Diabetic foot ulceration (DFU) is a serious and prevalent complication of diabetes, ultimately affecting some 25% of those living with the disease (1). DFUs have a consistently negative impact on quality of life and productivity as diabetic patients report stigma, social isolation, unemployment, and depression (2–5). Patients with DFUs also have morbidity and mortality rates equivalent to aggressive forms of cancer (2). These ulcers remain an important risk factor for lower-extremity amputation as up to 85% of amputations are preceded by foot ulcers (6). It should therefore come as no surprise that some 33% of the $116 billion in direct costs generated by the treatment of diabetes and its complications was linked to the treatment of foot ulcers (7). Another study has suggested that 25–50% of the costs related to inpatient diabetes care may be directly related to DFUs (2).
National standards have been developed for DFU prevention and care (8–10). Given the high prevalence, severity, costs, and morbidity of diabetic foot complications, one would expect that federal funding for DFU research would be proportionate to its public health impact. The National Institutes of Health (NIH) is the major source of federal funding for medical research in the U.S. We therefore examined NIH funding for both diabetes and DFUs using the NIH Research Portfolio Online Reporting Tools (RePORT) from 2002 to 2011 (11). We also examined differences in the number of peer-reviewed publications (using PubMed at www.ncbi.nlm.nih.gov) on both diabetes and diabetic foot ulcers between the years 1980–2010. The search terms included “diabetes,” “diabetic foot ulcers” and the following search string: [diabetic AND (foot OR feet OR toes) AND (wound OR ulcer)]. We used a similar strategy to that of our colleagues Meador et al. (12) and Sen et al. (13), who evaluated disparities between epilepsy research and wound healing.
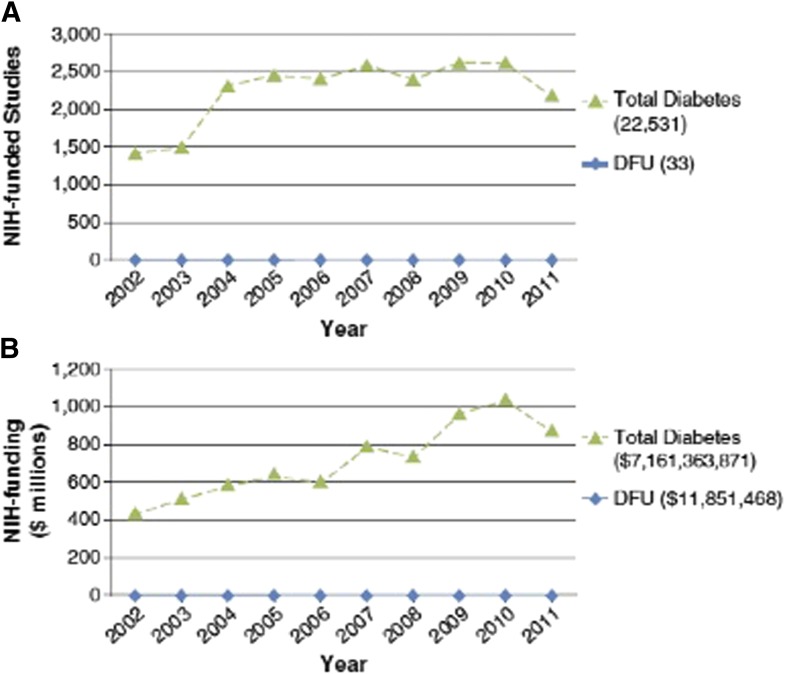
The number of peer-reviewed DFU publications increased 78% between the periods of 1980–1989 to 2000–2009. This was similar to the number of total diabetes publications, which increased 72% over the same period (Table 1). The similarities, however, appear to end there. We identified 22,531 NIH-funded projects in diabetes between 2002–2011. Remarkably, of these, only 33 (0.15%) were specific to DFUs. Likewise, these 22,531 NIH-funded projects yielded $7,161,363,871 in overall diabetes funding, and of this, only $11,851,468 (0.17%) was specific to DFUs. Thus, a 604-fold difference exists between overall diabetes funding and that allocated to DFUs. These data are outlined in Fig. 1.
Table 1.
Comparison of peer-reviewed publications on diabetes vs. DFUs
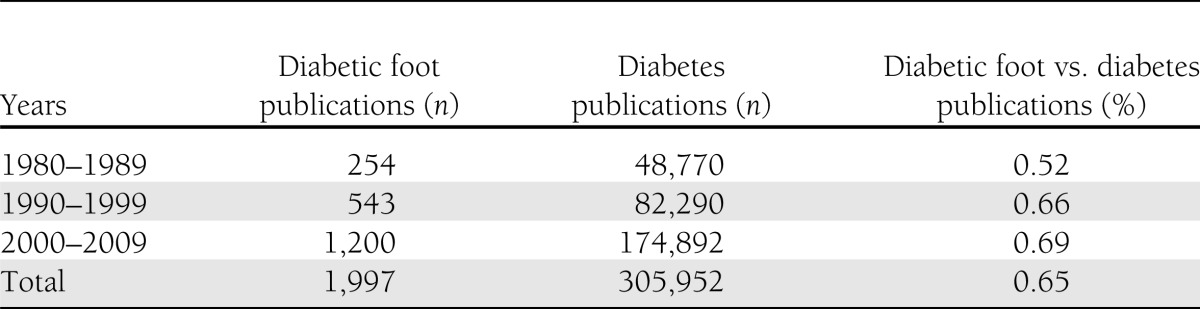
Figure 1.
Comparison of NIH funding for diabetes and DFUs between 2002 and 2011. A: Total number of NIH-funded studies per year for diabetes, diabetic neuropathy, and DFUs. Total number of studies in each group is shown in parentheses. The proportion of diabetes funding allocated to DFUs as a function of total NIH diabetes studies is 0.0015. B: Total NIH funding (in millions) allocated per year for diabetes and DFUs. Sum total for each category between 2002 and 2001 is shown in parentheses. The proportion of diabetes funding allocated to DFUs as a function of total NIH diabetes funding is 0.0017.
As DFUs are prevalent and have a negative impact on the quality of life of patients with diabetes, it would stand to reason that U.S. federal funding specifically for DFUs would be proportionate with this burden. Unfortunately, this yawning gap in funding (and commensurate development of a culture of subspecialty research) stands in stark contrast to the outsized influence of DFUs on resource utilization within diabetes care.
This disparity does not appear to be isolated to one developed nation. Indeed, in the U.K., 89 out of 402 diabetes-related grant applications received by Diabetes UK were funded between 2010 and 2011 (direct request for information, Diabetes UK, 2012). Further, of these 402 U.K. grant applications, only 15 were specific to the diabetic foot. Of these, only one grant application specific to the diabetic foot was funded, accounting for a mere 1.7% of the total Diabetes UK funding during that time period.
Over the past generation, the number of peer-reviewed publications on DFUs has increased fivefold (Table 1). These data are similar to those reported by Boulton (6), who reported that 2.7% of all diabetes publications listed on PubMed were specific to the diabetic foot from 1998 to 2004 compared with 0.7% during the 1980–1998 time period, yielding a fourfold increase. This increase tracks well with the interest level of clinician-scientists treating the disease.
Why, then, is the gap between the impact of DFUs on the diabetic condition and DFU funding so expansive? Chronic wounds, as a whole, affect nearly 6.5 million patients in the U.S. alone, accounting for approximately $25 billion in expenditures (13). One could postulate that grants submitted to the NIH on diabetic foot disease were of poor quality and therefore the majority were not funded: This explanation, however, appears to be unlikely as the number of original publications on diabetic foot disease in the peer-reviewed literature has substantially increased in recent years with many articles appearing in high–impact factor journals. An alternative explanation—and a more pragmatic one—might be that mentors specializing in diabetes are advising young physician-scientists against pursuing DFU research because of a lack of opportunity for funding and career advancement. Clearly, the gap between prevalence and funding could have serious consequences for future patient care and research.
It is worth reemphasizing that DFUs are a frequent and costly complication of diabetes. The cumulative lifetime incidence of foot ulcers in diabetic patients may be as high as 25% (14). According to estimates, nearly $9,000,000,000 were spent on DFU treatment in 2001 alone (13). Between 2005 and 2007, the total incidence of diabetes increased 13.5% (13). From a worldwide perspective, as we face an increasing incidence of type 1 diabetes and an epidemic of type 2 diabetes, the prevalence of diabetic foot ulcers will only rise. The cost of care of people with diabetic foot ulcers is 5.4 times higher in the year after the first ulcer episode than the cost of care of people with diabetes without foot ulcers (10).
Neuropathy and ischemia are the primary underlying risk factors for DFU development (15). Patients with DFUs and concomitant ischemic and neuroischemic disease have worse outcomes. Indeed, amputation and mortality rates are higher in patients with ischemic and neuroischemic ulcers than in patients with neuropathic ulcers (7,16). Patients with ischemic ulcers also show a higher rate of recurrence, nearly twice as many amputations, and inferior maintenance of ambulation and independence than patients with neuropathic foot ulcers (17). The prevalence of neuroischemic DFUs has been rising since the 1990s from approximately 33% of patients to where it now appears to be the most common etiology of foot ulcers (compared with purely neuropathic wounds) (18,19). Remarkably, no U.S. Food and Drug Administration–approved products or medical devices for patients with neuroischemic diabetic foot ulcers are currently available as these patients are frequently excluded from clinical study programs.
As we highlight in this article, there is a lack of federally and not for profit–funded research directed toward diabetic foot ulcers. This funding gap is disproportionately large in comparison with the public health impact of this sequela. As a diabetes-related extremity amputation is now performed every 20 s (20), we see a clear and present medical and fiscal calamity. We must mind this gap as a locomotive of lower-extremity complications is approaching our station and is anything but stationary.
Acknowledgments
No potential conflicts of interest relevant to this article were reported.
References
- 1.Singh N, Armstrong DG, Lipsky BA. Preventing foot ulcers in patients with diabetes. JAMA 2005;293:217–228 [DOI] [PubMed] [Google Scholar]
- 2.Kantor J, Margolis DJ. Treatment options for diabetic neuropathic foot ulcers: a cost-effectiveness analysis. Dermatol Surg 2001;27:347–351 [DOI] [PubMed] [Google Scholar]
- 3.Winkley K, Stahl D, Chalder T, Edmonds ME, Ismail K. Risk factors associated with adverse outcomes in a population-based prospective cohort study of people with their first diabetic foot ulcer. J Diabetes Complications 2007;21:341–349 [DOI] [PubMed] [Google Scholar]
- 4.Moulik PK, Mtonga R, Gill GV. Amputation and mortality in new-onset diabetic foot ulcers stratified by etiology. Diabetes Care 2003;26:491–494 [DOI] [PubMed] [Google Scholar]
- 5.Morbach S, Furchert H, Gröblinghoff U, et al. Long-term prognosis of diabetic foot patients and their limbs: amputation and death over the course of a decade. Diabetes Care 2012;35:2021–2027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Boulton AJ. The diabetic foot: from art to science. The 18th Camillo Golgi lecture. Diabetologia 2004;47:1343–1353 [DOI] [PubMed] [Google Scholar]
- 7.Driver VR, Fabbi M, Lavery LA, Gibbons G. The costs of diabetic foot: the economic case for the limb salvage team. J Am Podiatr Med Assoc 2010;100:335–341 [DOI] [PubMed] [Google Scholar]
- 8.Boulton AJ, Armstrong DG, Albert SF, et al. American Diabetes Association. American Association of Clinical Endocrinologists Comprehensive foot examination and risk assessment: a report of the Task Force of the Foot Care Interest Group of the American Diabetes Association, with endorsement by the American Association of Clinical Endocrinologists. Diabetes Care 2008;31:1679–1685 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.U.S. Department of Health and Human Services. HealthyPeople.gov: 2020 topics and objectives [Internet], 2012. Available from http://www.healthypeople.gov/2020/topicsobjectives2020/objectiveslist.aspx?topicid=8 Accessed 8 December 2012
- 10.Tan T, Shaw EJ, Siddiqui F, Kandaswamy P, Barry PW, Baker M, Guideline Development Group Inpatient management of diabetic foot problems: summary of NICE guidance. BMJ 2011;342:d1280. [DOI] [PubMed] [Google Scholar]
- 11.National Institutes of Health. NIH Research Portfolio Online Reporting Tool (RePORT) [Internet], 2012. Available from http://report.nih.gov/ U.S. Department of Health and Human Services. Accessed 21 November 2012
- 12.Meador KJ, French J, Loring DW, Pennell PB. Disparities in NIH funding for epilepsy research. Neurology 2011;77:1305–1307 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sen CK, Gordillo GM, Roy S, et al. Human skin wounds: a major and snowballing threat to public health and the economy. Wound Repair Regen 2009;17:763–771 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cavanagh PR, Lipsky BA, Bradbury AW, Botek G. Treatment for diabetic foot ulcers. Lancet 2005;366:1725–1735 [DOI] [PubMed] [Google Scholar]
- 15.Laing P. The development and complications of diabetic foot ulcers. Am J Surg 1998;176(2A Suppl.):11S–19S [DOI] [PubMed]
- 16.Margolis DJ, Malay DS, Hoffstad OJ, et al. Prevalence of diabetes, diabetic foot ulcer, and lower extremity amputation among Medicare beneficiaries, 2006 to 2008. Data Points #1. Agency for Healthcare Research and Quality. Rockville, MD, Data Points Publication Series, 2011 [PubMed] [Google Scholar]
- 17.Prompers L, Schaper N, Apelqvist J, et al. Prediction of outcome in individuals with diabetic foot ulcers: focus on the differences between individuals with and without peripheral arterial disease. The EURODIALE Study. Diabetologia 2008;51:747–755 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Yost ML. Diabetic foot ulcers, peripheral artery disease and critical limb ischemia. Atlanta, GA, The Sage Group, 2011
- 19.Armstrong DG, Cohen K, Courric S, Bharara M, Marston W. Diabetic foot ulcers and vascular insufficiency: our population has changed, but our methods have not. J Diabetes Sci Tech 2011;5:1591–1595 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.International Diabetes Federation, International Working Group on the Diabetic Foot. Diabetes and foot care: time to act. Brussels, International Diabetes Federation, 2005 [Google Scholar]