Abstract
Objective. To implement and evaluate the use of a situated-learning experience to prepare second-year pharmacy students to conduct medication history interviews in preparation for introductory pharmacy practice experiences (IPPE) at ambulatory clinic sites.
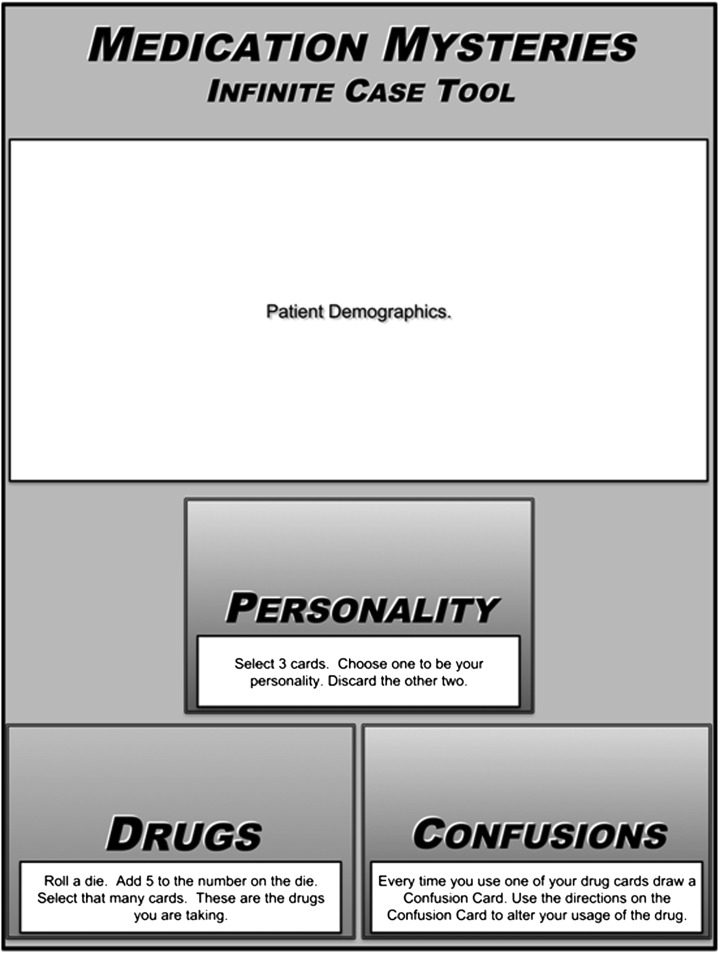
Design. Second-year doctor of pharmacy (PharmD) students (n=200) used the Medication Mysteries Infinite Case Tool, a game-like educational tool in which groups of 3 students assumed the roles of pharmacist, patient, and observer and rolled a die and drew cards to determine the drugs, patient personality, medication problems, and other variables that guided a medication history taking session.
Assessment. After the laboratory session, faculty members assessed students’ medication history-taking skills. One hundred sixteen (58%) and 78 (39%) of 200 students achieved excellence or competence, respectively, on the final assessment. Two weeks after the assessment, 53 of 200 (26.5%) students completed a survey instrument. The respondents indicated that their self-confidence in conducting medical history taking significantly improved following completion of the learning experience.
Conclusion. Using the Medication Mysteries Infinite Case Tool increased students’ confidence and skills in conducting medication history taking prior to their clinical IPPE experience.
Keywords: medication reconciliation, medication history, self-efficacy, introductory pharmacy practice experiences
INTRODUCTION
The 2012 Joint Commission cites the need to “maintain and communicate accurate patient information” as a National Patient Safety Goal in a variety of healthcare settings. The process of medication reconciliation is intended to identify and resolve discrepancies and involves comparing the medications a patient is taking (or should be taking) with those newly prescribed.1 The ability to perform a patient interview is identified by the Agency for Health Care Research and Quality as a key training component for the process of medication reconciliation.2 In various healthcare settings, pharmacist involvement in medication reconciliation has been shown to reduce preventable adverse drug events.3-5
Accreditation Council for Pharmacy Education (ACPE) standards for pharmacy education include conducting patient interviews to gather patient information as an important learning objective for introductory as well as advanced pharmacy practice experiences (IPPEs and APPEs). Education on the process of medication reconciliation during transitions of care is also suggested as content to include within the basic clinical sciences curriculum.6 A white paper from the American College of Clinical Pharmacy recommends that medication reconciliation and the performance of other activities related to care transitions be included in IPPEs as well as APPEs.7 Also, the importance of effective communication by pharmacists is emphasized by the ACPE as well as the American Association of Colleges of Pharmacy’s Center for Advancement of Pharmaceutical Education Educational Outcomes.6,8
In order to provide second-year PharmD students with unique opportunities to observe and conduct medication reconciliation, ambulatory clinic settings were added to the experiential component of IPPEs at the University of Florida in 2010. Students were assigned to these ambulatory clinic settings in groups of 4 to 5 students and expected to conduct medication history interviews and perform medication reconciliation under the supervision of the site preceptor. Initially, students were not provided any formal training on conducting medication history interviews or performing reconciliation. After a few semesters, faculty members began receiving feedback from site preceptors that many of the students had difficulties with effectively communicating with patients during interviews.
Faculty members realized that students needed opportunities to practice communication skills within a safe-learning environment before conducting medication history interviews in a real-world practice setting. Repeated practice of these skills within a safe-learning environment might improve students’ confidence in conducting an effective medication history interview. However, this would require the creation of a sufficient number of patient cases to expose students to new medication history-taking scenarios each time they practiced. Standardized patients are often used to portray unique cases; however, hiring standardized patients can be cost prohibitive for some institutions. Pharmacy students can serve as mock patients to role-play with one another; however, they are typically young and therefore have too little personal experience with taking prescription and nonprescription drugs to provide a medication history detailed enough to create a meaningful learning experience for the student conducting the interview.
To address the need for training students in conducting medication reconciliation as well as medication history interviews, the authors developed a 2-hour laboratory session using the Medication Mysteries Infinite Case Tool (MMICT), an educational tool with game-like features, to initiate various patient interview scenarios. When used properly, educational games build knowledge and skills, are enjoyable for the participants, and appeal to students’ competitive nature, which motivates them to play the game.9 The majority of studies describing educational health care games found that students enjoyed playing them.9-16 Games allow health care educators to create real-life scenarios without real-life consequences. The format of educational games creates a setting that decreases student stress and facilitates student learning.
The authors hypothesized that use of the MMICT and laboratory session would improve student’s self-efficacy to conduct medication history interviews. The purpose of this study was to evaluate the influence of the MMICT laboratory session on student’s self-efficacy to perform medication history interviews and medication reconciliation in an ambulatory clinical environment for IPPE in the second year.
DESIGN
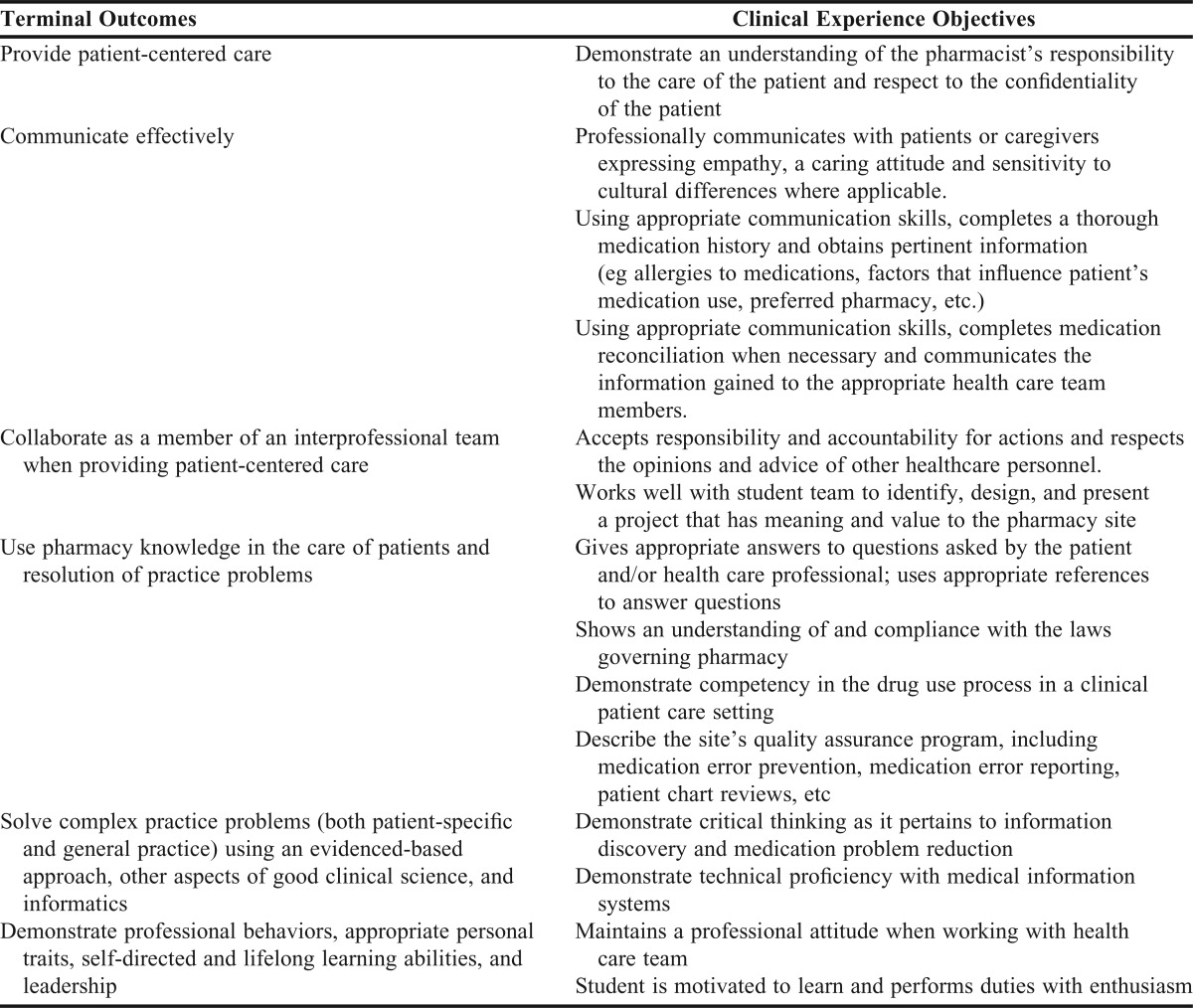
Second-year students at the University of Florida College of Pharmacy were required to enroll in IPPE III. Within IPPE III, students were assigned to a hospital practice experience or an ambulatory clinic practice experience (one experience was completed in the spring semester and the other in the fall semester). The terminal outcomes and experience objectives for IPPE III are presented in Table 1.
Table 1.
Course Mapping to Terminal Outcomes of Introductory Pharmacy Practice Experience and Clinical Practice Requirements for Second-Year Doctor of Pharmacy Students
During the first week of the semester in which they were assigned to the ambulatory clinic site, students first completed laboratory sessions. In preparation for these sessions, students were asked to view 1 hour of prerecorded lectures on medication histories, medication reconciliation, and a faculty demonstration of a medication history interview. The lectures addressed the importance of obtaining accurate medication histories, described the process of conducting a medication history interview and medication reconciliation, and discussed the role of pharmacists and pharmacy students in these processes.
Each laboratory session consisted of up to 24 students and at least 1 faculty facilitator. Rather than assigning standard cases for students to role-play with instructors to practice conducting medication history interviews, the authors created the Medication Mysteries Infinite Case Tool, which used game-like features to allow students to practice medical history taking in a fun, risk-free environment (all materials available upon request to authors).
The students were grouped into teams of 3 and each team was provided with the Medication Mysteries Infinite Case Tool packet. The packet contained a game board (Figure 1); decks of drug, confusion, and personality cards; a 6-sided die; instruction sheet; patient demographic sheets; and an evaluation rubric. The deck of drug cards contained 40 cards, each of which listed the proprietary name of a drug commonly used in the ambulatory care setting, as well as the drug’s generic name, strength, dosage, route of administration, and frequency. There were an equal number of confusion cards, half stating “no confusion with this drug” and half with various statements (called “confusers”) intended to add complexity to the exercise (eg, “I am not taking this drug because I am scared about the side effects” or “I take this medication but don’t remember how often I should take it”). To enhance role-playing and to vary the “patients,” the personality cards included short descriptors of 10 different personalities (eg, “I can’t hear very well” or “I go off on tangents”) and 6 wild cards. Patient demographic sheets were provided to allow the student playing the patient a place to record the patient name, age, gender, drug allergies, provider name, and pharmacy used. An evaluation rubric was provided to the student observing the interview to provide feedback on the “pharmacist’s” performance. It included a “yes” or “no” checklist for skills performed during the interview as well as examples of positive and negative feedback on interview performance. The students were encouraged to bring their laptop or mobile computing devices so they could refer to online drug information sources during the laboratory session.
Figure 1.
Medication Mysteries Infinite Case Tool Game Board.
At the beginning of the 2-hour laboratory session, the faculty facilitator stated the purpose of the session, introduced the MMICT, and reviewed the instructions. During the session, the facilitator monitored the students and answered any questions they asked. To play, each student assumed a role – patient, pharmacist, or evaluator. Prior to starting, the 3 decks of cards were placed on the corresponding sections of the board, the “patient” secured a patient demographic sheet, the “pharmacist” accessed any drug information sources he/she planned to use, and the “evaluator” reviewed the evaluation rubric. To start the round, the “patient” rolled the die, and drew the number of drug cards as dictated by the die (the number on the die plus 5), an equal number of confusion cards, and 3 personality cards. The “patient” chose 1 of the personality cards for his/her role and placed the other 2 cards at the bottom of the personality deck. The “patient” then filled out the demographic sheet based upon the personality and drug cards chosen and then placed the sheet face down. The “pharmacist” then began the interview. Each time the “pharmacist” asked about a medication, the “patient” used a corresponding confusion card to respond. Once the “pharmacist” had collected all of the information needed, the interview was over. The “evaluator” then shared the evaluation rubric that he/she had completed during the interview with the “pharmacist” and the team discussed the interview. After the first round was completed, subsequent rounds were played so that every student had the opportunity to play each role.
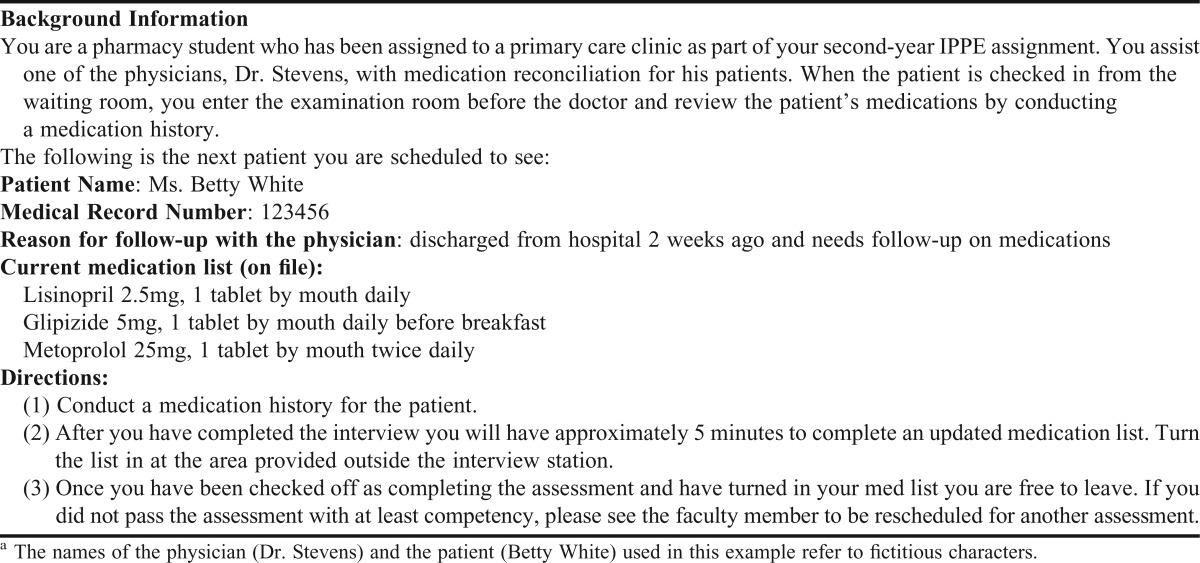
To demonstrate evidence of learning, students underwent individual assessments with a faculty member, teaching assistant, or resident acting as a mock patient beginning the day after the laboratory session. The assessments were conducted in small patient examination rooms. Students were scheduled every 20 minutes with the expectation that the medication history interview would last approximately 15 minutes, allowing the final 5 minutes for the faculty member to provide feedback to the student. Assessments took place over 3 days with a different patient case used each day to prevent students from sharing case information with students who had not completed the assessment (Table 2). Cases were designed with similar difficulty and number of medications to achieve standardization in the assessment. Students were allowed 15 minutes to review the patient scenario prior to entering the examination room. Students were also given a copy of the medication history form to document the patient’s demographic information, current medications (including name, strength, route of administration, frequency, and any comments on the use of the medication such as adverse effects, noncompliance, etc), allergies, and pharmacy information.
Table 2.
Example of a Standardized Patient Case Used for Individual Assessmenta
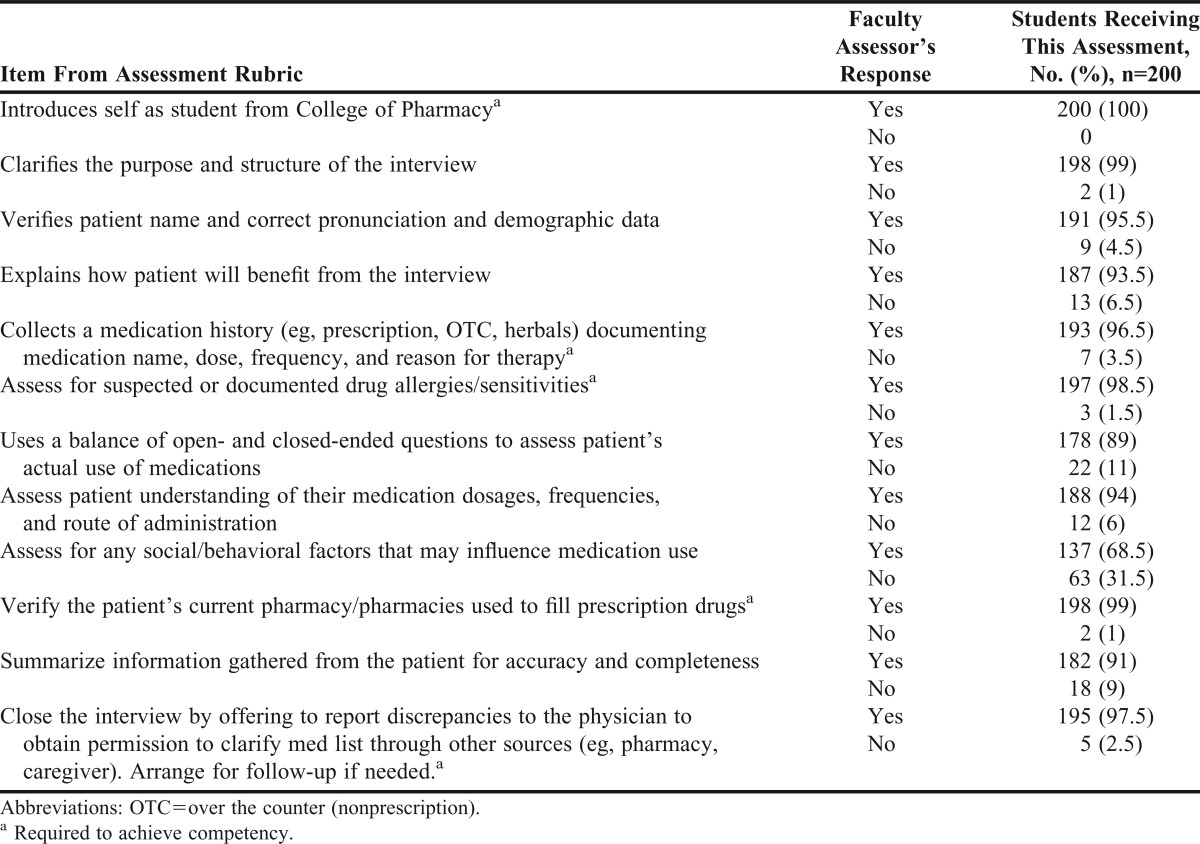
Assessors used a rubric with 12 criteria to evaluate students during the medication history interview (Table 3). Students were able to pass the assessment by earning a rating of “competence” or “excellence.” “Excellence” was demonstrated if all 12 criteria were satisfied. The student may have exhibited skills above the level required for assessment and demonstrated several behaviors that elicited positive feedback. “Competence” was demonstrated if all required criteria were satisfied. The student may have demonstrated some behaviors that elicited positive feedback with some areas noted for improvement. A “deficiency” rating was given if the student did not complete all required criteria and/or demonstrated behaviors that were inappropriate or distracting during the interview. A “deficiency” rating resulted in the student failing the assessment and required that the student be reevaluated within 1 week with a different assessor and case.
Table 3.
Individual Assessment of Pharmacy Students’ Performance in a Medication History-Taking Interview After Using the Medication Mysteries Infinite Case Tool
The second page of the rubric contained several positive (eg, strong introduction with good eye contact) and negative feedback (eg, mumbled or did not speak in a tone understandable by the patient) items that assessors could select based on the student’s performance during the interview. These were designed in a checkbox format to minimize extensive writing on the rubric as well as to provide examples of positive and negative feedback. After completion of the patient interview, students were allowed approximately 5 minutes to finalize their medication history form before turning it in for evaluation. Any students who received a “deficient” rating on their initial assessment were individually contacted via e-mail to arrange for a make-up time within 1 week of their original assessment. Feedback was given to the student in the e-mail about which areas of the assessment they did not perform well on and how they could improve.
EVALUATION AND ASSESSMENT
The University of Florida Institutional Review Board determined this study to be exempt from review. Data were collected for this study over a 1-year period (fall and spring semesters). The University of Florida College of Pharmacy is a distance-based 4-year PharmD program with 4 campuses (Gainesville, St. Petersburg, Orlando, and Jacksonville). Data were not available from the Orlando campus as students from that campus completed their IPPEs over the summer after this study was conducted.
Two weeks after the assessment, all students who participated in the laboratory session and completed the individual assessment were invited to complete a survey instrument via e-mail. The e-mail explained the voluntary nature of the survey as well as an estimate of the time it would take to complete it.
The survey instrument consisted of 50 items and was divided into 4 sections. The first section included 2 items asking students to identify their campus as well as the length of time they had worked as a pharmacy technician or intern. The second and third sections each included 17 items and asked students to reflect on their confidence to perform a patient interview and medication reconciliation prior to and following the MMICT laboratory session. Each assessment rubric item as well as key curricular objectives were translated into self-efficacy items.17 A retrospective pretest-posttest design was chosen for this survey instrument to minimize response-shift bias which can occur with traditional pretest-posttest survey design.18 Responses for sections 2 and 3 were gauged using a 6-point Likert scale (very unconfident to very confident). The fourth section included 15 items that measured student’s perceptions of the effectiveness of the preparatory materials, the MMICT, and the individual assessments. Reponses for section 4 were rated using a 5-point Likert scale (strongly disagree to strongly agree).
Student scores on the 17 matched pre-activity and post-activity survey questions were compared using the two-tailed matched pairs Wilcoxon signed-rank test. Based on the number of students who completed the survey instrument, an effect size of 0.72 with 80% power and an alpha level of 5% was detected. Differences were considered significant if p was less than 0.05.
Overall, 200 students on 3 campuses completed the individual assessments following the laboratory session (Table 3). Fifty-eight percent achieved excellence and 39% achieved competence on the individual assessment. Only 3% were assessed as being deficient on their performance and were required to repeat the assessment. The most common reason for deficiency was failure to collect a complete medication history (eg, forgot to assess for nonprescription medications or herbal supplements). All students who were required to repeat the assessment passed with at least a rating of “competency” on their second attempt. Greater than 90% of students achieved 10 of 12 criteria. A majority of the students gave a strong introduction when greeting the patient and spoke clearly in a tone and volume understandable by the patient. A majority of students also used appropriate nonverbal communication skills and conducted the interview in an organized fashion.
One area with which students struggled was using a balance of open-and closed-ended questions to assess the patient’s actual use of medications. While a majority of students achieved this criterion (89%), it was a common area of negative feedback provided and did not meet the same level of achievement as some of the other criteria assessed. Another area in which many students needed improvement was in the assessment of social/behavioral factors that may influence medication use. Students were expected to assess for alcohol and tobacco use, as well as any dietary or social behavior that could impact medication therapy. Across all campuses, 68.5% of students achieved this criterion, which was the lowest level of achievement for any of the criteria on the rubric.
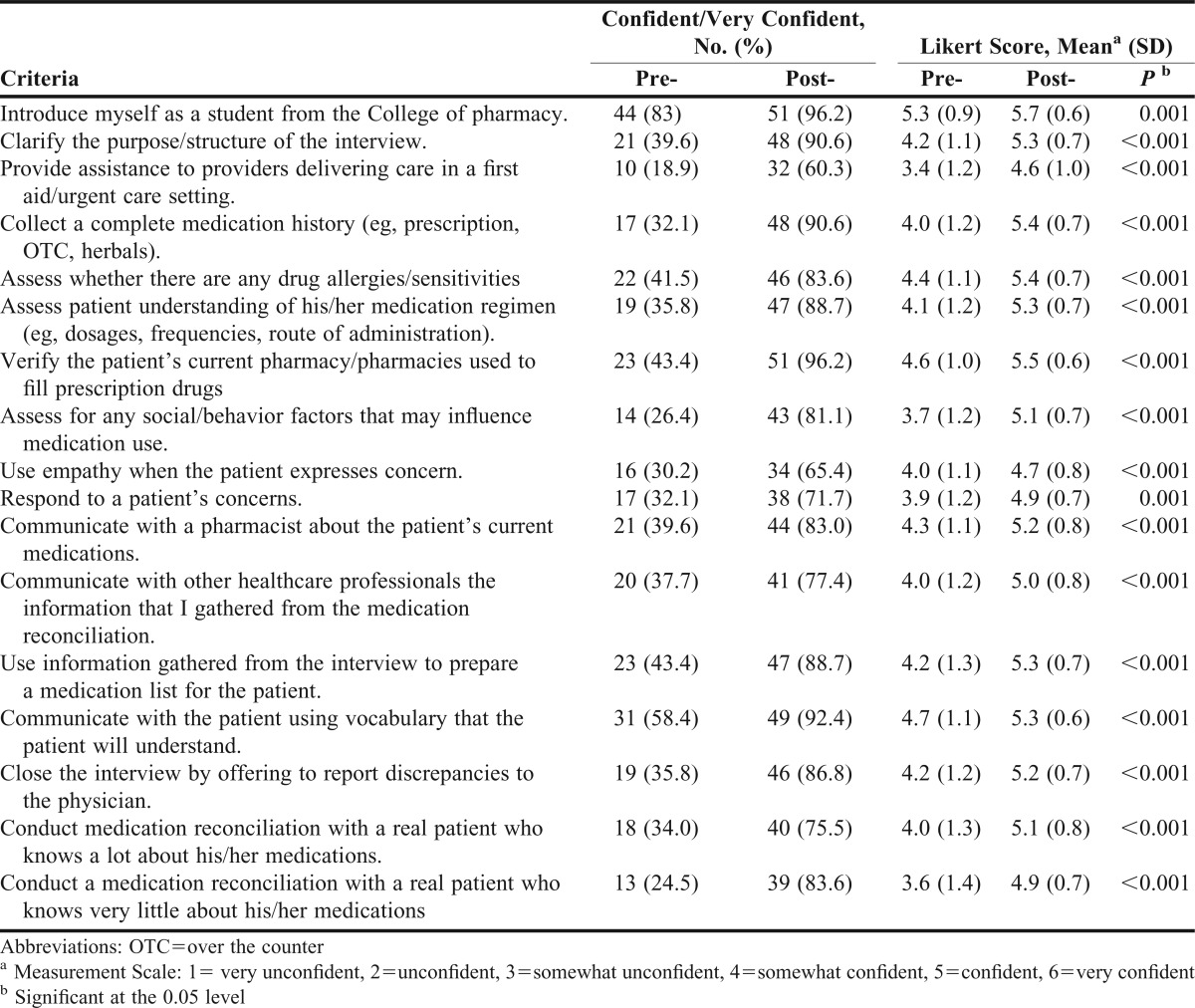
Fifty-three of 200 students (26.5% response rate) participated in the survey that was administered 2 weeks after the assessment. Sixty-four percent (n=34) of respondents were from the Gainesville campus, 22.6% (n=12) were from the Jacksonville campus, and 13.2% (n=7) were from the St. Petersburg campus. A majority of students (66%) had previously worked in a pharmacy as a technician or intern for 1 year or less. Few students (7.5%) had extensive pharmacy work experience (4 or more years). Students’ self-efficacy significantly improved after using the MMICT and completing the laboratory session (Table 4). A large majority of students felt the laboratory session was valuable (96.2%) and that the information and skills learned during the laboratory session could be applied to the real world (96.2%). A majority of students (>80%) also agreed or strongly agreed that the preparation materials viewed prior to the laboratory session were valuable. Overall, 86.8% agreed or strongly agreed that the MMICT was an excellent way to experience how to reconcile medication. A strong majority of students (94.3%) felt the laboratory session should be retained in the curriculum. All students surveyed agreed or strongly agreed that the individual assessments were fair. Nearly all students agreed or strongly agreed (98.1%) that the feedback provided by the faculty member at the end of the individual assessment was valuable and gave them insight on how to improve their medication history interview.
Table 4.
Changes in Pharmacy Students’ Self-Efficacy After Using the Medication Mysteries Infinite Case Tool and Completing the Laboratory Session (n=53)
In addition to the student survey, faculty members who participated in the laboratory session and individual assessment from each campus were asked to provide feedback via e-mail regarding how they felt about use of the MMICT, as well as the assessments. Overall, the feedback was positive. Faculty members observed that use of the MMICT was easily facilitated and well received by the students. Little direction from faculty members was needed during the laboratory session. Faculty members noticed students enjoying themselves and actively participating in each case scenario while using the MMICT.
Positive feedback was also elicited from several of the preceptors who supervised the students during their ambulatory clinic IPPEs. For example, a preceptor who had precepted students during the year prior to implementation of the MMICT and assessment session noted an improvement in the ability of students to conduct medication reconciliation. Preceptors submitted their level of satisfaction with students’ performance during the ambulatory clinic IPPEs, and this was factored into the students’ course grades. Areas of satisfaction evaluated included overall demonstration of competencies (Table 1), attendance, team interaction, and completion of a final project. Preceptor satisfaction was individually evaluated on a 5-point scale with “5” indicating the highest level of satisfaction with student performance. For the students assigned to clinical IPPE sites in the fall of 2011, the average preceptor satisfaction was 4.9 out of 5.
A brief survey instrument was also e-mailed to the preceptors who hosted IPPE students in their ambulatory care sites. A 5-point Likert scale (strongly disagree to strongly agree) was used to evaluate responses. The survey instrument consisted of 10 items and evaluated how the preceptors felt the students performed on the medication history-taking exercise, whether the students exhibited professional behaviors, and whether the students’ service provided value to the preceptor’s clinic site. With the exception of an individual preceptor, all responses from preceptors were positive (a score of 4 or 5) regarding the students’ performance and value to the preceptor’s clinic.
DISCUSSION
The use of educational games in pharmacy education is becoming more prevalent as instructors look to create innovative ways of delivering course material. Description of games used in pharmacy education are found in several curriculum areas including the basic clinical sciences, patient care electives, and APPEs.9-16The literature supports that students enjoy playing educational games; however, there is some debate about how much educational games improve student learning.10,15 To our knowledge, this study is the first to evaluate the use of a game-like tool for teaching medication history taking. In addition, this study demonstrated that the use of the MMICT enhanced student learning through individual assessment of key learning objectives.
While students performed well in the assessment overall, there were 2 areas in which students struggled. Using a balance of open- and closed-ended questions was a common area of negative feedback during the assessment. An explanation for this struggle is that students participating in this assessment had not yet completed Professional Communications in Pharmacy Practice, a 2-credit hour course in the spring semester of the second year. During this course, students practice communication skills including the use of open-and closed-ended questions during patient interviews. The lack of experience with this important communication skill may have led to a lower achievement of this criterion during the assessment. Another area of struggle was the low overall assessment of social and behavioral factors affecting medication use. A possible reason for this low achievement may have to do with the design of the medication history form. It was noted following the assessments that there was no spot on the form to record social or behavior factors such as alcohol or tobacco use. Not having this criteria “visible” on the medication history form may have caused students to forget this step in the interview process. Following this study, the form was updated to include a space to record social and behavioral factors.
One limitation of this study is the low survey response rate. Students were invited to complete the survey instrument via e-mail. Survey fatigue, which is becoming more prevalent in educational research including among students, may have contributed to the low response rate.19 Use of a paper-based survey administered after the laboratory session and individual assessment may have increased response rates. Another limitation of the study is that preceptor survey instruments were collected post-activity only. It may have been valuable to assess preceptor opinions on student performance prior to the training implementation. However, we did receive qualitative data and verbal feedback from preceptors expressing an improvement in student performance after use of the MMICT during the laboratory session.
This tool could easily be implemented at other institutions. This training exercise requires the following resources: the MMICT, adequate space with tables for students to work in groups of 3, supervisory personnel, and training for the supervisors in the use of the tool. An adequate number of copies of the items in the MMICT tool kit can be printed for an average-size class of students for less than $1,000. The toolkit would then be available for use in subsequent years with minimal maintenance (eg, replacement of lost cards or game pieces). The assessment portion of the case requires the following resources: standardized medication history cases, adequate space for the event (eg, small interview or examination rooms), supervisory personnel, and a training session for supervisors in how to perform the standardized case and conduct the assessment.
Furthermore, because of the simplicity of the tool and the style of training and assessment, this design could be adopted for other training purposes. For instance, this tool could be used for improving students’ communication skills, providing remediation for students who need more practice in medication history taking, or training other health professional students, or could be used as a group study aid outside of class. Additional decks of cards could be created for more advanced or specialized topics. We have also discussed the possibility of creating an electronic version of this tool. However, we feel the tactile aspect of using the MMICT (ie, selecting, holding, and reorganizing the cards; rolling the die) feels like playing a traditional board game and the familiarity of this interface may make players want to use this learning tool more than they would a computer software program. Throughout the training sessions, the students were highly engaged and were actually having fun practicing medication history taking, and we believe that was in part because of the game-like qualities of the activity.
SUMMARY
The Medication Mysteries Infinite Case Tool was well-received by our students, facilitators, and assessors. Pharmacy students gained confidence performing medication histories after completing the pre-instruction session (watching videos on medication history taking) and the laboratory session (using the case tool). Additionally, we received generally positive feedback from preceptors regarding the students’ performance in conducting medication histories at their ambulatory clinic sites. The Medication Mysteries Infinite Case Tool was a valuable addition to the pharmacy curriculum and helped students prepare for their clinical site IPPEs.
REFERENCES
- 1.The Joint Commission. 2012 national patient safety goals. http://www.jointcommission.org/standards_information/npsgs.aspx. Accessed November 15, 2012.
- 2.Gleason KM, Brake H, Agramonte V, Perfetti C. Medications at Transitions and Clinical Handoffs (MATCH) Toolkit for Medication Reconciliation. Rockville, MD: Agency for Healthcare Research and Quality; 2011. [Google Scholar]
- 3.Whittington J, Cohen H. OSFs healthcare’s journey in patient safety. Qual Manag Health Care. 2004;13(1):53–59. doi: 10.1097/00019514-200401000-00005. [DOI] [PubMed] [Google Scholar]
- 4.Pronovost P, Weast B, Schwarz M, et al. Medication reconciliation: a practical tool to reduce the risk of medication errors. J Crit Care. 2003;18(4):201–205. doi: 10.1016/j.jcrc.2003.10.001. [DOI] [PubMed] [Google Scholar]
- 5.Schnipper JL, Kirwin JL, Contugno MC, et al. Role of pharmacist counseling in preventing adverse drug events after hospitalization. Arch Intern Med. 2006;166(5):565–571. doi: 10.1001/archinte.166.5.565. [DOI] [PubMed] [Google Scholar]
- 6.Accreditation Council for Pharmacy Education. Accreditation standards and guidelines for the professional program in pharmacy leading to the doctor of pharmacy degree. https://www.acpe-accredit.org/pdf/FinalS2007Guidelines2.0.pdf. Accessed November 15, 2012.
- 7.Hume AL, Kirwin J, Bieber HL, et al. Improving care transitions: current practice and future opportunities for pharmacists. Pharmacotherapy. 2012;32(11):e326–e337. doi: 10.1002/phar.1215. [DOI] [PubMed] [Google Scholar]
- 8.American Association of Colleges of Pharmacy. Center for the Advancement of Pharmaceutical Education. Educational outcomes 2004. http://www.aacp.org/resources/education/Documents/CAPE2004.pdf. Accessed November 15, 2012.
- 9.Barclay SM, Jeffres MN, Bhakta R. Educational card games to teach pharmacotherapeutics in an advanced pharmacy practice experience. Am J Pharm Educ. 2011;75(2):Article 33. doi: 10.5688/ajpe75233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Persky AM. Stegall-ZanationJ, DupuisRE. Students perceptions of the incorporation of games into classroom instruction for basic and clinical pharmacokinetics. Am J Pharm Educ. 2007;71(2):Article 21. doi: 10.5688/aj710221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Roche VF, Alsharif NZ, Ogunbadeniyi AM. Reinforcing the relevance of chemistry to the practice of pharmacy through the Who wants to be a millionaire? learning game. Am J Pharm Educ. 2004;68(5):Article 116. [Google Scholar]
- 12.Kennedy DH, Fanning KD, Thornton PL. The age game: an interactive tool to supplement course material in a geriatrics elective. Am J Pharm Educ. 2004;68(5):Article 115. [Google Scholar]
- 13.Evans S, Lombardo M, Belgeri M, Fontane P. The geriatric medication game in pharmacy education. Am J Pharm Educ. 2005;69(3):Article 46. [Google Scholar]
- 14.Oliver CH, Hurd PD, Beavers M, Gibbs E, Goeckner B, Miller K. Experiential learning about the elderly: the geriatric medication game. Am J Pharm Educ. 1995;59(2):155–158. [Google Scholar]
- 15.Patel J. Using game format in small group classes for pharmacotherapeutics case studies. Am J Pharm Educ. 2008;72(1):Article 21. doi: 10.5688/aj720121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Shah S, Lynch LMJ, Macias-Moriarity LZ. Crossword puzzles as a tool to enhance learning about anti-ulcer agents. Am J Pharm Educ. 2010;74(7):Article 117. doi: 10.5688/aj7407117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Plaza CM, Draugalis JR, Retterer J, Herrier RN. Curricular evaluation using self-efficacy measurements. Am J Pharm Educ. 2002;66(1):51–54. [Google Scholar]
- 18.Nicholson T, Belcastro PA. Retrospective pretest-posttest analysis versus traditional pretest posttest analysis. Psychol Rep. 1985;57(2):525–526. [Google Scholar]
- 19.Lipka S. Want data? Ask students. Again and again. Chron High Educ. August 7, 2011. http://chronicle.com/article/Want-Data-Ask-Students-Again/128537/. Accessed January 21, 2013. [Google Scholar]