Abstract
Background
Identifying prodromal features that predate the onset of bipolar disorder (BD) may enable the prevention of BD and aid early intervention. This review addresses two key questions: Is there a bipolar prodrome? And, if there is, what are its characteristic features?
Method
A comprehensive search of databases (PubMed, MedLine, Embase, and PsychInfo) supplemented with hand-searches was used to identify studies of symptoms preceding the onset BD.
Results
Fifty-nine studies were identified, of which fourteen studies met inclusion criteria. Symptoms can predate the onset of BD by months to years and can be categorized as attenuated forms of BD symptoms, general symptoms common to a range of mental disorders, and personality traits, particularly cyclothymia. Two studies provided sufficient data to enable sensitivity and specificity to be calculated. Specificity of a number of the features was high (above 90%). However, sensitivity was generally low (all<60%). We propose a model based on the findings in the studies reviewed to illustrate the potential trajectory to BD and the points at which it may be possible to intervene.
Conclusions
Clinical features preceding the onset of BD can be identified. However, conclusions on whether there is a distinct prodrome to BD are restricted by the limitations of current evidence. The high specificity of some features suggests they may be useful in clinical practice. Large scale longitudinal studies are needed to validate these features and characterise their specificity and sensitivity in independent samples.
Keywords: bipolar disorder, affective disorders, prodrome, prodromal, identification, intervention, onset, symptoms, risk, risk factors, mania, hypomania, precursor, early
Introduction
Bipolar disorder (BD) is a common condition, and ranked amongst the top ten causes of global disability amongst adults by the WHO (Murray and Lopez, 1997; McIntyre and Konarski, 2004). A major factor contributing to the burden of disease is the substantial delay between the first experience of symptoms and the initiation of treatment, which can be as long as 8-9 years (Baldessarini et al. 1999; Highet et al. 2004; McIntyre and Konarski, 2004). Delays in initiating treatment for BD are associated with greater subsequent morbidity (Franchini et al. 1999; Baldessarini et al. 2003), and the response to mood stabilizer treatment is better earlier in the course of the disorder (Swann et al. 1999).
The association between early treatment initiation and better outcome suggests that the early identification of BD may be useful (Mrazek D and Mrazek PJ, 2004). There is an increasing movement towards early intervention in psychiatric illnesses (McGorry et al. 2003). One component of this approach is to identify, and offer intervention to, individuals who are in the prodromal phase that precedes the onset of frank illness (Yung and McGorry, 1996; McGorry et al. 2003).
The prodrome, by definition, can only be determined in retrospect. It constitutes a period of disturbance characterized by distinct features/symptoms leading up to the development of the full blown disorder (Conus et al. 2008). Prodromal features can, however, be used to identify individuals prospectively; although their clinical utility will depend on how specific they are to the illness in question.
The availability of specific treatments for bipolar disorder, and evidence that early intervention in BD is associated with a better outcome (Mrazek D and Mrazek PJ, 2004; Bauer et al. 2008), suggests that prevention could be effective in BD. However, it is as yet unclear whether a specific prodromal phase for BD can be identified. This comprehensive review provides a summary of the evidence evaluating the putative bipolar prodrome and addresses two key questions:
Is there a bipolar prodrome?
If there is bipolar prodrome, what are its characteristic features and how long does it last?
The paper reviews studies of symptoms/clinical features prior to the first manic or hypomanic episode as it is at this point that the diagnosis for BD can be first made. Features linked to the subsequent development of BD in patients with other diagnoses are beyond the scope of this review and have been addressed elsewhere (Berk et al. 2004; Calabrese et al. 2006; Henin et al. 2007).
METHODS
Search strategy
The PubMed, MedLine, Embase, Embase Classic and PsychInfo databases were electronically searched to identify relevant studies (see supplementary methods for further details). The abstracts of the papers identified by the search were screened by OH, SL and GT to identify papers meeting the selection criteria set out below. The papers identified through this process were then reviewed in full to identify those that those that met the selection criteria.
Selection Criteria
The following inclusion criterion was used:
Studies of clinical features preceding the onset of the first manic or hypomanic episode.
The following exclusion criteria were applied:
Studies that did not report specific clinical signs or symptoms.
Studies purely of diagnoses preceding the development of BD.
Reviews and other papers not reporting original data.
Data Extraction
Data were extracted independently by S.L. and G.T. and agreement confirmed by O.H. For each study the following variables were recorded: a) the year of publication, b) study design, c) sample characteristics, d) measurement scales used, e) frequency of putative prodromal features, f) criteria used to diagnose BD and g) time period from onset of putatively prodromal features to the onset of BD.
Method of analysis
It was not possible to combine the results for statistical analysis as the studies used different scales to assess putative prodromal features, and reported findings in a variety of ways. Rather we appraise and synthesise the data to address the key questions and calculate the sensitivity and specificity of putatively prodromal features for BD (see supplementary methods).
Results
Three hundred and eighteen studies were identified by the searches. The screening process is described in the supplementary methods and shown in supplementary figure 1. Following screening fourteen studies were identified for inclusion in the review. These have been divided according to methodology into retrospective and prospective studies and are summarized in tables 1 and 2 respectively.
Table 1. Retrospective studies.
| Author | Sample | Source | Instruments | BD diagnosis according to: |
Rating by | Size (n) |
Gender (M=male; F=female) |
Mean Age (SD) /yrs |
Comparator group |
Time Course: symptom onset to diagnosis |
|---|---|---|---|---|---|---|---|---|---|---|
| Lish et al. 1994 | Adults with BD (subtype not specified) |
Members of a BD support group |
Bespoke self-report questionnaire |
Self report | Patients | 500 | 181 M 313 F (6 N/A) |
N/A | None | % of sample in range: <6mth: 23% 6mths-5 yrs: 26% >5yrs: 51% |
| Egeland et al. 2000 | Bipolar I adults admitted to hospital for the first time. |
Single Amish community |
Bespoke semi- structured rating scale of antecedent symptoms recorded in clinical notes |
Research Diagnostic Criteria |
Investigators | 58 | 32 M 26 F |
N/A | None | Range: 9 to 12 years. |
| Fergus et al. 2003 | Children diagnosed with BD I and BD II |
Recruited through adverts in local press |
Bespoke symptom check-list rated for each year of life until diagnosis |
Parental report of a diagnosis given by a community clinician. |
Parents of children diagnosed with BD |
78 | 34 M 34 F |
13.7 (6.6) |
Well children (n=82) and children with other psychiatric diagnoses (n=38). |
N/A |
| Berk et al. 2007 | Adults diagnosed with BD I or schizo-affective disorder |
Recruited by adverts in local press and hospitals. |
Bespoke semi- structured questionnaire |
Not stated. | Investigators | 218 | 125 F 93 M |
41.8 (12.7) | None | Median time between first symptoms and first manic episode = 6.6 years (sd=n/a) |
| Correll et al. 2007 | Children diagnosed with BD I |
Subjects in a treatment trial |
Bespoke semi- structured interview of patient or carer (BPSS-R) |
KSADS criteria for n=33 and WASH-U- KSADS criteria for n=19 |
Investigators | 48 | 27 F 25 M |
16.2 (2.8) | None | Mean (sd) time between first symptoms and BD diagnosis= 1.8 (1.7) years |
| Rucklidge et al. 2008 |
Adolescents (13- 17yrs) diagnosed with BD I or II |
Recruited from an earlier study of neuro-cognitive function. |
Bespoke symptom checklist of range of psychiatric symptoms. |
DSM-IV-TR criteria for BD I or II based on WASH-U- KSADS |
Filled in by parents of subjects. |
25 | 10 M 15 F |
15.71 (1.55) |
Normal controls (n=28) and children with ADHD (n=29) |
N/A |
| Conus et al. 2010 | Adolescents/ adults diagnosed with a first episode of psychotic mania or schizo- affective disorder |
Recruited from referrals to a specialist service for first episode psychosis |
Bespoke questionnaire (IMPQ) |
DSM-IV criteria for BD I plus YMRS score>19 |
Investigators | 22 | 18 M 4 F |
23 (2.9) |
Nil | Mean (sd) time between first symptoms and diagnosis= 20.9 (16.4) weeks, range 2-49 weeks. |
* The authors have also published a report of an earlier follow-up of the same cohort
SADS= Schedule for Affective disorders and Schizophrenia. CDRS= Children’s depression rating scale YMRS= Young Mania Rating Scale GAF= Global Assessment of Functioning scale. PGBI= Parent General Behavior Inventory CBCL=Child Behavior Checklist DSM-IV= Diagnostic and statistical Manual, 4th edition. SSAS=Schizophrenia for School-Age Children, WASH-U-KSADS= Washington University in St Louis Schedule for Affective Disorders and Schizophrenia. BPSS-R= Bipolar Prodrome Symptom Scale-Retrospective. HAMD12= Hamilton Depression Rating Scale, CGI-BP= Clinical Global Impression Scale-Bipolar Version, CDME= Current Major Depressive/Manic Episode Checklist. RDC=Research Diagnostic Criteria. K-SADS-PL= Schedule for Affective Disorders and Schizophrenia for School Age Children; Present and Lifetime version. CRS= Conners’ Rating Scales, CBC= Child Behavior Rating Checklist, IMPQ= Initial Mania Prodrome Questionnaire, YMRS= Young Mania Rating Scale.
Table 2. Prospective studies.
| Author | Sample | Source | Instruments | BD diagnosis according to: |
Rating by | Size (n) of risk sample |
Gender (n) |
Mean Age (years old) |
Comparator Group |
Duration of study period. |
|---|---|---|---|---|---|---|---|---|---|---|
| Akiskal et al. 1985 | Relatives of BD | Referrals to a specialist outpatient clinic because of possible early signs of BD |
Bespoke questionnaire categorizing sub- syndromal mood symptoms based on a clinical interview |
Feighner Schema based on DSM-III criteria |
Investigator | 68 (n=39 developed a BD spectrum disorder) |
39 males, 29 females |
N/A (all <25 years old) |
68 older onset BD patients (all 25 years or older at onset) |
Mean=3 years (sd=n/a; range 1-8 years) |
| Thompson et al. 2003 |
3 patients referred to a specialist clinic for people at high risk of psychosis |
PACE (Personal Assessment and Crisis Evaluation) clinic in Australia. |
DSM-IV SCID BPRS YMRS |
DSM-IV criteria |
Investigator | 3 (all developed BD) |
3 females | 21 | None | 12 months |
| Angst et al. 2003 | High scoring adults on the SCL-90-R |
General community sample |
Social variables and emotional and vegetative lability measured using the SCL-90-R |
DSM-IV criteria for bipolar spectrum disorders |
Investigator | 591 (n=127 developed a BD spectrum disorder) |
Total sample: 299 females 292 males |
N/A (range 19- 20 at recruitment) |
A random sample of subjects scoring below the SCL-90 high score cut-off (n=261) |
15 years |
| Blechert and Meyer. 2005 | Adolescents scoring above a cut-off on the hypomanic personality scale |
Pupils at selected schools in Germany |
HYP, RIG, IMP, EPI-Lie |
DSM-IV criteria for BD II using a SCID inter- view. |
Teacher, Investigator |
114 (n=15 developed BD II) |
69 females 45 males |
19. 9 (sd=1.3) |
Adolescents scoring below a cut- off on the hypomanic personality scale (n=35) |
2 years |
| Kochman et al. 2005 | Children with major depression |
Consecutive children admitted to a hospital in France |
K-SADS, CHT, CDI, YMRS, CGAS, OAS |
DSM-IV criteria |
Investigator | Total=80 (n=35 developed BD) |
N/A | N/A (range: 7- 17) |
Subjects who did not develop BD (n=45) |
Mean=26.6 (sd=9) months |
| Cornell et al. 2008 |
Youths presenting with psychotic NOS or brief psychotic episode |
Referrals to an early intervention service for psychosis. |
K-SADS, SIDP-IV, SOPS, BDI, BAI, CDI |
DSM-IV criteria |
Investigator | 26 (n=4 developed BD) |
2 males, 2 females |
15.1 (sd=1.6) |
Referrals who did not develop BD (n=22) |
Mean=22.8 (sd=19.4) months |
| Tijssen et al. 2010a | Adolescents/young adults with no prior DSM IV diagnosis of BD or prior use of mental health services. |
Random population sample drawn from government registers for a geographic area. |
DIA-X/M-CIDI | DSM-IV criteria (for manic/ hypomanic episode). |
Investigator | 1902 (n=21 developed the outcome) |
Total sample: 1025 males, 877 females |
18.3 (sd=3.3). (range 14- 24) |
All subjects (n=1881) who had not developed BD by the study end |
Mean=8.3 years (sd=0.7; range 7.4- 10.6 years) |
BAI= Beck anxiety inventory, BDI= Beck depression inventory, BIS/BAS=behavioral inhibition/ activation scale, CARE- Child and Adolescent Research and Evaluation interview, CDI=children’s depression inventory, CHT=cyclothymic-hypersensitive questionnaire, CGAS=Clinical Global Assessment Scale, DSM-IV= Diagnostic and statistical manual version IV, EPI-lie= lie scale of the Eysenck Personality Inventory, HYP= Hypomanic Personality scale, IMP= Impulsive nonconformity scale, K-SADS= Schedule for Affective disorders and Schizophrenia for school age children, MSED=mood and self esteem diary, NOS=not otherwise specified, OAS= Overt Aggression Scale, PSQI=Pittsburgh Sleep Questionnaire, RIG= rigidity subscale of the Munich Personality Test, RSQ=response style questionnaire, SADS-L=Schedule for Affective Disorders and Schizophrenia-Lifetime version, SCL-90-R= Symptom Checklist-90-R, SIDP-IV=Structured interview for DSM-IV personality, SOPS= Scale of prodromal symptoms, YMRS= Young Mania Rating Scale. DIA-X/M-CIDI= Munich Composite International Diagnostic Interview.
Is there a prodrome to bipolar disorder?
The seven retrospective studies used a variety of methodologies to collect data from bipolar individuals and/or their carers about clinical features that predated the onset of the disorder (Lish et al. 1994; Egeland et al. 2000; Fergus et al. 2003; Berk et al. 2007; Correll et al. 2007; Rucklidge, 2008; Conus et al. 2010). These studies clearly indicate that there are symptoms that commonly precede the onset of frank BD in many patients. However, they have a number of methodological limitations, in particular the possibility recall bias has influenced the findings, and, in three studies, the lack of a validated assessment to determine the diagnosis (Lish et al. 1994; Fergus et al. 2003; Berk et al. 2007).
The seven prospective studies are less susceptible to recall bias and all use validated diagnostic assessments, indicating that they are likely to be more reliable sources of evidence. The case series by Thompson et al. (2003) describes the prospective assessment of cases using validated diagnostic instruments and rating scales. Consequently, one can be confident that the patients in this small case series did not meet diagnostic criteria for BD at initial assessment, and that the symptoms reported were not influenced by recall bias.
Three studies examined high risk clinical groups- either children/adolescents with unipolar depressive (Kochman et al. 2005), youths with brief psychotic episodes (Correll et al. 2008), or the relatives of individuals diagnosed with BD who were referred to a specialist clinic with suspected early signs of the condition (Akiskal et al.1985). All three studies report clinical features preceding the onset of BD, providing clear evidence of symptoms/clinical features preceding the onset of BD. However, these studies and the case series by Thompson et al. (2003) are in select samples, and so the findings may not be representative of the general population.
Data on putatively prodromal features of BD in general population community samples are provided in three studies (Angst et al. 2003; Blechert and Meyer, 2005; Tijssen et al. 2010a). Of these, the outcome in the study by Blechert & Meyer (2005) was a manic symptom dimension, rather than a diagnosis of BD, and so, whilst informative, it is less specific to the prodrome of BD than the other studies. The studies by Angst et al. (2003) and Tijssen et al. (2010a) are noteworthy in recruiting large community samples and in conducting follow-up assessments for up to fifteen and ten years respectively. The outcome in Angst et al. (2003) was bipolar spectrum disorder or BD-II, rather than a BD-I diagnosis. Angst et al. (2003) enriched their sample by identifying high risk subjects (those with high scores on the Symptom Checklist-90R, whom they hypothesized would be more likely to subsequently develop BD) and, importantly, included a control group- a random sample of average scorers on the same checklist. The study by Tijssen et al. (2010a) recruited its sample of adolescents/young adults at random from the population register for the Munich area so the sample is likely to be representative of the general population. Other strengths of this study are the exclusion of symptoms that were directly attributed to alcohol or drug use, and excluding subjects with a past or current diagnosis of BD at baseline. Subjects were assessed at two intermediate time points before the final assessment so the persistence of symptoms over time could also be evaluated. Both studies provide evidence of clinical features/symptoms preceding the onset of BD. Tijssen et al (2010a) report that over 70% of the subjects who subsequently developed BD had previously experienced at least two manic/hypomanic and/or depressive symptoms, whilst Angst et al. (2003) found that over 40% of subjects who developed BD-II had previously experienced mood lability.
Characteristics of the putatively prodromal features
Frequency and form of clinical features
Seven studies report the frequency of specific symptoms occurring within the putative bipolar prodrome, summarized in Table 3. The most commonly reported putatively prodromal features were mood lability/swings and depressive mood. In the study by Angst et al. (2003), one of the most methodologically sound studies, mood lability was the strongest risk factor for the subsequent diagnosis of a bipolar spectrum disorder (odds ratio, OR=14), greater even than a family history of mania (OR=7). Depressive mood was reported in five of the seven studies (jointly with mood swings in one study). However, even these relatively common features were not seen in all subjects. In addition, such symptoms were also reported to a lesser degree in control samples. Thus, depressed mood was reported in 5.8% of controls by Angst et al. (2003) and in 9% of controls by Egeland et al. (2003).
Table 3.
Frequency of specific symptoms preceding BD
| SYMPTOMS | Lish et al. 1994 | Shaw et al. 2005 | Angst et al. 2003 | Fergus et al. 2003 | Berk et al. 2007 | Correll et al. 2007 | Rucklidge et al. 2008 |
|---|---|---|---|---|---|---|---|
| Depressive mood | 32.8% | 11% | Not reported |
14.2% | 90.3% | 53.8% | 60% |
| Mood lability/swings |
12.8% | 10% | 32.6% | Not reported |
90.3% | 57.7% | 72% |
| Anxiety | Not reported |
13% | 39.5% | Not reported |
Not reported |
43.1% | 28% |
| Racing thoughts | Not reported |
Not reported |
Not reported |
11% | Not reported |
57.4% | 60% |
| Irritability/anger | 9.4% | 7% | Not reported |
14.1% | Not reported |
61.5% | 55.2% |
| Physical agitation |
32.0% | Not reported |
Not reported |
14.1% | Not reported |
48.1% | 48% |
Although data for individual symptoms are not reported in the study by Tijssen et al. (2010a), they did find that the combination of greater persistence and greater number of symptoms was associated with the greatest risk of subsequent transition to BD. Thus, symptom load may be more important than specific symptoms.
Many of the putatively prodromal symptoms (see table 3) are seen in established BD, and are probably attenuated forms of symptoms seen in the frank illness, whilst others are also features of other psychiatric disorders (American Psychiatric Association, 2000), and so may show relatively low specificity for BD.
In seven studies cyclothymic features were identified as a precursor of BD (Akiskal et al. 1985; Egeland et al. 2000; Fergus et al. 2003; Angst et al. 2003; Kochman et al. 2005; Berk et al. 2007; Rucklidge, 2008). However, these features are also seen in the well relatives of people with BD (Findling et al. 2005; Jones et al. 2006) so it is not clear if these features could be a correlate of risk status also seen in some relatives who do not go on to develop BD. Furthermore, it remains to be determined whether these features reflect premorbid personality characteristics or are part of a distinct prodrome to BD, an issue that could be usefully addressed in future research.
Only one report, by Fergus et al. (2003), included an analysis of the degree to which individual symptoms clustered together. The principal component analysis revealed four symptom dimensions associated with the later diagnosis of BD: depression, irritability/dyscontrol, mania and psychosis/suicidality. Together these explained about 50% of the variance.
Sensitivity and specificity of putative prodromal features
None of the studies give the sensitivity or specificity of the putatively prodromal symptoms for BD, and only two provided sufficient data to calculate these. We have calculated the sensitivity and specificity for the symptoms that were significantly associated with BD in these two studies (table 4).
Table 4.
Sensitivity and specificity of symptoms for BD compared to a healthy control group
| Symptoms occurring with onset aged 6-11 yrs old. Rucklidge et al. 2008 |
Sensitivity | Specificity |
|---|---|---|
| Elevated/ Irritable Mood lasting >1hour/day | 56% | 79% |
| Elevated/ Irritable Mood lasting >6hour/day | 32% | 95% |
| Depressed Mood lasting >1hour/day | 32% | 93% |
| Depressed Mood lasting >6hour/day* | 24% | 100% |
| Grandiosity | 32% | 82% |
| Racing Thoughts | 24% | 79% |
| Mood Swings | 48% | 77% |
|
Symptoms occurring with onset aged 12- 16 yrs old. Rucklidge et al,. 2008 |
Sensitivity | Specificity |
| Tantrums | 52% | 71% |
| Extremely Clingy | 24% | 91% |
| Excessive Anxiety and Worry | 48% | 82% |
| Anxiety causing impairment to Social Functioning |
28% | 89% |
| Marked Changes in Appetite | 44% | 79% |
| Elevated/ Irritable Mood lasting >1hour/day | 76% | 58% |
| Elevated/ Irritable Mood lasting >6hour/day* | 60% | 89% |
| Elevated/ Irritable Mood lasting >2days* | 56% | 93% |
| Depressed Mood lasting >1hour/day | 60% | 68% |
| Depressed Mood lasting >6h/day | 56% | 84% |
| Depressed Mood lasting >2 days | 44% | 89% |
| Suicidal Ideation | 52% | 82% |
| Self Harm | 48% | 84% |
| Often Awakes at Night | 44% | 79% |
| Very Rapid Speech | 60% | 72% |
| Racing Thoughts | 60% | 68% |
| Mood Swings | 72% | 53% |
| Takes Excessive Risks | 28% | 72% |
| Hears Voices | 28% | 96% |
| Grandiosity | 72% | 70% |
|
Symptoms of bipolar spectrum illness.
Angst et al. 2003 |
Sensitivity | Specificity |
| Mood lability | 30% | 89% |
incidence of symptoms differed significantly between subjects with BD and subjects with ADHD and controls.
Time course of putatively prodromal symptoms
Four studies provide data on the time lag between the onset of putatively prodromal features and the subsequent development of BD (see tables 1 and 2), although the mean duration of the prodrome to BD is only reported in two studies. It was 1.7 (SD=1.8) years in patients who developed psychotic mania, and 1.9 (SD=1.5) in those who developed non-psychotic mania (Correll et al. 2007), whilst in the other study, which was of patients with psychotic mania and schizo-affective disorder, it was 20.9 weeks (SD=16.4) (Conus et al. 2010).
There are also indications that distinguishing features may be present from very early on in development (Fergus et al. 2003; Shaw et al. 2005). Fergus et al. (2003) report when the incidence of the symptoms within each of the dimensions they examined was 10% greater in the BD children than in the comparator groups by age. The striking finding from this fine-grained analysis was that the irritability/dyscontrol symptom cluster differentiated the BD children from the comparator groups from age one onwards, a decade before the onset of BD. Symptoms from the other clusters differentiated the BD children from around age eight, four years on average before the onset of BD. The main caveat with this study is that the diagnosis of BD was not operationalised and is likely to have included children with a broad version of childhood BD, which favours the inclusion of subjects with marked irritability, rather than euphoria (Baroni et al. 2009).
Discussion
The existence of symptoms predating the onset of BD is a consistent finding across retrospective and prospective studies, and symptoms may be present in many patients for months to years before a definitive diagnosis of BD is made. This suggests that there may be a relatively prolonged prodrome to BD, contrary to previous ideas that it is brief (Kraepelin, 1921). We have identified a number of features that may comprise a putative prodromal phase of BD. These include attenuated affective symptoms, such as depressive mood and mood swings, and symptoms common to a number of disorders, such as higher levels of anger, irritability and dyscontrol. Thus, it may be possible to identify people with the prodromal signs of BD well in advance of the onset of the disorder. However, the extent to which people experiencing putatively prodromal symptoms of BD present to services requesting help is unclear. This highlights the need for further large scale population studies in this area.
Limitations of the evidence
Our review has highlighted a number of methodological factors that limit the interpretation of the findings and the comparison across studies. Retrospective studies are useful in highlighting features that may be significant. However, such studies are limited by the possibility that subjects actually met diagnostic criteria for BD at an earlier stage, and that the results may be significantly affected by recall biases. The more methodologically robust prospective studies have in the main recruited subjects from selected populations, limiting generalisability and comparison across studies. However, two prospective studies have recruited from general community samples (Angst et al. 2003; Tijssen et al. 2010a). A further issue is that some of the studies were of childhood onset BD and/or use a broad definition of BD- conclusions based on studies of childhood onset BD may not be applicable to adult onset BD, and vice versa. Differential diagnosis is controversial in childhood onset BD, but a more narrow definition of BD may be more appropriate (Baroni et al. 2009). Future studies comparing putatively prodromal symptoms in childhood and adult onset BD would help address this issue.
Specificity and sensitivity
Whilst the literature has identified a number of putatively prodromal features, it is striking that none of the studies reviewed provided both their specificity and sensitivity, and only two (one a relatively small retrospective study) gave sufficient data to allow these to be calculated. This highlights the need for future studies to include specificity and sensitivity. Where we were able to calculate these variables, our key finding was that while the specificity of many of the prodromal symptoms is high, their sensitivity is relatively low. However, the balance between the competing needs for specificity and sensitivity depends on the risks associated with false negative or false positive cases. In the case of the bipolar prodrome, high specificity may be useful if the risk of a false positive is considered substantial- in this case the risks are those associated with initiating treatments such as mood stabilizers in people who are unlikely to benefit from them. However, other potential interventions, such a psychoeducation or life-style advice, are likely to be associated with a lower risk of adverse events- in which case sensitivity may be considered relatively more important than specificity. Nevertheless the high specificity of some of the features indicates they may have potential to identify patients in the prodrome to BD.
Future directions
As no single prodromal feature has been identified in all subjects, the BD prodrome may be best defined by a cluster of features. One approach for future studies would be to evaluate which combination of the symptoms listed in table 4 provides the highest predictive accuracy for a subsequent diagnosis of BD.
An alternative strategy is to focus on other risk factors, such as family history or personality traits, possibly in combination with the putatively prodromal symptoms, as used in the criteria for the prodrome to psychosis (Yung et al. 2005). The high rate of BD spectrum disorders in people with cyclothymia suggests that this is a promising candidate risk feature to be included. The two approaches may be combined to complement each other. This combinatorial approach was used in the study (Akiskal et al. 1985) that showed the highest proportion of subjects that subsequently developed BD- suggesting that this approach might be most useful in clinical practice. Focusing on youths/young adults is likely to give the highest yield as this is the peak period for onset of BD- the risk of developing a first manic/hypomanic episode may decrease sharply after age 21 years old (Tijssen et al. 2010b).
Studies that included a psychiatric comparator group indicated that many of the putatively BD prodromal features may also be seen in other psychiatric disorders (Angst et al. 2003; Fergus et al. 2003; Rucklidge, 2008). One key outstanding question is thus whether the putative prodrome to BD can be reliably identified in a distinct, stable enough form to permit specific intervention, as appears to be the case in psychosis, or whether it is manifest as an ‘at risk mental state’ that gradually develops into one of a number of disorders, including BD. The specificity of putative BD prodromal features needs to be determined with respect to the prodrome of other psychiatric conditions, particularly schizophrenia and recurrent unipolar depression. Furthermore, the existence of childhood traits, such as cyclothymia, as well as the later development of frank symptoms suggests that there may be ‘early’ and ‘late’ prodromal features, as has been described for the prodrome of schizophrenia (Hambrecht et al. 2002).
Finally it is also evident from our review that there has been little investigation of the neurobiology of the BD prodromal phase, beyond a study of its relationship to alterations in sleep (Jones et al. 2005). Neurobiological markers may be used in people at risk on the basis of clinical features to enhance sensitivity and specificity of identifying the prodrome- an approach that has been tried in psychosis (McGuire et al. 2008).
Proposed model of the development of BD
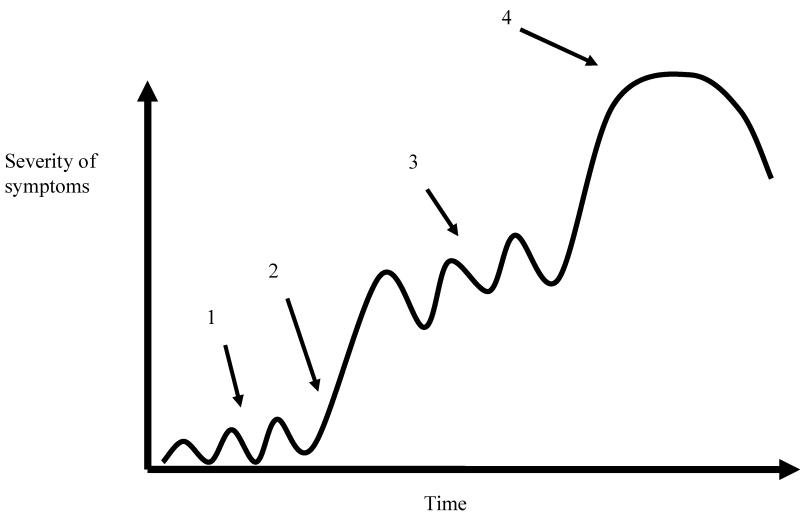
Overall our findings suggest key differences in the trajectory to BD from models of the prodrome to psychotic illnesses (Yung and McGorry, 1996). In particular, BD is a fluctuating condition, and, as shown in tables 3 and 4, many of the symptoms potentially predating it have a fluctuating nature. Moreover, the first manic episode may have been preceded by a major depressive episode, and the clinical picture may be further complicated by treatment for depression. This contrasts with psychotic illnesses such as schizophrenia, where the diagnosis can be made on the basis of the first episode of frank illness alone. The prodrome to BD is therefore harder to define than that to psychosis, as there may have been a prodrome to the first affective episode and residual symptoms from that episode. We have constructed an illustrative model (figure 1) that encapsulates features of the putative trajectory to BD based on our reading of the evidence in this review. This model is intended to highlight likely key aspects of the prodrome to BD that need to be considered by future studies. It is will undoubtedly need to be revised in the light of future evidence. The model has three components. Firstly features such as cyclothymic traits and/or manic/hypomanic symptoms may be apparent many years before the development of the frank illness (Fergus et al. 2003; Tijssen et al. 2010a), in a pre-prodromal phase (arrow 1). Secondly, over time, and possibly triggered by life events or other factors ((Mathew et al. 1994; Johnson et al. 2000) (arrow 2)), persisting and worsening symptoms become apparent that indicate a prodrome to BD (arrow 3) leading on to, thirdly, the first manic episode (arrow 4). Some patients will receive intervention for depression in the prodromal phase, although it may not be designed to prevent the later onset of BD and many BD patients do not receive intervention at this point (McIntyre and Konarski, 2004). The figure highlights that there are a number of potential points when preventive intervention could occur-primary intervention could be instituted during the period marked by arrow 1, and secondary prevention during the periods marked by arrows 2 and 3. Furthermore it is likely that intervention will need to be tailored to the phase- for example psychosocial interventions with proven benefit in BD (Sachs, 2008) could be beneficial in the pre-prodromal phase, whereas targeted cognitive behavioural therapy and/or medication may be used later once prodromal features are apparent.
Figure 1.
Model illustrating the possible development of bipolar disorder over time. Potential points for preventive intervention are identified by arrows 1, 2 and 3.
1= fluctuating mood representing underlying cyclothymia or at risk mental state
2= life events precipitating transition to
3= prodromal phase and
4= first manic episode
Conclusions
Symptoms predating the onset of BD have been identified in a number of studies, but further work is required to determine if these represent a distinct prodrome to BD. These putatively prodromal features can be grouped as attenuated symptoms of BD, general psychopathological features, and cyclothymic traits. The specificity and sensitivity of these features to the putative prodrome of BD remains to be established, and will require longitudinal studies that include appropriate psychiatric controls to determine whether a prodrome to BD can be reliably identified. We have proposed a model of the trajectory to BD based on our reading of the evidence reviewed to illustrate the points at which it may be possible to intervene clinically. However, further work is required before it will be possible to determine the full potential for early and preventive intervention for BD.
Supplementary Material
Footnotes
Declaration of interest: The authors have no conflicts of interest.
Declaration of interests: None.
Reference List
- Akiskal HS, Downs J, Jordan P, Watson S, Daugherty D, Pruitt DB. Affective disorders in referred children and younger siblings of manic-depressives. Mode of onset and prospective course. Archives of General Psychiatry. 1985;42:996–1003. doi: 10.1001/archpsyc.1985.01790330076009. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders DSM-IV-TR Fourth Edition. American Psychiatric Publishing Inc; Washington DC: 2000. [Google Scholar]
- Angst J, Gamma A, Endrass J. Risk factors for the bipolar and depression spectra. Acta Psychiatrica Scandinavica. 2003;418:15–19. doi: 10.1034/j.1600-0447.108.s418.4.x. [DOI] [PubMed] [Google Scholar]
- Baldessarini RJ, Tondo L, Hennen J. Treatment-latency and previous episodes: relationships to pretreatment morbidity and response to maintenance treatment in bipolar I and II disorders. Bipolar Disorders. 2003;5:169–179. doi: 10.1034/j.1399-5618.2003.00030.x. [DOI] [PubMed] [Google Scholar]
- Baldessarini RJ, Tondo L, Hennen J, Floris G. Latency and episodes before treatment: response to lithium maintenance in bipolar I and II disorders. Bipolar Disorders. 1999;1:91–97. doi: 10.1034/j.1399-5618.1999.010206.x. [DOI] [PubMed] [Google Scholar]
- Baroni A, Lunsford JR, Luckenbaugh DA, Towbin KE, Leibenluft E. Practitioner review: the assessment of bipolar disorder in children and adolescents. Journal of Child Psychology and Psychiatry. 2009;50:203–215. doi: 10.1111/j.1469-7610.2008.01953.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bauer M, Juckel G, Correll CU, Leopold K, Pfennig A. Diagnosis and treatment in the early illness phase of bipolar disorders. European Archives of Psychiatry and Clinical Neuroscience. 2008;258(Suppl 5):50–54. doi: 10.1007/s00406-008-5009-z. [DOI] [PubMed] [Google Scholar]
- Berk M, Dodd S, Callaly P, Berk L, Fitzgerald P, de Castella AR, Filia S, Filia K, Tahtalian S, Biffin F, Kelin K, Smith M, Montgomery W, Kulkarni J. History of illness prior to a diagnosis of bipolar disorder or schizoaffective disorder. Journal of Affective Disorders. 2007;103:181–186. doi: 10.1016/j.jad.2007.01.027. [DOI] [PubMed] [Google Scholar]
- Berk M, Malhi GS, Mitchell PB, Cahill CM, Carman, A C, Hadzi-Pavlovic D, Hawkins MT, Tohen M. Scale matters: the need for a Bipolar Depression Rating Scale (BDRS) Acta Psychiatrica Scandinavica. 2004;422:39–45. doi: 10.1111/j.1600-0447.2004.00412.x. [DOI] [PubMed] [Google Scholar]
- Blechert J, Meyer TD. Are measures of hypomanic personality, impulsive nonconformity and rigidity predictors of bipolar symptoms? British Journal of Clinical Psychology. 2005;44:15–27. doi: 10.1348/014466504X19758. [DOI] [PubMed] [Google Scholar]
- Calabrese JR, Muzina DJ, Kemp DE, Sachs GS, Frye MA, Thompson TR, Klingman D, Reed ML, Hirschfeld RM. Predictors of bipolar disorder risk among patients currently treated for major depression. Medscape General Medicine. 2006;8:38. [PMC free article] [PubMed] [Google Scholar]
- Conus P, Ward J, Hallam KT, Lucas N, Macneil C, McGorry PD, Berk M. The proximal prodrome to first episode mania--a new target for early intervention. Bipolar Disorders. 2008;10:555–565. doi: 10.1111/j.1399-5618.2008.00610.x. [DOI] [PubMed] [Google Scholar]
- Conus P, Ward J, Lucas N, Cotton S, Yung AR, Berk M, McGorry PD. Characterisation of the prodrome to a first episode of psychotic mania: Results of a retrospective study. Journal of Affective Disorders. 2010 doi: 10.1016/j.jad.2009.12.021. In press. (PMID: 20085850, Jan 18) [DOI] [PubMed] [Google Scholar]
- Correll CU, Penzner JB, Frederickson AM, Richter JJ, Auther AM, Smith CW, Kane JM, Cornblatt BA. Differentiation in the preonset phases of schizophrenia and mood disorders: evidence in support of a bipolar mania prodrome. Schizophrenia Bulletin. 2007;33:703–714. doi: 10.1093/schbul/sbm028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Egeland JA, Hostetter AM, Pauls DL, Sussex JN. Prodromal symptoms before onset of manic-depressive disorder suggested by first hospital admission histories. Journal of the American Academy of Child and Adolescent Psychiatry. 2000;39:1245–1252. doi: 10.1097/00004583-200010000-00011. [DOI] [PubMed] [Google Scholar]
- Fergus EL, Miller RB, Luckenbaugh DA, Leverich GS, Findling RL, Speer AM, Post RM. Is there progression from irritability/dyscontrol to major depressive and manic symptoms? A retrospective community survey of parents of bipolar children. Journal of Affective Disorders. 2003;77:71–78. doi: 10.1016/s0165-0327(02)00176-3. [DOI] [PubMed] [Google Scholar]
- Findling RL, Youngstrom EA, McNamara NK, Stansbrey RJ, Demeter CA, Bedoya D, Kahana SY, Calabrese JR. Early symptoms of mania and the role of parental risk. Bipolar Disorders. 2005;7:623–634. doi: 10.1111/j.1399-5618.2005.00260.x. [DOI] [PubMed] [Google Scholar]
- Franchini L, Zanardi R, Smeraldi E, Gasperini M. Early onset of lithium prophylaxis as a predictor of good long-term outcome. European Archives of Psychiatry and Clinical Neuroscience. 1999;249:227–230. doi: 10.1007/s004060050091. [DOI] [PubMed] [Google Scholar]
- Hambrecht M, Lammertink M, Klosterkotter J, Matuschek E, Pukrop R. Subjective and objective neuropsychological abnormalities in a psychosis prodrome clinic. British Journal of Psychiatry. 2002;43:s30–s37. doi: 10.1192/bjp.181.43.s30. [DOI] [PubMed] [Google Scholar]
- Henin A, Biederman J, Mick E, Hirshfeld-Becker DR, Sachs GS, Wu Y, Yan L, Ogutha J, Nierenberg AA. Childhood antecedent disorders to bipolar disorder in adults: a controlled study. Journal of Affective Disorders. 2007;99:51–57. doi: 10.1016/j.jad.2006.09.001. [DOI] [PubMed] [Google Scholar]
- Highet NJ, McNair BG, Thompson M, Davenport TA, Hickie IB. Experience with treatment services for people with bipolar disorder. Medical Journal of Australia. 2004;181:S47–S51. doi: 10.5694/j.1326-5377.2004.tb06353.x. [DOI] [PubMed] [Google Scholar]
- Johnson L, Andersson-Lundman G, berg-Wistedt A, Mathe AA. Age of onset in affective disorder: its correlation with hereditary and psychosocial factors. Journal of Affective Disorders. 2000;59:139–148. doi: 10.1016/s0165-0327(99)00146-9. [DOI] [PubMed] [Google Scholar]
- Jones SH, Hare DJ, Evershed K. Actigraphic assessment of circadian activity and sleep patterns in bipolar disorder. Bipolar Disorders. 2005;7:176–186. doi: 10.1111/j.1399-5618.2005.00187.x. [DOI] [PubMed] [Google Scholar]
- Jones SH, Tai S, Evershed K, Knowles R, Bentall R. Early detection of bipolar disorder: a pilot familial high-risk study of parents with bipolar disorder and their adolescent children. Bipolar Disorders. 2006;8:362–372. doi: 10.1111/j.1399-5618.2006.00329.x. [DOI] [PubMed] [Google Scholar]
- Kochman FJ, Hantouche EG, Ferrari P, Lancrenon S, Bayart D, Akiskal HS. Cyclothymic temperament as a prospective predictor of bipolarity and suicidality in children and adolescents with major depressive disorder. Journal of Affective Disorders. 2005;85:181–189. doi: 10.1016/j.jad.2003.09.009. [DOI] [PubMed] [Google Scholar]
- Kraepelin E. Manic-Depressive Insanity and Paranoia. Livingstone; Edinburgh: 1921. [Google Scholar]
- Lish JD, me-Meenan S, Whybrow PC, Price RA, Hirschfeld RM. The National Depressive and Manic-depressive Association (DMDA) survey of bipolar members. Journal of Affective Disorders. 1994;31:281–294. doi: 10.1016/0165-0327(94)90104-x. [DOI] [PubMed] [Google Scholar]
- Mathew MR, Chandrasekaran R, Sivakumar V. A study of life events in mania. Journal of Affective Disorders. 1994;32:157–161. doi: 10.1016/0165-0327(94)90013-2. [DOI] [PubMed] [Google Scholar]
- McGorry PD, Yung AR, Phillips LJ. The “close-in” or ultra high-risk model: a safe and effective strategy for research and clinical intervention in prepsychotic mental disorder. Schizophrenia Bulletin. 2003;29:771–790. doi: 10.1093/oxfordjournals.schbul.a007046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGuire P, Howes OD, Stone J, Fusar-Poli P. Functional neuroimaging in schizophrenia: diagnosis and drug discovery. Trends in Pharmacological Sciences. 2008;29:91–98. doi: 10.1016/j.tips.2007.11.005. [DOI] [PubMed] [Google Scholar]
- McIntyre RS, Konarski JZ. Bipolar disorder: a national health concern. CNS Spectrums. 2004;9:6–15. doi: 10.1017/s1092852900028844. [DOI] [PubMed] [Google Scholar]
- Mrazek D, Mrazek PJ. Prevention of psychiatric disorders in children and adolescents. In: Sadock BJ, Sadock VA, editors. Kaplan and Sadock’s comprehensive textbook of psychiatry. Lippincott Williams and Wilkins; New York: 2004. p. 3513. [Google Scholar]
- Rucklidge JJ. Retrospective parent report of psychiatric histories: do checklists reveal specific prodromal indicators for postpubertal-onset pediatric bipolar disorder? Bipolar Disorders. 2008;10:56–66. doi: 10.1111/j.1399-5618.2008.00533.x. [DOI] [PubMed] [Google Scholar]
- Sachs GS. Psychosocial interventions as adjunctive therapy for bipolar disorder. Journal of Psychiatric Practice. 2008;14(Suppl 2):39–44. doi: 10.1097/01.pra.0000320125.99423.b7. [DOI] [PubMed] [Google Scholar]
- Shaw JA, Egeland JA, Endicott J, Allen CR, Hostetter AM. A 10-year prospective study of prodromal patterns for bipolar disorder among Amish youth. Journal of the American Academy of Child and Adolescent Psychiatry. 2005;44:1104–1111. doi: 10.1097/01.chi.0000177052.26476.e5. [DOI] [PubMed] [Google Scholar]
- Swann AC, Bowden CL, Calabrese JR, Dilsaver SC, Morris DD. Differential effect of number of previous episodes of affective disorder on response to lithium or divalproex in acute mania. American Journal of Psychiatry. 1999;156:1264–1266. doi: 10.1176/ajp.156.8.1264. [DOI] [PubMed] [Google Scholar]
- Tijssen MJ, van OJ, Wittchen HU, Lieb R, Beesdo K, Mengelers R, Krabbendam L, Wichers M. Evidence that bipolar disorder is the poor outcome fraction of a common developmental phenotype: an 8-year cohort study in young people. Psychological Medicine. 2010a;40:289–299. doi: 10.1017/S0033291709006138. [DOI] [PubMed] [Google Scholar]
- Tijssen MJ, van OJ, Wittchen HU, Lieb R, Beesdo K, Mengelers R, Wichers M. Prediction of transition from common adolescent bipolar experiences to bipolar disorder: 10-year study. British Journal of Psychiatry. 2010b;196:102–108. doi: 10.1192/bjp.bp.109.065763. [DOI] [PubMed] [Google Scholar]
- Yung AR, McGorry PD. The prodromal phase of first-episode psychosis: past and current conceptualizations. Schizophrenia Bulletin. 1996;22:353–370. doi: 10.1093/schbul/22.2.353. [DOI] [PubMed] [Google Scholar]
- Yung AR, Yuen HP, McGorry PD, Phillips LJ, Kelly D, Dell’Olio M, Francey SM, Cosgrave EM, Killackey E, Stanford C, Godfrey K, Buckby J. Mapping the onset of psychosis: the Comprehensive Assessment of At-Risk Mental States. Australian and New Zealand Journal of Psychiatry. 2005;39:964–971. doi: 10.1080/j.1440-1614.2005.01714.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.