Abstract
Clear cell odontogenic carcinoma is a rare odontogenic tumor occurring predominantly in posterior mandible during 5th-7th decades with a female predilection. It is a potentially aggressive tumor, capable of frequent recurrences and loco-regional and distant metastases. Till date, only 73 cases have been reported in the literature. Current case is of a 55-year-old woman with tumor mass extending from canine to molar region on the left maxillary arch. Being locally aggressive tumor with the capacity to metastasize, it demands to be distinguished from other primary and metastatic clear cell tumors of the oral and maxillofacial region. A brief compilation of the reported cases is being attempted in the current article to better understand the behavior of the tumor.
Keywords: Biphasic pattern, clear cell odontogenic carcinoma, clear cells
INTRODUCTION
Clear cell odontogenic carcinoma (CCOC) is a rare neoplasm of the jaws and was first described by two separate groups of researchers, Hansen et al., and Waldron et al., in 1985. It was then termed as clear cell odontogenic tumor considering its locally destructive nature.[1,2] In 1992, it was included in the World Health Organization (WHO) classification of odontogenic tumors and was defined as a benign neoplasm with a capacity for locally invasive growth, and was considered more aggressive than ameloblastoma. Reichart and Philipsen proposed a revision of the classification of odontogenic tumors in 2003, clearly considering the clear cell odontogenic tumor as a carcinoma.[2] However, owing to its behavior as an infiltrative neoplasm with a marked tendency for local recurrence, regional lymph node metastasis and possible distant pulmonary metastasis, in the WHO classification of 2005, CCOC was denoted as a malignant tumor of odontogenic origin.[3] In the past, the terms “clear cell ameloblastoma” and “clear cell odontogenic tumor” were synonymous for CCOC.[3,4]
CASE REPORT
A 55-year-old woman reported to the Department of Oral Pathology, Dr. R. Ahmed Dental College and Hospital, Kolkata with a four month history of painless swelling in left upper jaw region. On inspection, a smooth surfaced, mucosal colored swelling of 3 cm diameter was observed with buccal cortical plate expansion extending from 23 to 25. The premolars were slightly displaced and an ulcer was observed in the interdental region on the palatal aspect [Figure 1]. On palpation, the swelling was non-tender, non-fluctuant, and firm in consistency. The regional teeth 24 and 25 were non-tender, but mobile. Bilateral cervical lymph nodes were not palpable. Orthopantomogram revealed a well-delineated, unilocular radiolucent lesion extending from the mesial aspect of 23-26 with divergence of roots of the regional teeth [Figure 2]. The patient's personal, family, and medical histories were non-contributory. The hematological tests were also within normal limits and no other systemic abnormality was observed.
Figure 1.

Intraoral view showing buccal cortical expansion with ulceration on the palatal aspect
Figure 2.
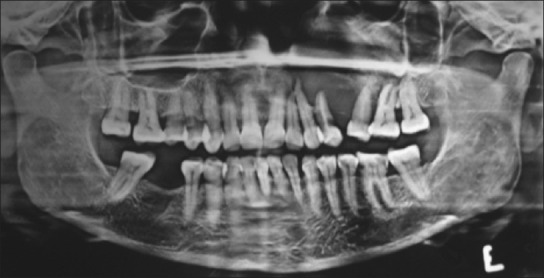
Orthopantomogram showing ill-defined radiolucent lesion i.r.t. right maxillary posterior region with displaced roots of the regional teeth
With a provisional diagnosis of intraosseous odontogenic tumor, incisional biopsy was performed under local anesthesia. Microscopically, sections stained with H and E revealed sheets and islands of large clear cells separated by a delicate fibrous connective tissue stroma [Figure 3]. Under higher magnification, biphasic population of cells characterized by polygonal, clear cells and hyperchromatic, basaloid cells with eosinophilic cytoplasm were seen. Occasional islands showed peripheral palisading. Nuclear pleomorphism was minimal, and mitotic figures were rare. In addition, the fibrous connective tissue stroma exhibited some areas of hyalinization, but no fibrous capsule was identified at the periphery of the tumor [Figure 4].
Figure 3.
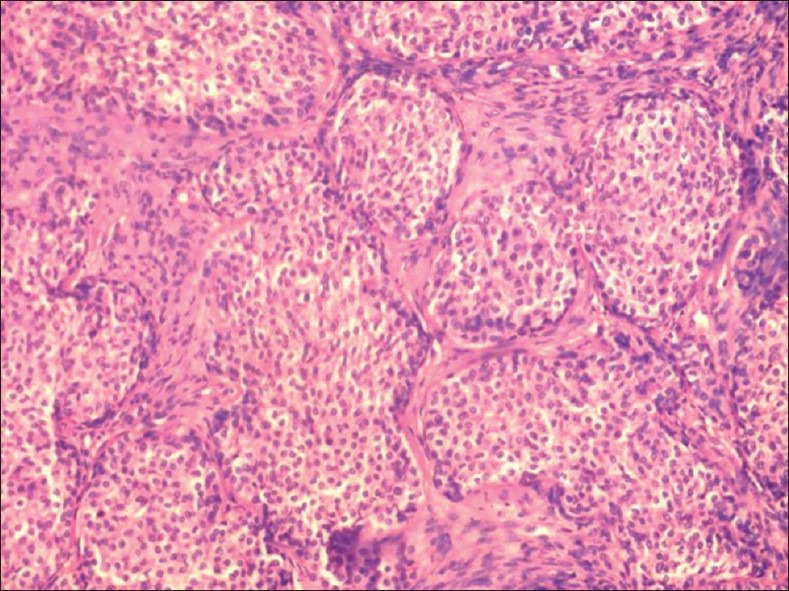
H and E stained section showing islands of clear cells in fibrous connective tissue stroma (×40)
Figure 4.
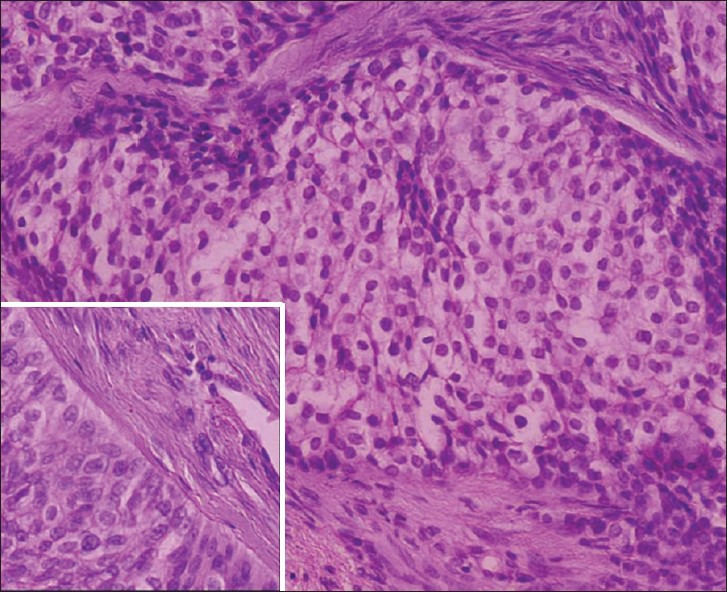
H and E stained section showing islands of polygonal, clear cells with interspersed hyperchromatic, columnar cells having eosinophilic cytoplasm (×100), Inset: Nuclear palisading observed at the periphery of the island (×400)
The abundant cytoplasm of the clear cells showed diastase sensitive Periodic Acid Schiff-positive granules, indicating intracytoplasmic glycogen deposition [Figure 5]. Tumor cells were immunoreactive for cytokeratins (CKs) 8 and 19, while non-reactive for S-100 and vimentin. Focal heterogeneous moderate immunostaining pattern was observed for CK-8 [Figure 6]. CK-19 on the other hand showed moderate, diffuse, heterogeneous pattern of immunoreactivity in the tumor islands [Figure 7]. Vimentin was strongly positive in the fibrous stromal component only [Figure 8].
Figure 5.
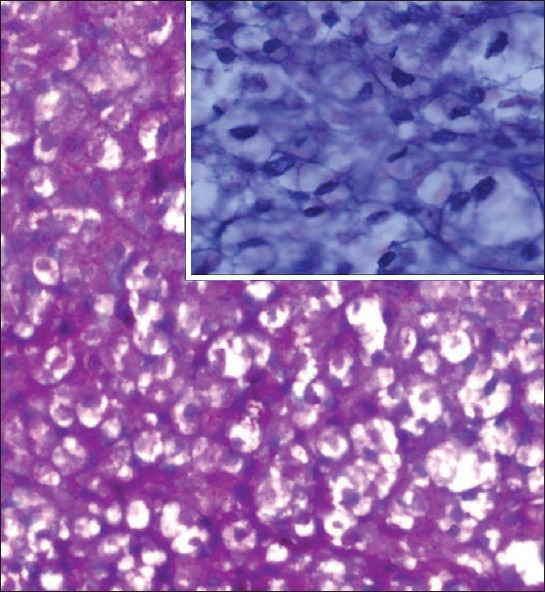
PAS-positive cytoplasmic granules. Inset: diastase sensitive granules (×400)
Figure 6.
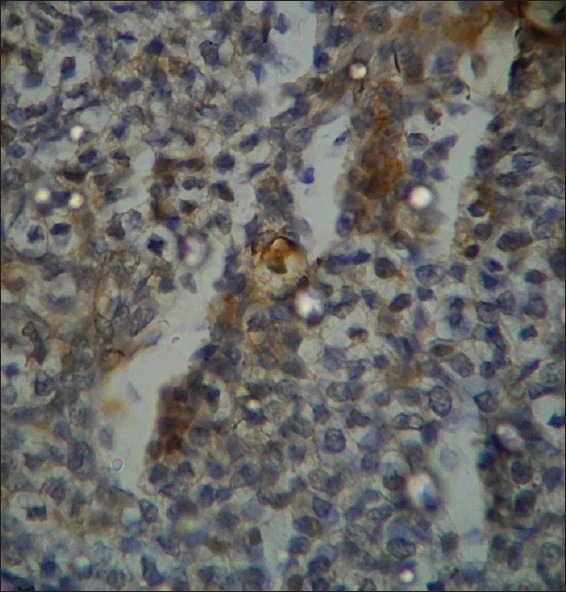
Mild cytokeratin (CK-8) immunoreactivity in the tumor islands (×400)
Figure 7.
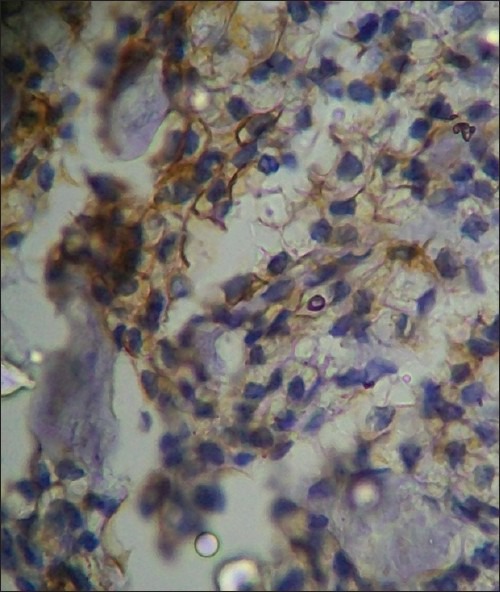
Moderate cytokeratin (CK-19) immunoreactivity (×400)
Figure 8.
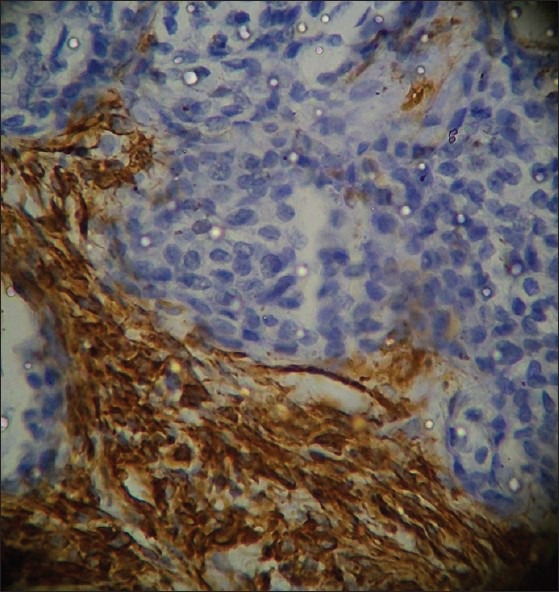
Vimentin immunoreactivity localized to the fibrous connective tissue stroma (×400)
Finally, a diagnosis of CCOC was made and the patient underwent radical resection of the tumor with wide surgical margins. The post-operative histopathological diagnosis was consistent with the incisional biopsy results. The patient made an uneventful recovery with no recurrence and metastasis observed 1 year post-operatively.
DISCUSSION
Clear cell odontogenic tumor was originally considered a benign, but locally invasive neoplasm. Later on, its local aggressive growth, frequent recurrences, and occasional metastases recorded in several cases led some authors to consider it as an odontogenic carcinoma.[5–9]
To the best of our knowledge, 73 cases of CCOC have been reported (excluding the present one) in the English dental literature till date. On analyzing the previous cases and the present one, CCOC has a female predilection with M/F ratio of 1:1.8 and majority of cases have been diagnosed in patients older than 40 years (81.0%). Mean age at the time of diagnosis was 54.2 years (range 17-89), with 58.2 years for women and 41.8 years of men. Mandible was involved in 57 cases (77.0%) and maxilla in 17 cases (23%). Posterior region of jaws is the more frequent site for CCOC in comparison to anterior (48% vs. 30%). In only 13% of cases, both anterior and posterior regions of the jaws were involved. The classic clinical presentation of CCOC has been reported to be of a painless swelling in the mandible or maxilla.[10–14] Pain and regional teeth mobility were the occasionally associated symptoms. Three patients complained of paresthesia of the lower lip.
On studying the radiographic appearance of the reported cases, 69 cases (93.2%) manifested as radiolucent, whereas five cases (6.8%) exhibited a mixed radiolucent–radiopaque lesion.[15–19] Cases in which exact radiographic appearance were registered showed that the lesion demonstrated as both well and poorly delineated in a ratio approximately 1:1 (22:21).[15,20] Histopathologically, CCOC exhibits three histological patterns: Biphasic, monophasic, and ameloblastomatous.[4,5,10,11,20] Majority of tumors reported had a biphasic pattern with nests of clear cells along with small islands of hyperchromatic, polygonal cells with eosinophilic cytoplasm. These cells surround the periphery of the tumor islands or may form ductal structure at times. The monophasic pattern has islands of clear cells entirely. The ameloblastomatous pattern is the least common type, and is characterized by presence of clear cells in the nests within the follicular network.[21] According to some authors, CCOC and clear cell ameloblastoma are continuum of the same pathological process, but this contention has not gained much acceptance.[5]
Several authors have noticed occurrence of hyalinized or partly hyalinized stroma separating the neoplastic islands.[21] Miyauchi et al., and Kumamoto et al., found eosinophilic hyaline deposits (reminiscent of amyloid-like globules) in calcifying epithelial odontogenic tumor formed in direct contact with epithelial nests in their reported cases.[17,21,22] The degree of nuclear pleomorphism, hyperchromatism, and number of mitoses in CCOC are quite variable. In general, encapsulation is seldom seen and it frequently invades the medullary bone, muscle, and the neural tissue.[23,24]
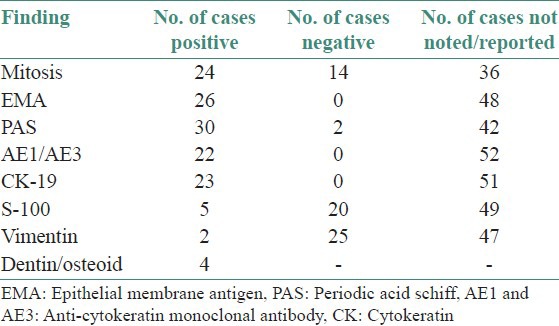
Glycogen storage is quite common in these tumors displaying PAS positivity which is diastase sensitive.[9,21–23,25] The reports on immunohistochemical findings of CCOC have been inconsistent. Immunoreactivity for CKs, specifically for CKs 8, 13, 18 and 19 has been reported.[4,5] Data from the 74 reported cases of CCOC (including the present case) were compiled and it was noted that 32.43% cases showed increased and atypical mitotic activity. PAS positivity was reported in 40.5% of the cases. Tumor cells were immunoreactive to Epithelial Membrane Antigen (EMA) in 35.2%, AE1/AE3 in 29.7%, CK-19 in 31.1%, S-100 in 6.7%, and Vimentin in only 2.7% of the cases.[2–6,9,10,12,20,26–32] However, the major limitation was lack of reporting in majority of cases. Findings are summarized in Table 1.
Table 1.
Special findings and immunoprofile of the 74 reported cases
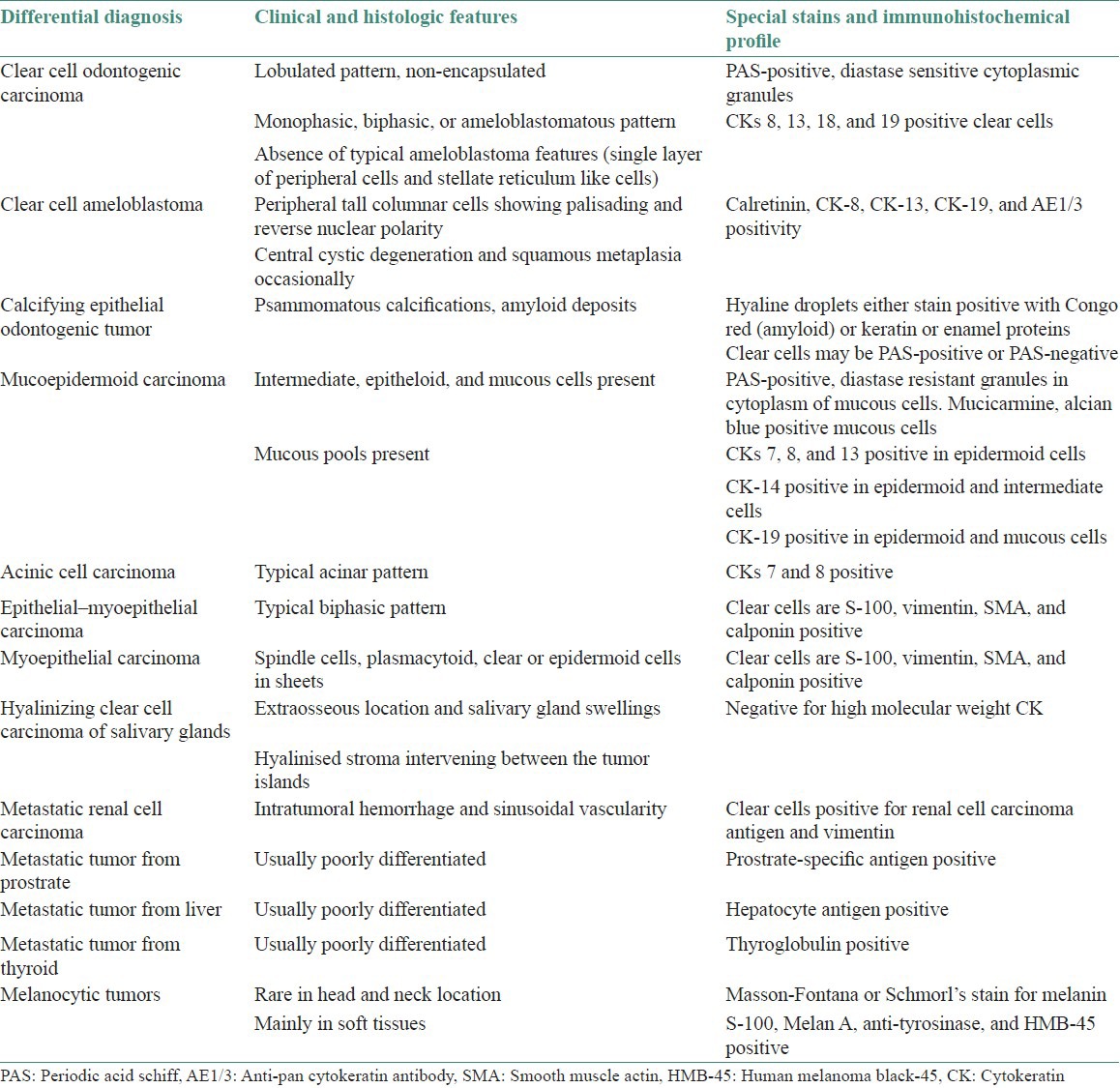
Differential diagnosis includes a wide range of clear cell lesions that may occur in the oral and maxillofacial regions. They may originate from various sources including odontogenic tumors such as ameloblastoma, calcifying epithelial odontogenic tumor, odontogenic carcinoma, and salivary gland tumors like mucoepidermoid carcinoma or hyalinizing clear cell carcinoma. Also includes intraosseous melanocytic tumors, and metastatic tumors from kidney, thyroid, and prostate.[23–26,33] PAS, mucicarmine, and alcian blue stains must be negative to rule out mucoepidermoid carcinoma; in addition, amyloid deposition and/or calcifications in the tumor cells or the intercellular space must be absent to exclude the clear cell variant of calcifying epithelial odontogenic tumor on Congo red-stained slides. Finally, a metastatic lesion can be excluded on clinical and radiological grounds. Microscopically, CCOC lacks prominent sinusoidal vascularity and intratumoral hemorrhage that characterize metastatic renal carcinoma, which is the main possibility when considering a distant primary neoplasm with clear cell differentiation. In addition, immunohistochemistry may be useful in the differential diagnosis of CCOC, as clear cell salivary gland tumors tend to express positive results for S-100 protein, CK, vimentin, and muscle actin, whereas odontogenic tumors with clear cell differentiation react negatively for vimentin and muscle actin.[27–29,33–38] Considerable histological and immunological overlaps may result in difficulty in differentiating clear cell carcinoma of salivary gland from CCOC in the maxillary or mandibular region. Ellis and Elizabeth et al., favored location as a criterion and suggested that the central osseous destruction seen with CCOC is more supportive of odontogenic origin.[39,40] A brief compilation of the differential diagnosis is given in Table 2.
Table 2.
Differential diagnosis of clear cell odontogenic carcinoma
Treatment for CCOC is primarily resection with a wide margin. Other treatment modalities reported include curettage or enucleation, surgical resection with or without lymph node dissection, post-operative radiotherapy, and/or chemotherapy. In the literature, 53 (73%) patients were initially treated with surgical resection, 15 (21%) patients underwent curettage or enucleation, and 1 patient was treated from the onset with chemotherapy. Although no specific treatment was mentioned in literature for four cases. Nine patients had a neck dissection in addition to the surgery. Local recurrences, most of them as multiple regional node and distant metastases are frequently reported.[3,12,34] On long-term follow-up, the overall recurrence rate for this tumor was 38.35% (28/73), thus emphasizing the need for long-term follow-up. Of the 15 patients who were treated by enucleation or curettage, 13 (86.7%) patients had local and/or regional recurrences, 3 of 4 (75%) patients who died of the tumor developed distant metastatic disease. By contrast, local and/or regional recurrence occurred in 14 (14/53, 26.4%) patients who underwent surgical resection. Therefore, the recurrence rate after initial treatment by resection was lower than conservative therapy (26.4 vs. 86.7%).[21,41–49] The survival rate at 13 years after initial diagnosis is around 21%. Adjuvant radiation therapy may be beneficial in patients with extensive soft tissue or perineural invasion, in cases in which tumor-free margins are not possible or in patients with positive nodes and/or extracapsular spread.[5,31–33,50,51]
CONCLUSION
CCOC is a rare malignant odontogenic neoplasm with benign looking histology. The acknowledgment of this rare tumor and its distinction from other clear cell neoplasms is crucial in establishing the appropriate therapeutic plan. Furthermore, as only small number of cases are reported in the literature, long-term follow-up studies might help in understanding the biological behavior of this tumor.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Hansen LS, Eversole LR, Green TL, Powell NB. Clear cell odontogenic tumor: A new histologic variant with aggressive potential. Head Neck Surg. 1985;8:115–23. doi: 10.1002/hed.2890080208. [DOI] [PubMed] [Google Scholar]
- 2.Reichart PA, Philipsen HP. Odontogenic Tumors and Allied Lesions. London: Quintessence Publishing Co Ltd; 2004. Metastasizing, malignant ameloblastoma; pp. 239–48. [Google Scholar]
- 3.Barnes L, Eveson JW, Reichart PA, Sidransky D. WHO Classification of Tumors, Pathology and Genetics of Head and Neck Tumours. Lyon, France: IARC Press; 2005. WHO histological classification of odontogenic tumours; p. 284. [Google Scholar]
- 4.Werle H, Blake FA, Reichelt U, Schmelzle R, Heiland M. Clear-cell odontogenic carcinoma: A new case and long-term follow-up of an old case, and review of the literature. J Oral Maxillofac Surg. 2009;67:1342–8. doi: 10.1016/j.joms.2008.06.020. [DOI] [PubMed] [Google Scholar]
- 5.Maiorano E, Altini M, Viale G, Piattelli A, Favia G. Clear cell odontogenic carcinoma. Report of two cases and review of the literature. Am J Clin Pathol. 2001;116:107–14. doi: 10.1309/WUQ8-D3A8-YV1Y-0VTR. [DOI] [PubMed] [Google Scholar]
- 6.Xavier FC, Rodini CO, Ramalho LM, Sarmento VA, Nunes FD, de Sousa SC. Clear cell odontogenic carcinoma: Case report with immunohistochemical findings adding support to the challenging diagnosis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008;106:403–10. doi: 10.1016/j.tripleo.2008.03.010. [DOI] [PubMed] [Google Scholar]
- 7.Yamamoto H, Inui M, Mori A, Tagawa T. Clear cell odontogenic carcinoma: A case report and literature review of odontogenic tumors with clear cells. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1998;86:86–9. doi: 10.1016/s1079-2104(98)90155-x. [DOI] [PubMed] [Google Scholar]
- 8.Muramatsu T, Hashimoto S, Inoue T, Shimono M, Noma H, Shigematsu T. Clear cell odontogenic carcinoma in the mandible: Histochemical and immunohistochemical observations with a review of the literature. J Oral Pathol Med. 1996;25:516–21. doi: 10.1111/j.1600-0714.1996.tb00308.x. [DOI] [PubMed] [Google Scholar]
- 9.Mosqueda-Taylor A, Meneses-García A, Ruíz-Godoy Rivera LM, de Lourdes Suárez-Roa M. Clear cell odontogenic carcinoma of the mandible. J Oral Pathol Med. 2002;31:439–41. doi: 10.1034/j.1600-0714.2002.00133.x. [DOI] [PubMed] [Google Scholar]
- 10.Ariyoshi Y, Shimahara M, Miyauchi M, Nikai H. Clear cell odontogenic carcinoma with ghost cells and inductive dentin formation: Report of a case in the mandible. J Oral Pathol Med. 2002;31:181–3. doi: 10.1034/j.1600-0714.2002.310310.x. [DOI] [PubMed] [Google Scholar]
- 11.Benton DC, Eisenberg E. Clear cell odontogenic carcinoma: Report of a case. J Oral Maxillofac Surg. 2001;59:83–8. doi: 10.1053/joms.2001.19300. [DOI] [PubMed] [Google Scholar]
- 12.Braunshtein E, Vered M, Taicher S, Buchner A. Clear cell odontogenic carcinoma and clear cell ameloblastoma: A single clinicopathologic entity. A new case and comparative analysis of the literature? J Oral Maxillofac Surg. 2003;61:1004–10. doi: 10.1016/s0278-2391(03)00311-2. [DOI] [PubMed] [Google Scholar]
- 13.Chera BS, Villaret DB, Orlando CA, Mendenhall WM. Clear cell odontogenic carcinoma of the maxilla: A case report and literature review. Am J Otolaryngol. 2008;29:284–90. doi: 10.1016/j.amjoto.2007.08.001. [DOI] [PubMed] [Google Scholar]
- 14.Ng KH, Siar CH. Peripheral ameloblastoma with clear cell differentiation. Oral Surg Oral Med Oral Pathol. 1990;70:210–3. doi: 10.1016/0030-4220(90)90121-8. [DOI] [PubMed] [Google Scholar]
- 15.Chaine A, Pitak-Arnnop P, Dhanuthai K, Bertrand JC, Bertolus C. An asymptomatic radiolucent lesion of the maxilla. Clear cell odontogenic carcinoma. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009;107:452–457. doi: 10.1016/j.tripleo.2008.09.029. [DOI] [PubMed] [Google Scholar]
- 16.Dahiya S, Kumar R, Sarkar C, Ralte M, Sharma MC. Clear cell odontogenic carcinoma: A diagnostic dilemma. Pathol Oncol Res. 2002;8:283–5. doi: 10.1007/BF03036748. [DOI] [PubMed] [Google Scholar]
- 17.Iezzi G, Rubini C, Fioroni M, Piattelli A. Clear cell odontogenic carcinoma. Oral Oncol. 2002;38:209–13. doi: 10.1016/s1368-8375(01)00038-0. [DOI] [PubMed] [Google Scholar]
- 18.Miyauchi M, Ogawa I, Takata T, Ito H, Nikai H, Ijuhin N, et al. Clear cell odontogenic tumour: A case with induction of dentin-like structures? J Oral Pathol Med. 1998;27:220–4. doi: 10.1111/j.1600-0714.1998.tb01945.x. [DOI] [PubMed] [Google Scholar]
- 19.Sadeghi EM, Levin S. Clear cell odontogenic carcinoma of the mandible: Report of a case. J Oral Maxillofac Surg. 1995;53:613–6. doi: 10.1016/0278-2391(95)90079-9. [DOI] [PubMed] [Google Scholar]
- 20.Nair MK, Burkes EJ, Chai-U-Dom O. Radiographic manifestation of clear cell odontogenic tumor. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2000;89:250–4. doi: 10.1067/moe.2000.101796. [DOI] [PubMed] [Google Scholar]
- 21.Eversole LR, Duffey DC, Powell NB. Clear cell odontogenic carcinoma. A clinicopathologic analysis. Arch Otolaryngol Head Neck Surg. 1995;121:685–9. doi: 10.1001/archotol.1995.01890060083017. [DOI] [PubMed] [Google Scholar]
- 22.Kumamoto H, Yamazaki S, Sato A, Yamaguchi T, Tezuka F, Ooya K. Clear cell odontogenic tumor in the mandible: Report of a case with duct-like appearances and dentinoid induction. J Oral Pathol Med. 2000;29:43–7. doi: 10.1034/j.1600-0714.2000.290108.x. [DOI] [PubMed] [Google Scholar]
- 23.Müller H, Slootweg P. Clear cell differentiation in an ameloblastoma. J Maxillofac Surg. 1986;14:158–160. doi: 10.1016/s0301-0503(86)80283-1. [DOI] [PubMed] [Google Scholar]
- 24.Zhang J, Liu L, Pan J, Tian X, Tan J, Zhou J, et al. Clear cell odontogenic carcinoma: Report of 6 cases and review of the literature. Med Oncol. 2011;28:626–33. doi: 10.1007/s12032-010-9668-z. [DOI] [PubMed] [Google Scholar]
- 25.Avninder S, Rakheja D, Bhatnagar A. Clear cell odontogenic carcinoma: A diagnostic and therapeutic dilemma. World J Surg Oncol. 2006;4:91. doi: 10.1186/1477-7819-4-91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Marí A, Escutia E, Carrera M, Pericot J. Clear cell ameloblastoma or odontogenic carcinoma. A case report. J Craniomaxillofac Surg. 1995;23:387–90. doi: 10.1016/s1010-5182(05)80135-0. [DOI] [PubMed] [Google Scholar]
- 27.Ebert CS, Jr, Dubin MG, Hart CF, Chalian AA, Shockley WW. Clear cell odontogenic carcinoma: A comprehensive analysis of treatment strategies. Head Neck. 2005;27:536–42. doi: 10.1002/hed.20181. [DOI] [PubMed] [Google Scholar]
- 28.August M, Faquin W, Troulis M, Kaban L. Clear cell odontogenic carcinoma: Evaluation of reported cases. J Oral Maxillofac Surg. 2003;61:580–6. doi: 10.1053/joms.2003.50114. [DOI] [PubMed] [Google Scholar]
- 29.Adebiyi K, Ugboko V. Clear cell odontogenic carcinoma of the maxilla: A case report. Internet J Dent Sci. 2005:2. [Google Scholar]
- 30.Kumar M, Fasanmade A, Barrett AW, Mack G, Newman L, Hyde NC. Metastasising clear cell odontogenic carcinoma: A case report and review of the literature. Oral Oncol. 2003;39:190–4. doi: 10.1016/s1368-8375(02)00012-x. [DOI] [PubMed] [Google Scholar]
- 31.Brandwein M, Said-Al-Naief N, Gordon R, Urken M. Clear cell odontogenic carcinoma: Report of a case and analysis of the literature. Arch Otolaryngol Head Neck Surg. 2002;128:1089–95. doi: 10.1001/archotol.128.9.1089. [DOI] [PubMed] [Google Scholar]
- 32.Elbeshir EI, Harris M, Barrett AW. Clear cell odontogenic carcinoma of the maxilla: Clinical, histological and immunohistochemical features of a case. Oral Oncol Extra. 2004;40:91–4. [Google Scholar]
- 33.Adamo AK, Boguslaw B, Coomaraswarmy MA, Simos C. Clear cell odontogenic carcinoma of the mandible: Case report. J Oral Maxillofac Surg. 2002;60:121–6. doi: 10.1053/joms.2002.27539. [DOI] [PubMed] [Google Scholar]
- 34.Li TJ, Yu SF, Gao Y, Wang EB. Clear cell odontogenic carcinoma: A clinicopathologic and immunocytochemical study of 5 cases. Arch Pathol Lab Med. 2001;125:1566–71. doi: 10.5858/2001-125-1566-CCOC. [DOI] [PubMed] [Google Scholar]
- 35.de Aguiar MC, Gomez RS, Silva EC, de Araújo VC. Clear-cell ameloblastoma (clear-cell odontogenic carcinoma): Report of a case. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1996;81:79–83. doi: 10.1016/s1079-2104(96)80153-3. [DOI] [PubMed] [Google Scholar]
- 36.Carinci F, Volinia S, Rubini C, Fioroni M, Francioso F, Arcelli D, et al. Genetic profile of clear cell odontogenic carcinoma. J Craniofac Surg. 2003;14:356–62. doi: 10.1097/00001665-200305000-00014. [DOI] [PubMed] [Google Scholar]
- 37.Favia G, Altini M, Maiorano E. Clear cell odontogenic carcinoma: Ultrastructural and immunohistochemical study of two cases. J Oral Pathol Med. 1998;27:365. [Google Scholar]
- 38.Odukoya O, Arole O. Clear-cell ameloblastoma of the mandible (a case report) Int J Oral Maxillofac Surg. 1992;21:358–9. doi: 10.1016/s0901-5027(05)80762-3. [DOI] [PubMed] [Google Scholar]
- 39.Ellis GL. Clear cell neoplasms in salivary glands: Clearly a diagnostic challenge. Ann Diagn Pathol. 1998;2:61–78. doi: 10.1016/s1092-9134(98)80035-x. [DOI] [PubMed] [Google Scholar]
- 40.Bilodeau EA, Hoschar AP, Barnes EL, Hunt JL, Seethala RR. Clear cell carcinoma and clear cell odontogenic carcinoma: A comparative clinicopathologic and immunohistochemical study. Head Neck Pathol. 2011;5:101–7. doi: 10.1007/s12105-011-0244-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Bang G, Koppang HS, Hansen LS, Gilhuus-Moe O, Aksdal E, Persson PG, et al. Clear cell odontogenic carcinoma: Report of three cases with pulmonary and lymph node metastases. J Oral Pathol Med. 1989;18:113–118. doi: 10.1111/j.1600-0714.1989.tb00746.x. [DOI] [PubMed] [Google Scholar]
- 42.Fan J, Kubota E, Imamura H, Shimokama T, Tokunaga O, Katsuki T, et al. Clear cell odontogenic carcinoma. A case report with massive invasion of neighboring organs and lymph node metastasis. Oral Surg Oral Med Oral Pathol. 1992;74:768–75. doi: 10.1016/0030-4220(92)90406-g. [DOI] [PubMed] [Google Scholar]
- 43.Milles M, Doyle JL, Mesa M, Raz S. Clear cell odontogenic carcinoma with lymph node metastasis. Oral Surg Oral Med Oral Pathol. 1993;76:82–9. doi: 10.1016/0030-4220(93)90299-j. [DOI] [PubMed] [Google Scholar]
- 44.Piattelli A, Sesenna E, Trisi P. Clear cell odontogenic carcinoma. Report of a case with lymph node and pulmonary metastases. Eur J Cancer B Oral Oncol. 1994;30B:278–80. doi: 10.1016/0964-1955(94)90010-8. [DOI] [PubMed] [Google Scholar]
- 45.Brinck U, Gunawan B, Schulten HJ, Pinzon W, Fischer U, Füzesi L. Clear-cell odontogenic carcinoma with pulmonary metastases resembling pulmonary meningothelial-like nodules. Virchows Arch. 2001;438:412–7. doi: 10.1007/s004280000365. [DOI] [PubMed] [Google Scholar]
- 46.Duffey DC, Bailet JW, Newman A. Ameloblastoma of the mandible with cervical lymph node metastasis. Am J Otolaryngol. 1995;16:66–73. doi: 10.1016/0196-0709(95)90012-8. [DOI] [PubMed] [Google Scholar]
- 47.Vesper M, Wilck T, Donath K, Schmelzle R. Clear cell odontogenic carcinoma in connection with squamous epithelial carcinoma. Case report and review of the literature. Mund Kiefer Gesichtschir. 1998;2:270–4. doi: 10.1007/s100060050073. [DOI] [PubMed] [Google Scholar]
- 48.Siriwardena BS, Tilakaratne WM, Rajapaksha RM. Clear cell odontogenic carcinoma: A case report and review of literature. Int J Oral Maxillofac Surg. 2004;33:512–4. doi: 10.1016/j.ijom.2003.08.006. [DOI] [PubMed] [Google Scholar]
- 49.Waldron CA, Small IA, Silverman H. Clear cell ameloblastoma – An odontogenic carcinoma. J Oral Maxillofac Surg. 1985;43:707–17. doi: 10.1016/0278-2391(85)90198-3. [DOI] [PubMed] [Google Scholar]
- 50.Berho M, Huvos AG. Central hyalinizing clear cell carcinoma of the mandible and the maxilla a clinicopathologic study of two cases with an analysis of the literature. Hum Pathol. 1999;30:101–5. doi: 10.1016/s0046-8177(99)90308-8. [DOI] [PubMed] [Google Scholar]
- 51.Kumamoto H, Kawamura H, Ooya K. Clear cell odontogenic tumor in the mandible: Report of a case with an immunohistochemical study of epithelial cell markers. Pathol Int. 1998;48:618–22. doi: 10.1111/j.1440-1827.1998.tb03959.x. [DOI] [PubMed] [Google Scholar]


