Abstract
Study Design
Case-control.
Objective
To precisely quantify and compare intervertebral segmental contributions to cervical spine flexion-extension during continuous, functional flexion-extension in asymptomatic subjects to single-level anterior arthrodesis patients.
Summary of Background Data
Segmental contributions to cervical flexion-extension have traditionally been determined using single images collected at full flexion and full extension. These calculations neglect mid-range motion, and assume percentage contributions to motion remain constant throughout the entire flexion-extension range of motion (ROM).
Methods
6 single-level (C5/C6) anterior arthrodesis patients and 18 asymptomatic control subjects performed flexion-extension while biplane radiographs were collected at 30 images per second. A previously validated tracking process determined three-dimensional vertebral position with sub-millimeter accuracy during continuous flexion-extension. Mixed-effects models of segmental percentage contribution to C2/C7 flexion-extension were developed to identify differences in percentage contribution within each motion segment, among motion segments, and between control and arthrodesis patients over the full ROM.
Results
The C2/C3, C3/C4 and C4/C5 motion segments made their maximum contributions during the mid-range of motion. The C5/C6 and C6/C7 motion segments, in contrast, made their maximum contributions near the start and end of the ROM. Arthrodesis patients’ contribution from the C4/C5 motion segment increased significantly over the range of motion from 30% to 95% of the total flexion-extension ROM (average increased contribution of 5.1%) and arthrodesis patients’ contribution from the C6/C7 motion segment increased significantly over the entire flexion-extension ROM (average increased percentage contribution of 8.9%) in comparison to controls.
Conclusion
Cervical motion segment contributions to flexion-extension change significantly during the flexion-extension motion. The largest change in percentage contribution to motion, relative to controls, occurs at the C6/C7 motion segment, over the entire range of motion, suggesting a potential mechanical mechanism for the clinical observation of increased incidence of adjacent segment degeneration at C6/C7 rather than at C4/C5 following C5/C6 arthrodesis.
Keywords: spine, kinematics, anterior cervical fusion, intervertebral, disc
Introduction
Degenerative changes adjacent to cervical arthrodesis have been widely reported1–7. These degenerative changes occur in 16%6 to 25%4 of the patients within 10 years of the operation, and require adjacent level surgery in 6% to 10% of the patients5,8–11. The etiology of adjacent segment disease following cervical arthrodesis remains controversial. The disease may progress due to the underlying spondylosis4,12,13, the arthrodesis may lead to increased motion in adjacent vertebrae, resulting in overload and instability2,14–17, or adjacent segment degeneration may result from a combination of these two factors1,5. In an attempt to eliminate the potential overload of adjacent segments following arthrodesis, several motion-preserving disc replacement devices have been recently developed18–21.
The effects of anterior arthrodesis or disc arthroplasty on adjacent segment kinematics are often evaluated clinically using full flexion and full extension radiographs. These end-range images are not necessarily representative of mid-range cervical kinematics and are characterized by substantial inter-subject variability in range of motion22–26, potentially due to variable patient effort during imaging. These limitations associated with static end-range imaging make it impossible to determine if cervical motion segment contributions to flexion-extension are constant or if they fluctuate throughout the range of motion. Furthermore, while arthrodesis may not affect overall range of motion in adjacent segments27, it is not clear if it affects the normal patterns of contributions to motion, which may reflect altered disc loading following arthrodesis. Collecting continuous cervical kinematics over the entire flexion-extension motion and performing a within-subject analysis of the segmental contributions to overall spine motion may overcome the limitations associated with static, end-range imaging.
The first objective of this study was to characterize segmental percentage contributions to cervical flexion-extension in an asymptomatic control group. The hypothesis tested was that segmental contributions to spine motion would be level dependent and uniform over the entire range of motion. Specifically, contributions from the C4/C5 and C5/C6 motion segments were expected to be the largest and contributions from C2/C3 and C6/C7 were expected to be the smallest throughout the entire range of motion. The second objective of this study was to assess the effect of single-level anterior arthrodesis on adjacent segment contributions to cervical flexion-extension. It was hypothesized that motion segments adjacent to the arthrodesis would disproportionally increase their contribution to cervical flexion-extension over the entire range of motion.
Materials and Methods
Subjects
Following Institutional Review Board (IRB) approval, data was collected from 6 single-level (C56) anterior arthrodesis patients (average age: 48.8 ± 6.9 yrs.; 1 M, 5 F; 7.6±1.2 mo. post-surgery) and 18 asymptomatic control subjects of similar age (average age: 45.6 ± 5.8 yrs.; 5 M, 13 F) who provided informed consent to participate in this research study. Pregnant women, patients diagnosed with osteoporosis, and patients with any other injury or disease that interferes with spine function were excluded. Patients were identified during clinic visits. Control subjects were recruited through an advertisement in an employee newsletter and word of mouth.
Data Collection
High-resolution CT scans (0.29×0.29×1.25 mm voxels) of the cervical spine (C2–C7) were acquired on each participant (GE Lightspeed 16). Bone tissue was segmented from the CT volume using a combination of commercial software (Mimics software, Materialise, Leuven, Belgium) and manual segmentation28. A three-dimensional (3D) model of each vertebra was generated from the segmented bone tissue. Markers were interactively placed on the 3D bone models to define bone-specific anatomic coordinate systems. The effective dose of a cervical spine CT scan has been reported to be between 3.0 mSv and 4.36 mSv29,30.
Subjects were seated within a biplane X-ray system and directed to continuously move their head and neck through their entire range of flexion-extension. A metronome set at 40 to 44 beats per minute was used to ensure the participants moved at a continuous, steady pace to complete each full movement cycle in 3 seconds or less. Biplane radiographs were collected at 30 images per second for 3 seconds for each trial of continuous flexion-extension (X-ray parameters: 70 KV, 160 mA, 2.5 ms X-ray pulses, source-to-subject distance 140 cm). Radiographs were recorded for 2 or 3 trials for each subject, resulting in a total of 63 movement trials analyzed for this study. Multiple trials from the same subject were averaged to yield a single average dataset for each subject used for statistical analysis. A static trial with the subject looking forward with the head in the neutral position was also collected for each participant. The effective radiation dose for each 3-second dynamic flexion-extension motion trial was estimated to be 0.16 mSv (determined using PCXMC simulation software, STUK, Helsinki, Finland).
Data Processing
A previously validated tracking process determined three-dimensional vertebral position in each pair of radiographs with sub-millimeter accuracy31 for all static and dynamic trials. Details describing the volumetric model-based tracking process, including hardware and software specifications, calibration and distortion correction procedures, and computational algorithms have been described previously31–34. Tracked bone movement data was filtered at 1.0 Hz using a fourth-order, low-pass Butterworth filter with the filter frequency determined using residual analysis35. Six degree-of-freedom (DOF) kinematics between adjacent vertebrae (3 translations, 3 rotations) were calculated following established standards for reporting spine kinematics36,37. Intervertebral position and orientation in each frame of the continuous dynamic trial were normalized to the static neutral trial for each subject. Only the flexion-extension component of vertebral rotation is presented in the current analysis.
C2 flexion-extension motion relative to C7 (C2/C7) was interpolated to obtain C2/C7 motion at 1% increments of the total cervical ROM for each participant. In this way, the total cervical spine flexion-extension ROM (from C2 to C7) of each participant was standardized to 100%, allowing for comparisons among subjects. Segmental flexion-extension rotation was then interpolated to obtain relative flexion-extension at each intervertebral motion segment for every 1% increment of C2/C7 spine motion. Initial analysis was performed separately for the flexion and extension motions.
Statistical Design and Analysis
Statistical analysis was performed by fitting separate mixed-effects models for control and arthrodesis groups, with the random intercept for individual subjects and the cluster variation among motion segments (C2/C3, C3/C4, C4/C5, C5/C6 and C6/C7) to account for the dependency in the data. Each fitted model included motion segment, percent contribution, squared percent contribution, and their interaction terms with the motion segment to capture the curvature in the percentage contribution curves over the ROM. Differences in percent contributions between groups and between motion segments were assessed at given movement percentages by comparing point-wise 95% confidence intervals (CI) from the fitted models.
Results
Percentage contributions to C2/C7 flexion-extension were not significantly different at any motion segment between the flexion and extension movement (all p ≥ .190 for direction of movement; all p ≥ .571 for direction by group interaction). Thus, segmental flexion contributions and segmental extension contributions to overall C2/C7 motion were combined at corresponding percentages of ROM for analysis purposes.
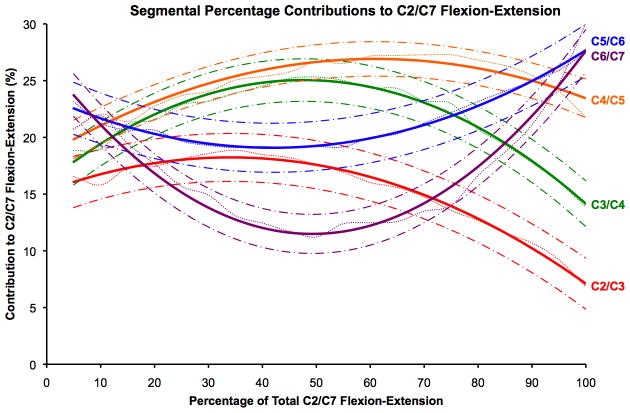
Segmental percentage contributions varied substantially within each motion segment over the full range of flexion-extension in control subjects (Figure 1). Two general patterns of contributions to flexion-extension were apparent. The C2/C3, C3/C4 and C4/C5 motion segments, in general, made their maximum contributions during the midrange of motion, and decreased their percentage contributions near the start and end of the ROM (Figure 1). The C5/C6 and C6/C7 motion segments, on the other hand, made their maximum contributions near the start and end of the ROM, and generally made their smallest contributions over the mid-range of motion (Figure 1). The lack of overlap between 95% confidence interval boundaries from different motion segments (e.g. C3/C4 and C4/C5 from 70% to 100% of total C2/C7 ROM), indicate the contributions being compared are statistically different at all of the non-overlapping movement percentage points at a significance level of .05. Similarly, within a single motion segment, the 95% confidence intervals may be used to identify portions of the flexion-extension movement cycle where the contributions due to a specific motion segment are statistically different at a significance level of .05 (e.g. the C6/C7 contribution from 40% to 60% of total ROM is less than the C6/C7 contribution from 0%-25% and 75%–100% of total C2/C7 ROM).
Figure 1.
Control group average segmental percentage contributions to C2/C7 flexion-extension. Data for each motion segment is represented by observed data (dots), predicted contributions from the mixed-model analysis (solid lines), and 95% confidence interval (dash-dot).
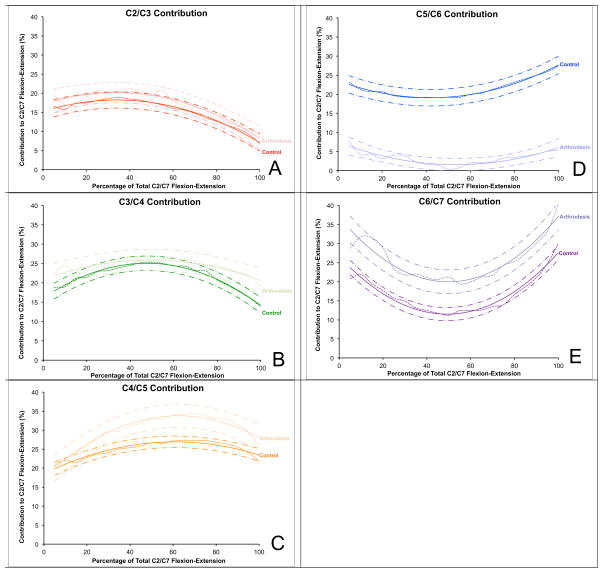
Segmental percentage contributions to C2/C7 flexion-extension in arthrodesis patients followed patterns similar to those in control subjects, with the obvious exception of very little motion attributed to the operated (C5/C6) motion segment (Figure 2). The reduced contribution from the C5/C6 motion segment in arthrodesis patients was compensated by an increased contribution from the C4/C5 and C6/C7 motion segments. The contribution from the C4/C5 motion segment in arthrodesis patients was significantly increased over the range of motion from 30% to 95% of the total C2/C7 ROM relative to controls (Figure 2C). The contribution from the C6/C7 motion segment in arthrodesis patients was significantly increased over the entire flexion-extension range of motion relative to controls (Figure 2E). The C2/C3 and C3/C4 motion segment contributions were not significantly different between control and arthrodesis groups at any percentage of the C2/C7 flexion-extension movement. The average differences between arthrodesis and control groups in percentage contribution from the C2/C3, C3/C4, C4/C5, C5/C6 and C6/C7 motion segments were 1.7%, 2.5%, 5.1%, −18.2% and 8.9%, respectively, where positive (or negative) values indicate increased (or decreased) percentage contributions in arthrodesis patients relative to controls.
Figure 2.
Control and arthrodesis group average segmental percentage contributions to C2/C7 flexion-extension. Data for each motion segment is represented in an identical fashion to Figure 1. The control group data is designated by darker symbols and arthrodesis group is designated by lighter symbols. Differences between groups are statistically significant at all ROM percentages when the 95% confidence interval boundaries do not overlap.
C2/C7 flexion-extension ROM in the control group (67°±10°) was significantly greater than in the arthrodesis group (57°±7°) (p = .037). This difference between groups was primarily due to the reduced ROM at C5/C6 in the arthrodesis group (p < .001). No significant differences in total range of motion were observed at any other motion segment (Figure 3).
Figure 3.
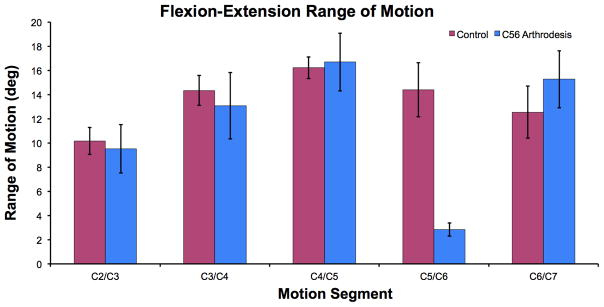
Average range of motion at each motion segment for the control and arthrodesis groups. Only the C5/C6 motion segment was significantly different between groups (p < .001; all other p ≥ 0.197; unpaired t-tests). Error bars represent 95% confidence intervals.
Discussion
Segmental percentage contributions to cervical spine flexion-extension have been reported previously using end ROM data (a single full extension and a single full flexion radiograph)38–40 and images collected from selected midrange positions41. These studies found that, in control subjects, segmental contributions were greatest at the C4/C5 motion segment and decreased progressively in the superior and inferior motion segments. The current study provides a more detailed and comprehensive analysis of segmental contributions to flexion-extension. The current study indicates that in asymptomatic subjects, midrange flexion-extension is dominated by C3/C4 and C4/C5 motion, while contributions from C5/C6 and C6/C7 motion segments increase near the start and end of the ROM. Although the C5/C6 and C6/C7 motion segments increase their contributions to spine flexion-extension when loads on the spine are greatest, a clear connection cannot yet be made between these kinematic results and increased disc degeneration at the C56 and C67 disc levels42,43. Further computational modeling of the in vivo cervical spine (e.g. inverse dynamics or finite element modeling) will be necessary to reveal the interaction between kinematics, loading, and disc stress that may lead to degeneration at specific motion segments.
The results indicate that cervical motion segment percentage contributions change significantly through the flexion-extension motion. These fluctuations in segmental contributions suggest that the distribution of compressive and shear loads also fluctuates among the motion segments over the full range of motion. These results make it clear that cervical spine mechanics cannot be fully characterized by static measurements. It is evident that the motion of the vertebrae, and accompanying deformation of the discs, are dependent on the orientation of the head and the muscular loading that occurs with functional motion. This information cannot be obtained from single full-flexion and full-extension radiographs.
As hypothesized, the motion segments adjacent to the arthrodesis significantly increased their contributions to C2/C7 flexion-extension. Care should be taken to avoid misinterpretation of this result. The increased percentage contributions from motion segments adjacent to the arthrodesis do not necessarily indicate an increased total ROM at these motion segments. This is because overall C2/C7 motion was decreased in the arthrodesis groups. As Figure 3 demonstrates, and as we have previously reported for this cohort, there were no significant differences in the total flexion-extension ROM at each non-operated motion segment in arthrodesis and control subjects27. A previous clinical study that included 374 cervical arthrodesis patients identified a significantly higher risk of new adjacent segment disease at the C6/C7 motion segment in comparison to the C4/C5 motion segment4. The results of the current study suggest a potential mechanical mechanism for this clinical finding. The C6/C7 motion segment percentage contribution is, on average, 8.9 percentage points higher in arthrodesis patients than in controls, while the C4/C5 motion segment contribution is only 5.1 percentage points higher in arthrodesis patients than controls, on average. Additionally, the increase in percentage contribution from the C6/C7 motion segment is continually greater than the increase from the C4/C5 motion segment over the entire ROM. This implies that even if the arthrodesis patients are advised to limit their ROM following surgery (i.e. avoid full extension and full flexion), the largest change in percentage contribution to motion, relative to controls, will still occur at the C6/C7 motion segment, even over the mid-range of motion.
The results indicate C5/C6 arthrodesis does not drastically alter the pattern of cervical motion segment contributions to flexion-extension. Following arthrodesis, C2/C3, C3/C4 and C4/C5 continue to make their largest contributions to motion through the mid-range, while the C6/C7 motion segment still contributes more near the ends of the range of motion. Although these results suggest the pattern of motion experienced by the discs is not affected by single-level arthrodesis, further research will be required to determine if arthrodesis affects the shear and compressive forces applied to cervical discs following arthrodesis.
One limitation of the current study is that the surgical patients were not tested prior to surgery. Therefore, it is not certain that the observed differences between groups were entirely due to the surgery, as some differences may have existed due to underlying spondylosis. However, pre-surgical testing of surgical patients has indicated substantial variability in range of motion related to pain44, and therefore pre-surgical data was unlikely to be informative. Second, surgical patient testing occurred relatively soon after surgery. Follow-up testing will be necessary to evaluate the longer-term effects of arthrodesis on segmental contributions to flexion-extension. An additional limitation of the current study is the relatively narrow age range for the asymptomatic control subjects. Although the control subjects in this study were within a clinically relevant age range, continuous kinematics from younger and older asymptomatic cohorts may differ from the current results given the well-known changes that occur in the spine with age45–48.
Key Points.
Cervical segmental percentage contributions to flexion-extension varied substantially within each motion segment over the full range motion.
The C2/C3, C3/C4 and C4/C5 motion segments, in general, made their maximum contributions during the mid-range of motion, and decreased their percentage contributions near the start and end of the ROM. The C5/C6 and C6/C7 motion segments, on the other hand, made their maximum contributions near the start and end of the ROM, and made their smallest contributions during the mid-range of motion.
The reduced contribution from the C5/C6 motion segment in arthrodesis patients was compensated by an increased contribution from the C4/C5 motion segment from 30% to 95% of the total C2/C7 ROM and by an increased contribution from the C6/C7 motion segment over the entire ROM. The C2/C3 and C3/C4 motion segment contributions were not significantly different between control and arthrodesis groups.
The motion of the vertebrae, and accompanying deformation of the discs, are dependent on the orientation of the head and the muscular loading that occurs with functional motion. Therefore cervical spine mechanics cannot be fully characterized by static or end-position measurements.
Acknowledgments
The Manuscript submitted does not contain information about medical device(s)/drug(s). NIH/NIAMS and Spine Research Society 21st Century Developmental Grant funds were received to support this work. Relevant financial activities outside the submitted work: grants pending.
Contributor Information
William J Anderst, University of Pittsburgh, Department of Orthopaedic Surgery.
William F Donaldson, III, University of Pittsburgh, Department of Orthopaedic Surgery.
Joon Y Lee, University of Pittsburgh, Department of Orthopaedic Surgery.
James D Kang, University of Pittsburgh, Department of Orthopaedic Surgery.
References
- 1.Hunter LY, Braunstein EM, Bailey RW. Radiographic changes following anterior cervical fusion. Spine (Phila Pa 1976) 1980;5(5):399–401. doi: 10.1097/00007632-198009000-00002. [DOI] [PubMed] [Google Scholar]
- 2.Baba H, Furusawa N, Imura S, et al. Late radiographic findings after anterior cervical fusion for spondylotic myeloradiculopathy. Spine. 1993;18(15):2167–73. doi: 10.1097/00007632-199311000-00004. [DOI] [PubMed] [Google Scholar]
- 3.Gore DR, Sepic SB. Anterior discectomy and fusion for painful cervical disc disease. A report of 50 patients with an average follow-up of 21 years. Spine (Phila Pa 1976) 1998;23(19):2047–51. doi: 10.1097/00007632-199810010-00002. [DOI] [PubMed] [Google Scholar]
- 4.Hilibrand AS, Carlson GD, Palumbo MA, et al. Radiculopathy and myelopathy at segments adjacent to the site of a previous anterior cervical arthrodesis. J Bone Joint Surg Am. 1999;81(4):519–28. doi: 10.2106/00004623-199904000-00009. [DOI] [PubMed] [Google Scholar]
- 5.Goffin J, Geusens E, Vantomme N, et al. Long-term follow-up after interbody fusion of the cervical spine. J Spinal Disord Tech. 2004;17(2):79–85. doi: 10.1097/00024720-200404000-00001. [DOI] [PubMed] [Google Scholar]
- 6.Ishihara H, Kanamori M, Kawaguchi Y, et al. Adjacent segment disease after anterior cervical interbody fusion. Spine J. 2004;4(6):624–8. doi: 10.1016/j.spinee.2004.04.011. [DOI] [PubMed] [Google Scholar]
- 7.Kulkarni V, Rajshekhar V, Raghuram L. Accelerated spondylotic changes adjacent to the fused segment following central cervical corpectomy: magnetic resonance imaging study evidence. J Neurosurg. 2004;100(1 Suppl Spine):2–6. doi: 10.3171/spi.2004.100.1.0002. [DOI] [PubMed] [Google Scholar]
- 8.Bohlman HH, Emery SE, Goodfellow DB, et al. Robinson anterior cervical discectomy and arthrodesis for cervical radiculopathy. Long-term follow-up of one hundred and twenty-two patients. J Bone Joint Surg Am. 1993;75(9):1298–307. doi: 10.2106/00004623-199309000-00005. [DOI] [PubMed] [Google Scholar]
- 9.Gore DR, Sepic SB. Anterior cervical fusion for degenerated or protruded discs. A review of one hundred forty-six patients. Spine (Phila Pa 1976) 1984;9(7):667–71. doi: 10.1097/00007632-198410000-00002. [DOI] [PubMed] [Google Scholar]
- 10.Watters WC, 3rd, Levinthal R. Anterior cervical discectomy with and without fusion. Results, complications, and long-term follow-up. Spine (Phila Pa 1976) 1994;19(20):2343–7. doi: 10.1097/00007632-199410150-00016. [DOI] [PubMed] [Google Scholar]
- 11.Hilibrand AS, Yoo JU, Carlson GD, et al. The success of anterior cervical arthrodesis adjacent to a previous fusion. Spine (Phila Pa 1976) 1997;22(14):1574–9. doi: 10.1097/00007632-199707150-00009. [DOI] [PubMed] [Google Scholar]
- 12.Fuller DA, Kirkpatrick JS, Emery SE, et al. A kinematic study of the cervical spine before and after segmental arthrodesis. Spine. 1998;23(15):1649–56. doi: 10.1097/00007632-199808010-00006. [DOI] [PubMed] [Google Scholar]
- 13.Song KJ, Choi BW, Jeon TS, et al. Adjacent segment degenerative disease: is it due to disease progression or a fusion-associated phenomenon? Comparison between segments adjacent to the fused and non-fused segments. Eur Spine J. 2011;20(11):1940–5. doi: 10.1007/s00586-011-1864-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Fielding JW. Normal and Selected Abnormal Motion of the Cervical Spine from the Second Cervical Vertebra to the Seventh Cervical Vertebra Based on Cineroentgenography. J Bone Joint Surg Am. 1964;46:1779–81. [PubMed] [Google Scholar]
- 15.Dunsker SB, Colley DP, Mayfield FH. Kinematics of the cervical spine. Clin Neurosurg. 1978;25:174–83. doi: 10.1093/neurosurgery/25.cn_suppl_1.174. [DOI] [PubMed] [Google Scholar]
- 16.Matsunaga S, Kabayama S, Yamamoto T, et al. Strain on intervertebral discs after anterior cervical decompression and fusion. Spine. 1999;24(7):670–5. doi: 10.1097/00007632-199904010-00011. [DOI] [PubMed] [Google Scholar]
- 17.Schwab JS, Diangelo DJ, Foley KT. Motion compensation associated with single-level cervical fusion: where does the lost motion go? Spine. 2006;31(21):2439–48. doi: 10.1097/01.brs.0000239125.54761.23. [DOI] [PubMed] [Google Scholar]
- 18.Sasso RC, Anderson PA, Riew KD, et al. Results of cervical arthroplasty compared with anterior discectomy and fusion: four-year clinical outcomes in a prospective, randomized controlled trial. J Bone Joint Surg Am. 2011;93(18):1684–92. doi: 10.2106/JBJS.J.00476. [DOI] [PubMed] [Google Scholar]
- 19.Jawahar A, Cavanaugh DA, Kerr EJ, 3rd, et al. Total disc arthroplasty does not affect the incidence of adjacent segment degeneration in cervical spine: results of 93 patients in three prospective randomized clinical trials. Spine J. 2010;10(12):1043–8. doi: 10.1016/j.spinee.2010.08.014. [DOI] [PubMed] [Google Scholar]
- 20.McAfee PC, Reah C, Gilder K, et al. A Meta-Analysis of Comparative Outcomes Following Cervical Arthroplasty or Anterior Cervical Fusion: Results from Four Prospective Multi-center Randomized Clinical Trials and up to 1226 Patients. Spine (Phila Pa 1976) 2011 doi: 10.1097/BRS.0b013e31823da169. [DOI] [PubMed] [Google Scholar]
- 21.Kelly MP, Mok JM, Frisch RF, et al. Adjacent segment motion after anterior cervical discectomy and fusion versus Prodisc-c cervical total disk arthroplasty: analysis from a randomized, controlled trial. Spine (Phila Pa 1976) 2011;36(15):1171–9. doi: 10.1097/BRS.0b013e3181ec5c7d. [DOI] [PubMed] [Google Scholar]
- 22.Lind B, Sihlbom H, Nordwall A, et al. Normal range of motion of the cervical spine. Arch Phys Med Rehabil. 1989;70(9):692–5. [PubMed] [Google Scholar]
- 23.Dvorak J, Froehlich D, Penning L, et al. Functional radiographic diagnosis of the cervical spine: flexion/extension. Spine. 1988;13(7):748–55. doi: 10.1097/00007632-198807000-00007. [DOI] [PubMed] [Google Scholar]
- 24.Frobin W, Leivseth G, Biggemann M, et al. Sagittal plane segmental motion of the cervical spine. A new precision measurement protocol and normal motion data of healthy adults. Clin Biomech. 2002;17(1):21–31. doi: 10.1016/s0268-0033(01)00105-x. [DOI] [PubMed] [Google Scholar]
- 25.Reitman CA, Mauro KM, Nguyen L, et al. Intervertebral motion between flexion and extension in asymptomatic individuals. Spine. 2004;29(24):2832–43. doi: 10.1097/01.brs.0000147740.69525.58. [DOI] [PubMed] [Google Scholar]
- 26.Wu SK, Kuo LC, Lan HC, et al. The quantitative measurements of the intervertebral angulation and translation during cervical flexion and extension. Eur Spine J. 2007;16(9):1435–44. doi: 10.1007/s00586-007-0372-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Anderst W, Donaldson W, Lee J, et al. Six Degree of Freedom Cervical Spine Range of Motion During Dynamic Flexion-Extension in Single-Level Anterior Arthrodesis Patients and Asymptomatic Controls. Journal of Bone and Joint Surgery. doi: 10.2106/JBJS.K.01733. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Thorhauer E, Miyawaki M, Illingworth K, et al. Accuracy of bone and cartilage models obtained from ct and mri. American Society of Biomechanics; Providence, RI: 2010. [Google Scholar]
- 29.Biswas D, Bible JE, Bohan M, et al. Radiation exposure from musculoskeletal computerized tomographic scans. J Bone Joint Surg Am. 2009;91(8):1882–9. doi: 10.2106/JBJS.H.01199. [DOI] [PubMed] [Google Scholar]
- 30.Fazel R, Krumholz HM, Wang Y, et al. Exposure to low-dose ionizing radiation from medical imaging procedures. N Engl J Med. 2009;361(9):849–57. doi: 10.1056/NEJMoa0901249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Anderst WJ, Baillargeon E, Donaldson WF, 3rd, et al. Validation of a noninvasive technique to precisely measure in vivo three-dimensional cervical spine movement. Spine (Phila Pa 1976) 2011;36(6):E393–400. doi: 10.1097/BRS.0b013e31820b7e2f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bey MJ, Zauel R, Brock SK, et al. Validation of a new model-based tracking technique for measuring three-dimensional, in vivo glenohumeral joint kinematics. J Biomech Eng. 2006;128(4):604–9. doi: 10.1115/1.2206199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Martin DE, Greco NJ, Klatt BA, et al. Model-based tracking of the hip: implications for novel analyses of hip pathology. J Arthroplasty. 2011;26(1):88–97. doi: 10.1016/j.arth.2009.12.004. [DOI] [PubMed] [Google Scholar]
- 34.Anderst W, Zauel R, Bishop J, et al. Validation of three-dimensional model-based tibio-femoral tracking during running. Med Eng Phys. 2009;31(1):10–16. doi: 10.1016/j.medengphy.2008.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Winter DA. Biomechanics and Motor Control of Human Movement. 4. Hoboken, New Jersey: Wiley; 2009. [Google Scholar]
- 36.Wu G, Siegler S, Allard P, et al. ISB recommendation on definitions of joint coordinate system of various joints for the reporting of human joint motion--part I: ankle, hip, and spine. International Society of Biomechanics. J Biomech. 2002;35(4):543–8. doi: 10.1016/s0021-9290(01)00222-6. [DOI] [PubMed] [Google Scholar]
- 37.Kane T, Likins P, Leivseth G. Spacecraft dynamics. New York: McGraw-Hill; 1983. [Google Scholar]
- 38.Auerbach JD, Anakwenze OA, Milby AH, et al. Segmental contribution toward total cervical range of motion: a comparison of cervical disc arthroplasty and fusion. Spine (Phila Pa 1976) 2011;36(25):E1593–9. doi: 10.1097/BRS.0b013e31821cfd47. [DOI] [PubMed] [Google Scholar]
- 39.Holmes A, Wang C, Han ZH, et al. The range and nature of flexion-extension motion in the cervical spine. Spine (Phila Pa 1976) 1994;19(22):2505–10. doi: 10.1097/00007632-199411001-00003. [DOI] [PubMed] [Google Scholar]
- 40.Miyazaki M, Hong SW, Yoon SH, et al. Kinematic analysis of the relationship between the grade of disc degeneration and motion unit of the cervical spine. Spine (Phila Pa 1976) 2008;33(2):187–93. doi: 10.1097/BRS.0b013e3181604501. [DOI] [PubMed] [Google Scholar]
- 41.Wu SK, Kuo LC, Lan HC, et al. Segmental percentage contributions of cervical spine during different motion ranges of flexion and extension. J Spinal Disord Tech. 2010;23(4):278–84. doi: 10.1097/BSD.0b013e3181a98d26. [DOI] [PubMed] [Google Scholar]
- 42.Friedenberg ZB, Miller WT. Degenerative Disc Disease of the Cervical Spine. J Bone Joint Surg Am. 1963;45:1171–8. [PubMed] [Google Scholar]
- 43.Okada E, Matsumoto M, Ichihara D, et al. Aging of the cervical spine in healthy volunteers: a 10-year longitudinal magnetic resonance imaging study. Spine (Phila Pa 1976) 2009;34(7):706–12. doi: 10.1097/BRS.0b013e31819c2003. [DOI] [PubMed] [Google Scholar]
- 44.Reitman CA, Hipp JA, Nguyen L, et al. Changes in segmental intervertebral motion adjacent to cervical arthrodesis: a prospective study. Spine. 2004;29(11):E221–6. doi: 10.1097/00007632-200406010-00022. [DOI] [PubMed] [Google Scholar]
- 45.Benoist M. Natural history of the aging spine. Eur Spine J. 2003;12 (Suppl 2):S86–9. doi: 10.1007/s00586-003-0593-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Boden SD, McCowin PR, Davis DO, et al. Abnormal magnetic-resonance scans of the cervical spine in asymptomatic subjects. A prospective investigation. J Bone Joint Surg Am. 1990;72(8):1178–84. [PubMed] [Google Scholar]
- 47.Ferguson SJ, Steffen T. Biomechanics of the aging spine. Eur Spine J. 2003;12 (Suppl 2):S97–S103. doi: 10.1007/s00586-003-0621-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Matsumoto M, Okada E, Ichihara D, et al. Age-related changes of thoracic and cervical intervertebral discs in asymptomatic subjects. Spine (Phila Pa 1976) 2010;35(14):1359–64. doi: 10.1097/BRS.0b013e3181c17067. [DOI] [PubMed] [Google Scholar]