,000–49,999 | 11 (7.9) | |||
| 50,000–74,999 | 4 (2.9) | |||
| 75,000 + | 4 (2.9) | |||
| Number Children Living at Home | 139 | |||
| 1 | 17 (12.2) | |||
| 2–3 | 74 (53.3) | |||
| 4–5 | 38 (27.3) | |||
| 6+ | 10 (7.2) |
BMI = body mass index
missing income data for 3 participants
Table 2 shows the PA data collected by the SBAS, pedometer and accelerometer. Most participants were categorized in the inactive-to-low PA groups on the SBAS. Likewise, most women (89.1%) were sedentary or low active with 5,000 steps.d−1 or fewer recorded on the pedometers of which only 412 steps.d−1 were classified as aerobic intensity. ActiGraph wear time for the 120 participants who met the ActiGraph inclusion criteria was 849.7 ± 140.6 min.d−1 or about 14.1 h.d−1. Sixty percent of the ActiGraph wear-time period was in the inactive category and 28.5% was categorized as light-intensity. The remaining time was categorized as moderate-lifestyle, moderate-walking and vigorous-intensity.
Table 3 shows data from the PA records for time spent in reclining, sitting, standing, and walking body positions. Inclusive of sleep, most time was spent in a reclining position with progressively lesser time spent in sitting, standing, and walking body positions.
Table 3.
Mean and standard deviation minutes per day and percent of the day spent by body position based on recordings in the physical activity records (n=134)
| Variable | Mean ± SD | Minimum - Maximum |
|---|---|---|
| Reclining | 610 ± 101 (42%) |
366 – 900 |
| Sitting | 399 ± 118 (27%) |
158 – 765 |
| Standing | 280 ±122 (19%) |
30 – 700 |
| Walking | 163 ± 97 (11%) |
30 – 603 |
Table 4 shows the time spent in PA categories as recorded on the PAR-3 and PAR-7 and by preferred language. Nearly twice as many women kept the PAR for 7 days (n=88) as compared with 3 days (n=46). PAR’s from five participants were incomplete and unable to be scored. All women recorded home care, cooking, and childcare activities on both versions of the PAR. Fewer women recorded other activities on the both PAR types. Differences in the time reported for activities on the PAR-3 and PAR-7 ranged from 2 to 60 minutes. Compared with the PAR-3, participants completing the PAR-7 reported significantly more time in walking for exercise, and less time in childcare activities, walking with children, and conditioning and sports activities. There were no differences between the PAR-3 and PAR-7 for minutes spent in home care and cooking, general inactivity, self care, watching television, occupation, religious activities and lawn and garden activities. For the English and Spanish PARs, a more women completed the PARs in English (n=72) than in Spanish (n=62). Differences in the time reported for activities on the English and Spanish PARs ranged from 0 to 58 minutes. Compared with the Spanish records, those completing the records in English reported significantly more time in child care, watching television, walking with children, and conditioning and sports, and less time in home care and cooking, general inactivity, religious activities, and walking for exercise. There were no differences between English and Spanish PARs for the amount of time spent in self care, transportation, miscellaneous walking, leisure/recreation, occupation, and lawn and gardening activities.
Table 4.
Comparison of the means and standard deviations for the PA Record minutes per day completed for 3- and 7 days and completed in English and Spanish language (N = 134)
| Activity | 3-day PAR Mean ± SD |
7-day PAR Mean ± SD |
Diff Min.d−1 |
p- value |
English 3- and 7-day PAR Mean ± SD |
Spanish 3- and 7-day PAR Mean ± SD |
Diff Min.d−1 |
p- value |
|---|---|---|---|---|---|---|---|---|
| (n = 46) | (n = 88) | (n = 72) | (n = 62) | |||||
| Home Care and Cooking | 397 ± 141 (46) |
352 ± 113 (88) |
45 | .08 | 353 ± 139 (71) |
384 ± 106 (63) |
−31 | .03 |
| Child Care | 184 ± 98 (46) |
148 ± 69 (88) |
36 | .03 | 165 ± 91 (71) |
155 ± 70 (63) |
10 | .04 |
| General Inactivity | 64 ± 59 (39) |
75 ± 62 (88) |
−11 | .77 | 64 ± 51 (64) |
79 ± 70 (63) |
−15 | .01 |
| Self Care | 99 ± 30 (45) |
106 ± 36 (88) |
−8 | .14 | 100 ± 34 (70) |
108 ± 34 (63) |
−7 | .98 |
| Watching TV | 121 ± 75 (44) |
123 ± 63 (86) |
−2 | .18 | 131 ± 76 (69) |
112 ± 53 (61) |
19 | .005 |
| Transportation | 87 ± 42 (40) |
81 ± 38 (81) |
5 | .44 | 83 ± 40 (64) |
83 ± 38 (57) |
0 | .73 |
| Miscellaneous Walking | 34 ± 58 (24) |
48 ± 43 (71) |
15 | .05 | 54 ± 49 (47) |
50 ± 46 (48) |
4 | .72 |
| Walking with Children | 66 ± 43 (27) |
41 ± 33 (45) |
25 | .01 | 58 ± 40 (41) |
40 ± 35 (31) |
19 | .04 |
| Walking for Exercise | 42 ± 23 (14) |
57 ± 48 (46) |
−15 | .006 | 43 ± 26 (26) |
62 ± 53 (34) |
−18 | .004 |
| Leisure/Recreation | 83 ± 78 (14) |
58 ± 51 (36) |
25 | .05 | 75 ± 62 (26) |
54 ± 57 (24) |
21 | .70 |
| Occupation | 254 ± 185 (11) |
226 ± 183 (29) |
27 | .90 | 264 ± 182 (19) |
206 ± 181 (21) |
58 | .99 |
| Religious Activities | 105 ± 54 (5) |
103 ± 84 (24) |
2 | .40 | 102 ± 45 (10) |
104 ± 93 (19) |
−2 | .03 |
| Conditioning and Sports | 109 ± 88 (6) |
49 ± 36 (20) |
60 | .003 | 83 ± 65 (14) |
39 ± 35 (12) |
44 | .04 |
| Lawn and Garden | 34 ± 8 (4) |
41 ± 27 (13) |
−7 | .06 | 43 ± 24 (7) |
37 ± 25 (10) |
6 | .92 |
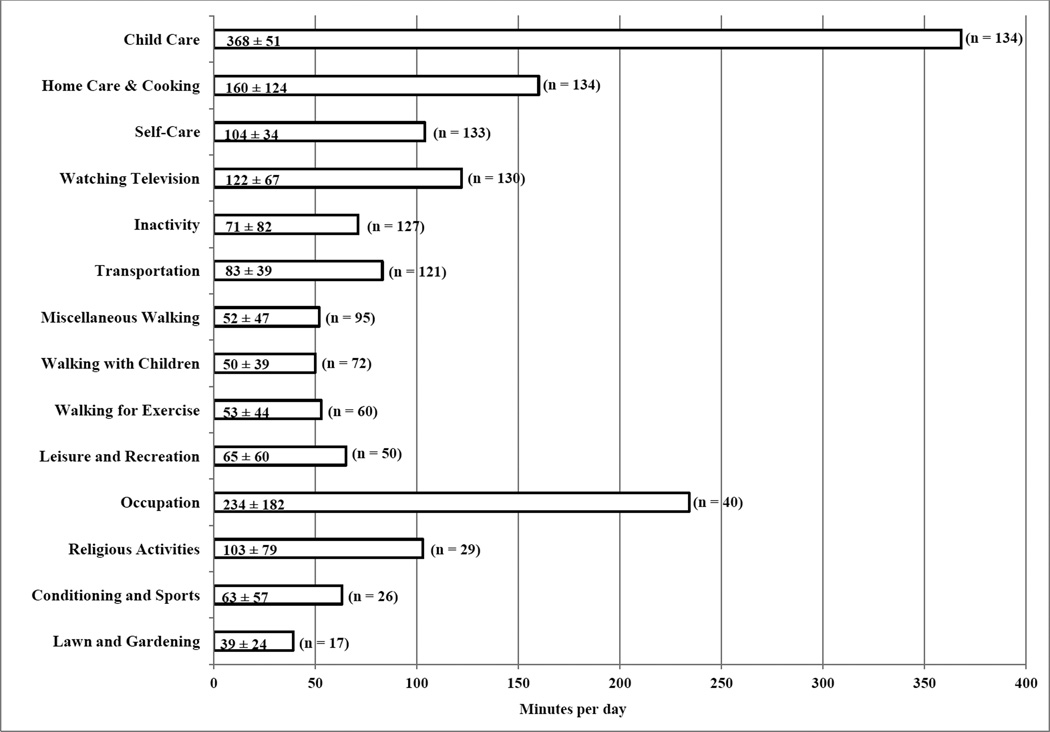
Figure 1 shows data from all PA records for time spent in different types of activities. 100% of the participants engaged in home care and cooking and child care activities. Over 90% engaged in self-care activities, transportation, watching television, and in general inactivity. Nearly half reported walking with their children. Fewer than half reported intentional PA such as leisure/recreation, walking for exercise, conditioning/sports, or working in the lawn and garden. Most time was spent in home care and cooking, occupation, general inactivity, and child care. The least amount of time was spent in lawn and garden, walking, and exercise and conditioning activities.
Figure 1.
Means and standard deviations for minutes per day spent in physical activities recorded in the baseline physical activity records. Categories were created from activity codes listed in the 2011 Compendium of Physical Activities [3]. Time is rounded to the nearest minute. The maximum sample size is 134 as five participants did not have 3 or more days of the PAR. The number in the parentheses reflects the participants reporting the activity.
DISCUSSION
Most studies measuring PA in postpartum Latina women have used questionnaires and/or pedometers to assess PA levels [6, 7, 12, 26, 47, 50] and none have used multiple subjective and objective PA measures to characterize PA levels as in the current study. We showed a consistent pattern of low engagement in health-enhancing PA on all measures in this population of sedentary, overweight or obese postpartum women. The SBAS classified 85% of the women as inactive or engaging in light-intensity PA based on a self-assessment of leisure-time and occupational PA. Pedometers classified 89% of women as sedentary or low active based on their steps taken and the ActiGraph cut-points placed women engaged in inactive or low-intensity activity for over 75% of the day. The PA records also portrayed women as having a daily routine comprised primarily of inactive and low-intensity PA. Nearly 70% (1008 min) of a 24-h period was spent in reclining and sitting positions. Subtracting an average of 576 min per night for reported sleep, 432 min or (7.2 h) was classified as spending time in reclining or sitting sedentary behaviors. Of this, 193 min (3.25 h) were spent watching TV and in general inactivity. This represents discretionary time that may be targeted for increasing active behaviors.
The richness of this PA record data is in the identification of the frequency and duration of the types of daily PA performed. Most activities recorded in the PA records were less than 3 METs with at least 95% of women engaging in household chores, child-care and self-care activities, watching television, and general inactivity. These five activities accounted for nearly 13.5 h.d−1 which was most of the time spent awake. As would be expected, the amount of time that women spent doing childcare and household chores was high, over 8 h.d−1, which far exceeded television time which was 2 h.d−1. As well, time spent in church was about equal to television time. This suggests that while watching television was highly prevalent, it was not the activity were most time was spent. Instead, obligatory activities of home and child care demanded the most time. This factor probably highlights the necessity of having multiple, shorter bouts of PA, i.e., 10 minutes as recommended by the 2008 U.S. PA Guidelines [37], to allow women to integrate activity into their daily routine rather than requiring a longer single bout PA intervention program. Walking as a health enhancing activity is encouraged for most adults.
Less than half of the women recorded intentional exercise, conditioning, walking for exercise, or recreational activities in the PA records. These findings are consistent with the eligibility criteria requiring women to engage in less than 2.5 hours of moderate-intensity PA per week. Indeed, as confirmed by the accelerometers and the PA records, the time spent in moderate- and vigorous-intensity PA’s were insufficient to meet the 2008 PA Guidelines of 150 min.wk−1 of moderate-intensity PA. This low engagement in leisure-time PA is consistent with PA surveillance systems [25] and research studies [27] showing Latinas to have a low prevalence of leisure-time PA when compared with Non-Hispanic whites other racial and ethnic groups [25]. This highlights the importance of understanding the types of PA performed by Latina’s to obtain an accurate picture of total PA levels and to design culturally-acceptable interventions to increase PA participation.
Nearly half (n = 70) of the women walked with their children and 99 women engaged in miscellaneous walking activities. Miscellaneous walking included walking in the house, shopping, visiting neighbors, going to the doctor, and other low-intensity walking activities (2.5 METs). Additionally, many women reported walking their children to school which is a low-end moderate intensity activity (3.0 METs). Walking is an activity that might be targeted for interventions because it is easily accessible and can easily fit into a woman’s obligatory household routine. Brisk walking can easily fit into short durations of 8–10 minutes at a time and repeated several times during the day. Additionally, walking with children is a positive parenting behavior that can be built into an intervention.
The ActiGraph accelerometers were worn to determine the minutes of moderate-intensity PA per day. Out of the 14.2 h.d−1 the ActiGraph monitors were worn, approximately 8.5 hours were spent in sedentary behaviors, 4 hours were spent in light-intensity activities, and a little over one hour was spent in moderate-intensity lifestyle activities. On average, only 16 minutes were recorded in moderate-intensity PA’s equivalent to a brisk walk. This level of inactivity is consistent with the eligibility criteria for the Madres study requiring women to engage in less than 150 min.wk−1 of moderate-intensity PA. We used the ActiGraph cut-points created by Matthews et al. [29, 31] to differentiate between time spent in sedentary behaviors, light-intensity, and moderate-lifestyle PA’s. These three intensity levels would be categorized by Freedson et al. [16] as light-intensity PA. Because our sample had such low activity levels, we felt using Freedson et al. broad light-intensity category would result in a loss of resolution about the distribution of lower-intensity PA.
Direct comparison of data from PA records and accelerometers should be interpreted with caution. Instead, they should be used to provide complimentary information about the frequency, duration, and types of PA performed by different population groups. The ActiGraph fails to detect movements that do not involve acceleration in the vertical plane (e.g., sitting quietly, cycling, and upper body activities) which can lead to an underestimation of time spent in some intensity levels. The PA records are subject to misclassification of behaviors when participants overestimate moderate-intensity activities as vigorous intensity [49], over-report the time spent in higher-intensity activities [34], and forget to report activities due to recall limitations [1]. While the PA records likely overestimate the time spent in moderate- and vigorous-intensity levels, they do characterize the types of activities performed and the relative proportion of the day spent in such activities.
Because so much of the day was spent in sedentary and low-intensity PA’s one could interpret these data as Latina women having undesirable PA habits. However this may not be the most important interpretation of the data. Nor are the absolute differences between the estimates of time spent in PA levels on the accelerometers and PA Records the most important interpretation of the data. What is important is the theme that intentional PA is not characteristic of women who have cultural values that emphasize needs of others, including families [23]. Intentional leisure time PA and exercise is simply not part of their hierarchy of values of the Latinas enrolled in this study. The PA records showed that the primary activities were household chores, caring for the family, and much of their discretionary time was spent sitting and reclining while watching TV or doing nothing. These data present an opportunity to understand and target lifestyle behaviors to potentially increase PA. This could be done through identifying approaches to household chores, family obligations and family recreation activities to incorporate short durations of intentional activities, such as10-minute bouts of physical movement, or to find ways to increase the intensity, frequency, and duration of what activities do occur.
Last, it is important to consider the demographic profile of the women enrolled in Madres para la Salud. The average BMI was 29.7 ± 5.6 (range 23.4 to 41.5) suggesting caution should be used when generalizing these results to women outside this range of BMI values. As well, about 75% (n=106) of the women had household incomes of <19,999/year. Many were low income and likely have priorities centering on survival strategies to feed and house their children, rather than thinking about leisure time PA. Additionally, not all of the participants resided in neighborhoods that they evaluated as safe or accessible for PA. Engaging in intentional PA in neighborhoods that lack safety and access for free or low-cost PA opportunities may be unrealistic unless such issues are addressed through community policy and environmental means [5].
There are strengths and limitations to this study. The primary strength is the use of multiple objective and subjective instruments to assess PA. Each instrument has its unique contributions to understanding the frequency, duration, and intensity, and types of activities performed to assess PA behavior in this Latina population. Combined, they provide a comprehensive profile of PA behaviors and levels. Also, the methods used to administer and score the instruments are tried and true as they have been used in multiple studies to assess PA [2]. While we consider this approach one of the strengths of the study, wearing an accelerometer, pedometer, and completing PA records concurrently may have caused reactivity in the participants PA levels potentially biasing the results. We also acknowledge the limitation of losing ActiGraph data for 19 participants due to low compliance of the days and/or hours the monitor were worn and the need to modify the 7-day PAR with a shorter, 3-day PAR version. While 15 women in our study were categorized in the somewhat active-to-highly active categories on the pedometer and some reported engaging in moderate-to-vigorous intensity PA’s by the ActiGraph accelerometer, it likely is due to some women being active in their occupational activities (e.g., employed as waitresses and caterers). This also points to limitations of how participants are screened for sedentary behaviors and has implications for studies that use screening methods similar to those used in this study.
Summary
These data show that this sample of post-partum Latina women demonstrate levels of PA far below what is recommended by virtually all public health organizations for health enhancing behavior. Many of the women had low household income levels and likely have priorities centering on survival strategies to feed and house their children, rather than thinking about PA. An intervention to increase walking for 150 min.wk−1 and/or 30 min.d−1 or more is warranted. The issues of Latinas to keeping or relinquishing values and behavior patterns from their own culture, such as prioritizing family matters and household maintenance, and how this impacts the ability to negotiate or value intentional activity or planning PA time within the context of their lives is worth considering [51].
ACKNOWLEDGEMENTS
We are grateful to our staff and participants for their contributions to the study. This project was supported by NIH R010356-01A2 (Dr. Colleen Keller, PI). The authors have no professional relationships to disclose. The results of the present study do not constitute endorsement by ACSM. This material is the result, in part, of work supported with resources and the use of facilities at the Phoenix VA Health Care System. The contents do not represent the views of the Department of Veterans Affairs or the United States Government.
Funding Source: NHI R01 0356-01A2
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest: The authors have no conflict of interest to report.
REFERENCES
- 1.Ainsworth B, Caspersen C, Matthews C, Mâsse L, Baranowski T, Zhu W. Recommendations to improve the accuracy of estimates of physical activity derived from self report. J Phys Act Health. 2012;9(Suppl 1):S76–S84. doi: 10.1123/jpah.9.s1.s76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ainsworth B, Coleman K. Physical Activity Measurement. In: McTiernan A, editor. Cancer Prevention and Management through Exercise and Weight Control. Boca Raton: CRC Press Inc; 2006. pp. 13–24. [Google Scholar]
- 3.Ainsworth B, Haskell W, Herrmann S, Meckes N, Bassett DJ, Tudor-Locke C, Greer J, Vezina J, Whitt-Glover M, Leon A. 2011 Compendium of Physical Activities: a second update of codes and MET values. Med Sci Sports Exerc. 2011;43(8):1575–1581. doi: 10.1249/MSS.0b013e31821ece12. [DOI] [PubMed] [Google Scholar]
- 4.Ainsworth B, Irwin M, Addy C, Whitt M, Stolarczyk L. Moderate physical activity patterns of minority women: the Cross-Cultural Activity Participation Study. J Womens Health Gend Based Med. 1999;8(6):805–813. doi: 10.1089/152460999319129. [DOI] [PubMed] [Google Scholar]
- 5.Ainsworth B, Wilcox S, Thompson W, Richter D, Henderson K. Personal, social, and physical environmental correlates of physical activity in African American women in South Carolina. Am J Prev Med. 2003;25(3Si):23–29. doi: 10.1016/s0749-3797(03)00161-2. [DOI] [PubMed] [Google Scholar]
- 6.Althuizen E, van Poppel M, de Vries J, Seidell J, van Mechelen W. Postpartum behavior as predictor of weight change from before pregnancy to one year postpartum. BMC Public Health. 2011;11:1–7. doi: 10.1186/1471-2458-11-165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bauer P, Pivarnik J, Feltz D, Paneth N, Womack C. Validation of an historical physical activity recall tool in postpartum women. J Phys Act Health. 2010;7(5):658–661. doi: 10.1123/jpah.7.5.658. [DOI] [PubMed] [Google Scholar]
- 8.Blair S, Haskell W, Ho P, Paffenbarger RJ, Vranizan K, Farquhar J, Wood P. Assessment of habitual physical activity by a seven-day recall in a community survey and controlled experiments. Am J Epidemiol. 1985;122(5):794–804. doi: 10.1093/oxfordjournals.aje.a114163. [DOI] [PubMed] [Google Scholar]
- 9.Callister L, Beckstrand R, Corbett C. Postpartum depression and help-seeking behaviors in immigrant Hispanic women. J Obstet Gynecol Neonatal Nurs. 2011;40(4):440–449. doi: 10.1111/j.1552-6909.2011.01254.x. [DOI] [PubMed] [Google Scholar]
- 10.Capewell S, Ford E, Croft J, Critchley J, Greenlund K, Labarthe D. Cardiovascular risk factor trends and potential for reducing coronary heart disease mortality in the United States of America. Bull World Health Organ. 2010;88:120–130. doi: 10.2471/BLT.08.057885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chavez A, Ainsworth B, Farr K, Vega-Lopez S. Reliability and validity of two physical activity surveys in Spanish-speaking Mexican Americans. Med Sci Sport Exerc. 2012;44(suppl):S461. [Google Scholar]
- 12.Durham H, Morey M, Lovelady C, Brouwer N, Karause K, Østbye T. Postpartum physical activity in overweight obese women. J Phys Act Health. 2011;8(7):988–993. doi: 10.1123/jpah.8.7.988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ertel K, Rich-Edwards J, Koenen K. Maternal depression in the United States: Nationally representative rates and risks. J Women's Health. 2011;20(11):1609–1617. doi: 10.1089/jwh.2010.2657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Flegal KM, Carrol MD, Ogden CL, Curtin LR. Prevalence and trends in obesity among US adults, 1999–2008. JAMA. 2010;303(3):235–241. doi: 10.1001/jama.2009.2014. [DOI] [PubMed] [Google Scholar]
- 15.Ford E, Bergmann M, Kröger J, Schienkiewitz A, Weikert C, Boeing H. Healthy living is the best revenge: findings from the European Prospective Investigation Into Cancer and Nutrition-Potsdam study. Arch Intern Med. 2009;169(15):1355–1362. doi: 10.1001/archinternmed.2009.237. [DOI] [PubMed] [Google Scholar]
- 16.Freedson P, Melanson E, Sirard J. Calibration of the Computer Science and Application, Inc. accelerometer. Med Sci Sports Exerc. 1998;30(5):777–781. doi: 10.1097/00005768-199805000-00021. [DOI] [PubMed] [Google Scholar]
- 17.Gould Rothberg B, Magriples U, Kershaw T, Rising S, Ickovics J. Gestational weight gain and subsequent postpartum weight loss among young, low-income, ethnic minority women. Am J Obst Gynecol. 2011;204(1):52, e1–e11. doi: 10.1016/j.ajog.2010.08.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Haskell W, Lee I, Pate R, Powell K, Blair S, Franklin B, Macera C, Heath G, Thompson P, Bauman A. Physical activity and public health: updated recommendation for adults from the American College of Sports Medicine and the American Heart Association. Circulation. 2007;28(9):1081–1093. doi: 10.1161/CIRCULATIONAHA.107.185649. [DOI] [PubMed] [Google Scholar]
- 19.Hasson R, Haller J, Pober D, Staudenmayer J, Freedson P. Validity of the Omron HJ-112 pedometer during treadmill walking. Med Sci Sports Exerc. 2009;41(4):805–809. doi: 10.1249/MSS.0b013e31818d9fc2. [DOI] [PubMed] [Google Scholar]
- 20.Heidemann C, Hoffmann K, Klipstein-Grobusch K, Weikert C, Pischon T, Hense H, Boeing H. Potentially modifiable classic risk factors and their impact on incident myocardial infarction: results from the EPIC-Potsdam study. Eur J Cardiovasc Prev Rehabil. 2007;14(1):65–71. doi: 10.1097/01.hjr.0000238392.19847.4c. [DOI] [PubMed] [Google Scholar]
- 21.Holbrook E, Barreira T, Kang M. Validity and reliability of Omron pedometers for prescribed and self-paced walking. Med Sci Sports Exerc. 2009;669–673(3):669–673. doi: 10.1249/MSS.0b013e3181886095. [DOI] [PubMed] [Google Scholar]
- 22.Howley E. You Asked For It: Question Authority. ACSM's Health Fit J. 2000;46(1):40. [Google Scholar]
- 23.Juarbe T, Lipson J, Turok X. Physical activity beliefs, behaviors, and cardiovascular fitness of Mexican immigrant women. J Transcult Nurs. 2003;14:108–118. doi: 10.1177/1043659602250623. [DOI] [PubMed] [Google Scholar]
- 24.Keller C, Ainsworth B, Records K, Belyea M. Madres para la Salud” [Mothers for Health]: Theoretical Rationale. Contemp Clin Trials. 2011;32:418–427. doi: 10.1016/j.cct.2011.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kruger J, Kohl H., III Prevalence of Regular Physical Activity Among Adults --- United States, 2001 and 2005. Morb Mortal Wkly Rep. 2007;56(46):1209–1212. [PubMed] [Google Scholar]
- 26.Lewis B, Martinson B, Sherwood N, Avery M. A pilot study evaluating a telephone-based exercise intervention for pregnant and postpartum women. J Midwifery Womens Health. 2011;56(2):127–131. doi: 10.1111/j.1542-2011.2010.00016.x. [DOI] [PubMed] [Google Scholar]
- 27.Marquez DX, Neighbors CJ, Bustamante EE. Leisure time and occupational physical activity among racial or ethnic minorities. Med Sci Sport Exerc. 2010;42(6):1086–1093. doi: 10.1249/MSS.0b013e3181c5ec05. [DOI] [PubMed] [Google Scholar]
- 28.Martinez S, Ainsworth B, Elder J. Culturally appropriate measures for promoting physical activity in the American Latino population. Ann Behav Med. 2008;36(2):195–207. doi: 10.1007/s12160-008-9063-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Matthews C, Ainsworth B, Hanby C, Pate R, Addy C, Freedson P, Jones D, Macera C. Development and testing of a short physical activity recall questionnaire. Med Sci Sports Exerc. 2005;37(6):986–994. [PubMed] [Google Scholar]
- 30.Matthews C, Ainsworth B, Thompson R, Bassett DJ. Sources of variance in daily physical activity levels as measured by an accelerometer. Med Sci Sports Exerc. 2002;34(8):1376–1381. doi: 10.1097/00005768-200208000-00021. [DOI] [PubMed] [Google Scholar]
- 31.Matthews C, Chen K, Freedson P, Buchowski M, Beech B, Pate R, Troiano R. Amount of time spent in sedentary behaviors in the United States, 2003–2004. Am J Epidemiol. 2008;167(7):875–881. doi: 10.1093/aje/kwm390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Maturi M, Afshary P, Abedi P. Effect of physical activity intervention based on a pedometer on physical activity level and anthropometric measures after childbirth: a randomized controlled trial. BMC Preg Childbirth. 2011;16(1):1–8. doi: 10.1186/1471-2393-11-103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Montpetit A, Plourde H, Cohen T, Koski K. Modeling the impact of pre-pregnancy BMI, physical activity and energy intake on gestional weight gain, infant birth weight, and post partum weight retention. J Phys Act Health. 2011;5 doi: 10.1123/jpah.9.7.1020. E-pub ahead of print. [DOI] [PubMed] [Google Scholar]
- 34.Nicaise V, Marshall S, Ainsworth B. Domain-specific physical activity and self-report bias among low-income Latinas living in San Diego County. J Phys Act Health. 2011;8(7):881–890. doi: 10.1123/jpah.8.7.881. [DOI] [PubMed] [Google Scholar]
- 35.Ostbye T, Peterson B, Krause K, Swarmy G, Lovelady C. Predictors of postpartum weight change among overweight and obese women: results from the Active Mothers Postpartum Study. J Womens Health Gend Based Med. 2012;21(2):215–222. doi: 10.1089/jwh.2011.2947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Pate R, Ross R, Dowda M, Trost S, Sirard J. Validation of a 3-day physical activity recall instrument in female youth. Ped Exerc Sci. 2003;13(3):257–265. [Google Scholar]
- 37.Physical Activity Guidelines Advisory Committee. Physical Activity Guidelines Advisory Committee Report. Washington, DC: US Department of Health and Human Services; 2008. p. E-45. [Google Scholar]
- 38.Rasmussen K, Yaktine A. Weight gain during pregnancy: re-examining the guidelines. Washington, DC: National Academies Press; 2009. [PubMed] [Google Scholar]
- 39.Records K, Keller C, Ainsworth B, Permana P. Instrument selecton for randomized controlled trials: Why this and not that? Contemp Clin Trials. 2012;33(1):143–150. doi: 10.1016/j.cct.2011.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Skouteris H, Hartley-Clark L, McCabe M, Milgrom J, Kent B, Herring S, Gale J. Preventing excessive gestational weight gain: a systematic review of interventions. Obes Rev. 2010;11:757–768. doi: 10.1111/j.1467-789X.2010.00806.x. [DOI] [PubMed] [Google Scholar]
- 41.Taylor-Piliae R, Fair J, Haskell W, Varady A, Iribarren C, Hlatky M, Go A, Fortmann S. Validation of the Stanford Brief Activity Survey: examining psychological factors and physical activity levels in older adults. J Phys Act Health. 2010;7(1):87–94. doi: 10.1123/jpah.7.1.87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Taylor-Piliae R, Norton L, Haskell W, Mahbouda M, Fair J, Iribarren C, Hlatky M, Go A, Fortmann S. Validation of a new brief physical activity survey among men and women aged 60–69 years. Am J Epidemiol. 2006;164(6):598–606. doi: 10.1093/aje/kwj248. [DOI] [PubMed] [Google Scholar]
- 43.Treuth M, Butte N, Puyau M. Pregnancy-related changes in physical activity, fitness, and strength. Med Sci Sports Exerc. 2005;37(5):832–837. doi: 10.1249/01.mss.0000161749.38453.02. [DOI] [PubMed] [Google Scholar]
- 44.Tudor-Locke C, Burkett L, Reis J, Ainsworth B, Macera C. How many days of pedometer monitoring predict weekly physical activity in adults? Prev Med. 2005;40(3):293–298. doi: 10.1016/j.ypmed.2004.06.003. [DOI] [PubMed] [Google Scholar]
- 45.PA Division of Nutrition, and Obesity, editor. U.S. Centers for Disease Control and Prevention. All States: Recommended Physical Activity: Gender by Race. Atlanta: Behavioral Risk Factors Surveillance System; 2009. [Google Scholar]
- 46.U.S. Department of Health and Human Services. 2008 Physical Activity Guidelines for Americans. Washington, DC: USDHHS; 2008. [Google Scholar]
- 47.Walker L, Freeland-Graves J, Milani T, George G, Hanss-Nuss H, Kim M, Sterling B, Timmerman G, Wilkinson S, Arheart K, Stuifbergen A. Weight and behavioral and psychosocial factors among ethnically diverse, low-income women after childbirth: II. Trends and correlates. Women Health. 2004;40(2):19–34. doi: 10.1300/J013v40n02_02. [DOI] [PubMed] [Google Scholar]
- 48.Welk G. Use of Accelerometry-Based Activity Monitors to Assess Physical Activity. In: Welk G, editor. Physical Activity Assessments for Health-Related Research. Champaign: Human Kinetics; 2002. p. 280. [Google Scholar]
- 49.Wilcox S, Irwin M, Addy C, Stolarczyk L, Ainsworth B, Whitt M, Tudor-Locke C. Agreement between participant-rated and compendium-coded intensity of daily activities in a triethnic sample of women ages 40 years and older. Ann Behav Med. 2001;23(4):253–262. doi: 10.1207/S15324796ABM2304_4. [DOI] [PubMed] [Google Scholar]
- 50.Wilkinson S, Huang C, Walker L, Sterline B, Kim M. Physical activity in low-income postpartum women. J Nurs Scholarsh. 2004;36(2):109–114. doi: 10.1111/j.1547-5069.2004.04022.x. [DOI] [PubMed] [Google Scholar]
- 51.Wolin K, Colangelo L, Chiu B, Gapstur S. Obesity and immigration among Latina women. J Immigr Minor Health. 2009;11:428–431. doi: 10.1007/s10903-007-9115-1. [DOI] [PMC free article] [PubMed] [Google Scholar]