Abstract
Aim:
To describe a technique of phalloplasty that is devoid of donor site scarring and suitable for urethral inlay and penile prosthesis in subsequent stages in cases of aphallia.
Materials and Methods:
Four patients with various disorders of sex development with 46 XY and severe penile deficiency, including one with complete androgen insensitivity syndrome who was initially raised as female, have been operated using a “Bird Wing” lower abdominal skin crease incision.
Results:
The patients’ age ranged from 6 to 17 years with preoperative stretched penile lengths between 1 and 2.5 cm. Phallic sizes between 7.5 and 12.5 cm was achieved leaving the donor site unremarkable with lower abdominal skin crease linear scar and excellent postoperative recovery.
Conclusions:
This phalloplasty technique can be utilized as a definitive procedure in many situations of penile insufficiency. Subsequent stages of urethral repair and insertion of penile prosthesis can be easily added.
Keywords: Androgen insensitivity syndrome, Aphallia, bladder exstrophy, disorders of sex development, gender dysphoria, phalloplasty
INTRODUCTION
Phallic reconstruction is indicated when penile development is either deficient due to congenital anomalies or loss of penis due to any cause or gender dysphoria.[1,2] Increasing recognition of the role played by androgens in the perinatal period and gender dysphoria occurring later in life has led to a paradigm shift in approach to gender assignment. As a result masculinizing genitoplasty is increasingly offered to children with aphallia and complete androgen insensitivity syndrome. Increasing acceptance of the transsexual individual by society will result in an increase in the number of patients presenting for sex reassignment.[3] Of the various procedures in vogue, the most popular has been the forearm flap.[4] Others are anterolateral thigh flap,[5] suprapubic flaps, lateral arm free flaps and extended pedicle island groin flap.[6–8] The current procedures involve aggressive interventions, undesirable sequele, and requirement of high level of technical expertise. Perfect technique does not exist and no flap can be considered the gold standard.[9]
We describe a novel technique which can be easily performed with a staged approach.
MATERIAL AND METHODS
We describe four patients who presented at different ages with penile deficiency. The first case had initially presented as a girl at 14 years with right inguinal hernia. Investigations revealed a female phenotype, a stretched penile length of 1.0 cm, a blind vaginal pouch, and chromosomal sex of 46XY. He was a case of complete androgen insensitivity syndrome (C.A.I.S.) who desired a gender reassignment to male at the age of 17 years. After taking appropriate steps in counseling, phalloplasty was performed. The second and fourth cases were partial androgen insensitivity syndrome (P.A.I.S.). The third was a case of 5 α reductase deficiency. They presented at 6, 19, and 15 years, respectively, with stretched penile lengths between 2.0 and 2.5 cm, all reared as males and wanted phalloplasty.
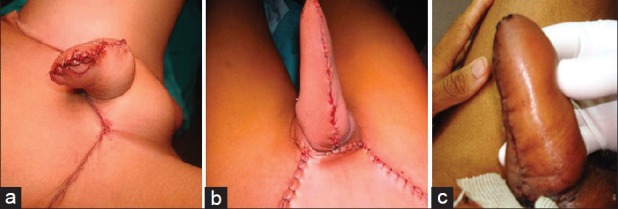
Technique: Abdominal flap demarcation: Under general anesthesia, patient is placed in lithotomy position. Urethral lumen is catheterized easily by inserting a Foley's catheter. A “bird wing” incision was marked with its base in suprapubic/mons pubic location and lateral extensions up to lower abdominal skin crease extending to both flanks [Figure 1]. The base to limb ratio of the flaps is kept at 4 or 5: 1, so that adequate blood supply is ensured to the most distal end. It may be noted that a unique feature of this flap design is the common base which sustains blood supply to both the flaps [Figures 1 and 2a]. The depth of the incision reaches up to the anterior rectus sheath and the external oblique aponeurosis, from medial to lateral. Thus, the blood supply of this region is provided by superficial epigastric and circumflex iliac vessels. Abdominal “flap-apposition” and phalloplasty: Both lateral “wings” are approximated in the midline using subcuticular sutures [Figure 2b].
Figure 1.
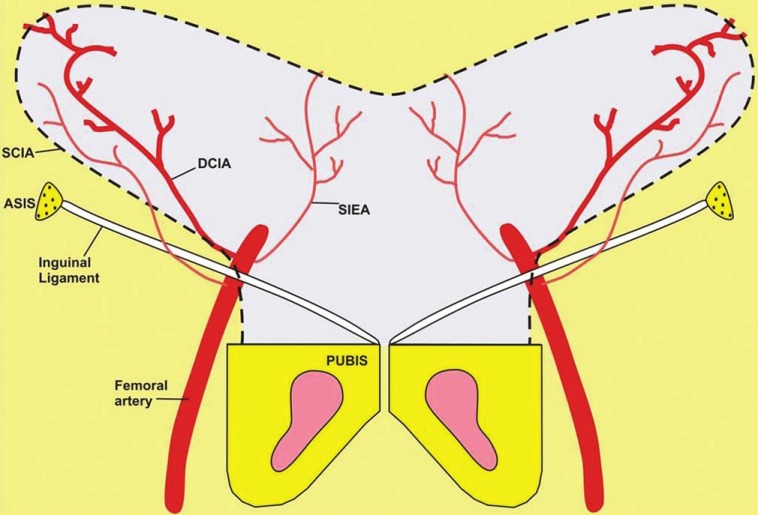
Vascular supply to the “bird wing abdominal flaps.” Abbreviations: ASIS-anterior superior iliac spine; SCIA—superficial circumflex iliac artery; DCIA—deep circumflex iliac artery; SIEA—superficial inferior epigastric artery
Figure 2a.

(a) A “bird wing” incision is marked with its base in mons pubic location and lateral extensions up to lower abdominal skin crease extending laterally. The base to limb ratio of the flaps is kept at 4 or 5:1 so that adequate blood supply is ensured to the most distal ends. It may be noted that a unique feature of this flap design is the common base which sustains blood supply to both the flaps.
Figure 2b.

(b) (immediate postoperative): Both lateral “wings” are approximated in the midline using subcuticular sutures. (c) at 1 year
RESULTS
The phalloplasty remained viable during the follow-up [Figure 2c]. Note the closure of donor area in a linear, skin crease suture line [Figure 3a]. The wound healing is excellent, both, at donor area as well as in the neo-phallus [Figures 3 and 4] and is ready for subsequent stages of urethroplasty and penile implantation. Case-wise duration of follow up in the present series is as follows: Case 1: 1 year; case 2: 6 months; case 3: 6 months and case 4: 4 months.
Figure 3.
(a-c) Note donor area suture line in lower abdominal skin crease and the immediate post-operative appearance of different cases
Figure 4.

(a) Preoperative and (b, c) early post-operative appearances
DISCUSSION
The most common indications for phalloplasty in children include aphallia, micropenis, ambiguous genitalia, phallic inadequacy associated with epispadias/bladder exstrophy, and female to male gender reassignment in adolescents.[10] While scrotal phalloplasty serves as an excellent and reproducible technique,[1] its use is restricted as a temporizing procedure suited for neonates born with aphallia (penile agenesis). In older children, the goal of phalloplasty is to ultimately make an aesthetically appearing neophallus followed by creation of a competent neourethra to allow for voiding while standing and sufficient rigidity. It is desirable that the donor site be left with minimal scarring and deformity.[11]
The psychological effects from penile dysmorphic disorders may have serious consequences. Use of genitoplasty will become an increasingly common place as patient satisfaction is reported. It would also be imperative to develop a technique which would meet the goals of phalloplasty and at the same time simple to construct with least complications. Presently, gender reassignment surgery is a series of complex surgical procedures (genital and non genital) performed for the treatment of gender dysphoria. Genital procedures performed for gender dysphoria, such as vaginoplasty, clitoro-labioplasty, penectomy and orchidectomy in male-to-female transsexuals, and penile and scrotal reconstruction in female-to-male transsexuals, are the core procedures in gender reassignment surgery.[12]
While preliminary phalloplasty is a desirable goal, it is often not immediately successful. Fistulas and strictures frequently accompany urethral reconstructions[13,14] and patients present with frequent urinary complications and extra scarred tissues. Refinements in technique[15] and necessity has led to acceptance of staged repair.[9,13,16] Recent flaps consist of (1) pedicled anterolateral thigh flap[7] (6 cases performed), (2) innervated island pedicled anterolateral thigh flap[17] (1 case), (3) free prefabricated fibular flap without fibula[18] (5 cases), (4) reinnervated latissimus dorsi myocutaneous free flap[19] (22 cases), with high complication rates (7 hematomas, 1 partial necrosis, 2 vascular thrombosis, 3 excessive swelling of the neophallus, 1 skin graft loss at donor site). In spite of the innovation of this technique, the complication rate is high, donor-site morbidity is still present (in terms of disfigurement and loss of function of the latissimus dorsi muscle), the urinary tract still needs to be reconstructed, and genital sensitivity is not reported. Recent review, specific to phalloplasty for sex reassignment surgery,[20] confirmed that only limited outcomes are present or given in the scientific literature, for social integration, patient satisfaction, and physiological function.[9] Studies confirm that complications are common, mainly with respect to urinary function, multistage procedure is the rule, and obtaining rigidity is still problematic.[14,21]
In the present technique, the first stage is completed by using lower abdominal wall flaps. The second stage involves urethral reconstruction and can be planned any time after 6 months to a year. Urethral reconstruction in neophalloplasty presents a great challenge for surgeons who manage genital reconstruction. Different flaps (penile skin, scrotal skin, abdominal skin, labial skin, vaginal flaps, etc.) or grafts (skin, bladder, buccal mucosa) have been suggested for urethral lengthening. Although possible in a single stage,[22] urethral reconstruction is generally delayed[1] as s ingle stage procedure using free grafts is associated with high complication rates[14,16,22,23] in order to allow adequate healing for the phallic procedure as has also been preferred in the present series.
Recent long-term follow-ups are now clarifying limitations posed by radial forearm flap, fibula flap, suprapubic flap, and metoidioplasty. Metoidioplasty can serve as an alternative[24] for patients who seek to change their external genitalia but who want to avoid the extensive scarring associated with more comprehensive phalloplasty techniques. However, the final result does not allow for sexual intercourse in hardly any of the patients; it allows for voiding while standing.[25] New techniques such as anterolateral thigh and latissimus dorsi flaps cause extensive scarring and cannot be judged properly at this moment because of limited cases performed and lack of long-term follow-up.[9]
The final stage in phalloplasty involves making a provision for rigidity required for penetration. Penile prostheses are subject to continuous development and divided into two general types: Semi rigid (malleable and mechanical) and inflatables.[26] Fasciocutaneous phalloplasties require the insertion of a penile prosthesis for penetration. Complications include erosion, exposure, infection, mechanical failure, and penile fibrosis. Autologous tissues including bone and cartilage have been used; however, these materials can resorb over time or fracture. It is generally felt that insertion of a penile prosthesis should be done at a stage when the neo-phallus is completely healed and protective sensation has returned about an year after the initial surgery.[27]
For neonates and infants who require phallic reconstruction, we routinely offer scrotal phalloplasty as a temporizing procedure.[1] Abdominal phalloplasty should be undertaken prior to (as in our case 2) or just around the time of puberty (10-14 years) in an effort to minimize the psychological trauma associated with genital inadequacy.[28,29] We offer abdominal phalloplasty as the definite procedure. All phalloplasty techniques use somatic tissue that is not hormone responsive and will grow commensurate with the rest of the body. A native penis, however, grows exponentially during puberty in response to hormonal surges. Thus, when reconstructing a pediatric patient a near adult size phallus should be planned as growth of the somatic tissue will be linear[29,30] as has been done in our cases in the present series [Figures 2–4].
CONCLUSION
There has been considerable reduction in the use of microsurgical techniques for penile reconstruction over the years. Long-term results reflect the constraints in achieving desired results. Aggressive procedures leave behind unacceptable deformities at donor sites and less than expected outcomes. Single stage reconstructions have given way to staged reconstruction mainly due to complications associated with urethral repair. It is hoped that a simpler technique such as the abdominal “bird wing” phalloplasty would pave the way for setting more pragmatic goals under the present circumstances.
Footnotes
Source of Support: Nil
Conflict of Interest: No
REFERENCES
- 1.Bajpai M. Scrotal phalloplasty: A novel surgical technique for aphallia during infancy and childhood by pre-anal anterior coronal approach. J Indian Assoc Pediatr Surg. 2012;17:162–4. doi: 10.4103/0971-9261.102335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Goenka A, Jain V, Sharma R, Gupta AK, Bajpai M. MR diagnosis of penile agenesis: Is it just absence of a phallus? Pediatr Radiol. 2008;38:1109–12. doi: 10.1007/s00247-008-0910-1. [DOI] [PubMed] [Google Scholar]
- 3.Gilbert DA, Winslow BH, Gilbert DM, Jordan GH, Horton CE. Transsexual surgery in the genetic female. Clin Plast Surg. 1988;15:471–87. [PubMed] [Google Scholar]
- 4.Wei FC, Jain V, Celik N, Chen HC, Chuang DC, Lin CH. Have we found an ideal soft tissue flap? An experience with 672 anterolateral thigh flaps. Plast Reconstr Surg. 2002;109:2219–26. doi: 10.1097/00006534-200206000-00007. [DOI] [PubMed] [Google Scholar]
- 5.Rashid M, Sarwar SU. Avulsion injuries of the male external genitalia: Classification and reconstruction with the customized radial forearm free flap. Br J Plast Surg. 2005;58:585–92. doi: 10.1016/j.bjps.2004.12.014. [DOI] [PubMed] [Google Scholar]
- 6.Hage JJ, de Graaf PU, van den Hoek JN, Bloem JJ. Phallic construction in female-to-male transsexuals using a lateral upper arm sensate free flap and a bladder mucosa graft. Ann Plast Surg. 1993;31:275–80. doi: 10.1097/00000637-199309000-00014. [DOI] [PubMed] [Google Scholar]
- 7.Felici N, Felici A. A new phalloplasty technique: The free anterolateral thigh flap phalloplasty. J Plast Reconstr Aesthet Surg. 2006;59:153–7. doi: 10.1016/j.bjps.2005.05.016. [DOI] [PubMed] [Google Scholar]
- 8.Akoz T, Kargi E. Phalloplasty in a female-to-male transsexual using a double pedicle composite groin flap. Ann Plast Surg. 2002;48:423–7. doi: 10.1097/00000637-200204000-00014. [DOI] [PubMed] [Google Scholar]
- 9.Selvaggi G, Elander A. Penile reconstruction/formation. Curr Opin Urol. 2008;18:589–97. doi: 10.1097/MOU.0b013e328313679c. [DOI] [PubMed] [Google Scholar]
- 10.Bluebond-Langner R, Redett RJ. Phalloplasty in complete aphallia and ambiguous genitalia. Sem Plast Surg. 2011;25:196–205. doi: 10.1055/s-0031-1281489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hage JJ, Bouman FG, de Graaf FH, Bloem JJ. Construction of the neophallus in female-to-male transsexuals: The Amsterdam experience. J Urol. 1993;149:1463–8. doi: 10.1016/s0022-5347(17)36416-9. [DOI] [PubMed] [Google Scholar]
- 12.Selvaggi G, Bellringer J. Gender reassignment surgery: An overview. Nat Rev Urol. 2011;8:274–82. doi: 10.1038/nrurol.2011.46. [DOI] [PubMed] [Google Scholar]
- 13.De Castro R, Merlini E, Rigamonti W, Macedo A., Jr Phalloplasty and Urethroplasty in Children With Penile Agenesis: Preliminary Report. J Urol. 2007;177:1112–7. doi: 10.1016/j.juro.2006.10.095. [DOI] [PubMed] [Google Scholar]
- 14.Panfilov DE. Augmentative phalloplasty. Aesthetic Plast Surg. 2006;30:183–97. doi: 10.1007/s00266-004-0153-y. [DOI] [PubMed] [Google Scholar]
- 15.Djordjevic ML, Bumbasirevic MZ, Vukovic PM, Sansalone S, Perovic SV. Musculocutaneous latissimus dorsi free transfer flap for total phalloplasty in children. J Pediatr Urol. 2006;2:333–9. doi: 10.1016/j.jpurol.2006.05.003. [DOI] [PubMed] [Google Scholar]
- 16.Descamps MJ, Hayes PM, Hudson DA. Phalloplasty in complete aphallia: Pedicled anterolateral thigh flap. Plast Reconstr Aesthet Surg. 2009;62:e51–4. doi: 10.1016/j.bjps.2007.04.014. [DOI] [PubMed] [Google Scholar]
- 17.Rubino C, Figus A, Dessy LA, Alei G, Mazzocchi M, Trignano E, et al. Innervated island pedicled anterolateral thigh flap for neo-phallic reconstruction in female-to-male transsexuals. J Plast Reconstr Aesthet Surg. 2009;62:e45–9. doi: 10.1016/j.bjps.2007.11.056. [DOI] [PubMed] [Google Scholar]
- 18.Dabernig J, Chan LK, Schaff J. Phalloplasty with free (septocutaneous) fibular flap sine fibula. J Urol. 2006;176:2085–8. doi: 10.1016/j.juro.2006.07.036. [DOI] [PubMed] [Google Scholar]
- 19.Vesely J, Hyza P, Ranno R, Cigna E, Monni N, Stupka I, et al. New technique of total phalloplasty with reinnervated latissimus dorsi myocutaneous free flap in female-to-male transsexuals. Ann Plast Surg. 2007;58:544–50. doi: 10.1097/01.sap.0000245123.16757.15. [DOI] [PubMed] [Google Scholar]
- 20.Sutcliffe PA, Dixon S, Akehurst RL, Wilkinson A, Shippam A, White S, et al. Evaluation of surgical procedures for sex reassignment: A systematic review. J Plast Reconstr Aesthet Surg. 2009;62:294–306. doi: 10.1016/j.bjps.2007.12.009. [DOI] [PubMed] [Google Scholar]
- 21.Monstrey S, Hoebeke P, Dhont M. Radial forearm phalloplasty: A review of 81 cases. Eur J Plast Surg. 2005;28:206–12. [Google Scholar]
- 22.Djordjevic M, Kojic S, Stanojevic D, Jocic D, Bizic M. Total phalloplasty in female transsexuals: Technique and outcomes. Eur Urol Suppl. 2011;10:579. [Google Scholar]
- 23.Chibber PJ, Shah HN, Jain P, Yadav P. Male gender assignment in aphallia: A case report and review of the literature. Intern Urol Nephrol. 2005;37:317–9. doi: 10.1007/s11255-004-7974-0. [DOI] [PubMed] [Google Scholar]
- 24.Perovic SV, Djordjevic ML. Metoidioplasty: A variant of phalloplasty in female transsexuals. BJU Int. 2003;92:981–5. doi: 10.1111/j.1464-410x.2003.04524.x. [DOI] [PubMed] [Google Scholar]
- 25.Hage JJ, van Turnhout AA. Long-term of metaidoioplasty in 70 female-to-male transsexuals. Ann Plast Surg. 2006;57:312–6. doi: 10.1097/01.sap.0000221625.38212.2e. [DOI] [PubMed] [Google Scholar]
- 26.Bettocchi C, Palumbo F, Spilotros M, Palazzo S, Saracino GA, Martino P, et al. Penile prostheses. Ther Adv Urol. 2010;2:35–40. doi: 10.1177/1756287209359174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hage JJ, De Graaf FH. Addressing the ideal requirements by free flap phalloplasty: Some reflections on refinements of technique. Microsurgery. 1993;14:592–8. doi: 10.1002/micr.1920140910. [DOI] [PubMed] [Google Scholar]
- 28.Masuda H, Azuma H, Segawa N, Iwamoto Y, Inamoto T, Takasaki N, et al. Surgical correction of buried penis after traffic accident: A case report. BMC Urol. 2004;4:6. doi: 10.1186/1471-2490-4-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hinman F., Jr Microphallus: Characteristics and choice of treatment from a study of 20 cases. J Urol. 1972;107:499. doi: 10.1016/s0022-5347(17)61063-2. [DOI] [PubMed] [Google Scholar]
- 30.Jezior JR, Brady JD, Schlossberg SM. Management of penile amputation injuries. World J Surg. 2001;25:1602–9. doi: 10.1007/s00268-001-0157-6. [DOI] [PubMed] [Google Scholar]


