Abstract
Objective. To assess the evolution and effectiveness of the Academician Preparation Program to provide knowledge and skills in teaching and evaluating to pharmacy residents, as well as generate interest in academic careers.
Design. Participants attended seminars and participated in additional teaching, precepting, facilitating, and evaluating activities. Residents maintained a teaching portfolio and met with a faculty mentor quarterly to review their progress toward completion of the requirements for the Academician Preparation Program certificate.
Assessment. Since the program was first offered in 2005, it has expanded to 7 sites throughout the state. As of June 2012, 155 residents had completed the program and 20 (13%) had accepted full-time academic positions. Many others were serving as adjunct faculty members or preceptors. The majority of those enrolled in pharmacy residencies completed the program.
Conclusion. An optional, organized academic preparation program was of interest to residents, fostered academic careers, and helped meet residency accreditation guidelines.
Keywords: resident, teaching certificate, academic careers
INTRODUCTION
There has been unprecedented growth in the number of US colleges and schools of pharmacy, as well as in student enrollment over the last 10 years. This growth has led to a shortage of faculty members, particularly in departments of pharmacy practice whose responsibility is to deliver the experiential aspects of the curriculum to students. Colleges and schools of pharmacy rely heavily on practitioners to provide quality practice experiences to students, and in some cases, to deliver lectures. Residents are likely candidates to fulfill these teaching/precepting roles after they finish their training programs.
In recognition of the demand for residency-trained individuals to educate pharmacy students and other healthcare professionals, as well as patients, the American College of Clinical Pharmacy has developed a Teaching and Learning Certificate Program.1 Also, the American Society of Health-System Pharmacists has incorporated goals and objectives into residency training standards that address the provision of education and training by residents.2 In response, many colleges and schools of pharmacy have initiated teaching certificate programs or residency programs that emphasize teaching in order to foster an interest in teaching that will help meet their needs for preceptors and full-time faculty members in the future.3-9 In a 2010 survey of residency programs, 312 programs stated that they offered an opportunity for residents to participate in a formal teaching certificate program generally administrated through a nearby college or school of pharmacy.10 This paper describes the evolution of such a program over the last 7 years. The objective of this study was to determine whether the Academician Preparation Program has been successful in its mission to provide knowledge and skills in teaching and evaluating as well as generate interest in academic careers among pharmacy residents.
DESIGN
Teaching, evaluating, precepting, and research activities have been part of the Medical University of South Carolina (MUSC) residency training for over 20 years. Prior to creation of the program, all MUSC residents were required to give 2 presentations (a seminar accredited by the Accreditation Council for Pharmacy Education and an interactive teaching experience), prepare an abstract for presentation at a professional conference, and write a manuscript suitable for submission to a peer-reviewed journal. Residents were also asked to evaluate formal pharmacy student presentations and often helped precept student practice experiences.
A review of existing teaching certificate programs at other institutions confirmed that MUSC’s existing requirements were similar. Further, as we noted a decline in the number of residents who were pursuing academic positions, the college of pharmacy created its own certificate program in 2005.
Specific goals and objectives for the program are listed in Appendix 1. The program was first offered as an option to 2005-2006 MUSC residents. Requirements to obtain the certificate included attendance (80% attendance required) at additional seminar sessions (12 the first year), development of a teaching portfolio, and participation in additional teaching/evaluating activities beyond what was already required in the MUSC residency program. An abstract and manuscript suitable for peer review was required by both the residency and the Academician Preparation Program. Each resident was assigned a full-time faculty mentor for the program. Residents met with their mentor quarterly to review their teaching portfolio to determine progress toward meeting program requirements. Mentors also evaluated residents’ lectures and small group teaching experiences. Residents maintained examples of lecture handouts and copies of evaluations that they had performed on students in their portfolio.
Based on its initial success, the program was expanded to include residents from the Veteran’s Medical Center in Charleston in the 2006-2007 academic year. In 2007-2008, the college of pharmacy used its distance technology capabilities to provide the seminar series to residents in 3 additional South Carolina cities (Columbia, Greenville, and Florence). In 2012, a new residency program in Spartanburg, SC, was established and their residents joined the Academician Preparation Program. Faculty members from the 3 campuses of the South Carolina College of Pharmacy (SCCP) served as mentors for the program.
At the initiation of the program, a check-off sheet that served as a table of contents and tracking for completion of required activities was developed for the portfolio. The following sections describe some of the specific areas in which additional changes took place since the program began.
Process for Assigning Mentors
In the first 4 years of the program, mentors were somewhat randomly assigned to residents. If there was a specialty postgraduate year 2 (PGY2) resident participating, they were often paired with a faculty mentor outside of their specialty area. The thought behind this approach was to expose the resident to an additional person with different ideas or suggestions for professional growth. Because mentors were asked to evaluate the residents who were facilitating small student group discussions, it became obvious that having a program mentor in the resident’s area of practice might be more convenient and valuable.
Beginning in 2009, the program administrator attempted to align faculty mentors within the area of interest expressed by the resident. For example, a resident doing a PGY2 residency in pediatrics would be paired with a faculty member with that expertise. Because most of the residents were completing general PGY1 residencies, they were paired with faculty members who had similar interests (critical care, ambulatory care, administration, etc)
Delivery of the Seminar Series
As the program expanded beyond Charleston, the delivery of the seminar series also required revision. Initially, twelve 1-hour seminar topics were identified for inclusion and presented once or twice a month from September through the beginning of May. Because the Veteran’s Medical Center in Charleston is within walking distance to the MUSC campus, it was easy for residents to incorporate a 4:00 pm seminar into their workday schedule.
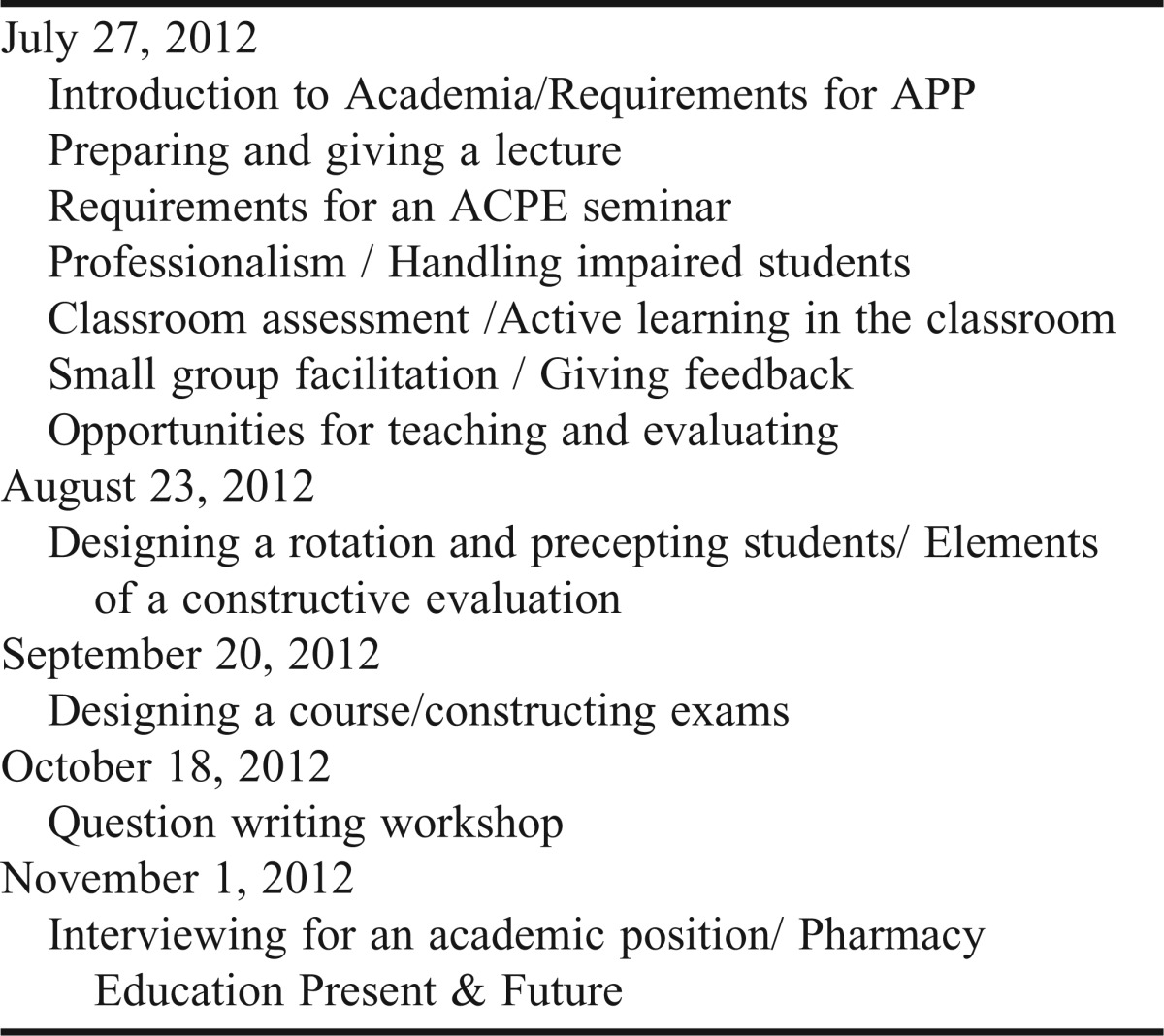
Once we expanded the seminar series to be offered via distance technology to residents in Columbia, travel time from the practice sites to the College of Pharmacy in Columbia became an issue because pharmacy practice sites were not close to the college campus. In addition, residents felt that they could have used some of the tips and strategies presented in the seminar series earlier in their residency programs. By working with residency program directors throughout the state, in 2009 we were able to identify a half-day in July when residents were asked to attend 5 hours of seminar sessions originating from Charleston and Columbia with the remaining 8 topics covered from August through November. The program administrator continued efforts in subsequent years to minimize the number of times residents had to leave their practice site. As of 2011, residents spent a full day in July attending seminar sessions and then completed 4 additional sessions lasting 90 minutes to 120 minutes over the subsequent 4 months. The entire series was completed by early November.
Some of the seminar topics were presented in traditional lecture format, while others were presented as panel discussions. The session on small group facilitation was a series of 5 simulations or skits where residents were shown a short video of actors portraying a number of different student behaviors that required a facilitator to intervene. Residents were asked to identify the behavior and discuss how they would approach the student.
Lectures
The number of lectures that participants in the Academician Preparation Program were required to deliver to students was reduced from 3 to 2 for several reasons. Because the majority of residents served as preceptors and not full-time faculty members the need to do more than 2 lectures seemed unnecessary. Also, in some courses, at one point nearly half the lectures were being given by residents, and students felt this was excessive and preferred that full-time faculty members deliver the lectures. In 2011, the College of Pharmacy department faculty began limiting the number of lectures in a course that could be given by residents.
For each lecture delivered, residents were asked to submit their learning objectives and test questions to the faculty preceptor and program director. These questions were then critiqued for clarity and formatting issues by 1 or more faculty members. Some of the questions submitted from the previous years were used as examples in a question-writing workshop, where residents critiqued and revised questions.
Small Group Facilitation
Although some residents enter academia after completing their residency and the certificate program, many more become adjunct faculty members and serve as preceptors. In either case, graduates of the program would be facilitating topic discussions among small groups of pharmacy practice experience students upon entering practice. Thus, over the years, the number of small group facilitation sessions that program participants were required to facilitate was increased from 3 to 5. From 2011 to 2012, the definition of what those experiences could entail was broadened to include teaching and/or evaluating non-lecture experiences. Residents were encouraged to help in hospital and community practice laboratories and patient simulation courses, in addition to facilitating small groups of practice experience students. Some residents served as tutors for students having difficulty with coursework. A faculty mentor evaluated each facilitation session performed by a resident.
EVALUATION AND ASSESSMENT
As of June 2012, 155 residents had completed the Academician Preparation Program and received a certificate from the South Carolina College of Pharmacy (Table 1). Of these, 20 (13%) accepted full-time academic positions within 2 years of finishing the program. Also, many former residents who entered practice serve as preceptors.
Table 1.
Enrollment and Completion Rates in the Academician Preparation Program
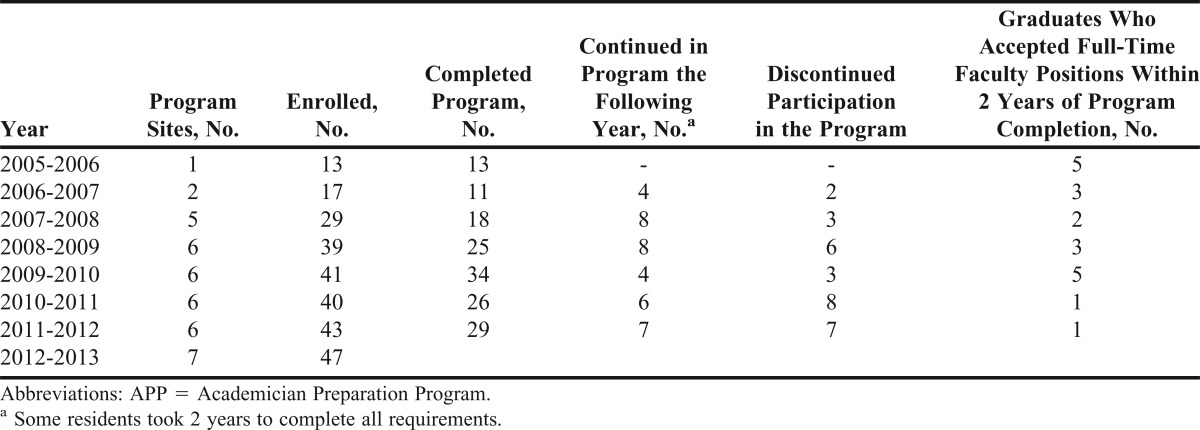
Thirty-one faculty members from the 3 campuses of the South Carolina College of Pharmacy served as mentors for the program in 2011-2012. For the 2012-2013 year, 47 residents were enrolled in the program, which was offered at 7 locations.
Each year since the program’s initiation, residents were asked to evaluate the seminars they attended and rate their overall achievement of program goals via an online survey instrument. The activities were rated on a 3-point scale: “useful/agree/true,” “partially useful/partially agree/partially true,” and “not useful/do not agree/false.” Space for open-ended comments and suggestions for improvement was provided. Table 2 and Table 3 show the last 3 years of results of the residents’ evaluation of the seminar series and overall program. For the seminar series, residents found the workshop on writing examination questions along with principles on constructing examinations the most useful (Table 4). They also ranked the workshops on preparing and giving a lecture, facilitation, precepting, and how to give feedback as very valuable. There was less interest in presentations on developing a course and developing a research concept. After completion of the entire program, the vast majority of residents felt that they could be effective role models when precepting pharmacy students and provide constructive feedback. In addition they gained confidence in teaching in a clinical setting and being able to facilitate small group discussions. Over half of the residents considered interviewing for an academic position.
Table 2.
Resident Evaluation of Seminar Topics Presented in the Academician Preparation Program, 2009-2011a
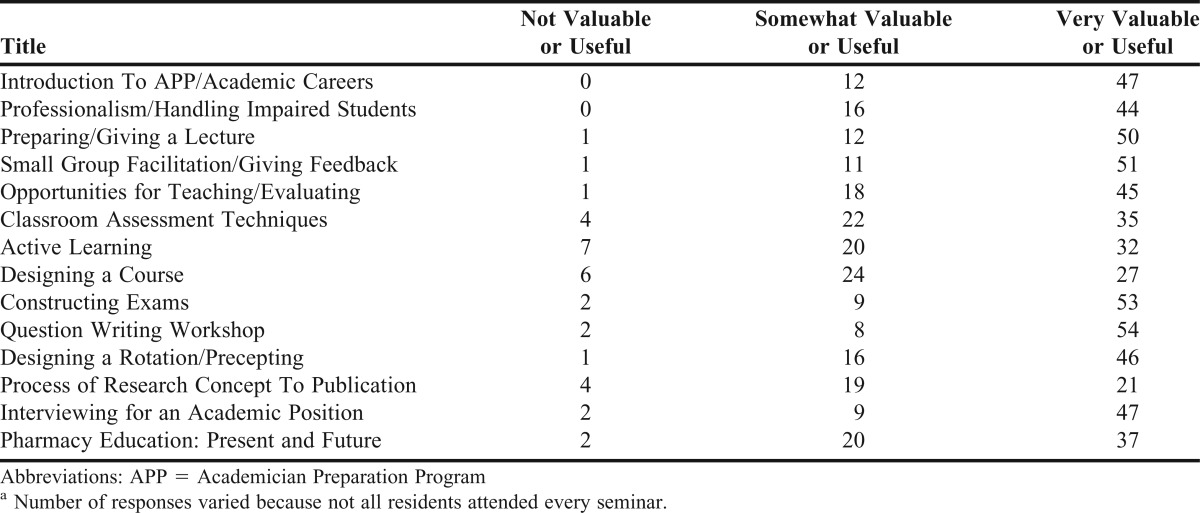
Table 3.
Exit Survey Responses of Graduates of the Academician Preparation Program, 2010- 2012a
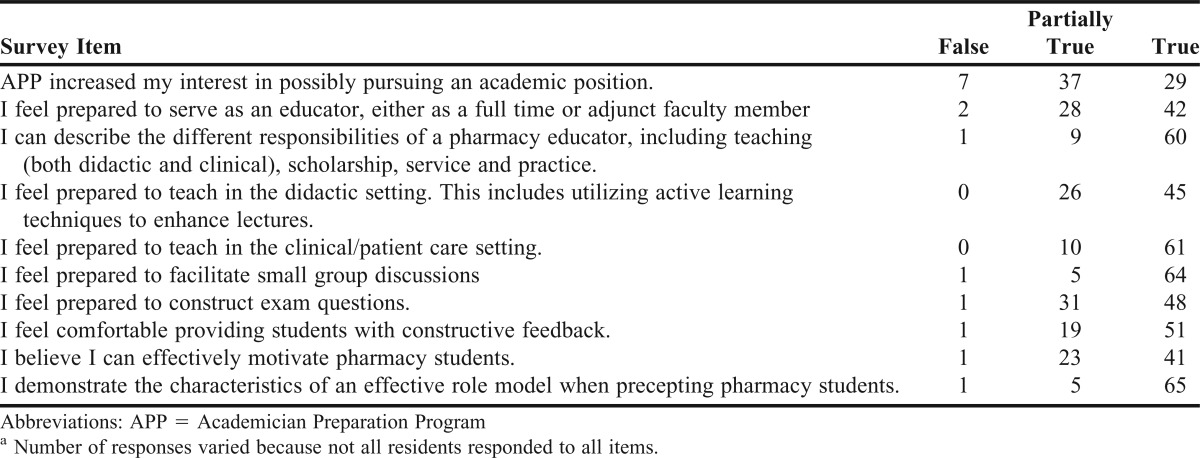
Table 4.
Academician Preparation Program Seminar Series
DISCUSSION
The Academician Preparation Program was initially intended to nurture those residents with a serious interest in entering academia. Completing the certificate program now has become the norm for all pharmacy residents in the state. Although this program is optional, because residency standards now include education and teaching goals, residency directors and residents see the Academician Preparation Program as one mechanism for meeting the ASHP accreditation standards. This could explain the high percentage (nearly 47%) of program participants who did not consider interviewing for a full-time faculty position. All residents are welcome to attend seminars and participate to whatever extent they choose, but they must complete all the requirements in order to receive a certificate of completion from the college.
Many of the changes described in the Design section, such as decreasing the number of lectures participants were required to give and increasing the number of small group facilitations, were made to the program based on feedback received from the annual survey. As the program has grown, it has become challenging to identify enough full-time faculty members to serve as mentors for residents Another challenge has been finding enough practice experiences where a resident can co-precept a student on 2 different occasions. Surprisingly, we have run into situations where preceptors are willing to work with a student or a resident but not both at the same time. This could be because of space limitations, but other reasons include the difficulty of trying to teach at 2 different levels or an increased amount of time needed to do evaluations of both a student and a resident.
One of the major goals of the program is to foster a serious interest in a full-time academic career; however, we have had limited success. There are numerous reasons why residents may choose a pharmacy career outside of academia. Many residents feel ill prepared, even at the end of a PGY2 program, for the rigors of an academic career. Some residents would rather hone their clinical skills for a few years before considering an academic career. Others may not be able for personal reasons to relocate to an area where a pharmacy college or school is located. Some of the residents enrolled in the Academician Preparation Program are doing residencies in institutions that are not academic medical centers and have more emphasis on patient care relative to teaching. Finally, salaries for academic positions still lag behind what the private sector can offer in many areas of the country.
Romanelli and colleagues have attempted to track the outcomes of the residents who have completed the University of Kentucky Teaching and Learning Certificate program through a survey instrument.4 As the Academician Preparation Program has expanded beyond the Medical University of South Carolina, the ability to track residents after completion of the program has been challenging. Our exit survey instruments (Table 3) suggest the majority of residents feel prepared to serve as preceptors and adjunct faculty members as the areas with the highest number of residents in full agreement with the outcome statements indicate comfort with activities associated with precepting. Residents feel less prepared in constructing examination questions, giving lectures that use active-learning methods, and motivating students.
CONCLUSIONS
An optional, comprehensive Academician Preparation Program was of interest to pharmacy residents, with more than 155 completing the program as of June 2012. Although the percentage of program graduates who have accepted full-time academic position has been small (13%), the program also prepares graduates who choose clinical practice and community pharmacy careers to serve as preceptors.
ACKNOWLEDGMENTS
The author would like to acknowledge the faculty mentors of the Department of Clinical Pharmacy and Outcome Sciences of the SCCP.
Appendix 1. South Carolina College of Pharmacy Academician Preparation Program 2005
The purpose of the South Carolina College of Pharmacy’s “Academician Preparation Program (APP)” is to prepare pharmacy residents to serve as educators, either in full-time or adjunct faculty positions.
Upon completion of the program, the resident should be able to:
-
Describe the responsibility of pharmacy educators
○ Describe different teaching environments
○ Define scholarship
○ Develop a teaching portfolio
○ Understand the differences among various types of faculty positions for practice, teaching, scholarship and service
-
Demonstrate use of varied teaching methods
○ Compare and contrast various teaching methods used in unique learning settings (for example, small group facilitation vs. large classroom didactic lecture)
○ Understand and, when appropriate, utilize principles of active learning
-
Evaluate student performance
○ Demonstrate skill in constructing exam questions
○ Provide constructive feedback for a defined learning experience
○ Demonstrate the characteristics of an effective role model when engaged in activities with pharmacy students
○ Employ effective preceptor strategies for motivating pharmacy students
Learning Activities
Each resident will be assigned a faculty mentor from the South Carolina College of Pharmacy (SCCP) to work with during the year. They will approve experiences used to fulfill learning activities and evaluate the residents’ progress.
-
Provide 3 contact hours of didactic lecture
○ At least one lecture should utilize active learning methods.
○ Lectures need to be completed either on the SCCP USC or MUSC campus. Mentors will evaluate the residents’ lectures.
-
○ Seminars completed at institutions as part of their residency requirement can account for one contact hour.
-
The resident will need to obtain approval from their mentor. In addition the resident will need to submit the following information:
Presentation Title
Date to be Given
Location
Audience (specify to whom this presentation will be given and ∼ number that will attend)
Final slide set
Final evaluation forms (copy of each form received)
Final mentor evaluation form (should include summation of all evaluations received)
All resident seminar presentations will be evaluated utilizing the same evaluation form. Mentors will evaluate the residents on the SCCP USC or MUSC campus during their seminars. If the resident is not on the USC or MUSC campus, a preceptor at that institution needs to agree to evaluate the resident.
-
-
Facilitate 3 small group discussions
-
○ These can be completed at the resident’s practice site; however, each experience used for small group facilitation need to be reviewed and approved by your mentor prior to performing. Examples of small group opportunities include but are not limited to: pharmacy student disease state discussions, pharmacy student patient case presentations, technician disease state or practice guideline presentations (ex. education for implementation of a practice guideline content and procedure), or pharmacist educational discussions. The resident should submit the teaching plan for approval prior to the activity. The plan should include the following information:
Discussion title
Participants
Key discussion concepts
Time required or allotted for this activity
Preparation required by facilitator
Evaluation tool to measure participants
Mentor responsible for oversight and evaluation of the resident
○ All small group facilitations will be evaluated utilizing the same evaluation form. Mentors will evaluate the residents performing small groups facilitations at the SCCP USC or MUSC campus. If residents choose to perform activity at their practice site, a preceptor must agree to evaluate.
○ There are many opportunities on the SCCP USC and MUSC campus.
-
-
Precept pharmacy students during at least one rotation
This experience needs to be reviewed and approved by your mentor prior to performing. A preceptor at the resident’s institution needs to agree to evaluate the resident on this experience.
-
Provide evaluation of pharmacy students
-
○ Evaluate pharmacy students on at least one rotation
This experience needs to be reviewed and approved by your mentor prior to performing. A preceptor at the resident’s institution needs to agree to evaluate the resident on this experience.
-
○ Evaluate at least 5 pharmacy student oral presentations (ex. Include but are not limited to: pharmacy student seminar presentations, clinical applications presentations, clinical assessment patient presentations)
This needs to be completed on the SCCP USC or MUSC campus.
-
-
Prepare a manuscript suitable for peer review and publication
○ Identification of the manuscript subject, journal to be submitted to, and potential authors needs to be reviewed and approved by your mentor prior to performing. The manuscript can be written with other preceptors; however, it will need to be included in your portfolio. Your mentor will review the finished product.
-
Prepare an abstract suitable for submission for a professional meeting on a local, state or national level
○ Identification of the abstract subject matter, related organization where the abstract will be submitted and potential authors needs to be reviewed and approved by your mentor prior to performing. The abstract can be written with other preceptors; however, it will need to be included in your portfolio. Your mentor will review the finished product.
-
Attend 80% of academic seminar series
○ Resident will need to attend the videostreamed seminar series at the SCCP USC or MUSC campus. There will be at least one to two seminars a month. We are trying to schedule a majority for Friday afternoons.
-
Prepare a teaching portfolio
○ This will contain all of your learning activities and evaluations. This will need to be turned into your mentor to review prior to completion of program.
REFERENCES
- 1.American College of Clinical Pharmacy. Teaching and learning certificate program. http://www.accp.com/academy/teachingAndLearning.aspx. Accessed September 28, 2012. [Google Scholar]
- 2.American Society of Health-System Pharmacists. Residency accreditation. http://www.ashp.org/accreditation-residency. Accessed September 10, 2012. [Google Scholar]
- 3.Romanelli F, Smith KM, Brandt BF. Certificate program in teaching for pharmacy residents. Am J Health-Syst Pharm. 2001;58:896–898. doi: 10.1093/ajhp/58.10.896. [DOI] [PubMed] [Google Scholar]
- 4.Romanelli F, Smith KM, Brandt BF. Teaching residents how to teach: a scholarship of teaching and learning certificate program (STLC) for pharmacy residents. Am J Pharm Educ. 2005;69(2):Article 20. [Google Scholar]
- 5.McNatty D, Cox CD, Seifert CF. Assessment of teaching experiences completed during accredited pharmacy residency programs. Am J Pharm Educ. 2007;71(5):Article 88. doi: 10.5688/aj710588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Castellani V, Haber SL, Ellis SC. Evaluation of a teaching certificate program for pharmacy residents. Am J Health-Syst Pharm. 2003;60(10):1037–1041. doi: 10.1093/ajhp/60.10.1037. [DOI] [PubMed] [Google Scholar]
- 7.Gettig JP, Sheehan AH. Perceived value of a pharmacy resident teaching certificate program. Am J Pharm Educ. 2008;72(5):Article 104. doi: 10.5688/aj7205104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Guillema S, Ly AV. A pharmacy practice residency (PGY1) with an emphasis on academia. Am J Pharm Educ. 2009;73(1):Article 13. [PMC free article] [PubMed] [Google Scholar]
- 9.Taylor JR, Scolaro KL, Williams JS. Development of a teaching certificate program utilizing distance education. Ann Pharmacother. 2006;40(6):1215. doi: 10.1345/aph.1H033. [DOI] [PubMed] [Google Scholar]
- 10.Aistrope DS, Attridge RT, Bickley AR, et al. Strategies for developing pharmacy residents as educators. Pharmacotherapy. 2011;31(5):65e–70e. [Google Scholar]


