Abstract
Objectives
To investigate the effect of rhinophototherapy with medical therapy on quality of life in persistent allergic rhinitis.
Methods
A prospective, randomized study was being performed between December 2009 and March 2010. The study included 65 patients with persistent allergic rhinitis. The diagnosis was confirmed with positive skin tests. All of the patients had house dust mite allergies. We divided the patients into two groups. First group (n=33) was given topical mometasone furoate 200 mcg/day and levocetirizine 5 mg/day for a month. Rhinophototherapy was applied with the same medical therapy to the second group (n=32), twice a week for three weeks continuously. Rhinophototherapy included visible light, ultraviolet A and ultraviolet B. We evaluated patients before the treatment, at the first month and at the third month after treatment with rhinoconjunctivitis quality of life questionnaire, nasal symptom scores and visual analogue scale (VAS) scores.
Results
Improvements of all variables of the quality of life questionnaire, nasal symptom scores and VAS were statistically significant in the second group both on the first and the third months when compared with the first group.
Conclusion
Allergic rhinitis is a social problem and impairs quality of life. Rhinophototherapy with medical therapy improves the quality of life in allergic rhinitis.
Keywords: Allergic rhinitis, Rhinophototherapy, Quality of life, Symptoms scores, Visual analogue scale
INTRODUCTION
Allergic rhinitis is an allergen-induced, IgE-mediated inflammation of the nasal mucosa [1], and it is the most frequent atopic disease which effects 25%-35% of the population with increasing prevalences [2,3]. Allergic rhinitis is also a social problem that negatively effects the patients' quality of life, performance and productivity, and thus, it is accepted as a major chronic respiratory disease with economic burdens and the risks for asthma [4]. There are several different therapy strategies for allergic rhinitis [4,5]. Allergen avoidance and patient education are important for every allergic patient [6,7]. Immunotherapy is the main treatment modality that changes the course of the disease [8]. Pharmacotherapy plays an important role in the management of allergic rhinitis, with aims to improve patient's quality of life by reducing the symptoms. However, in some patients, symptoms cannot be reduced with only medical treatment or medical treatment can be restricted due to several reasons. Alternative modalities are necessary for such patients.
Phototherapy, which has been mainly used for inflammatory skin diseases dermatologically for a long time, is becoming a new choice of alternative treatment in allergic rhinitis [9]. It has been reported that intranasal applications of phototherapy in allergic rhinitis patients has been effective, similarly to the applications on dermatological diseases [10-13]. Both atopic dermatitis and allergic rhinitis are different manifestations of the atopy and most of the their pathways are similar [14]. Phototherapy consists of ultraviolet and a visible light and its therapeutic effect is mostly attributed to its local immunosuppressive and immunomodulant actions. Phototherapy is able to inhibit the effector phase of the allergic reactions, such as inhibition of antigen presentation by dentritic cells, inducing apoptosis of immune cells, inhibition of synthesis and release of pro-inflammatory mediators from eosinophils, mast cells, basophils and T cells [14].
With this positively correlated data, we aim to investigate the effects of rhinophototherapy with medical therapy on the quality of life with persistent allergic rhinitis in this study.
MATERIALS AND METHODS
A prospective, randomized study was performed between December 2009 and March 2010. The study included 65 patients with a history of at least 2 years of moderate to severe persistent allergic rhinitis. The diagnosis was confirmed with positive skin tests, and all of the patients had house dust mite allergy. The study protocol was approved by the local ethical committee and written consent was obtained from each volunteer. Patients with nasal polyps, nasal septal deviation, nasopharyngeal pathologies, asthma, acute respiratory infections were excluded. All of patients in the study had used antihistamines and/or intranasal steroids previously but not within two weeks prior to beginning of the study.
We divided the patients into two groups for different treatment regimens. A randomization list was formed using simple randomization. The patients were assigned to their respective study groups by an investigator who blinded to the study treatment, using the randomization list. First group (n=33) was given topical mometasone furoate 200 mcg/day and oral levocetirizine 5 mg/day for a month. With the same medical therapy, rhinophototherapy was applied to the second group (n=32), twice a week for three weeks continuously. We evaluated the patients before the treatment, at the first and third months after the treatment with rhinoconjunctivitis quality of life questionnaire (RQLQ), symptom scores and visual analogue scale (VAS) scores. Nasal symptoms evaluated in this study were sneezing, nasal obstruction, rhinorea and nasal itching. All symptoms were graded according to the severity (0, none; 1, mild; 2, moderate; 3, severe). The RQLQ had 28 questions in seven domains (activity limitation, sleep problems, nose symptoms, eye symptoms, non-nose non-eye symptoms, practical problems and emotional function) and each question was scaled from 0 (not impaired at all) to 6 (severely impaired). VAS scores for severity of allergic rhinitis were also evaluated.
Statistical analyses
Data were analysed using the SPSS ver. 13.0 (SPSS Inc., Chicago, IL, USA) and Sigmastat ver. 3.1 (Systat Software Inc., San Jose, CA, USA). Chi square test was used to compare the sex and age distributions of the patients. Comparison of age distribution of groups was performed using independent samples t-test. Variation of mean values of nasal symptom scores, VAS scores and RQLQ scores during the treatment periods within the groups were compared by Wilcoxon signed rank test and Friedman test. The initial mean values of nasal symptom scores, VAS scores and RQLQ scores and the variation during the treatment period for all parameters between the groups were compared by the Mann-Whitney U-test. Results were expresed as mean and a P<0.05 was considered statistically significant.
RESULTS
Demographics and patient evaluation
The study population consisted of 24 male and 41 female patients. Mean age of the first group was 32.5 years (range, 18 to 55 years) and that of second group was 30.6 years (range, 17 to 61 years). In the pretreatment evaluation, there was no statistically significant differences between mean age, skin prick tests results, symptom scores, RQLQ scores, and VAS scores of the two groups. There was also no difference in compliance for the medication of each group. At first month and third month after treatment, the symptom scores, VAS scores and RQLQ scores were compared within each group and between the two groups.
Symptoms scores
For nasal obstruction, sneezing, rhinorea, and nasal itching; statistically significant improvement was found after the treatments at both 1st and 3rd month evaluations for each group when compared with pretreatment scores (for each symptoms P<0.05). The mean of symptom values increased at 3rd month when compared with 1st month. Statistically significant difference was found between 1st and 3rd month within the groups (P<0.05). When the two groups were compared for nasal symptoms; the scores of the second group were better than the first group at both 1st and 3rd months (for each symptoms P<0.05) (Table 1).
Table 1.
Mean values of symptom scores before treatment and after treatment at both 1st and 3rd months for each groups and P-value between the groups and within the groups
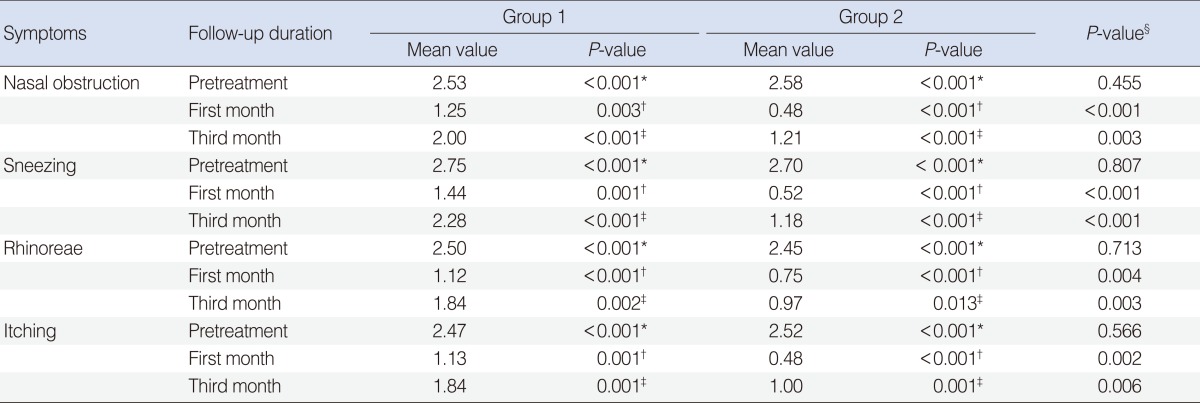
*P-value between pretreatment and 1st month within the group 1 and group 2. †P-value between pretreatment and 3rd month within the group 1 and group 2. ‡P-value between 1st and 3rd month within the group 1 and group 2. §P-values between the groups.
Rhinoconjunctivitis quality of life questionnaire
In each group, the RQLQ scores seven domains, namely: limited activity, sleep quality, non-nasal non-eye symptoms, practical problems, nasal symptoms, eye symptoms and emotional functions; such average results were statistically better after the treatment at 1st and 3rd month evaluations (for each domains P<0.05). The mean values of RQLQ scores increased at 3rd month when compared with 1st month. Statistically significant difference was found between 1st and 3rd month within the groups (P<0.05). When the two groups were compared at 1st and 3rd months; RQLQ average results for each seven domains were significantly better in the second group (for each domains P<0.05) (Table 2).
Table 2.
Mean values of rhinoconjunctivitis quality of life questionnaire (RQLQ) scores before treatment and after treatment at both 1st and 3rd months for each groups and P-value between the groups and within the groups
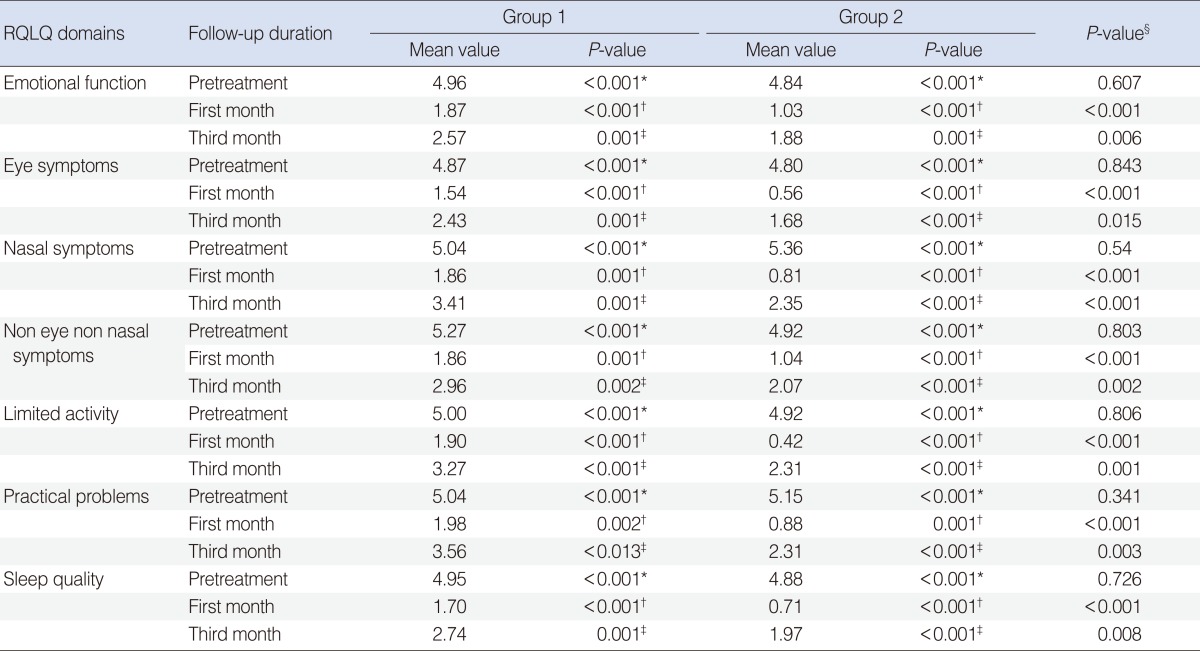
*P-value between pretreatment and 1st month within the group 1 and group 2. †P-value between pretreatment and 3rd month within the group 1 and group 2. ‡P-value between 1st and 3rd month within the group 1 and group 2. §P-values between the groups.
Visual analogue scale scores
A statistically significant improvement was determined for VAS after the treatment at both 1st and 3rd month evaluations in each groups (P<0.05). The mean values of VAS scores increased at 3rd month when compared with 1st month. Statistically significant difference was found between 1st and 3rd month within the groups (P<0.05). When VAS of the two groups were compared; the second group was significantly better than the first group at both 1st and 3rd months (P<0.05) (Table 3).
Table 3.
Mean values of visual analogue scale (VAS) scores before treatment and after treatment at both 1st and 3rd months for each groups and P-value between the groups and within the groups
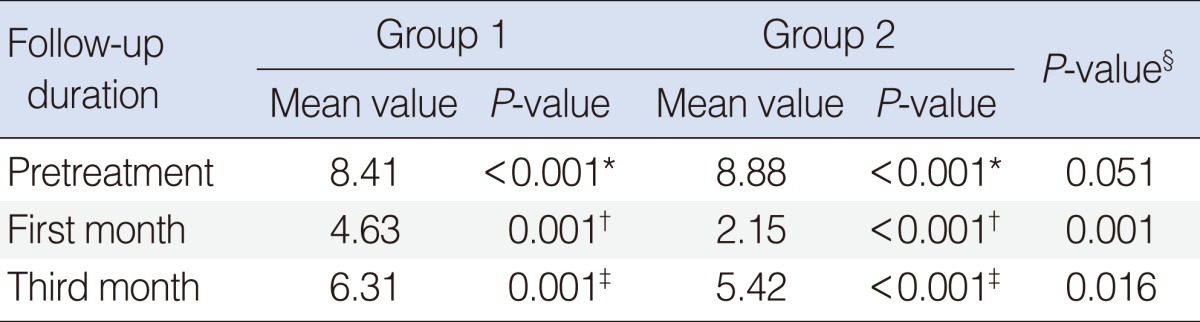
*P-value between pretreatment and 1st month within the group 1 and group 2. †P-value between pretreatment and 3rd month within the group 1 and group 2. ‡P-value between 1st and 3rd month within the group 1 and group 2. §P-values between the groups.
Side effects
Thirty four of patients had mild to moderate dryness of nasal mucosa during the therapy. Only one patient had anosmia problems which disappeared after one week.
DISCUSSION
Phototherapy is a new therapy method in the field of otolaryngology, and specifically a current issue in the management of allergic rhinitis. It has been used for the treatment of various inflammatory skin diseases for many years in dermatology. In the ancient times, the Romans, especially Galen and Celsus, understood the therapeutic benefits provided by the sun rays.
In the beginning of the twentieth century, Neils Finsen received the Nobel Prize by using the first artificial light sources for the treatment of lupus vulgaris. Today, light beam treatment, in terms of phototherapy, is being used for several medical indications with selected wavelengths and controlled dosages [14].
Having the beneficial effects of phototherapy on atopic dermatitis, the Hungarian researchers developed a device for intranasal phototherapy, based on the fact that atopic dermatitis and allergic rhinitis have similar pathophysiological pathways. They performed several researches to define the appropriate wavelengths and dosage. Eighteen patients with moderate to severe ragweed induced allergic rhinitis who were resistant to conventional anti-allergic therapies were being tested in a controlled study with the efficacy of 308 nm Xenon chloride (XeCl) ultraviolet B (UVB) laser. The first group received low dose irradiation, two treatments were given weekly for two weeks. The second group received medium dose irradiation, four treatments were given weekly for two weeks. The minimal erytema dose of each patient was determined by irradiating the skin in the gluteal region, and this was used for tailoring the dosage and its increments. There was no improvement on nasal symptoms and total nasal score (TNS) for the first group, while significant improvements on sneezing, rhinorrhea, nasal blockage and TNS were achieved by the second group. Additionally, the effect of light on skin prick tests was observed and dose-dependent inhibition was seen in the study [10]. The same study group also investigated the effectiveness of topical 8-methoxypsoralen plus ultraviolet A (PUVA) light treatment in 17 patients with hayfever in another study. At the end of the four treatments, improvements of all nasal symptoms and TNS were being observed. They also showed that PUVA treatment of the skin significantly supressed the skin prick test responses [11].
Different wavelengths of the light have different penetrations on the tissues, accordingly this causes different effects on immune cells. Therefore, UVA, UVB, and visible lights are combined in phototherapy, with the expectation of additional biological effects. It is also possible to use smaller doses of light in mixed form when compared to single form. Studies were done to observe the mixed light effects on allergic rhinitis. The effect of different wavelengths, on the allergen-induced wheal formation in skin prick tests, was evaluated. It was found that combined low doses of UVB, UVA, and visible light, referred as mUltraviolet/visible, had a dose-dependent inhibitory effect on immediate hypersensitivity reactions of the skin. However, UVA and visible light alone had only a slight inhibitory effect [15]. Hence, a new phototherapeutic device was designed, which was able to apply mixed light intranasally (Rhinolight-mUV/vis, Szeged, Hungary). In an another randomized double-blinded controlled trial, the effects of combined UVA, UVB, and visible lights (mUV/vis) therapy were evaluated in 49 patients with a history of at least 2 years of moderate to severe ragweed-induced allergic rhinitis. In the study group, mixed light was applied to each nasal cavity 3 times/week for 3 weeks, whereas only low intensity of visible light was applied to the control group as placebo. The total nasal symptom scores were significantly better in mUV/vis group after the treatment, and no significant improvement was seen in the control group at the end of the treatment [12].
Using combined UVA, UVB, and visible lights (mUV/vis) in a controlled prospective study of 100 patients; RQLQ and total symptom scores were assessed. It was concluded that phototherapy was an effective method to improve the symptoms on the disease and the quality of life in allergic rhinitis patients [16]. In another study, the clinical efficacy of rhinophototherapy was compared to the antihistamine, fexofenadine hydrochloride. Of the 18 ragweed induced allergic rhinitis patients, 11 patients received intranasal irradiation with increasing doses of mUV/vis light for 2 weeks and seven patients received 120 mg fexofenadine hydrochloride once daily within the same period. Rhinophototherapy was significantly better than fexofenadine hydrochloride treatment, with respect to the reduction of individual symptom scores for rhinorrhea, nasal obstruction and total nasal scores [17].
In our controlled prospective study of persistant allergic rhinitis patients, we found that adding phototherapy to medical treatment, using combined UVA, UVB, and visible lights (mUV/vis), is beneficial. We evaluated the patients in detail by using all symptom scores, the RQLQ scores and VAS scores. This is the first English study which evaluates the effect of phototherapy on house dust mite allergen induced persistent allergic rhinitis patients. Previous reports concerned the effects of phototherapy on hayfever. In this study, we showed that adding phototherapy to medical therapy is more effective than medical therapy for persistent allergic rhinitis patients. Our study reflected results over 3 months. The permanent effect of phototherapy at third month was shown in our study however this effect decreased when compared with the first month. Therefore, long-term assessments are necessary but even such results lead to the mangement of persistent allergic rhinitis.
When we looked at the side effect profiles; dryness was seen in all the previous studies. We also observed dryness within half of our patients but this was not as severe as to stop the therapy. We observed only one temporary anosmia just after the treatment. This was probably due to the edema of the nasal mucosa which disappeared within one week. Besides such side effects, we have already known that UV light induces DNA damage and it can be potentially associate with carcinogenesis on high doses. The molecular response ofnasal mucosa to therapeutic exposure of broad-band UV radiation in patients undergoing intranasal phototherapy had been investigated, and it had demonstrated that UV-specific markers of photodamage 10 days after treatment were similar to the baseline. They suggested that the UV-induced DNA damages responsing to respiratory epithelium is very similar to that of the human epidermis; and such nasal mucosa has the ability to efficiently repair UVB-induced DNA damage [18]. It was also reported in another study that markers of DNA damages elevated immediately after phototherapy were not presented within several days of treatment [19].
The major goal of our study was to determine if there was an additive effect of phototherapy on medical treatments within persistent allergic rhinitis. With this prospective randomized clinical trial; we found that the rhinophototherapy plus medical therapy was better than purely medical therapy in patients with persistent and moderate/severe allergic rhinitis with respect to quality of life and symptoms improvement.
Footnotes
This study was presented at 29th European Academy of Allergy and Clinical Immunology Congress in London, UK 2010 as a poster presentation.
No potential conflict of interest relevant to this article was reported.
References
- 1.Oettgen HC, Geha RS. IgE in asthma and atopy: cellular and molecular connections. J Clin Invest. 1999 Oct;104(7):829–835. doi: 10.1172/JCI8205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Weber RW. Allergic rhinitis. Prim Care. 2008 Mar;35(1):1–10. doi: 10.1016/j.pop.2007.09.001. [DOI] [PubMed] [Google Scholar]
- 3.Kay AB. Allergy and allergic diseases: second of two parts. N Engl J Med. 2001 Jan;344(2):109–113. doi: 10.1056/NEJM200101113440206. [DOI] [PubMed] [Google Scholar]
- 4.Bousquet J, Khaltaev N, Cruz AA, Denburg J, Fokkens WJ, Togias A, et al. Allergic Rhinitis and its Impact on Asthma (ARIA) 2008 update (in collaboration with the World Health Organization, GA(2)LEN and AllerGen) Allergy. 2008 Apr;63(Suppl 86):8–160. doi: 10.1111/j.1398-9995.2007.01620.x. [DOI] [PubMed] [Google Scholar]
- 5.Krouse JH. Allergic rhinitis: current pharmacotherapy. Otolaryngol Clin North Am. 2008 Apr;41(2):347–358. doi: 10.1016/j.otc.2007.11.014. [DOI] [PubMed] [Google Scholar]
- 6.Ferguson BJ. Environmental controls of allergies. Otolaryngol Clin North Am. 2008 Apr;41(2):411–417. doi: 10.1016/j.otc.2007.11.006. [DOI] [PubMed] [Google Scholar]
- 7.Ahmad N, Zacharek MA. Allergic rhinitis and rhinosinusitis. Otolaryngol Clin North Am. 2008 Apr;41(2):267–281. doi: 10.1016/j.otc.2007.11.010. [DOI] [PubMed] [Google Scholar]
- 8.Calderon MA, Casale TB, Togias A, Bousquet J, Durham SR, Demoly P. Allergen-specific immunotherapy for respiratory allergies: from meta-analysis to registration and beyond. J Allergy Clin Immunol. 2011 Jan;127(1):30–38. doi: 10.1016/j.jaci.2010.08.024. [DOI] [PubMed] [Google Scholar]
- 9.Man LX. Complementary and alternative medicine for allergic rhinitis. Curr Opin Otolaryngol Head Neck Surg. 2009 Jun;17(3):226–231. doi: 10.1097/MOO.0b013e3283295791. [DOI] [PubMed] [Google Scholar]
- 10.Csoma Z, Koreck A, Ignacz F, Bor Z, Szabo G, Bodai L, et al. PUVA treatment of the nasal cavity improves the clinical symptoms of allergic rhinitis and inhibits the immediate-type hypersensitivity reaction in the skin. J Photochem Photobiol B. 2006 Apr;83(1):21–26. doi: 10.1016/j.jphotobiol.2005.11.009. [DOI] [PubMed] [Google Scholar]
- 11.Csoma Z, Ignacz F, Bor Z, Szabo G, Bodai L, Dobozy A, et al. Intranasal irradiation with the xenon chloride ultraviolet B laser improves allergic rhinitis. J Photochem Photobiol B. 2004 Sep;75(3):137–144. doi: 10.1016/j.jphotobiol.2004.05.001. [DOI] [PubMed] [Google Scholar]
- 12.Koreck AI, Csoma Z, Bodai L, Ignacz F, Kenderessy AS, Kadocsa E, et al. Rhinophototherapy: a new therapeutic tool for the management of allergic rhinitis. J Allergy Clin Immunol. 2005 Mar;115(3):541–547. doi: 10.1016/j.jaci.2004.11.005. [DOI] [PubMed] [Google Scholar]
- 13.Cingi C, Cakli H, Yaz A, Songu M, Bal C. Phototherapy for allergic rhinitis: a prospective, randomized, single-blind, placebo-controlled study. Ther Adv Respir Dis. 2010 Aug;4(4):209–213. doi: 10.1177/1753465810374610. [DOI] [PubMed] [Google Scholar]
- 14.Kemeny L, Koreck A. Ultraviolet light phototherapy for allergic rhinitis. J Photochem Photobiol B. 2007 Apr;87(1):58–65. doi: 10.1016/j.jphotobiol.2007.01.001. [DOI] [PubMed] [Google Scholar]
- 15.Koreck A, Csoma Z, Boros-Gyevi M, Ignacz F, Bodai L, Dobozy A, et al. Inhibition of immediate type hypersensitivity reaction by combined irradiation with ultraviolet and visible light. J Photochem Photobiol B. 2004 Dec;77(1-3):93–96. doi: 10.1016/j.jphotobiol.2004.08.008. [DOI] [PubMed] [Google Scholar]
- 16.Cingi C, Yaz A, Cakli H, Ozudogru E, Kecik C, Bal C. The effects of phototherapy on quality of life in allergic rhinitis cases. Eur Arch Otorhinolaryngol. 2009 Dec;266(12):1903–1908. doi: 10.1007/s00405-009-1048-y. [DOI] [PubMed] [Google Scholar]
- 17.Garaczi E, Boros-Gyevi M, Bella Z, Csoma Z, Kemeny L, Koreck A. Intranasal phototherapy is more effective than fexofenadine hydrochloride in the treatment of seasonal allergic rhinitis: results of a pilot study. Photochem Photobiol. 2011 Mar-Apr;87(2):474–477. doi: 10.1111/j.1751-1097.2010.00882.x. [DOI] [PubMed] [Google Scholar]
- 18.Mitchell D, Paniker L, Sanchez G, Bella Z, Garaczi E, Szell M, et al. Molecular response of nasal mucosa to therapeutic exposure to broad-band ultraviolet radiation. J Cell Mol Med. 2010 Jan;14(1-2):313–322. doi: 10.1111/j.1582-4934.2008.00442.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Koreck A, Szechenyi A, Morocz M, Cimpean A, Bella Z, Garaczi E, et al. Effects of intranasal phototherapy on nasal mucosa in patients with allergic rhinitis. J Photochem Photobiol B. 2007 Dec;89(2-3):163–169. doi: 10.1016/j.jphotobiol.2007.09.013. [DOI] [PubMed] [Google Scholar]


