Abstract
Floridcemento-osseous dysplasia (FCOD) is a“fibro-osseouslesion” that characteristically affects the jaw bones of the middle-aged with multi-quadrant radiopaque cementum-like masses. In thepast, the condition was known with a variety of names causing confusion in diagnosis and treatment. The condition is usually asymptomatic and needs no treatment as such. The diagnosis of FCOD is made on the basis of typical clinico-radiological features and biopsy is usually not recommended due to the risk of postoperative infection. This paper reports a rare case of FCOD affecting mandible bilaterally in a forty-two years old woman.
Keywords: Cementum, dysplasia, florid
INTRODUCTION
Florid cemento-osseous dysplasia (FCOD), described by Melrose et al. for the first time in 1976; refers to a group of fibro-osseous (cemental) exuberant lesions that involve multiple quadrants of jaw bones.[1,2] Although FCOD is commonly seen in middle aged black females, the same is not uncommon in Caucasians and Asians.[3–5]
These lesions are clinically asymptomatic and may be found as incidental radiological finding presenting as multiple radiopaque masses within peripheral radiolucent rim located in two or more quadrants usually in tooth-bearing areas.[6] Rarely, the patient may complain of dull pain and alveolar sinus tract may be present exposing the avascular yellowish sclerotic calcified mass to the oral cavity, which might be consequent to the progressive alveolar atrophy under artificial denture or following extraction of teeth in the affected area.[2]
Biopsy for histopathological examination may not be required to confirm the diagnosis due to their characteristic radiological features. On the contrary, such attempt may increase the risk of infection or fracture of the jaw and hence will adversely affect the patient's health.[7]
CASE REPORT
A 45-year-old female patient presented to our department with a chief complaint of pain in the left molar region of the mandible for 1 month. The patient was otherwise healthy, and her physical examination showed no significant abnormality. Intraoral examination revealed a carious left mandibular first permanent molar and a missing second permanent molar which was extracted due to caries 2 years ago.
Intraoral periapical radiograph showed well-defined irregularly shaped sclerotic masses corresponding to the roots of first and second permanent molar teeth of left mandible [Figure 1]. Orthopantomogram showed multiple well-defined sclerotic masses with radiolucent border in both right and left molar region of the mandible [Figure 2]. These sclerotic masses were surrounded by a thin radiolucent border and appeared to be unattached to the root apices. All teeth were vital. The results of routine hemogram and serum alkaline phosphatase were within normal limits. Biopsy was not done as the case was diagnosed as FCOD on the basis of characteristic clinico-radiological features.
Figure 1.
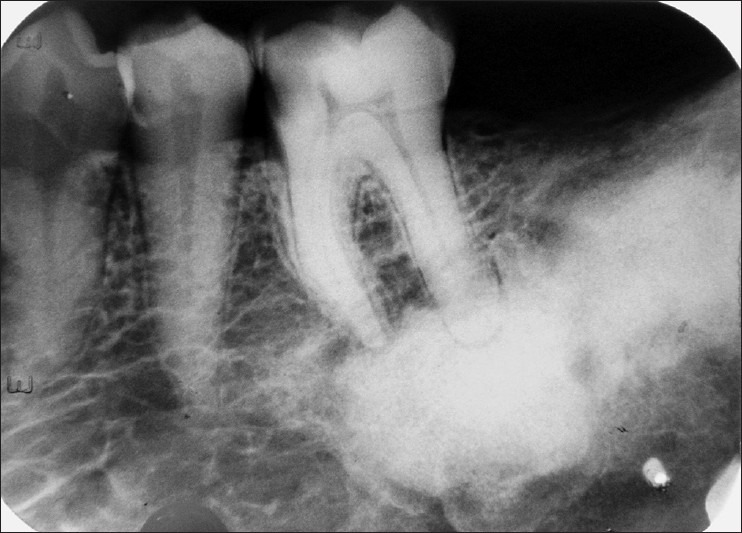
Intraoral periapical radiograph showing well-defined irregularly shaped sclerotic masses corresponding to the roots of left first and second permanent molar teeth of mandible
Figure 2.
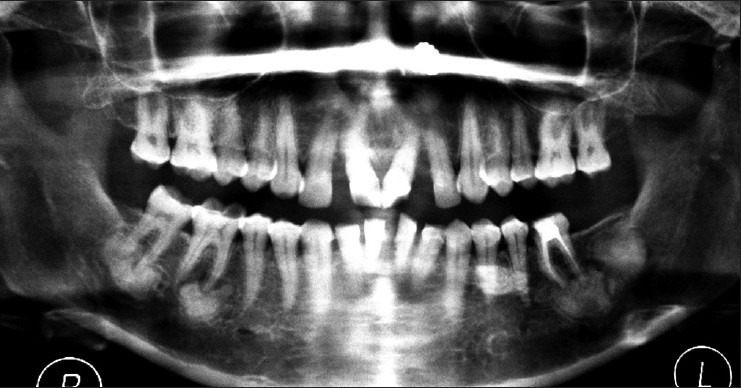
Orthopantomogram showing multiple well-defined sclerotic masses with radiolucent border in both right and left molar region of the mandible
DISCUSSION
FCOD is a non-neoplastic, reactive fibro-osseous lesion confined to the alveolar areas of the jaws and seen to have a typical female gender predilection affecting black women in 4th-5th decades with a mean age of 42 years. Similar lesions were found in oriental population and Caucasian females with identical age groups but a definite female predilection of the condition has not been explained.[8,9]
The pathogenesis of the condition still remains largely obscure. Some authors accredit to the proliferation of the fibroblastic mesenchymal stem cells in the apical periodontal ligament which are cementoblastic precursor stem cells, while others hold the view that it may arise from the remnants of the cementum left after tooth extraction.[10] Waldron[11] proposed that reactive or dysplastic changes in PDL might be the cause. Some authors attribute to the trauma from deep bite or heavy bite causing attrition of the teeth that may activate and cause proliferation of the fibroblasts in PDL causing FCOD.[10] However, we tend to disagree to the proposition of deep bite/occlusal trauma as contributing factors leading to FCOD as these conditions are uncommonly seen in males whose bite force is greater than the females.
FCOD may have certain jaw bone changes that are similar to familial gigantiform cementoma (FGC), another type of fibro-osseous lesion and thus creating great confusion in the differential diagnosis. However, FGC is an autosomal trait genetic disease and affects mostly children. The lesion is typical by its multi-quadrant expansile features affecting both the jaws; often crosses the midline producing asymmetry and facial disfigurement and is without any gender predilection. The overall behavior of FGC is more akin to benign neoplasia necessitating surgical intervention, which is otherwise contraindicated for the asymptomatic FCOD.[9]
The radiological features of enostosis or exostosis may sometimes cause diagnostic confusion for FCOD. However, their high dense radiopacities with common location of buccal surface of posterior maxillary teeth presenting as nodular growth with blanched out overlying mucosa differentiate exostosis from FCOD. The enostosis on the other hand, is not confined to jaw bones alone and may be found in other bones as well without a radiolucent rim surrounding the radiodense area, unlike FCODs.[8]
Some other lesions with similar features of FCOD are reported in the differential diagnosis including Gardener's syndrome, Paget's disease, chronic diffuse sclerosing osteomyelitis and cemento-ossifying fibroma.[8–10] Cemento-ossifying fibroma exhibits more buccolingual expansion than the FCOD whereas chronic diffuse sclerosing osteomyelitis are generally unilateral with soft-tissue swelling, fever and lymphadenopathy affecting primarily mandible with cyclic episodes of pain and is not always limited to the tooth bearing areas.[8,9] Sometimes it may be the complication of FCOD.[8] Unlike Gardener's syndrome, FCOD does not present other skeletal changes, no skin tumors or dental anomalies whereas Paget's disease affects mostly white males and is more of polyostotic with pathognomonic increase in serum alkaline phosphatase level.[9,10] Osteoblastoma causes more expansion of bony plates and have radiolucent rim.
The diagnosis of FCOD is principally based on clinical findings, localization of the lesion, patient's age, gender and ethnicity as well as radiological features.[8,10] The patients usually remain asymptomatic except when the disease is complicated by chronic osteomyelitis.[8–10]
In our case, we have diagnosed the condition as FCOD based on typical clinico-radiological features coupled with age and gender predilection and bilateral location in the mandible. We did not perform biopsy not only for the embodiment of the characteristic features leading to accurate diagnosis but also to avoid the risk of fractures of jaw bones and intractable infection.[8,10] Several authors have reported that following extraction of tooth in FCOD, the patients presented with poor socket healing and even sequestrum formation, thus complicating the condition. The antibiotics are usually not effective due to poor tissue diffusion.[8,9] Asymptomatic patients of FCOD generally do not require any treatment and should be kept under observation, and regular radiological follow-up.[8–10] Hence, we decided to abstain from surgical intervention and have kept the patient under regular clinico-radiological follow-up.
CONCLUSION
FCOD is a rare condition of jaw bones and diagnosed principally by its characteristic clinico-radiological features. As the condition remains asymptomatic, no surgical treatment is required. However, long term follow-up is carried out to assess the progress of the condition.
ACKNOWLEDGMENTS
We, the authors would like to thank Dr. Lipsa Bhuyan and Dr. Sambit Sarangi, PGT, Department of Oral Pathology and Microbiology, SCB Dental College and Hospital, Cuttack for their valuable assistance in editing the text and photographs and Sarat Kumar Nayak and Dr. Debabrata Giri, PGT, Department of Oral Pathology and Microbiology, SCB Dental College and Hospital, Cuttack for their technical work.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Mangala M, Ramesh DN, Surekha PS, Santosh P. Florid cemento-osseous dysplasia: Review and report of two cases. Indian J Dent Res. 2006;17:131–4. doi: 10.4103/0970-9290.29875. [DOI] [PubMed] [Google Scholar]
- 2.Kim JH, Song BC, Kim SH, Park YS. Clinical, radiographic, and histological findings of florid cemento-osseous dysplasia: A case report. Imaging Sci Dent. 2011;41:139–42. doi: 10.5624/isd.2011.41.3.139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gonçalves M, Píspico R, Alves F de A, Lugão CE, Gonçalves A. Clinical, radiographic, biochemical and histological findings of florid cemento-osseous dysplasia and report of a case. Braz Dent J. 2005;16:247–50. doi: 10.1590/s0103-64402005000300014. [DOI] [PubMed] [Google Scholar]
- 4.Pitak-Arnnop P, Dhanuthai K, Chaine A, Bertrand JC, Bertolus C. Florid osseous dysplasia: Report of a case presenting acute cellulitis. Med Oral Patol Oral Cir Bucal. 2009;14:e461–4. [PubMed] [Google Scholar]
- 5.Mac Donald-Jankowski DS. Florid cemento-osseous dysplasia: A systematic review. Dentomaxillofac Radiol. 2003;32:141–9. doi: 10.1259/dmfr/32988764. [DOI] [PubMed] [Google Scholar]
- 6.Babaria U, Patel H, Pandya H, Dewan H, Bhavasar B, Thakkar D, et al. Florid osseous dysplasia: A case report. J Dent Sci. 2011;2:10–1. [Google Scholar]
- 7.Dağistan S, Tozoğlu U, Göregen M, Cakur B. Florid cemento-osseous dysplasia: A case report. Med Oral Patol Oral Cir Bucal. 2007;12:E348–50. [PubMed] [Google Scholar]
- 8.Gündüz K, Avsever H, Karaçayli U, Senel B, Pişkin B. Florid cemento-osseous dysplasia: A case report. Braz Dent J. 2009;20:347–50. doi: 10.1590/s0103-64402009000400015. [DOI] [PubMed] [Google Scholar]
- 9.Bansa lS, Shetty S, Bablani D, Kulkarni S, Kumar V, Desai R. Florid osseous dysplasia. J Oral Maxillofac Pathol. 2011;15:197–200. doi: 10.4103/0973-029X.84497. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 10.Mehta RV, Khan S. Floridcement-osseousdysplasia: A case report. Indian Dent Res Rev. 2011;3:22–3. [Google Scholar]
- 11.Waldron CA. Fibro-osseous lesions of the jaws. J Oral Maxillofac Surg. 1985;43:249–62. doi: 10.1016/0278-2391(85)90283-6. [DOI] [PubMed] [Google Scholar]


