Abstract
OBJECTIVE
Recent study has suggested that not only the presence of hypertension but also the variability in systolic blood pressure (SBP) are risk factors for vascular disease and organ damage. The aim of this study was to investigate the relationship between visit-to-visit variability in SBP and change in urinary albumin excretion (UAE) or development of albuminuria in patients with type 2 diabetes.
RESEARCH DESIGN AND METHODS
We measured SBP in 354 consecutive patients at every visit during 1 year and calculated the coefficient of variation (CV) of SBP. We performed a follow-up study to assess change in UAE or development of albuminuria, the mean interval of which was 3.76 ± 0.71 years. Then, we evaluated relationships of variability of SBP to diabetic nephropathy using multiple regression analysis and multiple Cox regression model.
RESULTS
Multiple regression analysis demonstrated that CV of SBP was independently associated with change in UAE (β = 0.1758; P = 0.0108). Adjusted Cox regression analyses demonstrated that CV of SBP was associated with an increased hazard of development of albuminuria; hazard ratio was 1.143 (95% CI 1.008–1.302).
CONCLUSIONS
Visit-to-visit variability in SBP could be a novel risk factor for the development and progression of diabetic nephropathy in patients with type 2 diabetes.
Cardiovascular disease (CVD) is the primary cause of mortality and morbidity in patients with type 2 diabetes, and several risk factors including smoking, hypertension, and dyslipidemia have been shown to accelerate the progression of CVD (1,2). Elevated albumin excretion rate, which is a useful marker for diabetic nephropathy, has been reported to be associated with increased risk of cardiovascular mortality and the progression of CVD (3,4). The presence of hypertension and the variability in blood pressure are strong predictors of all mortality (5), CVD (6–8), and organ damage such as chronic kidney disease (9). However, there is a recent study that does not favor a prognostic role of variability in blood pressure. Mancia et al. (10) reported that in patients with mild-to-moderate hypertension, carotid intima-media thickness and cardiovascular outcomes were not related to on-treatment visit-to-visit clinic or 24-h blood pressure variability. A recent study suggested that visit-to-visit variability in blood pressure was associated with the development of diabetic nephropathy in patients with type 1 diabetes (9). Also, we recently reported that visit-to-visit variability in systolic blood pressure (SBP) is correlated with albuminuria in a cross-sectional study (11). However, a relationship between visit-to-visit variability in blood pressure and the progression or development of diabetic nephropathy in patients with type 2 diabetes has not been investigated. Therefore, we evaluated the relationship between visit-to-visit variability in SBP and change in the urinary albumin excretion (UAE) or the development of albuminuria in patients with type 2 diabetes.
RESEARCH DESIGN AND METHODS
Patients and study design
We performed a retrospective cohort study in 354 participants recruited from the outpatient clinic at the Kyoto Prefectural University of Medicine from April 2008 to September 2012. Type 2 diabetes was diagnosed according to the Report of the Expert Committee on the Diagnosis and Classification of Diabetes Mellitus (12). BMI was calculated as weight in kilograms divided by height in meters squared. Patients were classified as nonsmokers, past smokers, or current smokers according to a self-administered questionnaire. Nephropathy was graded as follows: normoalbuminuria, UAE <30 mg/g creatinine (Cr); microalbuminuria, 30–300 mg/g Cr; or macroalbuminuria, >300 mg/g Cr. Patients with advanced renal dysfunction (serum Cr >2.0 mg/dL) or malignancy, patients with major cardiovascular event or newly prescribed ACE inhibitor or angiotensin II receptor blocker during follow-up, and patients with any changes of medication for hypertension during 1 year of blood pressure data collection were excluded from this study. We then evaluated relationships of variability in blood pressure to change in UAE in all patients and calculated the hazard ratio for development of albuminuria in patients with normoalbuminuria. This study was approved by the local research ethics committee and was conducted in accordance with Declaration of Helsinki; informed consent was obtained from all participants.
Measurement of blood pressure and data collection
We measured blood pressure at every visit during 1 year and calculated the visit-to-visit variability in blood pressure. After collection of blood pressure data, blood and urine samples were collected as baseline data. As a follow-up study, we collected urine samples for calculation of UAE at the end of the follow-up.
Sitting blood pressure was measured twice after a 5-min rest at every visit during 1 year in quiet space using a device (HEM-906: OMRON) that automatically measures blood pressure, and the reference was an average of two values. The visit-to-visit variability in blood pressure was calculated as follows: coefficient of variation (CV) = SD/average blood pressure × 100.
Blood samples were taken in the morning at baseline. Serum total cholesterol and triglyceride concentrations were assessed using standard enzymatic methods. Hemoglobin A1c was assayed using high-performance liquid chromatography and expressed with the unit defined by the National Glycohemoglobin Standardization Program. Urinary albumin and Cr concentrations were determined from an early morning spot urine collection. The UAE was measured with an immunoturbidimetric assay. A mean value for UAE was determined from three urine collections. Change in UAE was calculated as follows: change in UAE = increase of UAE/follow-up duration (year). Development of albuminuria was defined as UAE ≥30 mg/g Cr.
Statistical analysis
Means and frequencies of potential confounding variables were calculated. Because triglycerides showed skewed distributions, log transformation was performed before performing correlation and regression analysis. The relationships between visit-to-visit variability in SBP and change in UAE as well as the relationships between visit-to-visit variability in SBP and age or other variables were examined by Pearson correlation analyses. To examine the effects of various factors on change in UAE or development of albuminuria defined as UAE ≥30 mg/g Cr, the following factors were considered simultaneously as independent variables for multiple regression analysis: age, sex, duration of diabetes, BMI, average SBP, CV of SBP, hemoglobin A1c, total cholesterol, logarithm of triglyceride, uric acid, smoking status, antihypertensive drug, and statin. For multiple Cox regression model, the following factors were considered simultaneously as independent variables: age, sex, duration of diabetes, BMI, average SBP, CV of SBP, hemoglobin A1c, total cholesterol, logarithm of triglyceride, uric acid, baseline UAE, smoking status, antihypertensive drug, and statin. All continuous variables are presented as the mean ± SD or absolute number. P < 0.05 was considered statistically significant. The size, direction, and statistical significance of relationships were estimated by the hazard ratio with 95% CI.
RESULTS
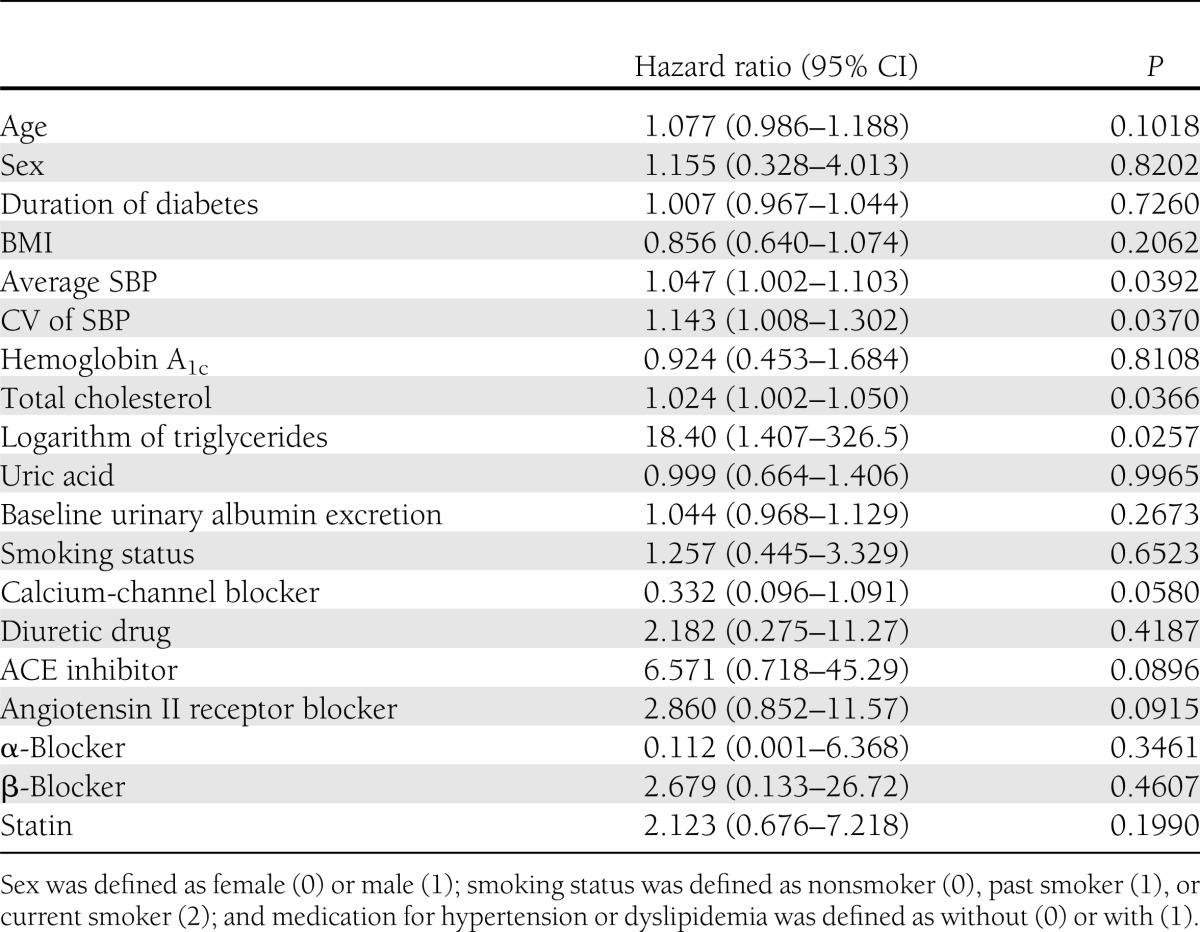
Characteristics of the 354 patients with type 2 diabetes enrolled in this study are shown in Table 1. Mean CV of SBP was 8.0 ± 4.0%. The average duration of follow-up was 3.76 ± 0.71 years. The average number of measurements per subject during the year of blood pressure data collection was 7.19 ± 2.02. The average interval of blood pressure measurements was 1.67 ± 0.47 months, and they were regularly spaced. Change in UAE was 16.1 ± 28.7 mg/g Cr. There were 218 patients (61.6%) with normoalbuminuria at baseline. During the study period, 28 patients had development of albuminuria. The CV of SBP positively correlated with age (r = 0.3042; P ≤ 0.0001), duration of diabetes (r = 0.2085; P = 0.0001), or change in UAE (r = 0.1447; P = 0.0085), and negatively correlated with BMI (r = −0.1239; P = 0.0215). No significant correlations were found between CV of SBP and average SBP, hemoglobin A1c, total cholesterol, logarithm of triglycerides, or uric acid. Multiple regression analyses of change in UAE are shown in Table 2. Multiple regression analysis demonstrated that the average of SBP (β = 0.2167; P = 0.0023) or CV of SBP (β = 0.1758; P = 0.0108) was independently associated with change in UAE. Adjusted Cox regression analyses demonstrated that average SBP, CV of SBP, total cholesterol, or logarithm of triglycerides were associated with an increased hazard of development of albuminuria; hazard ratios of those were 1.047 (95% CI 1.002–1.103), 1.143 (1.008–1.302), 1.024 (1.002–1.050), or 18.40 (1.407–326.5), respectively (Table 3).
Table 1.
Characteristics of patients
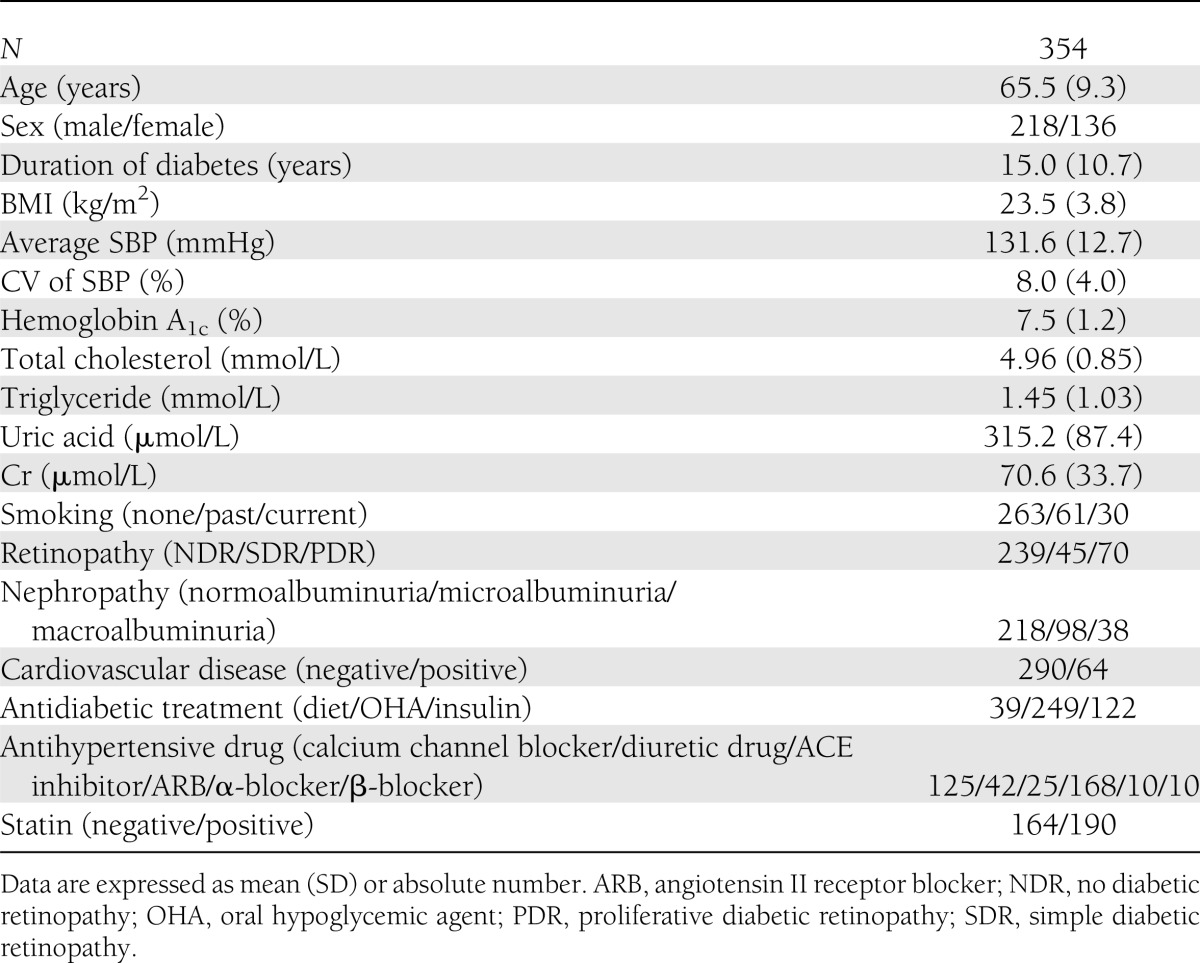
Table 2.
Simple correlation and multiple regression analyses on change in urinary albumin excretion
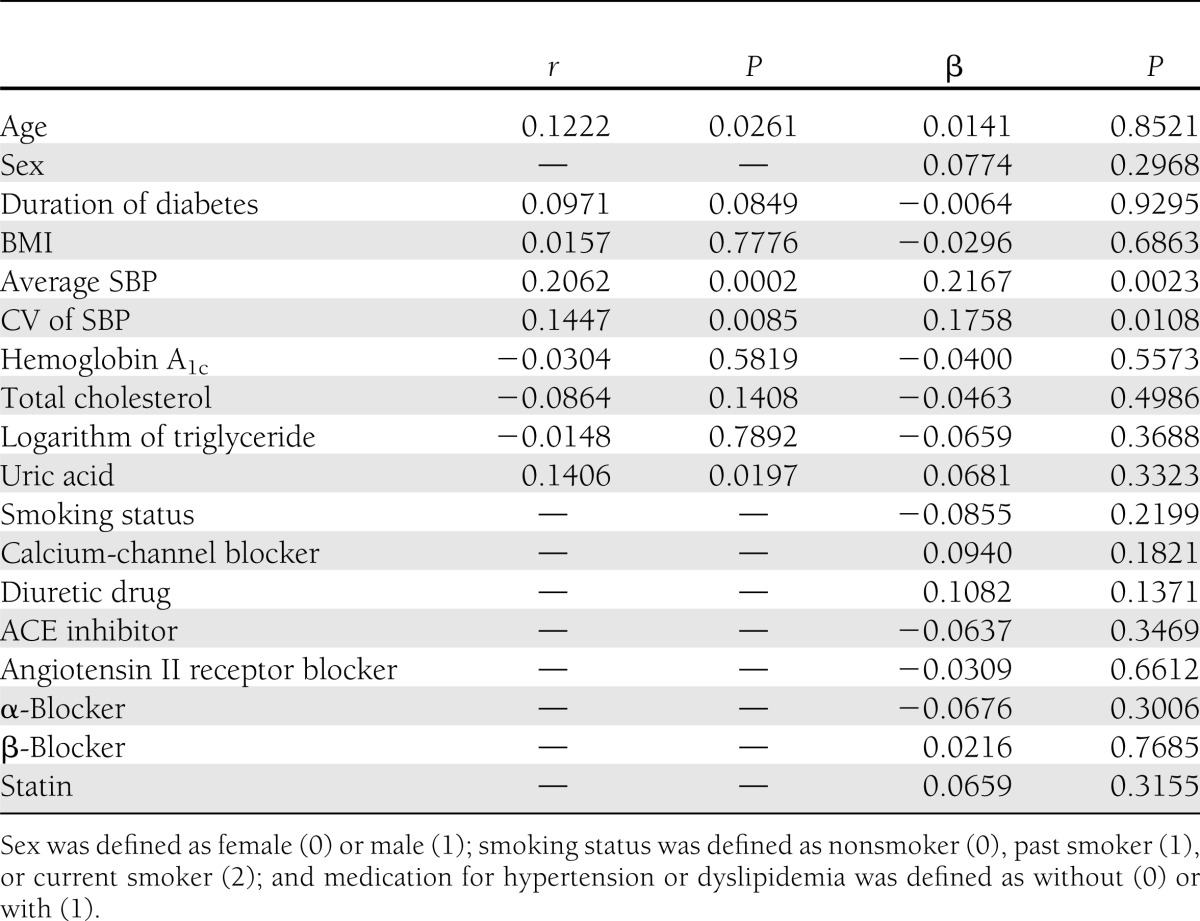
Table 3.
Multivariate adjusted hazard ratios for development of albuminuria
CONCLUSIONS
The major finding of our study is that visit-to-visit variability in SBP is a risk factor for progression of UAE or development of albuminuria.
Recent studies have suggested that an increased visit-to-visit variability in blood pressure was a risk factor for cerebrovascular events (7), myocardial infarction (8), and all mortality (5) independently of average blood pressure. Kilpatrick et al. (9) have reported that visit-to-visit variability in blood pressure consistently and independently added to mean blood pressure in predicting the risk of diabetic nephropathy, but not retinopathy, in the Diabetes Control and Complications Trial, which was a 9-year follow-up study of 1,441 participants with type 1 diabetes. Recently, we reported a cross-sectional study of relationship between visit-to-visit variability in SBP and diabetic nephropathy in patients with type 2 diabetes (11). In this study, multiple regression analysis revealed that CV of SBP was associated with progression of UAE after adjustment for the other risk factors, and multiple Cox regression model revealed that CV of SBP was associated with the increase in the hazard of development of albuminuria.
In other studies, not only SD of SBP but also CV of SBP exhibited an increase as average on-treatment blood pressure increased. For this reason, Rothwell et al. (6) made use of variation independent of mean at which this relationship was lost. However, no significant correlations were found between CV of SBP and average SBP, and CV of SBP was a risk factor for the development and progression of diabetic nephropathy after adjustment for average SBP in this study.
Because antihypertensive drugs such as angiotensin II receptor blocker could delay the development of albuminuria in patients with diabetes (13), we excluded patients with newly prescribed ACE inhibitor or angiotensin II receptor blocker during a follow-up. Because visit-to-visit variability could be determined by improper titration of antihypertensive therapy and by improper downward titration of antihypertensive drug regimen during summer (14), we excluded the patients with any changes of medication for hypertension during 1 year of data collection. Anglo-Scandinavian Cardiac Outcomes Trial Blood Pressure–Lowering Arm (ASCOT-BPLA) indicated that benefits of calcium channel blocker in the prevention of CVD may be partly attributed to the reduction in visit-to-visit variability in blood pressure (6). In our study, visit-to-visit variability in SBP was associated with progression of UAE or development of albuminuria even after adjustment for antihypertensive drug class.
Because a small proportion of normoalbuminuric patients had development of albuminuria, the increase in albuminuria associated with CV of SBP presumably occurs in patients with albuminuria. Multiple regression analysis demonstrated that average of SBP (β = 0.2510; P = 0.0054) or CV of SBP (β = 0.2039; P = 0.0271) was independently associated with change in UAE in patients with normoalbuminuria. Furthermore, inclusion of baseline UAE in the regression models did not affect the relationship between CV of SBP and development of albuminuria.
Variability in SBP is a dynamic and complex phenomenon as a result of intricate interactions among behavioral, environmental, humoral, and neural central or reflex influences (15). Particularly, visit-to-visit variability in blood pressure can be altered by environmental stimuli (16). It is still not clear how blood pressure variability impacts vascular damage or organ damage such as chronic kidney disease. Kawai et al. (17) reported that visit-to-visit variability in blood pressure was associated with renal vascular resistance, which was a useful marker for renal function and albuminuria. Eto et al. (18) suggested that increased blood pressure variability, independently of average blood pressure level, impairs endothelial function by inhibiting nitric oxide production, enhances neointimal formation, and thereby may contribute to atherogenesis in an animal model. Diaz et al. (19) suggested that blood pressure variability was increased with decreased endothelial function and was associated with the vascular smooth muscle response to nitric oxide.
There were several limitations in this study. First, although CV of SBP was measured in a period preceding measurement of UAE, and therefore preceded development of frank albuminuria in normoalbuminuric patients, this study was still unable to determine the direction of effect. An intervention reducing variability in SBP without direct renal effects would have the capacity to demonstrate causation. Second, the study population consisted of Japanese men and women; therefore, it is uncertain whether these findings are generalized in other ethnic groups. Third, medication nonadherence and difference of the time intervals from drug assumption at visits might be one of the causes of visit-to-visit BP variation. Unfortunately, however, we have no exact data for medication adherence and the time from drug assumption. Finally, the number of patients available for analysis was not large, the follow-up was rather short, and the cases of new albuminuria were rare in this study. To make use of all patients, we analyzed the data as a continuum, thereby considering small changes in UAE. Recently, however, Ruggenenti et al. (20) reported that any degree of measurable albuminuria had significant cardiovascular risk among normoalbuminuric patients with type 2 diabetes. We believe that increased UAE below the threshold or microalbuminuria is not likely to be clinically innocent. To assess small change in UAE exactly, UAE was assessed three times in this study. Large prospective trials are needed to better-assess the relationship between variability in SBP and progression of nephropathy or development of albuminuria in patients with type 2 diabetes.
Clinical guidelines emphasized the attention to hypertension as a risk factor for progression of atherosclerosis or organ damage. However, little attention to variability in SBP could be given. Therefore, it is important to clarify the role of variability in SBP in the progression of diabetic nephropathy. To the best of our knowledge, this is the first study to investigate the relationships between visit-to-visit variability in SBP and progression of UAE or development of albuminuria. In conclusion, visit-to-visit variability in SBP could be a novel risk factor for progression of diabetic nephropathy or development of albuminuria.
Acknowledgments
No potential conflicts of interest relevant to this article were reported.
H.O. researched data and wrote the manuscript. M.F., M.T., and G.H. researched data and contributed to discussion. S.M., Y.M., N.Nakan., M.A., and M.Y. researched data. N.Nakam. researched data and reviewed and edited the manuscript. M.F. is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
References
- 1.Isomaa B, Almgren P, Tuomi T, et al. Cardiovascular morbidity and mortality associated with the metabolic syndrome. Diabetes Care 2001;24:683–689 [DOI] [PubMed] [Google Scholar]
- 2.Multiple Risk Factor Intervention Trial Research Group Multiple risk factor intervention trial. Risk factor changes and mortality results. JAMA 1982;248:1465–1477 [PubMed] [Google Scholar]
- 3.Drury PL, Ting R, Zannino D, et al. Estimated glomerular filtration rate and albuminuria are independent predictors of cardiovascular events and death in type 2 diabetes mellitus: the Fenofibrate Intervention and Event Lowering in Diabetes (FIELD) study. Diabetologia 2011;54:32–43 [DOI] [PubMed] [Google Scholar]
- 4.Dinneen SF, Gerstein HC. The association of microalbuminuria and mortality in non-insulin-dependent diabetes mellitus. A systematic overview of the literature. Arch Intern Med 1997;157:1413–1418 [PubMed] [Google Scholar]
- 5.Muntner P, Shimbo D, Tonelli M, Reynolds K, Arnett DK, Oparil S. The relationship between visit-to-visit variability in systolic blood pressure and all-cause mortality in the general population: findings from NHANES III, 1988 to 1994. Hypertension 2011;57:160–166 [DOI] [PubMed] [Google Scholar]
- 6.Rothwell PM, Howard SC, Dolan E, et al. Prognostic significance of visit-to-visit variability, maximum systolic blood pressure, and episodic hypertension. Lancet 2010;375:895–905 [DOI] [PubMed] [Google Scholar]
- 7.Hata Y, Kimura Y, Muratani H, et al. Office blood pressure variability as a predictor of brain infarction in elderly hypertensive patients. Hypertens Res 2000;23:553–560 [DOI] [PubMed] [Google Scholar]
- 8.Hata Y, Muratani H, Kimura Y, et al. Office blood pressure variability as a predictor of acute myocardial infarction in elderly patients receiving antihypertensive therapy. J Hum Hypertens 2002;16:141–146 [DOI] [PubMed] [Google Scholar]
- 9.Kilpatrick ES, Rigby AS, Atkin SL. The role of blood pressure variability in the development of nephropathy in type 1 diabetes. Diabetes Care 2010;33:2442–2447 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mancia G, Facchetti R, Parati G, Zanchetti A. Visit-to-visit blood pressure variability, carotid atherosclerosis, and cardiovascular events in the European Lacidipine Study on Atherosclerosis. Circulation 2012;126:569–578 [DOI] [PubMed] [Google Scholar]
- 11.Okada H, Fukui M, Tanaka M, et al. Visit-to-visit variability in systolic blood pressure is correlated with diabetic nephropathy and atherosclerosis in patients with type 2 diabetes. Atherosclerosis 2012;220:155–159 [DOI] [PubMed] [Google Scholar]
- 12.Expert Committee on the Diagnosis and Classification of Diabetes Mellitus Report of the Expert Committee on the Diagnosis and Classification of Diabetes Mellitus. Diabetes Care 2003;26(Suppl. 1):S5–S20 [DOI] [PubMed] [Google Scholar]
- 13.Wu AY, Low LP. Managing vascular risk in hypertension with a focus on microalbuminuria: attitude and practices. Singapore Med J 2009;50:976–981 [PubMed] [Google Scholar]
- 14.Modesti PA, Morabito M, Bertolozzi I, et al. Weather-related changes in 24-hour blood pressure profile: effects of age and implications for hypertension management. Hypertension 2006;47:155–161 [DOI] [PubMed] [Google Scholar]
- 15.Parati G, Ochoa JE, Bilo G. Blood pressure variability, cardiovascular risk, and risk for renal disease progression. Curr Hypertens Rep 2012;14:421–431 [DOI] [PubMed] [Google Scholar]
- 16.Mancia G, Facchetti R, Parati G, Zanchetti A. Visit-to-visit blood pressure variability in the European Lacidipine Study on Atherosclerosis: methodological aspects and effects of antihypertensive treatment. J Hypertens 2012;30:1241–1251 [DOI] [PubMed] [Google Scholar]
- 17.Kawai T, Ohishi M, Kamide K, et al. The impact of visit-to-visit variability in blood pressure on renal function. Hypertens Res 2012;35:239–243 [DOI] [PubMed] [Google Scholar]
- 18.Eto M, Toba K, Akishita M, et al. Reduced endothelial vasomotor function and enhanced neointimal formation after vascular injury in a rat model of blood pressure lability. Hypertens Res 2003;26:991–998 [DOI] [PubMed] [Google Scholar]
- 19.Diaz KM, Veerabhadrappa P, Kashem MA, et al. Relationship of visit-to-visit and ambulatory blood pressure variability to vascular function in African Americans. Hypertens Res 2012;35:55–61 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ruggenenti P, Porrini E, Motterlini N, et al. BENEDICT Study Investigators Measurable urinary albumin predicts cardiovascular risk among normoalbuminuric patients with type 2 diabetes. J Am Soc Nephrol 2012;23:1717–1724 [DOI] [PMC free article] [PubMed] [Google Scholar]


