Abstract
Objective. To compare student accuracy in measuring normal and high blood pressures using a simulator arm.
Methods. In this prospective, single-blind, study involving third-year pharmacy students, simulator arms were programmed with prespecified normal and high blood pressures. Students measured preset normal and high diastolic and systolic blood pressure using a crossover design.
Results. One hundred sixteen students completed both blood pressure measurements. There was a significant difference between the accuracy of high systolic blood pressure (HSBP) measurement and normal systolic blood pressure (NSBP) measurement (mean HSBP difference 8.4 ± 10.9 mmHg vs NSBP 3.6 ± 6.4 mmHg; p<0.001). However, there was no difference between the accuracy of high diastolic blood pressure (HDBP) measurement and normal diastolic blood pressure (NDBP) measurement (mean HDBP difference 6.8 ± 9.6 mmHg vs. mean NDBP difference 4.6 ± 4.5 mmHg; p=0.089).
Conclusions. Pharmacy students may need additional instruction and experience with taking high blood pressure measurements to ensure they are able to accurately assess this important vital sign.
Keywords: assessment, simulation, blood pressure, pharmacy students, hypertension
INTRODUCTION
Cardiovascular disease remains the leading cause of mortality in the United States.1 Approximately 68 million Americans have hypertension, and the prevalence of this condition is increasing.2 In several published studies, pharmacists have been shown to improve care for patients with cardiovascular disease, notably patients with hypertension.3-7 In order to prepare students for clinical practice, colleges and schools of pharmacy are tasked with teaching about the management of hypertension as well as fostering the skill of blood pressure assessment.
One way of helping students to achieve this skill set is through patient simulation, a teaching approach that is being used by medical and nursing schools but has yet to be widely used by many colleges and schools of pharmacy. Additionally, the Accrediting Council for Pharmacy Education supports the use of active learning, such as simulation (Guideline 11.2).8
Although several reports of simulation in pharmacy education have been published, reports on the use of patient simulation are limited.9-13 Simulation-based learning was used to teach blood-pressure measurement to doctor of pharmacy (PharmD) students.14 The investigators assessed student knowledge and attitudes before and after they participated in classroom lectures and practical sessions using a high-fidelity computerized patient simulator and found significant improvement in clinical skills performance and knowledge of hypertension pharmacotherapy as well as high levels of satisfaction with this type of learning experience. However, accuracy of student blood-pressure measurements was not reported.
The aim of this study was to expand on this previous investigation. One of the challenges with traditional methods of blood pressure training programs is the inability to objectively verify the accuracy of each reading. Options include instructors taking a consecutive blood pressure after the student’s measurement or using training stethoscopes with dual headpieces. Patient simulation provides a precisely controlled environment wherein the simulator’s blood pressure reading can be adjusted and set to exact numbers. Prior to this study, pharmacy students have been assessing blood pressure measurements on healthy adults who are normotensive. Students do not gain much practice assessing either abnormally low or high blood pressure measurements before they enter their introductory or advanced pharmacy practice experiences (IPPEs or APPEs). The objective of this project was to compare student accuracy of only normal and high blood pressure measurements using a simulator arm.
METHODS
This study was designed as a prospective, single-blind, crossover study. Third-year pharmacy students who were enrolled in a required laboratory-based advanced pharmacy practice and skills course had the opportunity to participate in the study. All students were required to complete the activity as part of the course and were given credit for participation; however, students were not penalized for inaccurate blood pressure measurements. Participation in the study was voluntary, and students had the option to decide whether their data would be included. Informed consent was obtained, and the study was approved by the Drake University Institutional Review Board for the Protection of Human Subjects.
All students received the same baseline training in standard blood pressure assessment in an earlier part of the course series during their first and second years. Students were previously taught appropriate techniques for blood pressure measurement using the arm of a live subject (ie, a fellow student). They had been given opportunities to practice on their peers approximately 15 times in the previous 2 years and had been tested on their technique 4 times prior to the study. In this study, the students assessed blood pressure on simulator arms (Laerdal Medical Corporation, Stavanger, Norway), in which systolic and diastolic number, heart rate, and volume settings were preset using an external control panel.
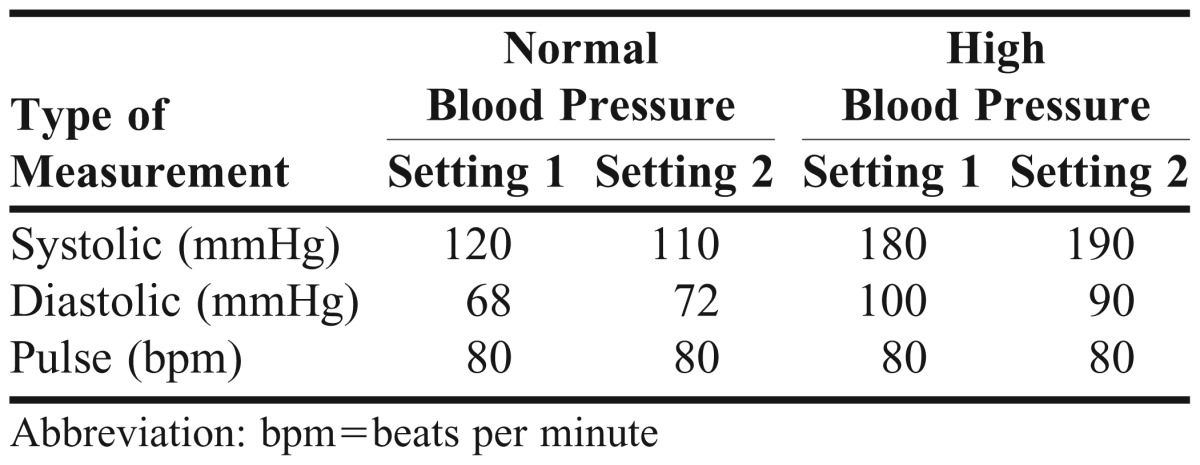
All study participants had the opportunity to practice taking blood pressure measurements with the simulator arms during a laboratory session a month before the study took place. Study investigators calibrated each simulator arm at the beginning of the day according to the manufacturer’s recommendations. To determine if the simulator arms were performing properly, the study investigators also verified that each simulator arm had accurate readings after it was calibrated as well as at random times throughout the data collection period. Students were randomly divided into 2 groups in each of the 5 laboratory sections. Group 1 was assigned a prespecified normal blood pressure measurement, and group 2 was assigned a prespecified elevated blood pressure (Table 1). Students were blinded to the group to which they were assigned. Investigators were not blinded and alternated randomly between 2 pre-specified blood pressure settings (setting 1 and setting 2) within the assigned group in an effort to minimize potential student communication about blood pressure settings. Volume was set to the highest setting. The faculty investigators, with the assistance of 4 fourth-year PharmD candidates, conducted the testing and managed data collection. The accuracy of both groups’ blood pressure readings was recorded by keeping track of the difference between the student-measured reading and the prespecified simulator arm setting. Additionally, the number of attempts needed to assess the blood pressure by the student was recorded. One week later, the students were asked to repeat the blood pressure readings. Students from group 1 were crossed over to the prespecified elevated blood pressure measurements, and students from group 2 were crossed over to the prespecified normal blood pressure readings.
Table 1.
Blood Pressure Configurations in a Study of Pharmacy Students’ Ability to Measure High and Normal Blood Pressure Using a Simulated Arm
The primary outcome was students’ accuracy in measuring blood pressure. Accuracy was assessed by determining the difference between the student-measured reading and the prespecified simulator arm setting. Blood pressure measurements obtained from students in group 1 were compared with those obtained from group 2. A secondary outcome included the number of attempts needed to assess the blood pressure. Statistical analysis was conducted using SPSS, version 19 (SPSS, Inc, Chicago, IL). All student data were de-identified. Basic descriptive statistics, including means and standard deviations, were calculated. Comparisons of continuous variables were carried out using Wilcoxon matched pairs signed-rank test. Pearson’s correlation was used to evaluate associations between the number of attempts and the accuracy of the blood pressure measurement. All significance tests were 2-sided and significance was set at p<0.05. The null hypothesis was that there would be no difference between groups 1 and 2 in the accuracy of blood pressure readings by pharmacy students.
RESULTS
One hundred twenty students (100% of class enrollment) in an advanced pharmacy practice and skills course consented to participate in the study. Although all students in the class agreed to participate in the study, data from only 116 students were included. Data from students who were unable to report 1 or more blood pressure measurements from the simulator arm (n=3) were excluded from analysis. Data were also excluded for 1 student who was erroneously assessed on normal blood pressure readings twice instead of being assessed on both normal and high blood pressure readings.
The mean high systolic blood pressure (HSBP) measurement difference was 8.4 ± 10.9 mmHg, and the mean normal systolic blood pressure (NSBP) measurement difference was 3.6 ± 6.4 mmHg. The mean high diastolic blood pressure (HDBP) measurement difference was 6.8 ± 9.6 mmHg, and the mean normal diastolic blood pressure (NDBP) measurement difference was 4.6 ± 4.5 mmHg. With respect to the number of attempts to assess the blood pressure, the mean for the high category was 1.9 ± 0.9, and the mean for the normal category was 1.8 ± 1.2. The distributions of the blood pressure measurements were tested for normality and did not pass; therefore, nonparametric tests were used. A Wilcoxon matched pairs signed-rank test was performed to examine the difference between the paired groups. There was a significant difference between the accuracy of the HSBP measurement compared with the NSBP measurement (p<0.001). However, there was not a significant difference in the accuracy of HDBP compared with that of the NDBP measurement (p=0.089). There was a significant correlation between the number of high and normal attempts (r=0.308; p=0.001), but there were no significant correlations between the number of attempts and the degree of inaccuracy of the blood pressure measurements.
DISCUSSION
Previous research has shown that using patient simulation as part of the pharmacy curriculum is an innovative strategy for promoting exposure to real-life situations in a nonthreatening environment. Faculty members are able to give students repetition in practicing skills and allow students to gain exposure to a variety of situations that may require unique approaches.10,13-15
Seybert and Barton studied simulation-based learning in pharmacy students by assessing accuracy of blood pressure measurement and student satisfaction.14 They found that student accuracy increased after each practice session, and there was agreement that patient simulation of blood pressure monitoring would increase student ability to perform a blood pressure assessment on a patient. However, this study did not specify the blood pressure ranges used to assess the students’ technique.
Another study used a crossover design to compare blood pressure measurements using a live subject and a simulator arm.15 Lee and colleagues found that students had more difficulty obtaining an accurate systolic blood pressure compared with an accurate diastolic blood pressure, a finding similar to that of the current study. In the Lee study, students were more likely to obtain an accurate systolic blood pressure on the simulator arm compared with the arm of a living subject. This finding differed from our study, which investigated measurements only on simulator arms. Lee and colleagues’ finding may be a result of students attempting to release the air valve at a steady rate while simultaneously listening for the first Korotkoff sound. Another potential error in measuring systolic blood pressure could be related to difficulty estimating the systolic pressure by radial pulse palpation. This finding is important because the magnitude of inaccurate HSBP measurements could potentially be even larger in a human patient than in the simulator arms used in our study. Although students in Lee’s study felt more confident regarding the accuracy of a blood pressure reading in a simulator arm (94.9%) than in a human arm (5.1%), they seemed to prefer learning how to check a blood pressure on a human arm (54.1%) compared with a simulator arm (45.9%). Our study did not measure student preferences, but this could be an area to explore in the future.
Our results showed that students who had difficulty accurately measuring HSBP also had difficulty measuring NSBP. There was a correlation between the number of blood pressure attempts in each group. This finding supports the need for further student practice sessions focused on determining the systolic pressure whether the blood pressure is abnormal or not. Simulator arms would be excellent tools to add practice sessions, considering that real patients or classmates cannot comfortably have their blood pressure repeatedly checked in a laboratory setting. Additionally, simulator arms provide an excellent opportunity for students to gain proficiency with assessing blood pressure extremes.
As in the Lee study, many students commented that they felt uncomfortable using the simulator arms.15 Aside from this experience, exposure to simulation in the PharmD curriculum is limited to a 2-hour interprofessional patient case at the local medical school, which occurs during the third year. While a few students may have completed their patient case at the time of this study, the blood pressure exercise required students to physically touch the mannequin, which differs from the exercise in the interprofessional case. Although students were given time in laboratory for orientation to the simulator arms prior to the start of the study, there may have been students who did not take advantage of the opportunity. Lack of familiarity with using the mannequin could have resulted in some of the inaccurate readings.
Students are expected to check patient blood pressures as a part of IPPEs at Drake. Faculty members have aimed to increase student comfort and competency with this skill by creating a 4-minute video that outlines the steps in performing a blood pressure assessment. Students also practice taking their peers’ vital signs in laboratory sessions and must demonstrate their ability to assess blood pressure as part of the laboratory practical in their first and second years. Although blood pressure technique is emphasized in the first 2 years, third-year students have limited exposure to evaluating blood pressure in laboratory and lecture. While it is important for students to continue having the opportunity to practice blood pressure on human arms, simulator arms provide a unique opportunity for students to practice measuring abnormally low or high blood pressures. This opportunity should not only improve student confidence in their technique but also prepare them to evaluate results of the measurement and make an appropriate treatment plan based on the case. The results of this study will help direct the efforts of faculty members to improve student blood pressure assessment, particularly if the blood pressure is abnormal.
There are several limitations to the study design that may affect the generalizability of the results to student blood pressure assessment in practice. Students were educated on the crossover design of the study as part of informed consent, which might have led to bias in blood pressure assessment. If students had recalled from the study description that they would be assessing blood pressures that were both normal and high, they might have been able to anticipate the general range of blood pressure simulation during the second session. For instance, students measuring a high blood pressure during the first laboratory time could have guessed that the next round would be normal (or vice versa). Considering that the 2 laboratory sessions were only a week apart, students were unlikely to forget the general scenario of the blood pressure simulation, potentially leading to an artificially inflated accuracy in blood pressure assessment. Although students also might have discussed the specific blood pressure reading with their peers in other laboratory sections, the investigators did not feel that this was a significant issue, considering that the students were graded solely on participation and not on the accuracy of their measurements. Additionally, investigators periodically alternated between 2 different prespecified readings for both the normal and high blood pressure treatment arms, thereby reducing the chances that interstudent communication regarding results would produce readings that were more accurate than they would have been without such communication.
Because the blood pressure simulator arms cannot mimic true interpatient variability in the brachial artery, students experienced challenges with palpating to find the location. The current study eliminated the variable of palpating to find the location, which could have resulted in an overrepresentation of student ability to assess blood pressures in clinical practice. However, some students had difficulties with measurements on the simulator arms even though the location for placing the bell of the stethoscope was distinctly marked. In fact, 3 students were unable to assess simulator arm blood pressures during at least 1 of their sessions.
Because simulator arms were programmed for the loudest volume setting, the Korotkoff sounds that students heard were likely more pronounced than they would be with blood pressure assessments for many patients. With the stethoscope placed in the appropriate location on the simulator arm, the main variable encountered for blood pressure assessment was a consistent sphygmomanometer pressure release rate at approximately 2 millimeters of mercury per second. Considering that the ability to hear Korotkoff sounds was controlled for in the study design, more error may be experienced in clinical practice.
Students were allowed as many attempts and as much time as they needed in order to assess blood pressures. This construct cannot be generalized to assessing blood pressure in live patients because of variables such as the patient’s arm comfort from multiple attempts, the patient’s allocated time for blood pressure assessment, and the clinician’s other responsibilities. While the mean number of attempts was only 2, students who made more attempts may not have as many chances to obtain accurate results in a true patient setting. An additional variable that could not be accounted for was the variability of the students’ IPPEs in the curriculum. Some students may have had more practical experience taking blood pressure assessments than others. Finally, because practice time on the simulator arms was not mandatory, some students may have practiced more and become more comfortable with the process than others. These issues should not impact the results, however, given that a crossover design was used in which students served as their own controls.
CONCLUSIONS
Students’ accuracy in measuring HSBP was significantly different (p<0.001) than in measuring NSBP using the simulator arm, but their accuracy in measuring HDBP was not significantly different (p < 0.089) from that of NDBP using the simulator arm. Additional instruction and experience with evaluating high blood pressure measurements may be needed. Future studies could focus on abnormal blood pressures (both hypertensive and hypotensive patient scenarios) to confirm these findings.
ACKNOWLEDGEMENTS
This project was funded by an internal grant from the Harris Research Endowment, Drake University College of Pharmacy and Health Sciences. We thank Andrea Kjos, PharmD, PhD, for providing consultation on methodological and statistical considerations.
REFERENCES
- 1.Murphy SL, Xu J, Kochanek KD. Deaths: preliminary data for 2010. Natil Vital Stat Rep. 2012;60(4) http://www.cdc.gov/NCHS/data/nvsr/nvsr60/nvsr60_04.pdf. Accessed June 11, 2012. [Google Scholar]
- 2.Centers for Disease Control and Prevention. Vital signs: prevalence, treatment, and control of hypertension: United States, 1999-2002 and 2005-2008. MMWR. 2011;60(4):103–108. [PubMed] [Google Scholar]
- 3.Reid F, Murray P, Storrie M. Implementation of a pharmacist-led clinic for hypertensive patients in primary care – a pilot study. Pharm World Sci. 2005;27(3):202–207. doi: 10.1007/s11096-004-2563-y. [DOI] [PubMed] [Google Scholar]
- 4.Chabot I, Moisan J, Gregoire JP, Milot A. Pharmacist intervention program for the control of hypertension. Ann Pharmacother. 2003;37(9):1186–1193. doi: 10.1345/aph.1C267. [DOI] [PubMed] [Google Scholar]
- 5.Mangum SA, Kraenow KR, Narducci WA. Identifying at-risk patient through community pharmacy-based hypertension and stroke prevention screening projects. J Am Pharm Assoc. 2003;43(1):50–55. [PubMed] [Google Scholar]
- 6.Carter BL, Zillich AJ, Elliott WJ. How pharmacists can assist physicians with controlling blood pressure. J Clin Hypertens. 2003;5(1):31–37. doi: 10.1111/j.1524-6175.2003.01460.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Vivian EM. Improving blood pressure control in a pharmacist-managed hypertension clinic. Pharmacotherapy. 2002;22(12):1533–1540. doi: 10.1592/phco.22.17.1533.34127. [DOI] [PubMed] [Google Scholar]
- 8.Accreditation Council for Pharmacy Education. Accreditation standards & guidelines for the professional program in pharmacy leading to the doctor of pharmacy degree. https://www.acpe-accredit.org/pdf/FinalS2007Guidelines2.0.pdf. Accessed June 11, 2012.
- 9.Westberg SM, Adams J, Thiede K, Stratton TP, Bumgardner MA. An interprofessional activity using standardized patients. Am J Pharm Educ. 2006;70(2):Article 34. doi: 10.5688/aj700234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Seybert AL, Laughlin KK, Benedict NJ, Barton CM, Rea RS. Pharmacy student response to patient-simulation mannequins to teach performance-based pharmacotherapeutics. Am J Pharm Educ. 2006;70(3):Article 48. doi: 10.5688/aj700348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chaikoolvatana A, Goodyer L. Evaluation of a multimedia case-history simulation program for pharmacy students. Am J Pharm Educ. 2003;67(1):Article 16. [Google Scholar]
- 12.Fernandez R, Parker D, Kalus JS, Miller D, Compton S. Using a human patient simulation mannequin to teach interdisciplinary team skills to pharmacy students. Am J Pharm Educ. 2007;71(3):Article 51. doi: 10.5688/aj710351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Seybert AL, Kobulinksy LR, McKaveney TP. Human patient simulation in a pharmacotherapy course. Am J Pharm Educ. 2008;72(2):Article 37. doi: 10.5688/aj720237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Seybert AL, Barton CM. Simulation-based learning to teach blood pressure assessment to doctor of pharmacy students. Am J Pharm Educ. 2007;71(3):Article 48. doi: 10.5688/aj710348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lee JL, Sobieraj DM, Kuti EL. Student measurement of blood pressure using a simulator arm compared with a live subject’s arm. Am J Pharm Educ. 2010;74(5):Article 82. doi: 10.5688/aj740582. [DOI] [PMC free article] [PubMed] [Google Scholar]


