Abstract
Introduction
While incretin-based therapies have been compared in clinical trials, data comparing their relative efficacy in clinical practice remain limited, particularly when prescribed according to clinical guidelines. This study assessed the clinical and cost-effectiveness of, and patient preference for, incretin-based therapies initiated according to the National Institute for Health and Clinical Excellence (NICE) recommendations in UK clinical practice.
Methods
In a retrospective chart audit, anonymized data were collected for patients receiving incretin-based therapy according to NICE recommendations in clinical practice in Wales, UK. Parameters assessed included glycated hemoglobin (HbA1c), weight, achievement of NICE treatment continuation criteria, adverse events, treatment discontinuation, and drug cost-effectiveness based on observed treatment effects. Treatment preference for a dipeptidyl peptidase-4 inhibitor (DPP-4i) or glucagon-like peptide-1 receptor agonist (GLP-1RA) was assessed prospectively.
Results
Patients (1,114) were followed-up for a median of 48 weeks (256 received liraglutide, 148 received exenatide twice daily, and 710 received a DPP-4i). Liraglutide reduced HbA1c significantly more versus exenatide or DPP-4i (both P < 0.05). Weight changes were similar for GLP-1RAs but significantly greater vs. DPP-4is (both P < 0.05). NICE treatment continuation criteria were met by 32% and 24% of liraglutide 1.2 mg- and exenatide-treated patients (≥1% HbA1c reduction, ≥3% weight loss), and 61% of DPP-4i-treated patients (≥0.5% HbA1c reduction). Life-years gained per patient were 0.12, 0.08, and 0.07, and costs per quality-adjusted life-year were £16,505, £16,648, and £20,661 for liraglutide, exenatide, and DPP-4is, respectively. More patients (62.5%) preferred the GLP-1RA profile, with these patients having higher baseline body mass index score and HbA1c values, and longer diabetes duration than those preferring the DPP-4i profile.
Conclusion
When prescribed according to NICE recommendations, incretin-based therapies are both clinically and cost-effective options, with liraglutide providing greatest HbA1c reductions. Greater body weight reductions occur with GLP-1RAs compared with DPP-4is. Patients with higher baseline HbA1c and longer diabetes duration prefer a GLP-1RA profile versus a DPP-4i.
Keywords: Clinical effectiveness, Cost-effectiveness, Incretin therapies, Routine clinical practice, Type 2 diabetes
Introduction
When metformin and lifestyle changes become insufficient in treating type 2 diabetes mellitus (T2DM), advancing treatment with traditional therapies (sulfonylureas [SUs], thiazolidinediones [TZDs], and insulin) can be complicated by weight gain and hypoglycemia [1]. In clinical trials, adding incretin-based therapies to existing oral therapy has been shown to improve glycemic control without weight gain and with low hypoglycemia incidence (especially when used without SUs) [2–6]. Head-to-head studies of up to 12 months’ duration suggest that glucagon-like peptide-1 receptor agonists (GLP-1RAs) have greater glycemic efficacy and result in significantly more weight loss compared with the dipeptidyl peptidase-4 inhibitor (DPP-4i) sitagliptin [7–10]. Furthermore, patient-reported data suggest a greater improvement in treatment satisfaction with liraglutide 1.8 mg versus sitagliptin; treatment satisfaction data were similar for liraglutide 1.2 mg versus sitagliptin [11].
The National Institute of Health and Clinical Excellence (NICE) recommendations for incretin-based therapies reflect their key benefits, endorsing use (in combination with one or two oral therapies) when hypoglycemia and/or weight gain are a particular concern [12–14]. In general, DPP-4is recommended earlier in the treatment pathway, with less stringent treatment continuation criteria compared with GLP-1RAs. While incretin-based therapies have been compared in clinical trials [7–10, 15, 16], Data comparing their relative efficacy in clinical practice remains limited, particularly when prescribed according to clinical guidelines.
With these issues in mind, using primary care data, a retrospective chart audit was conducted to compare the clinical and cost-effectiveness of liraglutide, exenatide twice daily (b.i.d.), and DPP-4is when initiated according to current NICE recommendations. Once-weekly exenatide was not included as it was unavailable for routine use at the time of this study. As NICE also advocates patient involvement in therapy choice and treatment goals [17], the audit was complemented by a prospective patient preference survey in patients considered appropriate for treatment intensification with incretin-based therapy. The survey’s aim was to compare preferences for GLP-1RAs with DPP-4is. Based on clinical trial data, it was hypothesized that liraglutide would provide greater glycated hemoglobin (HbA1c) efficacy compared with DPP-4is and exenatide. As GLP-1RA use can result in weight loss, we also hypothesized that patients with a greater baseline body mass index (BMI) would prefer a drug with a GLP-1RA profile.
Patients and Methods
Retrospective Survey, Patient Selection, Data Collection, and Analyses
Anonymized data were collected from 15 participating primary care centers in South Wales, UK, for patients with T2DM commencing treatment with a DPP-4i or GLP-1RA between May 2009 and November 2011 in accordance with current NICE recommendations [12, 13]. Data were collected at baseline and 3, 6, 9, and 12 months after incretin-based therapy initiation, and at audit end (November 2011). Extracted outcome data comprised HbA1c, weight, blood pressure, total cholesterol, and plasma triglycerides. Data on treatment discontinuation (including reasons for switching) and adverse events (AEs; including symptomatic hypoglycemia or severe hypoglycemia [requiring third-party assistance]) were also collected, where available.
Endpoints were calculated for the intent-to-treat population (patients receiving at least one dose of incretin-based therapy). Based on similar efficacy results for DPP-4is in clinical trials [18], patients receiving sitagliptin, saxagliptin, or vildagliptin were pooled into a DPP-4i treatment group. GLP-1RA use was divided into two groups—liraglutide (1.2 mg and 1.8 mg) and exenatide BID—due to significant differences in glycemic efficacy reported in a head-to-head clinical trial [15]. For baseline demographics, differences in the mean of continuous and categorical variables were compared using repeated analysis of variance (ANOVA). Changes from baseline to each time point were calculated for each group for HbA1c, weight, blood pressure, total cholesterol, and plasma triglyceride at 3, 6, 9, and 12 months, after checking residuals for normality. For patients previously receiving a DPP-4i, changes in HbA1c and weight from baseline were assessed following 12 months of liraglutide or exenatide treatment. Similarly, for patients previously receiving exenatide, the effect of 12-months liraglutide treatment was evaluated. No patients switched from liraglutide to exenatide.
The proportion of patients satisfying the NICE 6-month treatment continuation criteria [12, 13] for DPP-4is (≥0.5% HbA1c reduction) and triple-therapy GLP-1RA use (≥1% HbA1c reduction with ≥3% weight loss) was assessed. When used as dual therapy, liraglutide has different continuation criteria (≥1% HbA1c reduction) but, due to the small numbers of patients receiving this combination in this audit, for the endpoint analysis, the more stringent triple-therapy continuation criteria were applied. The proportion of patients achieving the composite endpoint ≥1% HbA1c reduction coupled with any weight loss was also analyzed. Comparisons between treatment groups were performed for the proportion of patients achieving the composite endpoint, frequency of treatment discontinuation, AEs, and hypoglycemia. Summary statistics were calculated for AEs and discontinuation, and changes in other blood glucose-lowering therapies.
All analyses were performed using SAS® version 9.1 (SAS Institute Inc., Cary, NC, US). P-values < 0.05 were deemed statistically significant. Statistical calculations were performed using Minitab® release 14.11 (Minitab Ltd, Coventry, UK).
Cost-Effectiveness
Based on observed treatment effects versus baseline, the UK Prospective Diabetes Study (UKPDS) 68 risk equations [19] were applied over a 20-year time horizon into the CORE diabetes model to independently calculate the cost-effectiveness of liraglutide, exenatide, and DPP-4is. This time horizon was chosen based on the mean patient age at therapy initiation and was thus considered to represent lifetime exposure. Cost per quality-adjusted life-year (QALY) for patients prescribed a DPP-4i was based on the annualized retail acquisition cost of the most commonly prescribed agent, sitagliptin (£433.57 per year) [20]. In addition, due to the different annual acquisition costs for the two liraglutide doses, cost calculations were based solely on patients receiving the 1.2 mg dose (£954.84 per year) [20] as the vast majority of patients were prescribed this dose. Standard acquisition costs were used for exenatide b.i.d. (£830.25 per year) [20].
Prospective Survey of Patient Preference
From August 4, 2011 to November 8, 2011, treatment preference was assessed in a separate group of patients judged by their primary care practitioner (PCP) to require therapy intensification and for whom incretin-based therapy was appropriate according to NICE recommendations. Patients were shown two medication “profiles” by their PCP: one representing a DPP-4i (sitagliptin), the other a GLP-1RA (liraglutide) (Table 1). As the longest head-to-head study was between sitagliptin and liraglutide, data from that study were used for the patient preference questionnaire for route of administration, efficacy, side effects, and treatment satisfaction [7, 8, 11]. Informed consent was obtained and patients were asked which drug they would prefer to be prescribed in addition to their current medication if their blood sugar levels were too high. Subsequent responses were anonymized and results collated.
Table 1.
Medication profiles shown to patients
| DPP-4i profile (sitagliptin) | GLP-1RA profile (liraglutide) | |
|---|---|---|
| How do you take the medication? | Tablet, once a day | Injection, once a day |
| How effective is the medication? |
Results can vary from person to person but, generally, it should lower your long-term blood sugar level (HbA1c) by between 0.5% and 1% About 15% of people treated with this medication have achieved a long-term blood sugar level of less than 7% (53 mmol/mol) without any weight gain or hypoglycemia (blood sugar levels going much too low) |
Results can vary from person to person but, generally, it should lower your long-term blood sugar level (HbA1c) by between 1% and 1.5% Between 30% and 40% of people treated with this medication have achieved a long-term blood sugar level of less than 7% (53 mmol/mol) without any weight gain or hypoglycemia (blood sugar level going much too low) |
| Side effects | This medication has a low risk of hypoglycemia (blood sugar levels going much too low) unless you are also taking a sulfonylurea (for example gliclazide), where there might be a higher risk of you experiencing hypoglycemia |
This medication has a low risk of hypoglycemia (blood sugar levels going much too low) unless you are also taking a sulfonylurea (for example gliclazide), where there might be a higher risk of you experiencing hypoglycemia About 10–20% of patients who take this medication may have feelings of sickness and about 5–7% may actually be sick About 8–15% of patients taking this medication may suffer from diarrhea. These side-effects normally go away after about 1 month (individual results may vary) |
| Other effects | This medication has no effects on weight or blood pressure, and people who have been given this medication say that they are now more satisfied with their treatment | This medication may lead to a weight loss of about 7.5 lb, as well as a small reduction in blood pressure. People who have been given this medication say that they are now more satisfied with their treatment |
Patients were shown the two medication profiles and given the following instructions: “At the moment, your blood sugar levels are still too high and we will need to give you an additional treatment to take with your current medication to help lower your blood sugar levels. Written below are the descriptions of two different medicines that are often given to people in your situation, with type 2 diabetes, to help lower their blood sugar levels (note: neither one is insulin). Based on the descriptions below, please tick which one you would prefer to take in addition to your current treatments. You are free to change your mind, stop the treatment at any time, or have additional treatments if needed or advised by your doctor.”
DPP-4i dipeptidyl peptidase-4 inhibitor, GLP-1RA glucagon-like peptide-1 receptor agonist, HbA 1c glycated hemoglobin
As in a previous patient preference survey [21], after patients reported their preference, they were asked to rank the importance of the following reasons for their decision: administration method (oral or injection); blood glucose-lowering effect; side-effects (nausea, vomiting, and diarrhea); and other effects (weight loss and blood pressure decrease). Continuous variables were compared using a t test, categorical variables using a χ2 test, and overall patient preference was assessed by logistic regression, controlling for all demographic and patient characteristic variables. All analyses and statistical calculations were performed using SAS and Minitab, as for the retrospective survey.
Results
Retrospective Survey
Baseline Characteristics
In total, 1,114 patients had detailed baseline and follow-up data and were included in the retrospective audit: 256 received liraglutide (1.2 mg once daily (o.d.): 229; 1.8 mg o.d.: 27), 148 exenatide 10 μg b.i.d., and 710 a DPP-4i (sitagliptin 100 mg o.d., n = 425; vildagliptin 50 mg o.d. or b.i.d., n = 210; saxagliptin 5 mg o.d., n = 75). The median (range) follow-up for the audit group as a whole was 48 (0.4–119) weeks.
At baseline, patients initiated on liraglutide or exenatide therapy had significantly higher mean baseline HbA1c, durations of diabetes, and mean body weights compared with patients starting DPP-4is (Table 2). Furthermore, the majority (92%) of GLP-1RA use was in triple therapy, while over 15% of DPP-4i use was in dual combination with metformin. Additionally, a significantly greater proportion of patients starting with liraglutide were receiving a DPP-4i at baseline, compared with those starting with exenatide (21.1 vs. 6.8%; P < 0.05); DPP-4i therapy was discontinued in 97% and 98% of patients starting liraglutide and exenatide, respectively.
Table 2.
Baseline characteristics of patients receiving either liraglutide, exenatide, or a DPP-4i
| GLP-1RA | DPP-4i (n = 710) | P value | ||
|---|---|---|---|---|
| Liraglutide (n = 256) | Exenatide (n = 148) | |||
| Caucasian (%) | 92.1 | 93.6 | 89.4 | NS |
| Male (%) | 66.9 | 59.3 | 53.8 | NS |
| Age, years (±SD) | 63.5 (8.9) | 64.1 (9.5) | 59.5 (7.8) | NS |
| HbA1c (mmol/mol) | 81 | 84 | 65 | <0.05*,** |
| HbA1c [% (±SD)] | 9.6 (0.5) | 9.8 (0.8) | 8.1 (0.4) | |
| Recorded duration of diabetes [years (±SD)] | 11.5 (6.6) | 12.8 (8.2) | 6.9 (4.1) | <0.05*,** |
| Weight [kg (±SD)] | 109.7 (9.9) | 110.6 (10.7) | 88.9 (9.1) | <0.05*,** |
| BMI [kg/m2 (±SD)] | 39.5 (6.4) | 40.2 (8.6) | 31.1 (4.5) | <0.05*,** |
| Blood pressure [mmHg (±SD)] | 156/86 (11/6) | 160/88 (15/8) | 153/79 (10/6) | NS |
| Total cholesterol [mmol/L (±SD)] | 4.5 (0.4) | 4.1 (0.6) | 4.6 (0.7) | NS |
| Plasma triglycerides [mmol/L (±SD)] | 2.9 (1.4) | 2.8 (1.9) | 2.6 (1.8) | NS |
| Previous oral therapy | ||||
| Metformin monotherapy (%) | 5.5 | 2.7 | 15.8 | <0.05*,** |
| Metformin/SU combination therapy (%) | 79.5 | 78.9 | 60.1 | <0.05*,** |
| Metformin and TZD combination therapy (%) | 12.2 | 13.5 | 16.9 | NS |
| SU monotherapy (%) | 3.2 | 3.9 | 4.1 | NS |
| TZD monotherapy (%) | 2.6 | 3.7 | 3.1 | NS |
| Previous incretin-based therapy | ||||
| DPP-4i (%) | 21.1 | 6.8 | N/A | <0.05*** |
| Exenatide (%) | 23.5 | N/A | N/A | NC |
| Lipid-lowering therapy (%) | 91.6 | 93.4 | 91.9 | NS |
| Antihypertensive therapy (%) | 88.9 | 86.9 | 85.7 | NS |
Data are expressed as mean (SD), unless otherwise stated
No patients had previously been treated with liraglutide
* P < 0.05 liraglutide versus DPP-4i, ** P < 0.05 exenatide versus DPP-4i, *** P < 0.05 liraglutide versus exenatide
BMI body mass index, DPP-4i dipeptidyl peptidase-4 inhibitor, GLP-1RA glucagon-like peptide-1 receptor agonist, HbA 1c glycated hemoglobin, N/A not applicable, NS not significant, NC not calculated, SD standard deviation, SU sulfonylurea, TZD thiazolidinedione
Efficacy
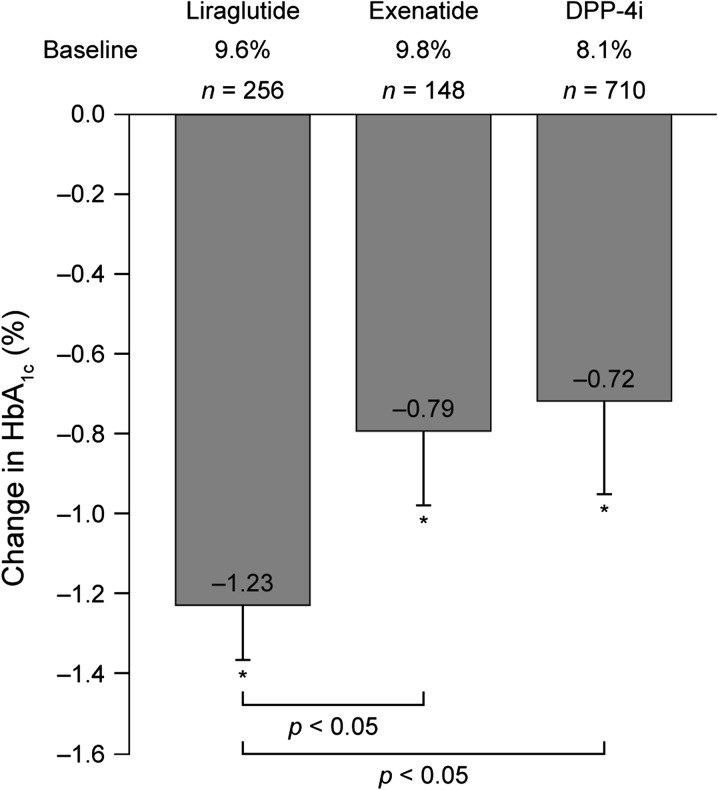
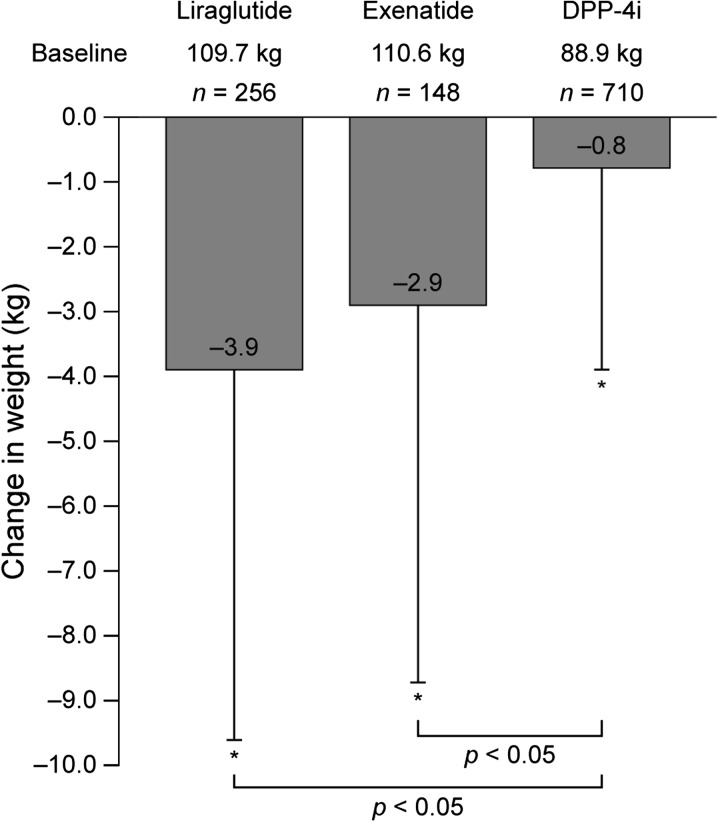
Significant reductions in HbA1c from baseline to audit end were apparent in all three treatment groups (all P < 0.05) (Fig. 1). The change in mean HbA1c was significantly greater for liraglutide (1.2 and 1.8 mg) than exenatide or DPP-4is (both P < 0.05), but not for exenatide versus DPP-4i (Fig. 1). Significant reductions in weight from baseline to audit end were observed for patients receiving a GLP-1RA (Fig. 2), with 3.1 and 2.1 kg greater weight reduction seen for liraglutide- and exenatide-treated subjects, respectively, versus those prescribed a DPP-4i. Mean HbA1c or weight at 12 months was not statistically different to the 3-, 6-, and 9-month measurements for each group (Table 3). Considering only those receiving liraglutide 1.8 mg (n = 27), the mean (standard deviation [SD]) HbA1c and body weight reductions from baseline were 1.28% (±0.35) and 4.1 kg (±7.2), respectively. Twelve liraglutide-treated subjects, 32 exenatide-treated subjects, and 25 DPP-4i-treated subjects either failed to complete 3 months of therapy or had no available follow-up data; tolerability issues were the most commonly recorded reason for therapy discontinuation over this time frame (n = 9 [liraglutide]; n = 27 [exenatide], and n = 9 [DPP-4i]).
Fig. 1.
Mean (SD) reduction in glycated hemoglobin (HbA1c) from baseline to end of audit. *P < 0.05 versus baseline. DPP-4i dipeptidyl peptidase-4 inhibitor, SD standard deviation
Fig. 2.
Mean (SD) reduction in weight from baseline to end of audit. *P < 0.05 versus baseline. DPP-4i dipeptidyl peptidase-4 inhibitor, SD standard deviation
Table 3.
Change from baseline in recorded parameters at 3, 6, 9, and 12 months, and at the end of audit
| Liraglutide (1.2 or 1.8 mg) | Time since initiation of incretin treatment (months) | ||||
|---|---|---|---|---|---|
| 3 | 6 | 9 | 12 | Audit enda | |
| n = 244 | n = 238 | n = 209 | n = 181 | n = 129 | |
| HbA1c [% (±SD)] | −1.29 (0.2)*,** | −1.21 (0.2)*,** | −1.19 (0.1)*,** | −1.15 (0.1)*,** | −1.22 (0.1)*,** |
| Body weight [kg (±SD)] | −4.4 (4.9)** | −2.9 (5.7) | −3.6 (5.8)** | −3.5 (6.1)** | −3.3 (5.9)** |
| Blood pressure [mmHg (±SD)] | −2.8/1.1 (5.5/4.2) | −2.4/0.9 (4.1/3.5) | −2.6/1.1 (4.1/4.2) | −2.2/1.1 (3.5/4.7) | −1.5/1.9 (5.5/3.9) |
| Total cholesterol [mmol/L (±SD)] | −0.3 (0.5) | −0.2 (0.4) | +0.1 (1.5) | −0.2 (0.3) | +0.1 (0.3) |
| Plasma triglycerides [mmol/L (±SD)] | −0.4 (0.6) | −0.5 (0.8) | −0.4 (0.9) | −0.2 (0.6) | −0.3 (0.8) |
| % Achieving NICE criteriab | 35 | 32 | 31 | 29 | 28 |
| Exenatide | Time since initiation of incretin treatment (months) | ||||
|---|---|---|---|---|---|
| 3 | 6 | 9 | 12 | Audit enda | |
| n = 116 | n = 101 | n = 96 | n = 92 | n = 66 | |
| HbA1c [% (±SD)] | −0.8 (0.19) | −0.72 (0.15) | −0.69 (0.36) | −0.75 (0.22) | −0.71 (0.31) |
| Body weight [kg (±SD)] | −3.1 (4.8) | −2.7 (5.7)*** | −2.9 (6.2)*** | −3.1 (6.9)*** | −2.5 (5.9)*** |
| Blood pressure [mmHg (±SD)] | −2.1/1.3 (4.4/2.5) | −1.5/2.1 (5.5/5.9) | −2.2/2.6 (4.8/3.9) | −1.9/1.7 (4.1/4.9) | −2.1/1.1 (4.4/3.7) |
| Total cholesterol, mmol/L (±SD) | −0.2 (0.2) | +0.2 (0.4) | −0.3 (0.2) | −0.1 (0.2) | +0.1 (0.3) |
| Plasma triglycerides, mmol/L (±SD) | −0.6 (0.6) | −0.5 (0.4) | −0.3 (0.7) | −0.3 (0.8) | −0.2 (0.8) |
| % Achieving NICE criteria | 27 | 24 | 26 | 25 | 21 |
| DPP-4i | Time since initiation of incretin treatment (months) | ||||
|---|---|---|---|---|---|
| 3 | 6 | 9 | 12 | Audit enda | |
| n = 685 | n = 551 | n = 471 | n = 301 | n = 266 | |
| HbA1c [% (±SD)] | −0.79 (0.21) | −0.69 (0.15) | −0.71 (0.14) | −0.74 (0.11) | −0.66 (0.19) |
| Body weight [kg (±SD)] | −0.9 (2.1) | −0.5 (1.9) | −1.1 (0.4) | −0.6 (0.9) | −0.7 (0.5) |
| Blood pressure [mmHg (±SD)] | +1.1/0.9 (3.5/2.9) | −1.3/1.7 (4.4/3.1) | +0.9/2.1 (5.5/3.7) | −1.5/1.1/(5.5/3.9) | −1.1/1.9 (4.5/3.9) |
| Total cholesterol [mmol/L (±SD)] | −0.1 (0.4) | −0.1 (0.5) | −0.3 (0.4) | −0.1 (0.6) | −0.2 (0.4) |
| Plasma triglycerides [mmol/L (±SD)] | −0.2 (0.2) | −0.4 (0.9) | −0.2 (0.4) | −0.3 (0.4) | −0.3 (0.3) |
| % Achieving NICE criteria | 59 | 61 | 52 | 54 | 57 |
Data are expressed as mean (±SD), unless otherwise stated
NICE continuation criteria for GLP-1RA therapy: ≥1% reduction in HbA1c and ≥3% body weight loss
NICE continuation criteria for DPP-4i therapy: ≥0.5% reduction in HbA1c
DPP-4i dipeptidyl peptidase-4 inhibitor, GLP-1RA glucagon-like peptide-1 receptor agonist, HbA 1c glycated hemoglobin, NICE National Institute for Health and Clinical Excellence, SD standard deviation
* P < 0.05 liraglutide versus exenatide; ** P < 0.05 liraglutide versus DPP-4i; *** P < 0.05 exenatide versus DPP-4i
aFor patients with 12-month data
bOnly for patients receiving liraglutide 1.2 mg
Patients previously treated with a DPP-4i switched to GLP-1RA following inadequate glucose reduction. In these patients, reductions in HbA1c and weight from baseline were apparent following 12-month liraglutide (1.2 mg or 1.8 mg) (n = 54) (−0.9 ± 0.6% and −2.5 ± 1.8 kg) or exenatide (n = 12) (−0.7% ± 0.9% and −2.3 kg ± 2.1 kg) treatment; the changes were statistically significant with liraglutide (both P < 0.05 vs. baseline) but not exenatide. For previous exenatide-treated patients, the most common reasons for conversion to liraglutide therapy were tolerability problems (62.6%) and insufficient HbA1c reduction (28.4%), with a mean (±SD) exposure to exenatide of 8.7 (±6.6) weeks. Following 12-month liraglutide treatment, significant HbA1c (−0.8% ± 0.3%) and weight (−2.1 kg ± 3.1 kg) reductions were observed (both P < 0.05).
The proportions of patients achieving the NICE 6-month treatment continuation criteria for GLP-1RAs with liraglutide 1.2 mg and exenatide were 32% and 24%, respectively. For DPP-4is, 61% of patients achieved the less stringent criteria at 6 months. The composite endpoint of ≥1% HbA1c reduction with any weight loss was achieved by 60%, 48%, and 14% of patients treated with liraglutide (1.2 mg and 1.8 mg), exenatide, or a DPP-4i, respectively.
Treatment Discontinuation and AEs
SU and TZD discontinuation was similar for both GLP-1RA- and DPP-4i-treated patients (liraglutide group: 6.9% and 7.9%; exenatide group: 8.6% and 10.9%; DPP-4i group; 7.2% and 12.1%). Insufficient HbA1c reduction was the most frequent reason for DPP-4i discontinuation (83%), while tolerability problems (22% and 42%) and insufficient HbA1c-lowering effects (27% and 29%) were the smost commonly recorded reasons for liraglutide and exenatide discontinuation, respectively.
AEs were more common in patients taking exenatide and liraglutide (39% and 29%, respectively) than DPP-4is (9.6%). The most commonly recorded AEs with liraglutide (26.5%) and exenatide (33.1%) were gastrointestinal (diarrhea, nausea, vomiting, abdominal pain, constipation, anorexia). The most commonly reported side effects with DPP-4is were diarrhea (3.9%), headache (2.1%), and nausea (1.7%). No major hypoglycemia was recorded; symptomatic hypoglycemia was recorded in 0.8%, 0.9%, and 0.8% of people taking liraglutide, exenatide, or a DPP-4i, respectively.
Cost-Effectiveness Analyses
Based on the end-of-audit observations, the calculated life-years gained per patient, compared with baseline, were 0.12, 0.08, and 0.07 for liraglutide, exenatide, and DPP-4i, respectively. The observed costs per QALY versus baseline for patients prescribed liraglutide, exenatide, or DPP-4i were £16,505, £16,648, and £20,661, respectively.
Prospective Survey of Patient Preference
A total of 188 patients completed the survey, with a mean (±SD) age of 63.9 years (±5.9), body weight 97.5 kg (±8.6), BMI 36.7 kg/m2 (±5.9), and HbA1c 74 mmol/mol (8.9%) (±1.1). Based on medication profiles provided, significantly more patients (62.5% vs. 37.5%) reported a preference for the drug with the GLP-1RA profile compared with the DPP-4i profile (P < 0.05). The demographics of patients choosing each drug are shown in Table 4. Weight loss was ranked the most important determinant of choice by 61% of patients choosing the GLP-1RA profile, and mode of administration by 66% of patients choosing the DPP-4i profile. Logistic regression analysis demonstrated that the likelihood of preferring the drug with the GLP-1RA profile grew with increasing BMI (odds ratio [OR] 1.54; 95% confidence interval [CI] 1.22–1.69), duration of diabetes (OR 1.32; 95% CI 1.12–1.99), and HbA1c level (OR 1.09; 95% CI 1.04–1.29).
Table 4.
Distribution and clinical profile of respondents to patient preference questionnaire
| DPP-4i profile (sitagliptin) | GLP-1RA profile (liraglutide) | P-value | |
|---|---|---|---|
| n [% (±SD)] | 70 (37.5) | 118 (62.5) | <0.05 |
| Age [years (±SD)] | 59.5 (5.1) | 62.6 (6.1) | N/A |
| Male/female (%) | 54/46 | 59/41 | NS |
| Body weight [kg (±SD)] | 88.9 (5.6) | 98.5 (6.9) | <0.05 |
| BMI [kg/m2 (±SD)] | 31.5 (5.5) | 37.8 (5.9) | <0.05 |
| HbA1c (mmol/mol) | 70 | 80 | <0.05 |
| HbA1c [% (±SD)] | 8.6 (0.5) | 9.5 (0.6) | N/A |
| Recorded duration of diabetes [years (±SD) | 6.5 (3.5) | 9.8 (3.1) | <0.05 |
| % On background monotherapy | 62.5 | 43.5 | <0.05 |
| % On background dual combination therapy | 37.5 | 56.5 | <0.05 |
Data are expressed as mean (±SD), unless otherwise stated
Comparisons made between people expressing a preference for drug B (GLP-1RA profile) versus drug A (DPP-4i profile)
BMI body mass index, DPP-4i dipeptidyl peptidase-4 inhibitor, GLP-1RA glucagon-like peptide-1 receptor agonist, HbA 1c glycated hemoglobin, N/A not applicable, SD standard deviation
Discussion
This retrospective UK case-note survey examined outcomes of therapy with GLP-1RAs (reported separately for liraglutide and exenatide) and DPP-4is (pooled for sitagliptin, vildagliptin, and saxagliptin) in routine practice. As treatments were initiated according to NICE recommendations [12, 13], patients prescribed GLP-1RAs had longer disease duration and higher baseline HbA1c and BMIs compared with patients prescribed DPP-4is. In this context, liraglutide provided a significantly greater mean reduction in HbA1c versus DPP-4is or exenatide; reduction in HbA1c was similar with exenatide and DPP-4is. Furthermore, in keeping with current NICE recommendations [13], the vast majority of liraglutide use was with 1.2 mg. Mean weight loss was greater with liraglutide compared with DPP-4is and exenatide, and was significantly greater with either GLP-1RA therapy compared with DPP-4is. A total of 32% and 24% of patients treated with liraglutide 1.2 mg and exenatide, respectively, met the 6-month NICE treatment continuation criteria for GLP-1RAs, while 61% of patients treated with a DPP-4i achieved their less stringent criteria [12, 13]. Based on input of the observed clinical effects of the different treatment options as applied of the UKPDS 68 risk equations into the widely accepted CORE diabetes model, liraglutide, exenatide, and DPP-4i therapy were cost-effective treatment options as prescribed at the currently accepted threshold of acceptability of £20,000 per QALY [12–14], although no direct comparison of the cost-effectiveness profile of these agents could be made from this study since baseline patient demographics were different, coupled with the absence of a randomized approach to therapy initiation. The majority of patients (62.5%) preferred the GLP-1RA profile, and these patients had greater BMIs, HbA1c, and durations of diabetes than patients preferring the DPP-4i.
While our observed relative efficacies of the incretin-based therapies are generally supported by head-to-head clinical trial data comparing liraglutide, exenatide, and sitagliptin [7, 8, 15], other factors may contribute to our observations. Baseline characteristics differed among treatment groups, with the DPP-4i group having lower HbA1c and BMIs than the GLP-1RA groups. Additionally, more patients in the liraglutide group than the other groups reduced or discontinued SU therapy, which may have contributed to greater absolute weight reduction observed in this cohort.
The relatively poor performance of liraglutide and exenatide in achieving the NICE treatment continuation criteria may reflect their later use in the disease course (baseline HbA1c 81–84 mmol/mol [9.6–9.8%], duration of diabetes 11.5–12.8 years) compared with the phase 3 studies (HbA1c 63–70 mmol/mol [7.9–8.6%], duration of diabetes 5–10 years) upon which the criteria are based [2, 22]. Achieving a 6-month 3% body weight loss may have been unrealistic for severely obese individuals in this audit (baseline BMI ~ 40 kg/m2 vs. 36 kg/m2 in phase 3 studies), requiring absolute weight loss beyond that observed in clinical trials [2, 22], particularly as these patients may represent a more treatment-resistant population. Therefore, the composite endpoint of ≥1% HbA1c reduction coupled with any weight loss may provide a better indication of incretin-based therapy efficacy in this setting. This endpoint was achieved by 60%, 48%, and 14% of patients treated with liraglutide (both 1.2 mg and 1.8 mg), exenatide, or a DPP-4i, respectively. Of note, no records of treatment discontinuation were identified as a consequence of NICE recommendations. Thus, although therapy may be initiated broadly in keeping with current NICE guidance, there appears to be poor adherence to therapy discontinuation rules in routine primary care.
Patients previously receiving exenatide achieved a 0.8% HbA1c reduction from baseline when switched to liraglutide, in excess of the 0.32% reduction from baseline seen in the clinical trial switching exenatide to liraglutide [23]. However, this may reflect suboptimal previous exenatide therapy, as the majority of these patients (62.6%) discontinued exenatide due to tolerability issues. Patients previously receiving DPP-4is demonstrated meaningful reductions in HbA1c and body weight from baseline when switched to exenatide or liraglutide. This likely reflects the higher GLP-1 receptor stimulation provided by GLP-1RA therapy compared with DPP-4is, and emphasizes the success of switching patients from a DPP-4i to a GLP-1RA [24, 25].
Despite widespread use of concomitant SU therapy, symptomatic hypoglycemia was reported by few patients (<1%). This may reflect underreporting by both patients and healthcare professionals and may also be related to the high baseline levels of glucose control. Gastrointestinal side effects were the most frequently reported AE in exenatide- (33.1%) and liraglutide-treated (26.5%) patients, in line with rates from clinical trials [22, 26]. However, therapy discontinuation due to gastrointestinal side effects was greater than seen in clinical trials [6–8, 15], possibly reflecting the impact of routine practice, as opposed to the clinical trial setting, which often includes highly motivated patients who undergo more monitoring than patients in routine clinical practice.
The health economic observations represent the cost-effectiveness profile of liraglutide, exenatide, and DPP-4is as prescribed in routine clinical practice, and thus may be more noteworthy than similar data derived from trials. However, as this analysis was limited to within-treatment group assessments compared with baseline, and as patients who were prescribed GLP-1RAs were markedly phenotypically different from those prescribed DPP-4is, it is impossible to directly compare the cost-effectiveness profiles of the different therapies.
The majority of patients surveyed preferred the GLP-1RA profile (62.5%) over the DPP-4i profile (37.5%); however, the phenotypic profile of the survey population may have been a source of potential bias with respect to the observed results. These data are at variance with a previous study [21], and may partly reflect the different patient populations included in each analysis; under a third of patients included in the previous survey had an HbA1c above their individual target at their last doctor’s visit. Weight loss was the most common reason for patients choosing the GLP-1RA profile, while mode of administration was important for those choosing the DPP-4i profile. These observations imply that, for patients with more advanced disease and higher baseline body weight, potential clinical effects, particularly relating to weight loss, may outweigh barriers presented by an injectable mode of administration. This is supported by treatment satisfaction data from the liraglutide versus sitagliptin phase 3 study [11]. For patients already close to their individual glycemic target, and for whom weight is not a particular concern, the ease of adding an orally administered DPP-4i to existing therapy may, however, be preferable.
While real-world observations such as these provide useful insight into the utility of different therapies in clinical practice, several limitations of the analysis should be considered. Selection bias, the uncontrolled nature of treatment changes, and the absence of strict research protocols and rigorous data capture are some of the inherent limitations. Additionally, the patient preference analysis did not include any validated measure of baseline health-utility state, representing another possibly confounding variable. Finally, for the economic analysis, the acquisition cost of sitagliptin was used for all patients prescribed a DPP-4i, which might affect interpretation of these data since there are small retail acquisition cost differences between the prescribed DPP-4is [20].
Conclusion
In summary, in this retrospective analysis of the clinical and cost-effectiveness of incretin-based therapies initiated according to NICE recommendations, liraglutide provided numerically greater reductions in HbA1c and body weight, compared with exenatide or DPP-4is, while liraglutide, exenatide, and DPP-4is appeared to represent cost-effective treatment options as prescribed. Patients with more advanced disease (higher baseline HbA1c and longer diabetes duration) and higher baseline BMIs appeared to prefer a drug with a GLP-1RA profile versus a DPP-4i. The observations from our analysis demonstrate the utility of liraglutide in routine clinical practice and suggest that clinical trial data appears to translate into therapeutic benefits in routine practice. Further research is, however, required in both clinical trials and routine practice, to evaluate the optimal positioning of the various incretin-based therapies in the T2DM treatment continuum.
Acknowledgments
The authors are grateful to Alison Clarke of University Hospital Llandough, Llandough, UK, for assistance with data collection and Dr. David Harvey of Watermeadow Medical, Witney, UK, for writing and editorial assistance, funded by Novo Nordisk. Dr. Marc Evans is the guarantor for this article, and takes responsibility for the integrity of the work as a whole.
Conflict of interest
Dr. Marc Evans has received honoraria and research awards from Novo Nordisk, Sanofi-aventis, Merck Sharp & Dohme, Novartis, Eli Lilly and GlaxoSmithKline. The remaining authors have no conflicts of interest to declare.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.
References
- 1.Inzucchi SE, Bergenstal RM, Buse JB, et al. Management of hyperglycaemia in type 2 diabetes: a patient-centered approach. Position statement of the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD) Diabetologia. 2012;55:1577–1596. doi: 10.1007/s00125-012-2534-0. [DOI] [PubMed] [Google Scholar]
- 2.Amori RE, Lau J, Pittas G. Efficacy and safety of incretin therapy in type 2 diabetes. JAMA. 2007;298:194–206. doi: 10.1001/jama.298.2.194. [DOI] [PubMed] [Google Scholar]
- 3.Victoza® 6 mg/ml solution for injection in pre-filled pen (summary of product characteristics). Novo Nordisk Limited; 2012. http://www.medicines.org.uk/emc/medicine/21986/. Accessed 04 Oct 2012.
- 4.Byetta® 5 micrograms solution for injection, prefilled pen. Byetta 10 micrograms solution for injection, prefilled pen (summary of product characteristics). Eli Lilly and Company Limited; 2012. http://www.medicines.org.uk/EMC/medicine/19257/ Accessed 04 Oct 2012.
- 5.BYDUREON® 2 mg powder and solvent for prolonged-release suspension for injection (summary of product characteristics). Eli Lilly and Company Limited; 2011. http://www.medicines.org.uk/EMC/medicine/24665/. Accessed 04 Oct 2012.
- 6.Shyangdan DS, Royle P, Clar C, Sharma P, Waugh NR. Glucagon-like peptide analogues for type 2 diabetes mellitus. Cochrane Database Syst Rev. 2011;5:CD006423. [DOI] [PMC free article] [PubMed]
- 7.Pratley RE, Nauck M, Bailey T, for the 1860-LIRA-DPP-4 Study Group et al. Liraglutide versus sitagliptin for patients with type 2 diabetes who did not have adequate glycaemic control with metformin: a 26-week, randomised, parallel-group, open-label trial. Lancet. 2010;375:1447–1456. doi: 10.1016/S0140-6736(10)60307-8. [DOI] [PubMed] [Google Scholar]
- 8.Pratley R, Nauck M, Bailey T, 1860-LIRA-DPP-4 Study Group et al. One year of liraglutide treatment offers sustained and more effective glycaemic control and weight reduction compared with sitagliptin, both in combination with metformin, in patients with type 2 diabetes: a randomised, parallel-group, open-label trial. Int J Clin Pract. 2011;65:397–407. doi: 10.1111/j.1742-1241.2011.02656.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.DeFronzo RA, Okerson T, Viswanathan P, Guan X, Holcombe JH, MacConell L. Effects of exenatide versus sitagliptin on postprandial glucose, insulin and glucagon secretion, gastric emptying, and caloric intake: a randomized, cross-over study. Curr Med Res Opin. 2008;24:2943–2952. doi: 10.1185/03007990802418851. [DOI] [PubMed] [Google Scholar]
- 10.Berg JK, Shenouda SK, Heilmann CR, Gray AL, Holcombe JH. Effects of exenatide twice daily versus sitagliptin on 24-h glucose, glucoregulatory and hormonal measures: a randomized, double-blind, crossover study. Diabetes Obes Metab. 2011;13:982–989. doi: 10.1111/j.1463-1326.2011.01428.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Davies M, Pratley R, Hammer M, Thomsen AB, Cuddihy R. Liraglutide improves treatment satisfaction in people with Type 2 diabetes compared with sitagliptin, each as an add on to metformin. Diabet Med. 2011;28:333–337. doi: 10.1111/j.1464-5491.2010.03074.x. [DOI] [PubMed] [Google Scholar]
- 12.NICE: Liraglutide for the treatment of type 2 diabetes. 2010. http://www.nice.org.uk/nicemedia/live/13248/51259/51259.pdf. Accessed 14 Jun 2012.
- 13.NICE. The management of type 2 diabetes. Clinical guideline 87. 2009. http://www.nice.org.uk/nicemedia/pdf/CG87NICEGuideline.pdf. Accessed 14 Jun 2012.
- 14.NICE: Exenatide prolonged-release suspension for injection in combination with oral antidiabetic therapy for the treatment of type 2 diabetes. 2012. http://www.nice.org.uk/nicemedia/live/13670/58205/58205.pdf. Accessed 14 Jun 2012.
- 15.Buse JB, Rosenstock J, Sesti G, LEAD-6 Study Group et al. Liraglutide once a day versus exenatide twice a day for type 2 diabetes: a 26-week randomised, parallel-group, multinational, open-label trial (LEAD-6) Lancet. 2009;374:39–47. doi: 10.1016/S0140-6736(09)60659-0. [DOI] [PubMed] [Google Scholar]
- 16.Buse JB, Nauck MA, Forst T, et al. Efficacy and safety of exenatide once weekly versus liraglutide in subjects with type 2 diabetes (DURATION-6): a randomised, open-label study. Diabetologia. 2011;54(Suppl. 1):S38. Abstract A75. [DOI] [PubMed]
- 17.NICE: Diabetes in adults quality standard. 2011. http://www.nice.org.uk/guidance/qualitystandards/diabetesinadults/diabetesinadultsqualitystandard.jsp. Accessed 14 Jun 2012.
- 18.Gerich J. DPP-4 inhibitors: what may be the clinical differentiators? Diabetes Res Clin Pract. 2010;90:131–140. doi: 10.1016/j.diabres.2010.07.006. [DOI] [PubMed] [Google Scholar]
- 19.Clarke PM, Gray AM, Briggs A, et al. A model to estimate the lifetime health outcomes of patients with Type 2 diabetes: the United Kingdom Prospective Diabetes Study (UKPDS) Outcomes Model (UKPDS no. 68) Diabetologia. 2004;47:1747–1759. doi: 10.1007/s00125-004-1527-z. [DOI] [PubMed] [Google Scholar]
- 20.MIMS: http://www.MIMS.co.uk. Accessed 12 Nov 2012.
- 21.Dibonaventura MD, Wagner JS, Girman CJ, et al. Multinational Internet-based survey of patient preference for newer oral or injectable Type 2 diabetes medication. Patient Prefer Adherence. 2010;4:397–406. doi: 10.2147/PPA.S14477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Davies MJ, Kela R, Khunti K. Liraglutide: overview of the preclinical and clinical data and its role in the treatment of type 2 diabetes. Diabetes Obes Metab. 2011;13:207–220. doi: 10.1111/j.1463-1326.2010.01330.x. [DOI] [PubMed] [Google Scholar]
- 23.Buse JB, Sesti G, Schmidt WE, Liraglutide Effect Action in Diabetes-6 Study Group et al. Switching to once-daily liraglutide from twice-daily exenatide further improves glycemic control in patients with type 2 diabetes using oral agents. Diabetes Care. 2010;33:1300–1303. doi: 10.2337/dc09-2260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Degn KB, Juhl CB, Sturis J, et al. One week’s treatment with the long-acting glucagon-like peptide 1 derivative liraglutide (NN2211) markedly improves 24-h glycemia and alpha- and beta-cell function and reduces endogenous glucose release in patients with type 2 diabetes. Diabetes. 2004;53:1187–1194. doi: 10.2337/diabetes.53.5.1187. [DOI] [PubMed] [Google Scholar]
- 25.Mari A, Sallas WM, He YL, et al. Vildagliptin, a dipeptidyl peptidase-IV inhibitor, improves model-assessed beta-cell function in patients with type 2 diabetes. J Clin Endocrinol Metab. 2005;90:4888–4894. doi: 10.1210/jc.2004-2460. [DOI] [PubMed] [Google Scholar]
- 26.Madsbad S. Exenatide and liraglutide: different approaches to develop GLP-1 receptor agonists (incretin mimetics)—preclinical and clinical results. Best Pract Res Clin Endocrinol Metab. 2009;23:463–477. doi: 10.1016/j.beem.2009.03.008. [DOI] [PubMed] [Google Scholar]