Abstract
Background
Framingham Risk Scores (FRS) were validated in a mostly Caucasian population. Evaluation of subclinical atherosclerosis by carotid ultrasound may improve ascertainment of risk in non-White populations. This study aimed to evaluate carotid intima-media thickness (cIMT) and carotid plaquing among Mexican Americans, and to correlate these markers with coronary risk factors and the FRS.
Methods/Results
Participants (n=141) were drawn from the Cameron County Hispanic Cohort. Carotid artery ultrasound was performed and cIMT measured. Carotid plaque was defined as areas of thickening >50% of the thickness of the surrounding walls. Mean age was 53.1±11.7 years (73.8% female). Most were overweight or obese (88.7%) and more than half (53.2%) had the metabolic syndrome. One third (34.8%) had abnormal carotid ultrasound findings (either cIMT ≥75th percentile for gender and age or presence of plaque). Among those with abnormal carotid ultrasound, the majority were classified as being at low 10-year risk for cardiovascular events. Carotid ultrasound reclassified nearly a third of the cohort as being at high risk. This discordance between 10-year FRS and carotid ultrasound was noted whether risk was assessed for hard coronary events or global risk. Concordance between FRS and carotid ultrasound findings was best when long-term (30-year) risk was assessed and no subject with an abnormal carotid ultrasound was categorized as low risk by the 30-year FRS algorithm.
Conclusions
Integration of carotid ultrasound findings to coronary risk assessments and use of longer term prediction models may provide better risk assessment in this minority population, with earlier initiation of appropriate therapies.
Keywords: Carotid ultrasound, Subclinical atherosclerosis, Framingham risk score, Minority population, Risk assessment
The Framingham Risk Score (FRS) is an established coronary risk assessment tool that has been shown to be predictive of cardiovascular morbidity and mortality.1 However, this scoring method was validated in a mostly Caucasian population, and evidence suggests that absolute risk varies among different populations independently of the major risk factors.2–4 Furthermore, short-term risk assessments may not adequately define the true risk burden especially in younger individuals and among women.5 Subclinical atherosclerosis as determined by carotid intimal medial thickness (cIMT) and carotid atherosclerotic plaque presence has been shown to be an independent predictor of cardiovascular risk.6–7 Recently, Folsom et al8 suggested that cIMT and carotid plaque presence can be included in coronary risk assessments and can be used along with the FRS to help better ascertain risk. The presence and amount of subclinical atherosclerosis differ by race and ethnicity.9–11 In the United States (US), the Hispanic population has almost doubled between 1990 and 2007 (9% to 15%),12 and is projected to reach 30% by the year 2050. Although usually classified as a single ethnic group, Hispanics are actually culturally, socioeconomically, and genetically heterogeneous with varying prevalence of coronary risk factors and extent of subclinical atherosclerosis.13 Of the Hispanics residing in the US, Mexican Americans represent the largest and ethnically distinct subgroup. Hence, understanding and describing prevalent disease and defining risk burden in this minority population are important as the racial/ethnic landscape of the US has changed since the original Framingham cohort was studied. This study aimed to evaluate cIMT and carotid plaquing among a random community-recruited Mexican American cohort, and to correlate these markers of subclinical atherosclerosis with prevalent coronary risk factors and different FRS algorithms.
METHODS
Study Population
This study was approved by the Institutional Review Board of the University of Texas Health Science Center-Houston. Study subjects were drawn from the Cameron County Hispanic Cohort (CCHC) (n=141), recruited from randomly selected blocks according to the 2000 Census as described previously.14 The CCHC is a homogenous community-dwelling Mexican American cohort living in Brownsville (Cameron County), Texas, a city in the lower Rio Grande River at the US-Mexico border.
Extensive family, socioeconomic, educational and personal medical histories were obtained using a directed questionnaire. Surveys and data collection were conducted in the participants’ language of preference (Spanish or English) by bilingual research nurses and field workers. Participants were asked to fast for at least 10 hours overnight before a clinic visit at the Clinical Research Unit. Anthropometric measurements obtained included height, weight, and waist circumference. Waist circumference (visceral adiposity) was measured at the level of the umbilicus to the nearest 0.2 cm, with the subject in a standing position and breathing normally. Height was measured to the nearest 0.2 cm using a stadiometer. Body mass index (BMI) was calculated as weight in kilograms divided by height squared in meters (kg/m2). The average of 3 blood pressure (BP) and HR readings taken 5 minutes apart were used. Laboratory studies performed included fasting lipid panel, hemoglobin (Hb) A1c, fasting plasma glucose, and high sensitivity C-reactive protein (CRP). CRP levels >10mg/L were excluded from analysis as such high levels likely represent acute illness.15
The presence of hypertension was both self-reported and measured as described below. The subject was deemed to be hypertensive if the mean systolic blood pressure (SBP) was ≥ 140mmHg or the mean diastolic blood pressure (DBP) was ≥ 90mmHg.16 Classification of diabetes was also both self-reported and based on measurement of HbA1c (HbA1c >6.5%) as per the latest guidelines from the American Diabetes Association.17 Smoking status was defined as an affirmative answer to the question “Do you currently smoke cigarettes?”. BMI was categorized according to the National Heart Lung and Blood Institute (NHLBI) with overweight defined as a BMI ≥ 25.0 kg/m2, and obesity defined as a BMI ≥ 30.0 kg/m2. Morbid obesity was defined as a BMI ≥ 40.0 kg/m2. Metabolic syndrome was defined according to the criteria used by the American Heart Association and NHLBI as the presence of at least 3 of the following: 1) elevated waist circumference (≥ 102cm in males and ≥ 88cm in females), 2) elevated triglyceride (≥ 150 mg/dL), 3) Low high density lipoprotein cholesterol (HDL-C) (< 40mg/dL in males and < 50mg/dL in females), 4) elevated BP (≥ 130/85mmHg), and 5) elevated fasting glucose (≥ 100mg/dL).18
Framingham Risk Score
Three gender-specific Framingham risk equation scores were calculated based on standard point values for each component. The 10-year coronary heart disease risk used age, total cholesterol, HDL-C, SBP, diabetes, and smoking status.1 This risk score gives the 10 year risk for hard coronary heart disease events, i.e., myocardial infarction or death from coronary heart disease. In addition, FRS was also calculated using a gender-specific multivariable risk factor algorithm to assess the 10-year general cardiovascular risk (coronary artery disease, cerebrovascular disease, peripheral arterial disease and heart failure).19 This FRS algorithm provides a single risk scoring system to assess an individual’s global risk for cardiovascular disease events. Subjects were then categorized based on the 10-year FRS into 3 risk categories: low risk group (<10%), intermediate risk group (10%–20%), or high risk group (>20%).18 Calculation of the FRS long-term (30-year) risk was also performed.5 This long-term risk of general cardiovascular disease events includes both hard coronary heart disease events such as coronary death and myocardial infarction, as well as general cardiovascular disease events such as coronary insufficiency, angina, ischemic stroke, hemorrhagic stroke, transient ischemic attack, peripheral artery disease, and heart failure.5 Subjects older than 59 years are excluded in this analysis as this specific FRS algorithm calculates long-term risk and was validated in subjects ages 20–59 years.5 Subjects were categorized by the 30-year FRS into 3 risk categories as recommended by Pencina et al: low risk group (<12%), intermediate risk group (12%–40%), or high risk group (>40%).5
Carotid Ultrasound Evaluation of Subclinical Atherosclerosis
Carotid ultrasound studies to evaluate subclinical atherosclerosis were performed using the Siemens Acuson X300 ultrasound system using a VF 13-5 linear array transducer. The protocol was designed following guidelines from the American Society of Echocardiography consensus statement on subclinical vascular disease.20 Both common carotids were imaged from three different angles for a total of six images. Carotid plaque presence was determined by examining the carotid bulb, its bifurcation and the carotid branch arteries in addition to the common carotid artery. cIMT was measured using the Carotid Analyzer software (Medical Imaging Applications, Coralville, Iowa), a semi-automated border detection program. Measurements were made at the R-wave of the EKG on a minimum of two clips from each side and the results were averaged. cIMT was categorized as being either < or ≥75th percentile for age and gender.20 Carotid plaque was defined as an area of wall thickening that was >50% of the thickness of the surrounding wall. Abnormal carotid ultrasound was then defined as a cIMT ≥75% for age and gender and/or presence of atherosclerotic plaque. All measurements were performed by a single blinded expert reader. Replicate readings were performed on 5% of the cohort and the intraclass correlation coefficient for our laboratory was 0.96.
Integration of Abnormal Carotid Ultrasound Findings and Framingham Risk Scores
Discordance between abnormal carotid ultrasound findings with FRS were computed and defined as any subject who was classified as low or intermediate risk by FRS who had an abnormal carotid ultrasound study, which reclassifies that subject as high risk. Concordance was defined as an abnormal carotid ultrasound and an actual classification of high risk by FRS.
Statistical Analysis
Data are summarized as mean and standard deviation for continuous variables and frequency and column percentages for categorical variables. Participant demographics were stratified by gender and evaluated using univariate analysis. Student’s t-test was used to compare groups for continuous parametric data, the Kruskall Wallis Test for continuous nonparametric data, and the Chi Square Test Statistic for categorical data. Pearson Product Moment Correlation was used to evaluate associations between variables. A Chi square test was performed to evaluate the trend in concordance between abnormal carotid ultrasound findings and FRS. A p value <0.05 was considered significant. All analyses were performed using SAS 9.2 TS level 1MO (SAS Institute Inc., Cary, NC).
RESULTS
Cohort Profile
A total of 141 cohort subjects had carotid ultrasound studies performed. Demographics are listed in Table 1. Mean age was 53.1 ± 11.7 years (range 24–80 years); 73.8% (n=104) were female. There was a high prevalence of coronary risk factors in this cohort. One in five subjects was hypertensive (27.7%), diabetic (19.9%), or a smoker (24.1%). Women had significantly higher total cholesterol (p=0.026), higher low density lipoprotein cholesterol (LDL-C) levels (p=0.022), but also higher HDL-C (p=0.007) than men. Men were more likely to be smokers than women (40.5% versus 18.3%, p=0.006) but women had higher BMI than men (32.3 ± 6.3 kg/m2 versus 29.9 ± 4.5 kg/m2; p=0.035) than men. Half of the cohort had the metabolic syndrome (53.2%), and more than half were obese (58.9%); 8.5% were morbidly obese. The majority was either overweight or obese (88.7%), and only 11.3% had a normal BMI.
Table 1.
Cohort Demographics.
| Total | Male | Female | P value* (Males vs. Females) |
|
|---|---|---|---|---|
| Continuous variable | Mean ± SD |
Mean ± SD |
Mean ± SD |
|
| Age (years) | 53.1±11.7 | 55.0±14.5 | 52.3±10.6 | NS |
| Mean SBP (mmHg) | 115.4±15.7 | 115.4±14.6 | 115.4±16.2 | NS |
| Mean DBP (mmHg) | 70.3±9.7 | 71.3±8.6 | 70.0±10.1 | NS |
| Fasting Plasma Glucose (mg/dL) | 109.1±32.1 | 110.3±29.6 | 108.6±33.1 | NS |
| HbA1c (%) | 5.0±0.9 | 5.3±0.9 | 5.0±0.9 | NS |
| CRP (mg/L) | 3.5±2.7 | 2.9±2.3 | 3.7±2.8 | NS |
| Total Cholesterol (mg/dL) | 188.6±37.2 | 177.0±34.3 | 192.2±37.5 | 0.026 |
| Triglyceride (mg/dL) | 139.0±68.2 | 157.8±85.6 | 132.3±59.4 | NS |
| HDL-Cholesterol (mg/dL) | 48.6±12.9 | 43.7±10.6 | 50.3±13.2 | 0.007 |
| LDL-Cholesterol (mg/dL) | 111.8±31.8 | 101.6±30.7 | 115.5±31.5 | 0.022 |
| BMI (kg/m2) | 31.7±5.9 | 29.9±4.5 | 32.3±6.3 | 0.035 |
| Waist Circumference (cm) | 104.3±13.1 | 104.1±10.4 | 104.3±13.9 | NS |
| Annual Household Income (USD) | $25,416.0±$24,365.8 | $31,846.4±$27,948.7 | $22,915.3±$22.541.7 | NS |
| Highest Level of Education (years) | 12.5±4.2 | 12.5±4.3 | 12.5±4.2 | NS |
| Categorical variable | n (%) | n (%) | n (%) | |
| Smoker | 34 (24.1) | 15 (40.5) | 19 (18.3) | 0.006 |
| Diabetic | 28 (19.9) | 6 (16.2) | 22 (21.1) | NS |
| Hypertensive | 39 (27.7) | 9 (24.3) | 30 (28.8) | NS |
| Metabolic Syndrome | 75 (53.2) | 21 (56.8) | 54 (51.9) | NS |
| Obese (BMI ≥30 kg/m2) | 83 (58.9) | 17 (45.9) | 66 (63.4) | NS |
Student's t-test for continuous variables and Chi-square test for dichotomous variables.
Carotid Ultrasound Findings
Representative images for cIMT (Figure 1) and carotid plaquing (Figure 2) are shown. The mean cIMT was 0.66±0.15 mm, with no gender differences (0.70 ± 0.17 mm in men versus 0.65 ± 0.14 mm in women; p=NS). cIMT was highly correlated with age (r=0.50, p<0.001). Mean cIMT was higher in patients with hypertension (0.72 ± 0.15 mm versus 0.64 ± 0.14 mm; p=0.007), diabetes (0.75 ± 0.20 mm versus 0.64 ± 0.13 mm; p=0.012), and those with the metabolic syndrome (0.71 ± 0.17 mm versus 0.61 ± 0.11 mm; p<0.001), but did not differ by smoking status. After controlling for age and gender, mean cIMT remained significantly correlated with diabetes (p=0.006), fasting glucose levels (p<0.001), HbA1c (p<0.001), total cholesterol (p=0.041), triglycerides (p=0.008), SBP (p=0.002), metabolic syndrome (p=0.008), and obesity (p=0.035).
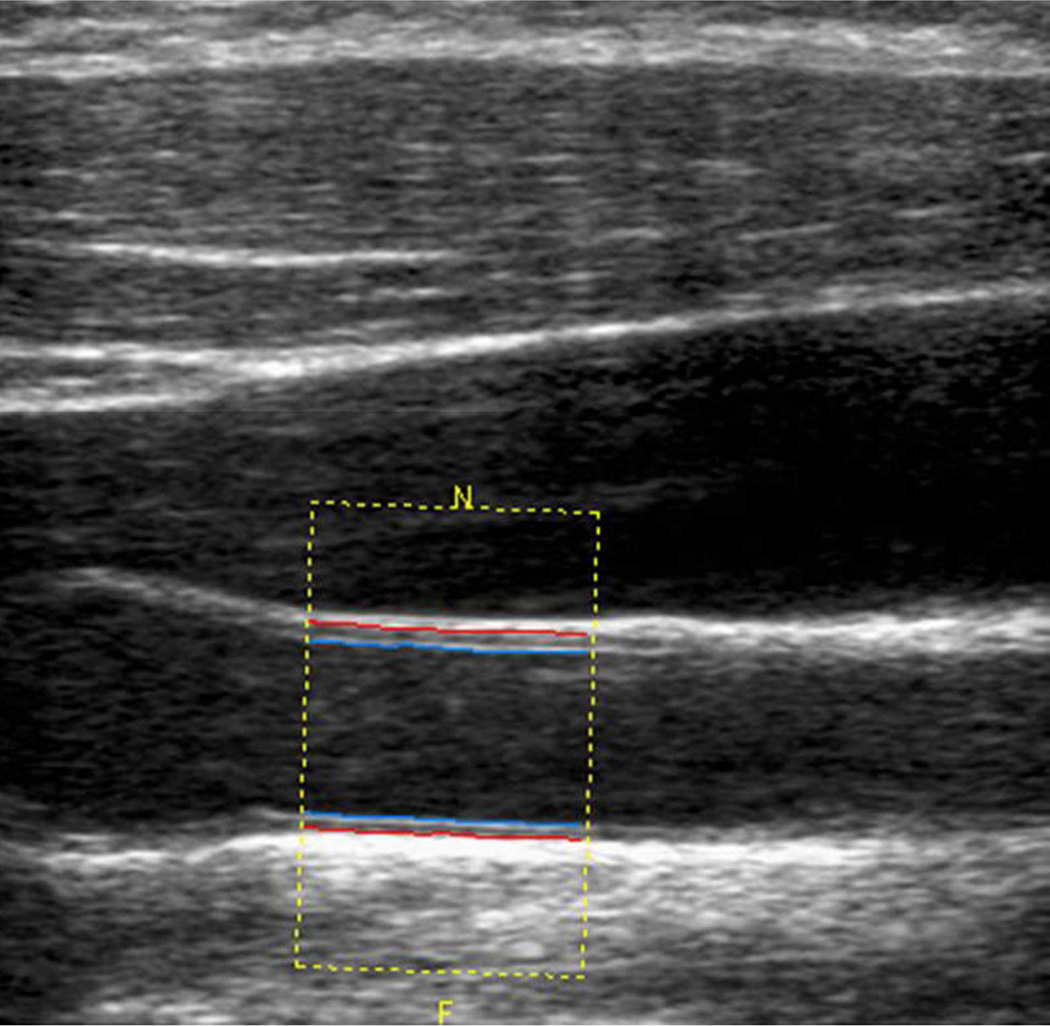
Figure 1.
Measured carotid intima-media thickness (cIMT) for one of the six angles used to calculate an averaged cIMT. On the image, the red line is the media-adventitia border and the blue line is the blood-intima border.
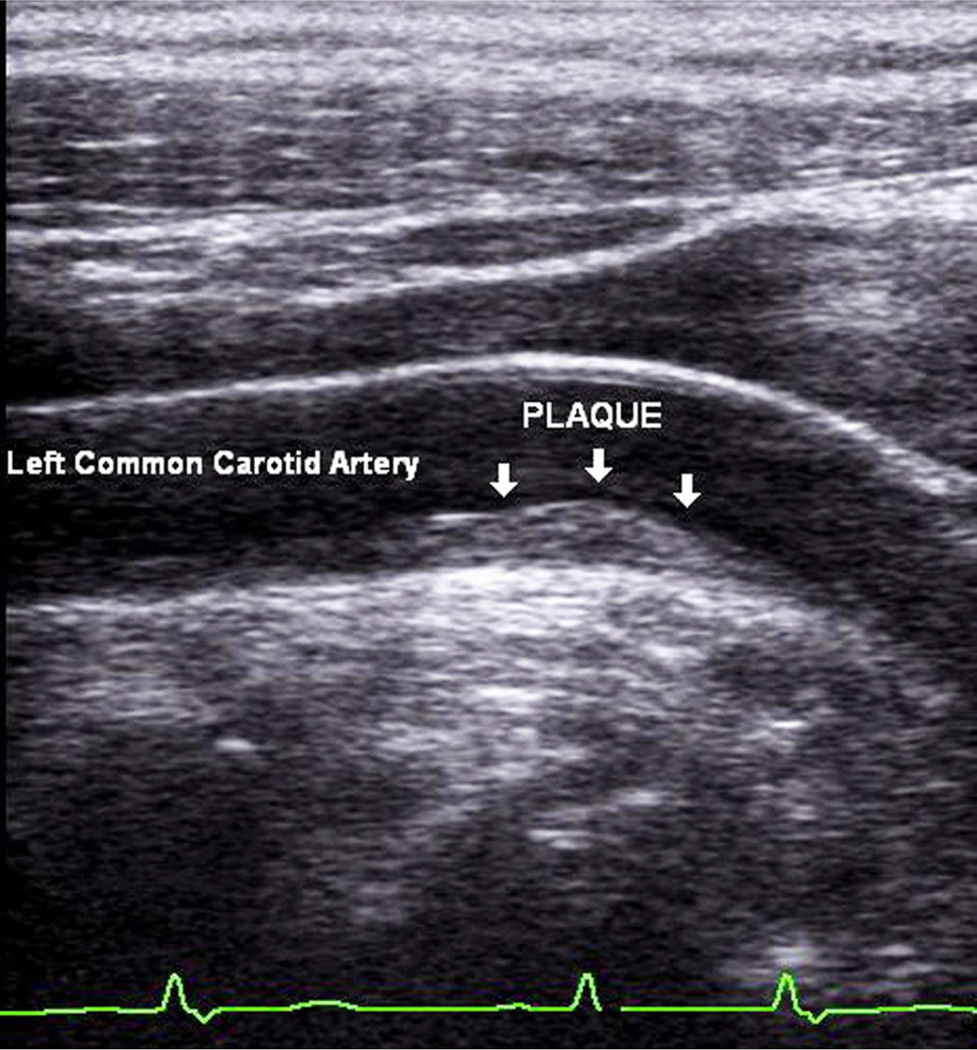
Figure 2.
Soft plaque in the left common carotid artery of a 72 year old female subject.
One third of the cohort (n=49; 34.8%) had abnormal carotid ultrasound findings. The prevalence for each component was 16.8% for cIMT ≥75th percentile for age and gender, and 23.1% for presence of atherosclerotic plaque. There were no gender differences between these variables. Abnormal carotid ultrasound findings were more prevalent in older subjects (p<0.001), hypertensives (p<0.001), diabetics (p=0.020), and in those with the metabolic syndrome (p=0.002) [Table 2]. Abnormal carotid ultrasound findings were also more prevalent in subjects with higher mean SBP (p<0.001), higher fasting plasma glucose (p=0.041) and HbA1c (p=0.010), and those with lower education levels (p=0.004) [Table 2].
Table 2.
Carotid Ultrasound Findings.
| Abnormal Carotid Ultrasound n=49 |
Normal Carotid Ultrasound n=92 |
P value* | |
|---|---|---|---|
| Continuous Variable | Mean ± SD | Mean ± SD | |
| Age (years) | 59.4±8.1 | 49.7±12.0 | <0.001 |
| Mean SBP (mmHg) | 122.0±17.3 | 111.9±13.7 | <0.001 |
| Mean DBP (mmHg) | 70.8±10.3 | 70.0±9.5 | NS |
| Fasting Plasma Glucose (mg/dL) | 117.6±39.2 | 104.2±26.7 | 0.041 |
| HbA1c (%) | 5.5±1.4 | 4.8±0.4 | 0.010 |
| CRP (mg/L) | 3.2±2.4 | 3.6±2.8 | NS |
| Total Cholesterol (mg/dL) | 193.9±39.8 | 185.8±35.6 | NS |
| Triglyceride (mg/dL) | 147.5±73.7 | 134.3±64.1 | NS |
| HDL-Cholesterol (mg/dL) | 48.1±16.1 | 48.8±10.9 | NS |
| LDL-Cholesterol (mg/dL) | 115.3±34.2 | 110.0±30.4 | NS |
| BMI (kg/m2) | 31.5±5.1 | 31.7±6.4 | NS |
| Waist Circumference (cm) | 103.9±11.1 | 104.5±14.0 | NS |
| Annual Household Income (USD) | $20,658.3±$17,138.7 | $28,457.8±$27,738.8 | NS |
| Highest Level of Education (years) | 11.2±4.1 | 13.3±4.1 | 0.004 |
| Categorical Variable | n (%) | n (%) | |
| Females | 32 (65.3) | 72 (78.3) | NS |
| Smoker | 15 (30.6) | 19 (20.6) | NS |
| Diabetes | 15 (30.6) | 13 (14.1) | 0.020 |
| Hypertensive | 22 (44.9) | 17 (18.5) | <0.001 |
| Metabolic Syndrome | 34 (69.4) | 41 (44.6) | 0.002 |
| Obese (BMI ≥ 30 kg/m2) | 30 (61.2) | 53 (57.6) | NS |
Student's t-test for continuous variable and Chi-square test for dichotomous variable
Framingham Risk Scores
Hard Coronary Heart Disease 10-Year Risk
The calculated overall cohort 10-year risk for hard coronary heart disease events was deemed to be low with a mean FRS of 4.1 ± 5.5%. The mean 10-year FRS for coronary heart disease was significantly higher in Mexican American men compared to women (10.2 ± 7.9% versus 2.0 ± 2.0%; p<0.001). Among Mexican American men, 48.7% were deemed to be in the low risk group, 32.4% in the intermediate risk group, and 18.9% were considered to be in the high risk group. In contrast, all Mexican American women were classified in the low risk group, despite the high prevalence of multiple risk factors in these women as described above. In this cohort, 86.5% were deemed to be in the low risk group; however, nearly a third (32.0%) of these “low risk” subjects actually had evidence of subclinical atherosclerosis by carotid ultrasound (Table 3). Subjects with abnormal carotid ultrasound findings had significantly higher 10-year risk for hard coronary heart disease events than those who had normal carotid ultrasound findings (6.6 ± 6.6% versus 2.9 ± 4.3%, p<0.001). Among those with abnormal carotid ultrasound, the majority (79.6%) were classified as being at low risk for coronary heart disease by FRS. Carotid ultrasound reclassified nearly a third of the cohort (31.9%; n=45; 13 males and 32 females) as actually being at high risk for myocardial infarction or coronary death (Table 3).
Table 3.
Carotid Ultrasound Findings and Framingham Risk Score. Number of participants in each category of the Framingham Risk Scores (low, intermediate, and high) related to normal or abnormal carotid ultrasound findings.
| Framingham Risk Score | Total | Abnormal Carotid Ultrasound |
Normal Carotid Ultrasound |
|---|---|---|---|
| Hard Coronary Heart Disease 10-Year Risk (n=141) | |||
| Low [n (%)] | 122 (86.5) | 39 (32.0) | 83 (68.0) |
| Intermediate [n (%)] | 12 (8.5) | 6 (50.0) | 6 (50.0) |
| High [n (%)] | 7 (5.0) | 4 (50.0) | 3(42.9) |
| General Cardiovascular Disease 10-Year Risk (n=141) | |||
| Low [n (%)] | 90 (63.8) | 19 (21.1) | 71 (78.9) |
| Intermediate [n (%)] | 32 (22.7) | 17 (53.1) | 15 (46.9) |
| High [n (%)] | 19 (13.5) | 13 (68.4) | 6 (31.6) |
| General Cardiovascular Disease 30-Year Risk (n=86) | |||
| Low [n (%)] | 16 (18.6) | 0 (0) | 16 (100.0) |
| Intermediate [n (%)] | 40 (46.5) | 8 (20.0) | 32 (80.0) |
| High [n (%)] | 30 (34.9) | 16 (53.3) | 14 (46.7) |
General Cardiovascular Disease 10-Year Risk
The calculated 10-year risk for general cardiovascular disease for the cohort was higher at 9.2 ± 8.6%, but similarly places the cohort at low risk for coronary artery disease, cerebrovascular disease, peripheral arterial disease, and heart failure. The mean 10-year FRS for general cardiovascular disease was significantly higher in Mexican American men compared to women (15.0 ± 10.7% versus 7.1 ± 6.6%; p<0.001). Among Mexican American men, 43.2% were deemed to be in the low risk group, 18.9% in the intermediate risk group, and 37.8% were deemed to be in the high risk group. Among Mexican American women, the majority (71.2%) were deemed to be in the low risk group, while 24.0% were in the intermediate risk group, and only 4.8% were categorized into the high risk group. In this cohort, the majority (63.8%) were deemed to be at low risk for general cardiovascular disease in 10 years. Similarly however, 21.1% of these “low risk” subjects actually already had evidence of subclinical atherosclerosis (Table 3). Subjects with abnormal carotid ultrasound findings had significantly higher 10-year risk for general cardiovascular disease than those who had normal carotid ultrasound findings (14.1 ± 9.1% versus 6.5 ± 7.0%, p<0.001). Among those with abnormal carotid ultrasound, more than a third (38.8%) were classified by FRS as being at low risk for coronary artery disease, cerebrovascular disease, peripheral arterial disease or heart failure in 10 years. Carotid ultrasound reclassified 25.5% of the cohort (n=36; 8 males and 28 females) as actually being at high risk for general cardiovascular disease (Table 3).
Cardiovascular Disease 30-Year Risk
Subjects older than 59 years were excluded in this analysis (n=55) as this FRS algorithm calculates long-term risk and was validated in subjects ages 20–59 years.5 This subgroup has a mean age of 46.2 ±8.8 years (range 24–59 years). The calculated 30-year risk for cardiovascular disease for the cohort was 32.1 ± 21.4%, which places them at intermediate risk for general cardiovascular disease events within 30 years. The mean 30-year FRS for general cardiovascular disease was not significantly different between Mexican American men and women (37.8 ± 23.8% versus 30.5 ± 20.5%; p=NS). Among Mexican American men, 26.3% were deemed to be in the low risk group, while 21.5% were in the intermediate risk group, and the majority (52.6%) were deemed to be in the high risk group. Among Mexican American women, 16.4% were deemed to be in the low risk group, 53.7% in the intermediate risk group, and 29.9% were categorized into the high risk group. In this cohort, nearly half (46.5%) were deemed to be at intermediate risk for general cardiovascular disease in 30 years (Table 3).
Subjects with abnormal carotid ultrasound findings had significantly higher 30-year risk for general cardiovascular disease than those who had normal carotid ultrasound findings (46.8 ± 16.9% versus 26.4 ± 20.3%, p<0.001). No subject with an abnormal carotid ultrasound was classified as low risk using this FRS algorithm (Table 3). Among those who had abnormal carotid ultrasound findings, the majority (53.3%) were classified as high risk. Among those with an abnormal carotid ultrasound, 20.8% were classified as being at intermediate 30-year risk for cardiovascular disease, and carotid ultrasound reclassified these subjects (3 males and 11 females) as actually being at high risk for general cardiovascular disease in 30 years.
Integration of Abnormal Carotid Ultrasound Findings and Framingham Risk Scores
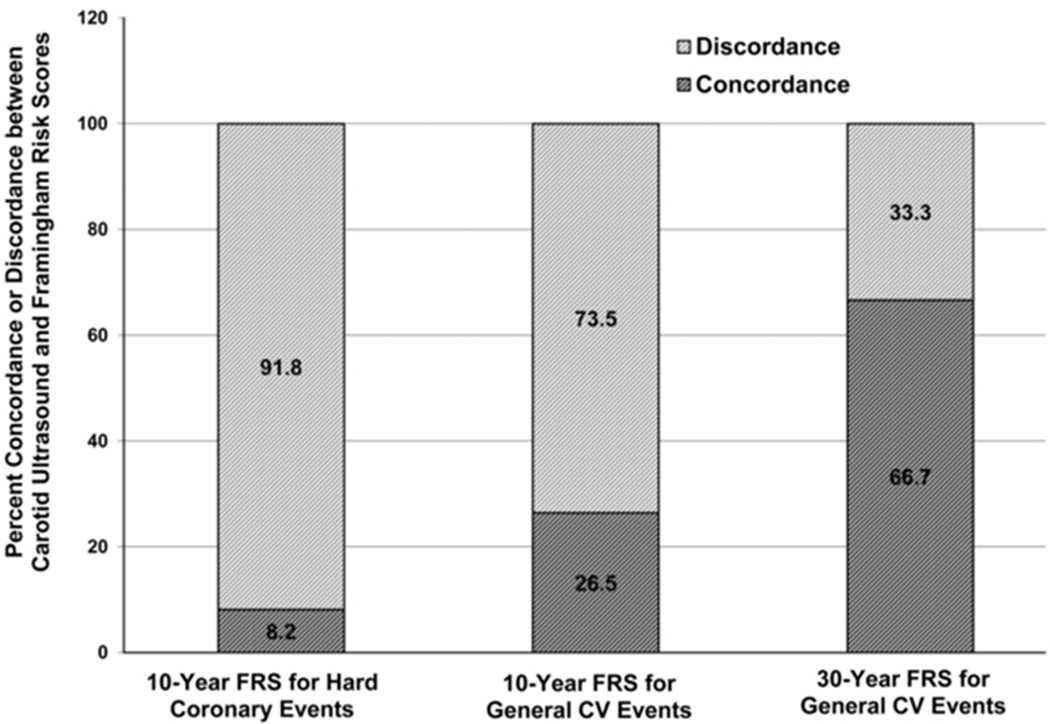
Among subjects with abnormal carotid ultrasound, 91.8% (n=45) had discordant results with the 10-year FRS for hard coronary heart disease events, and concordance between an abnormal carotid ultrasound and classification of high risk was seen in only 8.2% (n=4) of the subjects (Figure 3). Concordance was higher when 10-year FRS for general cardiovascular disease, and not just hard coronary events, was used, with 26.5% (n=13) showing agreement between an abnormal carotid ultrasound and classification of high risk by FRS. Nevertheless, the majority (73.5%; n=36) still had discordant results. Concordance was highest when a long term risk prediction algorithm was used (Figure 3; p=0.018). Concordance between the 30-year FRS for general cardiovascular disease and carotid ultrasound was 66.7% (n=16) and no subject with an abnormal carotid ultrasound was classified as low risk using this algorithm (discordance rate of 33.3%; n=8).
Figure 3.
Percent concordance and discordance between abnormal carotid ultrasound findings and Framingham risk Scores (FRS). Numbers represent percent of participants in each category of the FRS with abnormal carotid ultrasound findings and concordant or discordant Framingham risk classification. Chi square test for trend showed a significant difference in concordance between abnormal carotid ultrasound findings and the different FRS, being highest for the 30-year FRS for general cardiovascular events (p=0.018).
DISCUSSION
This study highlights the limitations of using the 10-year risk scoring by the FRS in a homogeneous Mexican American cohort. The overall estimated 10-year risk in this cohort was low (<10%) despite the marked prevalence of coronary risk factors, including a prevalence of overweight and obesity of 88.7%. Furthermore, all Mexican American women were classified in the low risk group for hard coronary heart disease events in 10 years, despite the high prevalence of multiple risk factors in these women including an obesity prevalence of 63.4% and a prevalence of metabolic syndrome of 51.9%. In this study, we found that a substantial proportion of Mexican Americans who were categorized into the low to intermediate 10-year risk group actually already had evidence of subclinical atherosclerosis, warranting reclassification into the high risk category. This discordance between 10-year FRS and carotid ultrasound findings was noted whether risk was assessed for hard coronary events (myocardial infarction or coronary death) or global risk was assessed for any cardiovascular event (development of coronary artery disease, cerebrovascular disease, peripheral arterial disease or heart failure), although discordance was less when global risk was considered versus only hard coronary events (73.5% versus 91.8%). Concordance between FRS and carotid ultrasound findings was best when long-term (30-year) risk was assessed (discordance of 33.3%) and no subject with an abnormal carotid ultrasound was categorized as low risk by the 30-year FRS algorithm. Integration of carotid ultrasound findings to coronary risk assessments and use of longer term prediction models may help better predict risk in this minority population, with resultant earlier initiation of appropriate therapies.
Although the FRS is a widely used method for estimating cardiovascular risk, it has recognized limitations, one of which is that it was derived from a mostly white Caucasian population. The FRS has been applied with reasonable effectiveness on other minority populations but often necessitated recalibration.2, 21–22 To our knowledge, there have been no studies demonstrating its applicability in Mexican Americans. The FRS uses only standard risk factors (age, gender, BP, total cholesterol, HDL cholesterol, diabetes, and smoking), but other risk factors such as insulin resistance, overweight and obesity, and the metabolic syndrome can contribute to the development of atherosclerosis and are highly prevalent among Mexican Americans; these are not accounted for in the FRS point system. Smoking and diabetes are considered only as dichotomous variables, i.e., whether they are absent or present, but the true burden of these risk factors is likely better described as a continuum. There is also a highly dominant effect of age and gender in the FRS algorithm compared to the other risk factors,23and FRS often underestimates risk in women and the young.24
Carotid IMT has been found to predict future risk of myocardial infarction and stroke, and a change in cIMT has been validated as a vascular marker for the progression of atherosclerosis.25–28 Some preventive trials with lipid-lowering medications that used cIMT as a surrogate endpoint have shown that retardation in the progression of cIMT is accompanied by a reduction in cardiovascular endpoints.29 It has already been suggested that noninvasive imaging can be used for subjects deemed to be at intermediate risk to help in further stratification to decide which patients will benefit from intensification of preventive therapy. However, FRS has been shown to have low predictive accuracy particularly in the low risk category.30–31 Our results showed that there is a substantial proportion of subjects in this community-based cohort who were classified into the low 10-year risk category who warranted reclassification into the high risk category. These subjects may actually be at a greater disadvantage than those categorized into the intermediate risk group as being categorized into the low risk group gives both the patient and the healthcare provider a false sense of security which then precludes initiation or intensification of life-saving preventive therapies. Hence carotid ultrasonography may be valuable not only for the intermediate risk patients but perhaps also for the low risk group. Classification of individuals as low risk, who then develop a cardiovascular event, represents a failure of the risk assessment tool used and this error needs to be regarded as a missed opportunity for preventive care.
Global and longer-term prediction tools complement short-term risk assessments as they provide a better estimate of the morbidity burden of coronary risk factors.32–33 Ten-year FRS may underestimate the true risk burden in some individuals, particularly women and the young, and they are often categorized into the low 10-year risk group for cardiovascular events, but in reality their lifetime risk for these events is substantial.33 In this study, using the 30-year FRS algorithm better stratified our subjects and there was better concordance between the 30-year FRS and the carotid ultrasound findings. Furthermore, the calculated mean 30-year FRS for the cohort was 32.1%, which places the cohort at intermediate risk for general cardiovascular disease events within 30 years, as opposed to a classification of low risk (4.1%) using the 10-year FRS. A long-term risk score may better motivate both physicians and patients into instituting and adhering to recommended preventive therapies and healthy behaviors, and may serve as a useful tool in public health education strategies.
There are some factors that may affect our results. Our sample size is small. Our cohort is also relatively young with a predominance of women. FRS has been shown to underestimate risk in these subgroups even among Whites.24 This is a cross-sectional study and cIMT was only evaluated once without long term follow-up. Prospective studies are needed to determine whether reclassification to a higher FRS category actually translates to increased cardiac events. Longitudinal data are currently being collected and will provide this answer.
The current study has a number of strengths one of which is the homogeneity of the cohort studied. To fully understand prevalent risk among Hispanics, the Hispanic population needs to be disaggregated into subgroups according to national origins and other characteristics34 as the paradoxical and conflicting findings related to health among Hispanics may reflect aggregation error of outcomes data across widely varied subgroups.35
In summary, a substantial gap still remains in the detection of asymptomatic individuals who ultimately develop coronary heart disease. The FRS is only moderately accurate for the prediction of short and long term risk of manifesting a major coronary event.36 The addition of personalized risk assessment by the noninvasive imaging of subclinical atherosclerosis could complement currently used risk assessment tools. Carotid ultrasonography is simple and safe, uses no radiation, is sensitive and reproducible, and is a relatively inexpensive test that can be brought to the community to assess for the presence of subclinical atherosclerosis. Using carotid ultrasound as a tool for motivating lifestyle changes and risk reduction has also been shown to be effective.37 The findings in this study are particularly relevant to future public health planning given the changing landscape of the composition of the US population.
ACKNOWLEDGEMENT
We thank our cohort team, particularly, Elizabeth Rangel, Julie Ramirez, Jody Rodriguez, and Rocio Uribe who not only recruited and documented the participants, but also performed the ultrasound studies under expert supervision. We also thank Marcela Montemayor and other laboratory staff for their contributions, and Christina Villarreal for administrative support. We thank Valley Baptist Medical Center, Brownsville, Texas for providing us space for our Center for Clinical and Translational Science Clinical Research Unit. We also thank the community of Brownsville and the participants who so willingly participated in this study in their city.
**This work was supported by MD000170 P20 funded from the National Center on Minority Health and Health Disparities, and the Centers for Translational Science Award 1U54RR023417-01 from the National Center for Research Resources
REFERENCES
- 1.Wilson PW, D'Agostino RB, Levy D, et al. Prediction of coronary heart disease using risk factor categories. Circulation. 1998;97(18):1837–1847. doi: 10.1161/01.cir.97.18.1837. [DOI] [PubMed] [Google Scholar]
- 2.D'Agostino RB, Grundy S, Sullivan LM, et al. Validation of the Framingham coronary heart disease prediction scores: Results of a multiple ethnic groups investigation. JAMA. 2001;286(2):180–187. doi: 10.1001/jama.286.2.180. [DOI] [PubMed] [Google Scholar]
- 3.Williams R, Bhopal R, Hunt K. Coronary risk in a British Punjabi population: Comparative profile of non-biochemical factors. Int J Epidemiol. 1994;23(1):28–37. doi: 10.1093/ije/23.1.28. [DOI] [PubMed] [Google Scholar]
- 4.Keys A, Menotti A, Aravanis C, et al. The Seven Countries Study: 2,289 deaths in 15 years. Prev Med. 1984;13:141–154. doi: 10.1016/0091-7435(84)90047-1. [DOI] [PubMed] [Google Scholar]
- 5.Pencina MJ, D’Agostino RB, Sr, Larson MG, et al. Predicting the 30-year risk of cardiovascular disease: The Framingham Heart Study. Circulation. 2009;119:3078–3084. doi: 10.1161/CIRCULATIONAHA.108.816694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Greenland P, Abrams J, Aurigemma GP, et al. Prevention Conference V: Beyond secondary prevention: Identifying the high-risk patient for primary prevention: Noninvasive tests of atherosclerotic burden: Writing Group III. Circulation. 2000;101:E16–E22. doi: 10.1161/01.cir.101.1.e16. [DOI] [PubMed] [Google Scholar]
- 7.Roman MJ, Naqvi TZ, Gardin JM, et al. Clinical application of noninvasive vascular ultrasound in cardiovascular risk stratification: A report from the American Society of Echocardiography and the Society of Vascular Medicine and Biology. J Am Soc Echocardiogr. 2006;19:943–954. doi: 10.1016/j.echo.2006.04.020. [DOI] [PubMed] [Google Scholar]
- 8.Folsom AR, Kronmal RA, Detrano RC, et al. Coronary artery calcification compared with carotid intima-media thickness in the prediction of cardiovascular disease incidence: The Multi-Ethnic Study of Atherosclerosis (MESA) Arch Intern Med. 2008;168(12):1333–1339. doi: 10.1001/archinte.168.12.1333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wassel CL, Pankow JS, Peralta CA, et al. Genetic ancestry is associated with subclinical cardiovascular disease in African-Americans and Hispanics from the Multi-Ethnic Study of Atherosclerosis. Circ Cardiovasc Genet. 2009;2:629–636. doi: 10.1161/CIRCGENETICS.109.876243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.D'Agostino RB, Burke G, O’Leary D, et al. Ethnic differences in carotid wall thickness: The Insulin Resistance Atherosclerosis Study. Stroke. 1996;27:1744–1749. doi: 10.1161/01.str.27.10.1744. [DOI] [PubMed] [Google Scholar]
- 11.Manolio TA, Arnold AM, Post W, et al. Ethnic differences in the relationship of carotid atherosclerosis to coronary calcification: The Multi-Ethnic Study of Atherosclerosis. Atherosclerosis. 2008;197:132–138. doi: 10.1016/j.atherosclerosis.2007.02.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bernstein R. US Hispanic population surpassed 45 million: Now 15 percent of total US. [Accessed March 2, 2011];Census Bureau News. 2008
- 13.Allison MA, Budoff MJ, Wong ND, et al. Prevalence of and risk factors for subclinical cardiovascular disease in selected US Hispanic ethnic groups: The Multi-Ethnic Study of Atherosclerosis. Am J Epidemiol. 2008;167:962–969. doi: 10.1093/aje/kwm402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Fisher-Hoch SP, Rentfro AR, Salinas JJ, et al. Socioeconomic status and prevalence of obesity and diabetes in a Mexican American community, Cameron County, Texas, 2004–2007. Prev Chronic Dis. 2010;7:A53. (Abstract). [PMC free article] [PubMed] [Google Scholar]
- 15.Pearson TA, Mensah GA, Alexander W, et al. Markers of inflammation and cardiovascular disease: Application to clinical and public health practice: A statement for healthcare professionals from the Centers for Disease Control and Prevention and the American Heart Association. Circulation. 2003;107:499–511. doi: 10.1161/01.cir.0000052939.59093.45. [DOI] [PubMed] [Google Scholar]
- 16.Chobanian AV, Bakris GL, Black HR, et al. Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension. 2003;42:1206–1252. doi: 10.1161/01.HYP.0000107251.49515.c2. [DOI] [PubMed] [Google Scholar]
- 17.Executive summary: Standards of medical Care in diabetes- 2010. Diabetes Care. 2010;33(Suppl 1):S4–S10. doi: 10.2337/dc10-S004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Grundy SM, Becker D, Clark LT, et al. Executive summary of the third report of the National Cholesterol Education Program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults. JAMA. 2001;285:2486–2497. doi: 10.1001/jama.285.19.2486. [DOI] [PubMed] [Google Scholar]
- 19.D'Agostino RB, Vasan RS, Pencina MJ, et al. General cardiovascular risk profile for use in primary care: The Framingham Heart Study. Circulation. 2008;117(6):743–753. doi: 10.1161/CIRCULATIONAHA.107.699579. [DOI] [PubMed] [Google Scholar]
- 20.Stein JH, Korcarz CE, Hurst T, et al. American Society of Echocardiography Carotid Intima-Media Thickness Task Force. Use of carotid ultrasound to identify subclinical vascular disease and evaluate cardiovascular disease risk: A consensus statement from the American Society of Echocardiography Carotid Intima-Media Thickness Task Force Endorsed by the Society for Vascular Medicine. J Am Soc Echocardiogr. 2008;21:93–111. doi: 10.1016/j.echo.2007.11.011. [DOI] [PubMed] [Google Scholar]
- 21.Marrugat J, D’Agostino R, Sullivan L, et al. An adaptation of the Framingham coronary heart disease risk function to European Mediterranean areas. J Epidemiol Community Health. 2003;57:634–638. doi: 10.1136/jech.57.8.634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Liu J, Hong Y, D’Agostino RB, Sr, et al. Predictive value for the Chinese population of the Framingham CHD risk assessment tool compared with the Chinese Multi-Provincial Cohort Study. JAMA. 2004;291:2591–2599. doi: 10.1001/jama.291.21.2591. [DOI] [PubMed] [Google Scholar]
- 23.Enriquez JR, De Lemos JA. Should we focus on novel risk markers and screening tests to better predict and prevent cardiovascular disease? Prev Cardiol. 2010;13(4):152–159. doi: 10.1111/j.1751-7141.2010.00080.x. [DOI] [PubMed] [Google Scholar]
- 24.Abe Y, Rundek T, Sciacca RR, et al. Ultrasound assessment of subclinical cardiovascular disease in a community-based multiethnic population and comparison to the Framingham score. Am J Cardiol. 2006;98:1374–1378. doi: 10.1016/j.amjcard.2006.06.034. [DOI] [PubMed] [Google Scholar]
- 25.Bots ML, Grobbee DR. Intima media thickness as a surrogate marker for generalized atherosclerosis. Cardiovasc Drug Ther. 2002;16:341–351. doi: 10.1023/a:1021738111273. [DOI] [PubMed] [Google Scholar]
- 26.Bots ML, Hoes AW, Koudstaal PJ, et al. Common carotid intima-media thickness and risk of stroke and myocardial infarction: The Rotterdam Study. Circulation. 1997;96:1432–1437. doi: 10.1161/01.cir.96.5.1432. [DOI] [PubMed] [Google Scholar]
- 27.O’Leary DH, Polak JF, Krommal RA, et al. Carotid-artery intima and media thickness as a risk factor for myocardial infarction and stroke in older adults. N Engl J Med. 1999;340:14–22. doi: 10.1056/NEJM199901073400103. [DOI] [PubMed] [Google Scholar]
- 28.Lorenz MW, Markus HS, Bots ML, et al. Prediction of clinical cardiovascular events with carotid intima-media thickness: A systematic review and meta-analysis. Circulation. 2007;115:459–467. doi: 10.1161/CIRCULATIONAHA.106.628875. [DOI] [PubMed] [Google Scholar]
- 29.Furberg CD, Adams HP, Jr, Applegate WB, et al. Effect of Lovastatin on early carotid atherosclerosis and cardiovascular events. Asymptomatic Carotid Artery Progression Study (ACAPS) Research Group. Circulation. 1994;90:1679–1687. doi: 10.1161/01.cir.90.4.1679. [DOI] [PubMed] [Google Scholar]
- 30.Akosah KO, Schaper A, Cogbill C, et al. Preventing myocardial infarction in the young adult in the first place: How do the National Cholesterol Education Panel III Guidelines perform? J Am Coll Cardiol. 2003;41:1475–1479. doi: 10.1016/s0735-1097(03)00187-6. [DOI] [PubMed] [Google Scholar]
- 31.Michos ED, Vasamreddy CR, Becker DM, et al. Women with a low Framingham risk score and a family history of premature coronary heart disease have a high prevalence of subclinical coronary atherosclerosis. Am Heart J. 2005;150:1276–1281. doi: 10.1016/j.ahj.2005.02.037. [DOI] [PubMed] [Google Scholar]
- 32.Lloyd-Jones DM. Short term versus long-term risk for coronary artery disease: Implications for lipid guidelines. Curr Opin Lipidol. 2006;17:619–625. doi: 10.1097/MOL.0b013e3280108740. [DOI] [PubMed] [Google Scholar]
- 33.Lloyd-Jones DM, Leip EP, Larson MG, et al. Prediction of lifetime risk for cardiovascular disease by risk factor burden at 50 years of age. Circulation. 2006;113:791–798. doi: 10.1161/CIRCULATIONAHA.105.548206. [DOI] [PubMed] [Google Scholar]
- 34.Zsembik BA, Fennell D. Ethnic variation in health and the determinants of health among Latinos. Soc Sci Med. 2005;61:53–63. doi: 10.1016/j.socscimed.2004.11.040. [DOI] [PubMed] [Google Scholar]
- 35.Hummer RA, Rogers RG, Amir SH, et al. Adult mortality differentials among Hispanic subgroups and Non-Hispanic Whites. Soc Sci Quart. 2000;81:459–476. [PubMed] [Google Scholar]
- 36.Pasternak RC, Abrams J, Greenland P, et al. 34th Bethesda Conference: Task force #1--Identification of coronary heart disease risk: Is there a detection gap? J Am Coll Cardiol. 2003;41(11):1863–1874. doi: 10.1016/s0735-1097(03)00358-9. [DOI] [PubMed] [Google Scholar]
- 37.Bovet P, Perret F, Cornuz J, et al. Improved smoking cessation in smokers given ultrasound photographs of their own atherosclerotic plaques. Prev Med. 2002;34:215–220. doi: 10.1006/pmed.2001.0976. [DOI] [PubMed] [Google Scholar]