Abstract
OBJECTIVE
To evaluate the usefulness of a fasting plasma glucose (FPG) at 24–28 weeks’ gestation to screen for gestational diabetes mellitus (GDM).
RESEARCH DESIGN AND METHODS
The medical records and results of a 75-g 2-h oral glucose tolerance test (OGTT) of 24,854 pregnant women without known pre-GDM attending prenatal clinics in 15 hospitals in China were examined.
RESULTS
FPG cutoff value of 5.1 mmol/L identified 3,149 (12.1%) pregnant women with GDM. FPG cutoff value of 4.4 mmol/L ruled out GDM in 15,369 (38.2%) women. With use of this cutoff point, 12.2% of patients with mild GDM will be missed. The positive predictive value is 0.322, and the negative predictive value is 0.928.
CONCLUSIONS
FPG at 24–28 weeks’ gestation could be used as a screening test to identify GDM patients in low-resource regions. Women with an FPG between ≥4.4 and ≤5.0 mmol/L would require a 75-g OGTT to diagnose GDM. This would help to avoid approximately one-half (50.3%) of the formal 75-g OGTTs in China.
In 2011, the Ministry of Health (MOH) in China published the diagnostic criteria for gestational diabetes mellitus (GDM) based on a 75-g oral glucose tolerance test (OGTT) carried out between 24 and 28 weeks’ gestation (1). As a formal glucose tolerance test may be difficult to implement in low-resource rural areas in China, the MOH sought to assess whether a fasting plasma glucose (FPG) could be used as a screening tool to reduce the number of OGTTs required. The following cut points were suggested: if FPG ≥5.1 mmol/L, GDM can be diagnosed immediately; if FPG <4.4 mmol/L, GDM can be considered unlikely. Thus, the 75-g OGTT only needs to be performed for women with FPG values ≥4.4 mmol/L and <5.1 mmol/L. As there was no scientific evidence from China to support this approach, we conducted this study to test the hypothesis.
RESEARCH DESIGN AND METHODS
During the past year, multiprofessional teams from 15 hospitals in different provinces of China were trained in screening, diagnosing, and providing care for women with GDM and to implement the new diagnostic standard (one-step approach). Pregnant women with previously known diabetes were excluded. Over a 10-month period, between 1 May 2011 and 29 February 2012, 24,854 pregnant women registered at the participating hospitals underwent a 75-g OGTT between 24 and 28 weeks of gestation. Venous plasma glucose values at 0, 1, and 2 h after a 75-g glucose load were recorded and analyzed. A diagnosis of GDM was made when any one of the following values was met or exceeded in the 75-g OGTT: 0 h (fasting), 5.1 mmol/L; 1 h, 10.0 mmol/L; and 2 h, 8.5 mmol/L, as per the guidelines of MOH in China. With use of the Predictive Analysis Software Statistics 18.0, performance of the FPG value to screen for GDM was analyzed based on the receiver operating characteristic (ROC) curve.
RESULTS
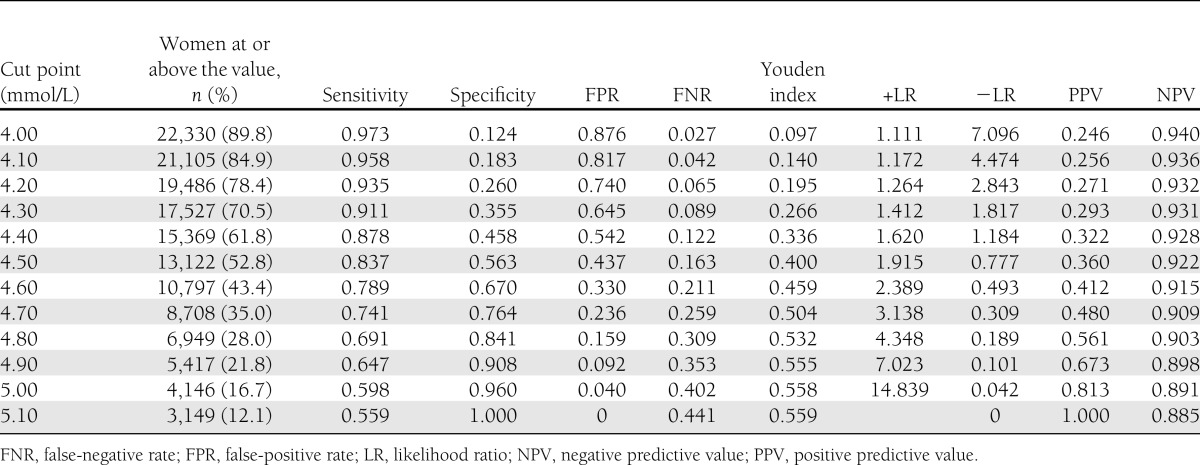
ROC curves to test the value of FPG at 24–28 weeks to diagnose GDM were created. The area under the ROC curve was 0.836 (95% CI 0.829–0.843), SE 0.004, P < 0.001. At 24–28 weeks, GDM diagnosis rate increased with rising FPG value, and at values >5.1 mmol/L all women with GDM (12.1%) were identified. As shown in Table 1, at the cut point 4.4 mmol/L, 87.8% of GDM women were diagnosed with specificity of 0.458 and predictive positive value and negative predictive value in the rational range. If 4.4 mmol/L were made the cut point to decide who should have the 75-g OGTT, then 50.3% (38.2% with values <4.4 mmol/L plus 12.1% with value >5.1 mmol/L) of pregnant women could avoid the 75-g OGTT with the probability that 12.2% of patients with GDM may be missed. The percentage missed would be 16.3% with 4.5 mmol/L or 8.9% with 4.3 mmol/L as the cut point.
Table 1.
FPG cutoff values of GDM diagnosis by MOH criteria
CONCLUSIONS
GDM is one of the common medical conditions associated with pregnancy with potentially serious health consequences for mother and offspring both in the short and long term (2–7). To address the problem, the MOH in China established guidelines and one-step diagnostic criteria for GDM based on the 75-g OGTT done at 24–28 weeks of gestation. Many poorly resourced facilities in China, particularly in small towns and rural areas, are unable to implement these guidelines. Therefore, a simple screening test and protocol to identify women who might need the 75-g OGTT would be extremely useful.
Our study shows that FPG value at 24–28 weeks’ gestation can help decide whether the 75-g OGTT is needed. In Chinese women with FPG value ≥5.1 mmol/L, one can make the diagnosis of GDM (specificity 100%) and, in those with value ≤4.4 mmol/L one can rule out GDM (87.8% sensitivity). These results are similar to those reported by Agarwal et al. (8) in the Hyperglycemia and Adverse Pregnancy Outcome (HAPO) cohort. In the HAPO study, risks of some adverse outcomes were low when FPG was 4.4 mmol/L (9). Considering these and efficiency, we conclude that FPG value of 4.4 mmol/L should be used as the optimal cut point. Women with FPG values between 4.4 and 5.1 mmol/L require a 75-g 2-h OGTT to confirm or rule out GDM. This strategy will reduce the number of OGTTs by about half (50.3%). These data are from China, and the results may only be applicable to a Chinese population, although the United Arab Emirates population studies also suggest the same cutoff points (10).
Acknowledgments
The authors thank the World Diabetes Foundation for funding the GDM project (project no. WDF10-517), which enabled data collection, monitoring, and analysis.
No potential conflicts of interest relevant to this article were reported.
W.-w.Z. searched the literature, collected and analyzed data, and drafted the report. L.F., L.-y.K., S.-p.S., Z.-l.W., Y.-l.H., M.-h.Z., L.-Z.S., Y.M., X.-p.D., H.Z., Y.-h.W., Y.-p.H., L.-r.Z., H.-r.W., N.L., and Y.-f.W. collected medical data. H.-x.Y. designed the study, contributed to discussion, and reviewed and edited the manuscript. A.K. contributed to discussion and edited the manuscript. H.-x.Y. is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
The National GDM Collaboration Research Group and Chinese Society of Perinatal Medicine assisted in implementation of the survey.
References
- 1.Yang HX, Medical Service Specialty Standard Committee of Ministry of Health Diagnostic criteria for gestational diabetes mellitus (WS 331-2011). Chin Med J (Engl) 2012;125:1212–1213 [PubMed] [Google Scholar]
- 2.Ferrara A, Weiss NS, Hedderson MM, et al. Pregnancy plasma glucose levels exceeding the American Diabetes Association thresholds, but below the National Diabetes Data Group thresholds for gestational diabetes mellitus, are related to the risk of neonatal macrosomia, hypoglycaemia, and hyperbilirubinaemia. Diabetologia 2007;50:298–306 [DOI] [PubMed] [Google Scholar]
- 3.McIntyre HD, Chang AM, Callaway LK, et al. Hyperglycemia and Adverse Pregnancy Outcome (HAPO) Study Cooperative Research Group Hormonal and metabolic factors associated with variations in insulin sensitivity in human pregnancy. Diabetes Care 2010;33:356–360 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Getahun D, Fassett MJ, Jacobsen SJ. Gestational diabetes: risk of recurrence in subsequent pregnancies. Am J Obstet Gynecol 2010;203:467.e1–467.e6 [DOI] [PubMed]
- 5.O’Sullivan JB. Body weight and subsequent diabetes mellitus. JAMA 1982;248:949–952 [PubMed] [Google Scholar]
- 6.Bellamy L, Casas JP, Hingorani AD, Williams D. Type 2 diabetes mellitus after gestational diabetes: a systematic review and meta-analysis. Lancet 2009;373:1773–1779 [DOI] [PubMed] [Google Scholar]
- 7.Chodick G, Elchalal U, Sella T, et al. The risk of overt diabetes mellitus among women with gestational diabetes: a population-based study. Diabet Med 2010;27:779–785 [DOI] [PubMed] [Google Scholar]
- 8.Agarwal MM, Weigl B, Hod M. Gestational diabetes screening: the low-cost algorithm. Int J Gynaecol Obstet 2011;115(Suppl. 1):S30–S33 [DOI] [PubMed] [Google Scholar]
- 9.Metzger BE, Gabbe SG, Persson B, et al. International Association of Diabetes and Pregnancy Study Groups Consensus Panel International association of diabetes and pregnancy study groups recommendations on the diagnosis and classification of hyperglycemia in pregnancy. Diabetes Care 2010;33:676–682 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Agarwal MM, Dhatt GS, Shah SM. Gestational diabetes mellitus: simplifying the international association of diabetes and pregnancy diagnostic algorithm using fasting plasma glucose. Diabetes Care 2010;33:2018–2020 [DOI] [PMC free article] [PubMed] [Google Scholar]


