Abstract
Background
Dyadic discord, while common in depression, has not been specifically evaluated as an outcome predictor in chronic major depressive disorder. This study investigated pretreatment dyadic discord as a predictor of non-remission and its relationship to depressive symptom change during acute treatment for chronic depression.
Method
Out-patients with chronic depression were randomized to 12 weeks of treatment with nefazodone, the Cognitive Behavioral Analysis System of Psychotherapy or their combination. Measures included the Marital Adjustment Scale (MAS) and the Inventory of Depressive Symptomatology – Self Report (IDS-SR30). Of 681 original patients, 316 were partnered and 171 of these completed a baseline and exit MAS, and at least one post-baseline IDS-SR30. MAS scores were analysed as continuous and categorical variables (‘ dyadic discord ’ v. ‘no dyadic discord ’ defined as an MAS score >2.36. Remission was defined as an IDS-SR30 of ≤14 at exit (equivalent to a 17-item Hamilton Rating Scale for Depression of ≤7).
Results
Patients with dyadic discord at baseline had lower remission rates (34.1%) than those without dyadic discord (61.2%) (all three treatment groups) (χ2=12.6, df=1, p=0.0004). MAS scores improved significantly with each of the treatments, although the change was reduced by controlling for improvement in depression. Depression remission at exit was associated with less dyadic discord at exit than non-remission for all three groups [for total sample, 1.8 v. 2.4, t(169)=7.3, p<0.0001].
Conclusions
Dyadic discord in chronically depressed patients is predictive of a lower likelihood of remission of depression. Couple therapy for those with dyadic discord may increase remission rates.
Keywords: Chronic depression, dyadic discord, major depressive disorder, predictors
Introduction
Major depressive disorder (MDD) is common in the general population, with a lifetime prevalence of 16.2% (Kessler et al. 2003). Its course is often recurrent or chronic: 15–25% of patients with MDD will have chronic MDD (episodes lasting 2 years or longer) (Keller et al. 1992; Hollon et al. 2006). MDD is also associated with substantial functional impairment (Broadhead et al. 1990). Whether chronic as opposed to episodic depression begets greater functional impairment is unclear (Friedman, 1993), though depressive symptom severity may be higher in chronic depression (Wells et al. 1992; Miller et al. 1998).
When two individuals become a couple, their network of friends becomes smaller and the partner assumes a larger place in the social network (Kalmijn, 2003). Correspondingly, a type of psychosocial impairment of particular importance in depression is dyadic discord (Whisman, 2001a). It is well established that dyadic discord is associated with both depressive symptoms and diagnostic depression (Whisman, 2001a). Even after recovery from a depressive episode, patients report lower marital satisfaction (Herr et al. 2007). Negative marital events predict future depressive symptomatology (Christian-Herman et al. 2001) and marital interaction patterns may contribute to the generation of future depressive episodes (Hammen, 1991; Davila et al. 1997).
While there has been less research specifically on chronic depression, dyadic discord levels have been found to be greater in chronic MDD than community controls (Hirschfeld et al. 2002). Whether treatment of depression improves dyadic discord in chronic depressions is unclear (Kocsis et al. 1988; Friedman et al. 1995; Miller et al. 1998).
One study to date has found that depressed patients with higher pretreatment levels of dyadic discord were less likely to achieve remission with treatment for chronic depression (Miller et al. 1998). Similarly, at the conclusion of treatment, patients who achieved remission from chronic depression had less dyadic discord at baseline than those who did not achieve remission (Miller et al. 1998). This study examined only medication treatments for chronic depression.
The present study examined the role of dyadic discord in chronically depressed patients treated with medication alone (nefazodone), psychotherapy alone [Cognitive Behavioral Analysis System of Psychotherapy (CBASP); McCullough, 2000] or their combination (Keller et al. 2000). The sample used in this report was found to have greater dyadic discord than a community reference sample (Hirschfeld et al. 2002), but the predictive value and the relationship between change in depressive symptoms and change in dyadic discord have not been evaluated.
We were interested in whether baseline dyadic discord would predict depressive symptom outcome in each treatment cell, and whether dyadic discord after treatment would distinguish those who did and did not remit from their depression. Prior research on MDD, that did not focus specifically on patients with chronic depression, has suggested that antidepressant medication, interpersonal therapy and cognitive therapy each improve dyadic discord only indirectly by their effects on depressive symptoms (Whisman, 2001b; Vittengl et al. 2004). We, therefore, also wanted to examine whether any improvements in dyadic discord were direct or indirect treatment effects. It is logical to estimate that CBASP would directly affect dyadic discord while medication would have an indirect effect.
This report addresses the following questions:
Is baseline dyadic discord predictive of remission of depression treated with nefazodone, CBASP or their combination?
Does dyadic discord improve after acute treatment with nefazodone, CBASP or their combination?
Is the improvement in dyadic discord a direct or indirect effect of treatment and does it depend on the type of treatment?
Is non-remission of depression at exit from acute treatment associated with greater dyadic discord than remission?
Method
Participants
The participants, design, therapists, instruments and treatments in this study have been described previously (Keller et al. 2000). In brief, 681 out-patient participants (aged 18–75 years) were recruited from 12 academic centers. They met criteria for either (a) chronic MDD (at least 2 years duration of the index major depressive episode); (b) MDD superimposed on dysthymic disorder; or (c) recurrent MDD with incomplete remission between episodes and at least 2 years of illness (Keller et al. 2000). They had to score ≥20 on the 24-item Hamilton Rating Scale for Depression (HAMD). Participants with chronic nonpsychotic MDD were randomized (1 :1:1) to up to 12 weeks of treatment with nefazodone (maximal dose 600 mg per day), CBASP (McCullough, 2000) or their combination.
Of the 316 participants who answered ‘yes’ to the question ‘Are you living with your spouse or have you been living with a partner in an intimate relationship ?’ on the Social Adjustment Scale (SAS) (Weissman & Paykel, 1974), 171 fully completed the Marital Adjustment Scale (MAS) at both baseline and exit and were included in this report.
Measures
Thirty-item Inventory of Depressive Symptomatology – Self Report (IDS-SR30)
The IDS-SR30 assesses the severity of the signs and symptoms of depression (Rush et al. 1996). Items assess all nine criterion symptoms of a major depressive episode and common associated symptoms such as anxiety. Each item is rated on a 0 to 3 scale (higher scores represent greater symptom severity). Of the 30 items, 28 contribute to the total score (range from 0 to 84), as only appetite increase or decrease and only weight increase or decrease are rated. The IDS-SR30 has good internal consistency (ά=0.90) and item-total correlations (Trivedi et al. 2004). The IDS-SR30 has performed well in relationship to the 17-item HAMD (Rush et al. 2006a) and has been used in numerous clinical studies (Rush et al. 2007). The IDS-SR30 was administered weekly for the first 4 weeks and biweekly thereafter through week 12 for those who completed the treatment protocol or time of withdrawal for those who did not.
MAS
Dyadic discord was assessed by MAS, a nine-item subscale of the SAS (Weissman & Paykel, 1974), which was administered at baseline, week 4, week 8 and week 12 (or study exit).
The nine items relate specifically to the relationship with a spouse or intimate partner over the last month. Sample items include ‘Have you had any open arguments with your partner in the last month? ’ and ‘How have you felt about your partner during the last month?’ Responses to each item are provided on a five-point scale. The mean of these nine items produces the total score (range 1 to 5). Higher scores indicate greater discord. Internal consistency for the MAS is adequate (0.67–0.68) (Whisman, 2001b). MAS scores are significantly associated with scores on the Marital Adjustment Test (Kaslow et al. 1992); the MAS has been used in other studies of depression (Whisman, 2001b).
Following the method of Vittengl et al. (2004), patients were classified as having ‘dyadic discord’ if their MAS scores were above 2.36. This score, which is 1.28 s.d. above the mean of a normative sample (Weissman et al. 1978), classifies about 10% of the general population as having dyadic discord. As noted by Vittengl et al. (2004), this cut-off is a compromise between the tradition of defining abnormality at 2 s.d. from the mean (Jacobson & Truax, 1991) (which classifies about 2% of the population as unhealthy) and research showing that social-interpersonal dysfunction is greater than 2% (e.g. about 9% in Fredman et al. 1988). The use of a 1.28 s.d. cut-off has also yielded significant results previously (Vittengl et al. 2004).
Statistical methods
Logistic regression was used to test the ability of baseline MAS scores in the ‘dyadic discord’ range to predict remission status at exit. Remission was defined as an IDS-SR30 score of 14 or less (Rush et al. 2003), which is equivalent to a score of ≤7 on the 17-item HAMD. A declining-effects random-regression analysis (Kashner et al. 2003) was done to test for a significant change from pretreatment to week 4 (initial effect) and from week 4 to week 12 in MAS scores and to test for a significant difference between groups (nefazodone, CBASP, combination) in initial effect and in improvement over time (time × group interaction) in MAS scores. The rationale for these time periods is that, in the original study, medication was found to have a greater effect on depression in the first 4 weeks while psychotherapy had a greater effect in the latter 8 weeks (Keller et al. 2000).
Covariates of age, gender, race (Caucasian or non-Caucasian), baseline MAS score and baseline IDS-SR30 total score were included in the model. To assess whether MAS score improved independently of depression symptom improvement, the basic random-regression model was refit with the inclusion of change in IDS-SR30 total score as a time-varying covariate. This model estimates the change in MAS scores that would have occurred if there had been no change in IDS-SR30 scores. To assess the change over time in MAS scores for depression remitters and non-remitters at exit, the basic random-regression model was refit with additional terms for remission status and interactions of remission status with initial effect and time. The presence or absence of dyadic discord at each visit was analysed using a generalized linear mixed model (Wolfinger & O’Connell, 1993) which adapts the random-regression model for use with a binary outcome as implemented in the SAS glimmix program (SAS Institute, Inc., USA). All tests were two-sided.
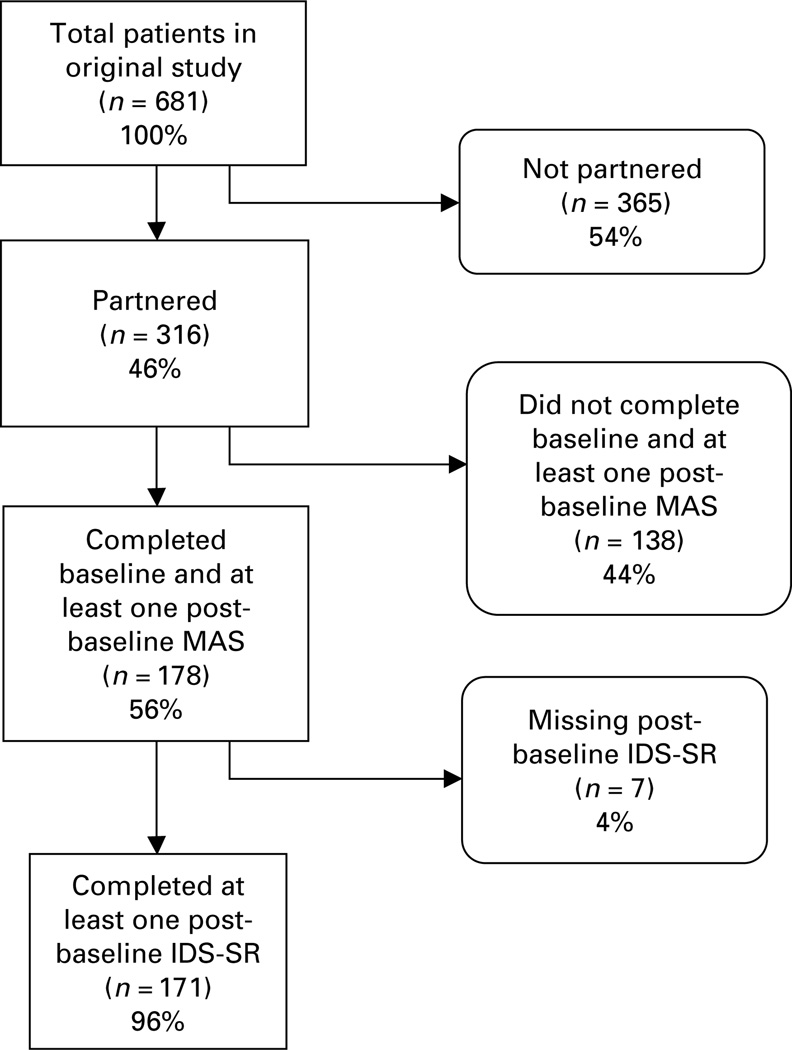
Results
Altogether, 316 of the 681 patients (46.4%) indicated that they were married or in an intimate relationship (‘partnered’ participants in Fig. 1). Of these, 209 of the 316 (66.1%) completed the baseline MAS. Of the 107 who did not complete the entire MAS, 87 (83.1%) were excluded due to not completing one or both of two items asking about the respondent’s sexual life1,†. Of the 209 with a complete baseline MAS, 178 (85.2%) completed the exit MAS to comprise the final sample. Of the subjects, seven were missing post-baseline IDS-SR30 scores so that their exit remission status could not be determined. Thus, 171 subjects were available for the analyses involving remission status.
Fig. 1.
Participant flow. MAS, Marital Adjustment Scale; IDS-SR, Inventory of Depressive Symptomatology – Self Report.
Baseline and exit characteristics
The evaluable sample had a mean age of 42.8 (s.d.=9.0) years, being 64.0% female and 91% Caucasian. Mean baseline scores were 39.6 (s.d.=8.2) for the IDS-SR30 and 2.40 (s.d.=0.5) for the MAS. Mean exit scores were 18.2 (s.d.=12.9) for the IDS-SR30 and 2.1 (s.d.=0.5) for the MAS. Depression remission rates (IDS-SR30 of ≤14) at the last available assessment (exit) were 39.7% (nefazodone), 40.0% (CBASP) and 58.7% (combination). Whereas slightly more than one half of the study group scored above the threshold for dyadic discord at study entry (52.8%, 94/178), 29.2% (52/178) of the sample was in the range of dyadic discord at study endpoint. No significant interactions were found between gender and treatment group, change over time in outcome or baseline dyadic discord.
Is dyadic discord at baseline associated with non-remission after depression treatment?
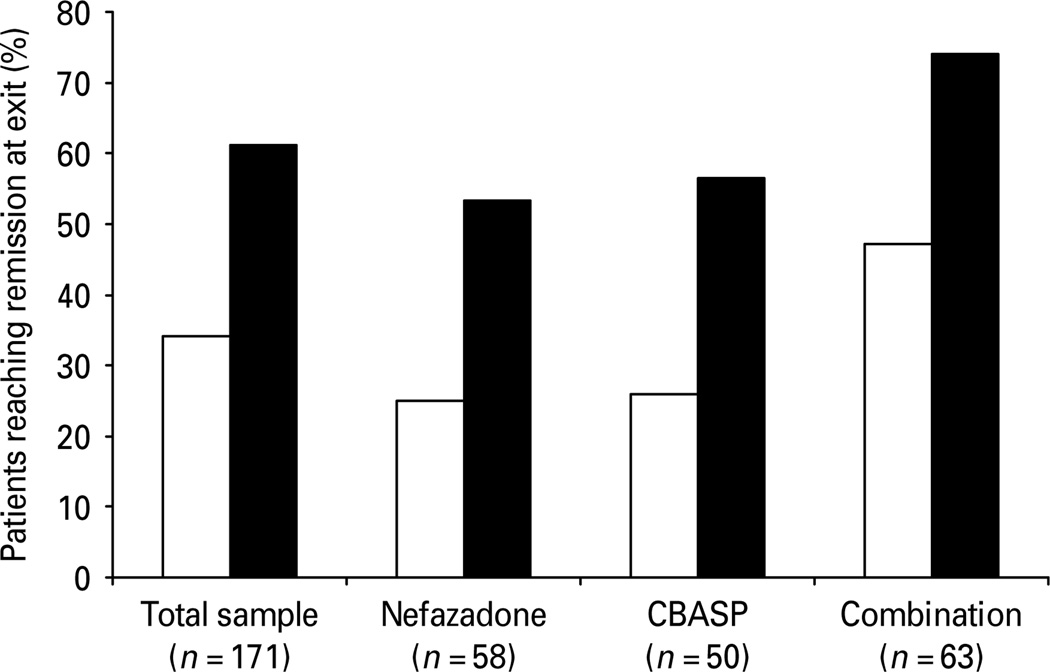
Patients with dyadic discord at study entry had a significantly lower rate of remission from depression at study exit than those without dyadic discord. Only 34.1% (31/91) of patients with dyadic discord before treatment remitted as compared with 61.2% (49/80) of patients without dyadic discord (χ2=12.6, df=1, p=0.0004). This finding held true for each of the three treatments. For the nefazodone group, 25.0% (7/28) of the discordant group remitted v. 53.3% (16/30) of the non-discordant group (χ2=4.8, df=1, p=0.0275). Similarly, for the CBASP group, only 25.9% (7/27) of the discordant group remitted v. 56.5% (13/23) of the non-discordant group (χ2=4.8, df=1, p=0.0277). For the combination group, the rates were 47.2% (17/36) v. 74.1% (20/27) (χ2=4.6, df=1, p=0.0322). The percentage of patients in the range of dyadic discord (or non-dyadic discord) at study entry for exit remitters is shown in Fig. 2.
Fig. 2.
Comparing exit rates of remission for patients with (□) and without (■) dyadic discord at baseline. Remission was defined as an Inventory of Depressive Symptomatology – Self Report (IDS-SR30) score of ≤14 at study exit. CBASP, Cognitive Behavioral Analysis System of Psychotherapy.
A logistic regression analysis that controlled for pretreatment characteristics as covariates showed that the baseline dyadic discord status (yes/no) still predicted exit depression remission status (yes/no) after adjustments for age, gender, race, treatment group and pretreatment IDS-SR30 score (χ2=8.8, df=1, p=0.003). Non-discordant patients at study entry were 2.8 times more likely to reach remission at exit (29.0%) than discordant patients (12.7%) [95% confidence interval (CI) 1.4–5.5]. The effect of baseline discordant status in relation to remission did not vary significantly by treatment group (treatment group × health status interaction : χ2=0.2, df=2, p=0.92) or by gender (gender × dyadic discord status interaction : χ2=4.0, df=2, p=0.14).
Does dyadic discord improve with depression treatment?
Change in dyadic discord was examined as both a continuous and categorical variable. Table 1 provides mean MAS scores. Results from the random-regression model showed that MAS scores improved significantly from baseline to week 4 [−0.21 points, t(224)=4.2, p<0.0001]. This improvement was not significantly different among treatment groups [F(2, 279)=0.3, p=0.77]. A significant decrease also occurred from week 4 to week 12 [F(1, 158)=31.9, p<0.0001], and a significant visit × treatment group effect was found [F(2, 158)=5.5, p=0.0050]. The decrease in MAS scores from week 4 to week 12 was greatest in the combination group at 0.18 points per month [t(154)=5.9, p<0.0001], least for the group receiving nefazodone alone at 0.03 points per month [t(161)=1.0, p=0.3008] and intermediate at 0.10 points per month for the patients receiving CBASP alone [t(159)=3.0, p=0.0028]. The decrease from week 4 to week 12 in the combination group was significantly greater than the decrease with nefazodone alone [t(158)=3.3, p=0.0012], while the decrease with CBASP was not significantly different from changes with either of the remaining two groups.
Table 1.
Average Marital Adjustment Scale score by treatment group and weeks in treatmenta
| Visit | All patients |
Nefazodone | Combination | CBASP |
|---|---|---|---|---|
| Baseline | 2.44 (0.5) | 2.43 (0.5) | 2.50 (0.5) | 2.37 (0.5) |
| n | 178 | 60 | 66 | 52 |
| Week 4 | 2.31 (0.5) | 2.36 (0.5) | 2.37 (0.6) | 2.20 (0.5) |
| n | 149 | 49 | 55 | 45 |
| Week 8 | 2.16 (0.5) | 2.24 (0.5) | 2.13 (0.5) | 2.08 (0.5) |
| n | 144 | 48 | 55 | 41 |
| Week 12 | 2.04 (0.5) | 2.18 (0.6) | 1.94 (0.5) | 1.99 (0.5) |
| n | 144 | 49 | 51 | 44 |
| Exitb | 2.10 (0.5) | 2.24 (0.6) | 2.04 (0.5) | 2.03 (0.5) |
| n | 178 | 60 | 66 | 52 |
CBASP, Cognitive Behavioral Analysis System of Psychotherapy.
Values are given as mean (standard deviation).
Lower scores represent less dyadic discord.
The ‘ Exit ’ score is the last score obtained from the participant whether it was at week 12 or earlier.
Table 2 provides the percentage of patients categorized as having dyadic discord at each assessment. The random-regression model for binary outcome (presence/absence of dyadic discord) showed that across all groups, the percentage of patients classified as having dyadic discord decreased significantly from baseline to week 4 [t(166)=2.3, p=0.0229] and from week 4 to completion of treatment [F(1, 250)=10.7, p=0.0012]. At study exit, however, a significant difference among groups was found (Table 2) (χ2=6.9, df=2, p=0.0314). Specifically, at exit there was no difference between the groups receiving CBASP alone or the combination of CBASP and nefazodone (24.2% v. 21.2%, χ2=0.2, df=1, p=0.6917). However, dyadic discord was more frequent with nefazodone alone than with the other two treatments collectively at exit (41.7% v. 22.9%, χ2=6.8, df=1, p=0.0092).
Table 2.
Participants with dyadic discord by treatment group and weeks in treatment
| Visit | All patients | Nefazodone | Combination | CBASP |
|---|---|---|---|---|
| Baseline | 178 (52.8) | 60 (48.3) | 66 (57.6) | 52 (51.9) |
| Week 4 | 149 (44.3) | 49 (51.0) | 55 (47.3) | 45 (33.3) |
| Week 8 | 144 (32.6) | 48 (37.5) | 55 (34.6) | 41 (24.4) |
| Week 12 | 144 (24.3) | 49 (36.7) | 51 (51.7) | 44 (20.4) |
| Exita | 178 (29.2) | 60 (41.7) | 66 (24.2) | 52 (21.2) |
CBASP, Cognitive Behavioral Analysis System of Psychotherapy.
Values are given as number of participants (percentage).
The ‘ Exit ’ score is the last score obtained from the participant whether it was at week 12 or earlier.
Is improvement in dyadic discord accounted for by improvement in depressive symptoms?
Overall, in the three treatment groups, a significant positive correlation was found between changes in dyadic discord and changes in depressive severity from baseline to treatment exit (change in IDS-SR30 v. MAS: r=0.50, p<0.0001). The correlations for the nefazodone, combination and CBASP groups were 0.45, 0.58 and 0.43, respectively. Adjusting for changes in IDS-SR30 scores allows estimation of the change in MAS scores that would have occurred if depressive symptoms had remained constant throughout the study. After adjustment for changes in IDS-SR30 scores during the study, the random-regression model showed no change in MAS scores from baseline to week 4 for all groups combined (n=171) [0.02 points, t(253)=0.3, p=0.7567]. However, the initial effect (i.e. the first 4 weeks of treatment) did vary by treatment group [F(2, 306)=3.9, p=0.0210] with a decrease of 0.10 points in the CBASP group, an increase of 0.01 points in the nefazodone group and an increase of 0.13 points in the combination group. Thus, the initial effect of CBASP on MAS scores is less dependent on improvement in depressive symptoms than the other groups. From week 4 to week 12 a non-significant decrease of 0.02 points per month was found [t(208)=1.4, p=0.1685] for all groups combined. This time effect did not vary by treatment group [F(2, 208)=1.7, p=0.1821]. Thus, change in MAS score was best accounted for by change in depressive symptoms during the latter two-thirds of the treatment protocol.
Do depression treatment remitters have less dyadic discord at study exit than non-remitters ?
MAS scores at exit were significantly lower among depression remitters than non-remitters using the random-regression model. This relationship held true for all patients [1.83 v. 2.35, t(169)=7.3, p<0.0001] and for each treatment : nefazodone [1.86 v. 2.49, t(56)=5.0, p<0.0001], combination [1.83 v. 2.34, t(61)=4.2, p<0.0001] and CBASP [1.79 v. 2.20, t(48)=3.2, p=0.0002].
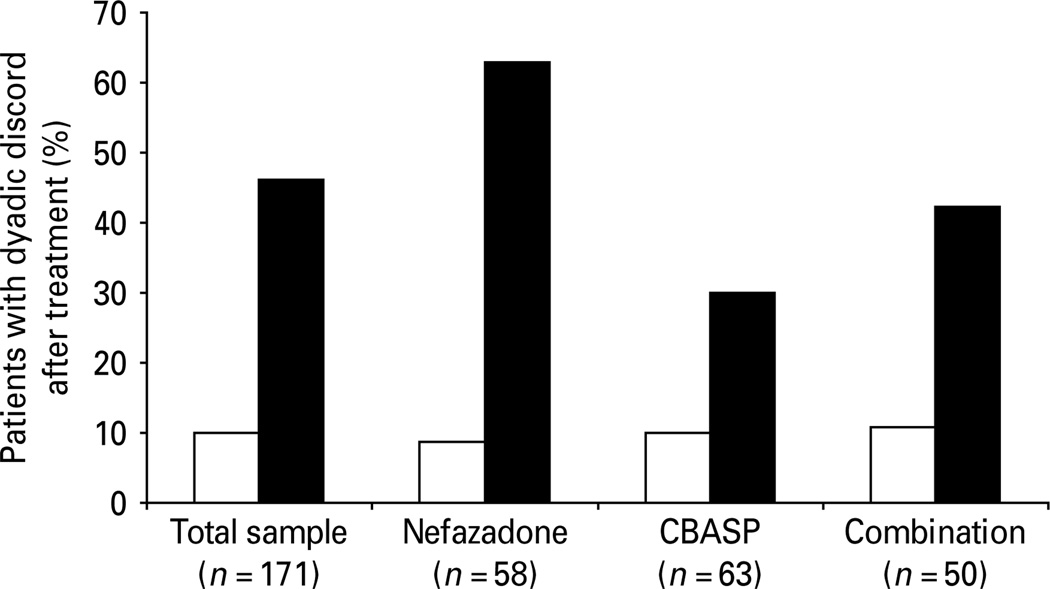
Examined dichotomously, fewer depression remitters had dyadic discord at exit than non-remitters (Fig. 3) did. For the total sample, 10.0% (8/80) of remitters had dyadic discord v. 46.2% (42/91) of non-remitters (χ2=26.9, df=1, p<0.0001). The difference was significant for the nefazodone and combination treatment groups: for nefazodone, 8.7% (2/23) of remitters had dyadic discord v. 62.9% (22/35) of non-remitters (χ2=16.8, df=1, p<0.0001). For combination therapy, 10.8% (4/37) of remitters had dyadic discord v. 42.3% (11/26) of non-remitters (χ2=8.4, df=1, p=0.0039). For the CBASP group, the numerical difference was not statistically significant : 10.0% (2/20) of remitters had dyadic discord v. 30.0% (9/30) of non-remitters (χ2=2.8, df=1, p=0.0944).
Fig. 3.
Comparing rates of dyadic discord at exit for depression remitters (□) and non-remitters (■). Dyadic discord was defined as a Marital Adjustment Scale score >2.36. CBASP, Cognitive Behavioral Analysis System of Psychotherapy.
A random-regression model was used to estimate improvement over time by exit remission status. For all patients, dyadic discord decreased among depression remitters by 0.26 points initially (baseline to week 4) and by 0.15 points per month subsequently (weeks 4 to 12), while depression non-remitters decreased by 0.10 points initially and by 0.06 points per month subsequently. MAS scores improved more in those whose depressions remitted than in those whose depressions did not remit both within the first 4 weeks (p=0.0076) and in the subsequent 8 weeks (p=0.0115).
For those receiving nefazodone alone, depression remitters significantly improved in dyadic discord initially (−0.25 points, p=0.0067) and subsequently (−0.12 points per month, p=0.0141), while non-remitters had a non-significant improvement initially (−0.13 points, p=0.0949) and a slight deterioration in dyadic discord subsequently (+0.03 points per month, p=0.4708). The depression remitters and non-remitters were significantly different in terms of change in MAS ratings in the last 8 weeks of treatment (p=0.0190).
For CBASP alone, depression remitters improved significantly in dyadic discord both initially (−0.22 points, p<0.0234) and subsequently (−0.20 points per month, p<0.0001). Depression non-remitters had an equally large significant initial improvement (−0.25 points, p=0.0022), but this improvement was not sustained. Only a very slight non-significant MAS score reduction (dyadic discord improvement) occurred from week 4 to week 12 (−0.02 points per month, p=0.6134). Over the last 8 weeks of treatment with CBASP, depression remitters had significantly greater improvement in MAS scores over time than non-remitters (p=0.0071).
For the combination group, depression remitters had a significant initial improvement (−0.33 points, p<0.0001), while non-remitters worsened (+0.09 points, p=0.3109). Both remitters and non-remitters had a similar magnitude of subsequent improvement in dyadic discord, and the difference between them was not different (−0.15 v. −0.20 points per month, respectively, p=0.4165).
Discussion
There are several results with clinical significance. Patients with dyadic discord when they began treatment were much less likely to reach remission from depression after 12 weeks of treatment, regardless of treatment modality. Combination treatment was almost twice as successful with dyadically discordant patients than either of the monotherapies (although still less successful than combination therapy with non-discordant patients). Overall, patients with dyadic discord were 2.8 times less likely to reach remission than were dyadically non-discordant patients. This finding is consistent with other studies finding dyadic discord to be a risk factor for poor treatment outcome (Hickie & Parker, 1992; Whisman, 2001b).
At the conclusion of treatment, patients who did not remit from their chronic depression had significantly greater levels of dyadic discord after treatment than did depression remitters, which replicates previous work (Miller et al. 1998). Another study, using continuous analyses rather than dichotomous, found no differences in dyadic discord between remitters v. responder non-remitters or responders v. non-responders; they did not, however, compare remitters with non-remitters (Papakostas et al. 2004).
Dyadic discord improved with each of the three treatments, and each was associated with more patients at exit without dyadic discord. Nefazodone alone, however, was less effective in reducing discord than the other two strategies – each of which included CBASP. The combination group had the greatest improvement in severity of dyadic discord ratings, while medication alone had the least improvement. CBASP alone produced an improvement in dyadic discord intermediate between the medication alone and combination treatment.
The improvement in dyadic discord was largely accounted for by reduction in depression symptom severity, which is consistent with earlier reports that depression treatments have an indirect effect on dyadic discord (Whisman, 2001b; Vittengl et al. 2004). Combination treatment likely produced the greatest improvement in dyadic discord because it produced the greatest improvement in depressive severity (Keller et al. 2000). During the first 4 weeks, CBASP alone (but not in combination with medication) did produce change in dyadic discord independent from change in depression but this effect did not continue during the last 8 weeks of the study.
Antidepressant treatments have variably improved dyadic discord in depressed patients. Several studies of patients with both depression and dyadic discord found that cognitive therapy was beneficial for depressive symptoms but not dyadic discord (O’Leary & Beach, 1990; Jacobson et al. 1991). Patients receiving cognitive therapy in another study experienced a significant improvement in dyadic discord, although scores at the completion of treatment were still in the discordant range (Vittengl et al. 2004). A study utilizing nortriptyline and sertraline found that treatment with neither medication resulted in improvement in dyadic discord (Logsdon et al. 2003). On the other hand, improvement in dyadic discord has been reported after treatment with imipramine, cognitive therapy or interpersonal therapy (Whisman, 2001b). Responders to fluoxetine similarly had an improvement in dyadic discord (results for non-responders were not reported) (Reimherr et al. 2001).
Focusing on chronic depression, Miller et al. (1998) found that both sertraline and imipramine produced improvements in dyadic discord. The present results add to these findings, and they indicate that depression treatments that do not include the partner (and may not even explicitly address relationship issues) can produce improvement in dyadic discord. That is, improving depression per se improves the relationship. Improvements in irritability or anhedonia may have an ameliorative effect on the relationship, for example, although the present data do not address this issue.
These results are limited by having data only from the depressed patients and not their partners. In a probabilistic community sample, 20.8% of men married to women with MDD also had MDD while 28.0% of women married to men with MDD also had MDD (McLeod, 1993). Dyadic discord levels are influenced by an interaction between both partners’ depression levels (Whisman et al. 2004) so that changes in dyadic discord in the present analyses are being influenced in unknown ways by depression levels in the partners. It is conceivable that having a partner with depression would have an impact on the associations reported here so that a replication including data from both partners would be important. Further, depression might bias patients’ evaluations of their relationship quality. Having partner data would provide an evaluation of the quality of the relationship not influenced by depression (in the case of non-depressed partners). Another limitation is that the sample was restricted to patients with chronic depression. The extent to which these findings will generalize to patients with non-chronic depression is not known.
The present data point toward dyadic discord as an important factor potentially contributing to non-remission in chronically depressed patients treated with medication, psychotherapy or the combination. Couple therapy has been found to be efficacious in the treatment of mixed forms of major depression (O’Leary & Beach, 1990; Leff et al. 2000; Dessaulles et al. 2003; Barbato & D’Avanzo, 2008). Whether adding couple therapy to depression treatment for patients with chronic depression might increase depression remission rates remains an unanswered question.
The present findings may also be relevant to the issue of how to sequence treatments for depression (Rush et al. 2006b; Murphy et al. 2007). After treatment, those who did not reach depression remission had significantly higher rates of dyadic discord than those who did. It might be worthwhile for clinicians to assess for dyadic discord in patients who have not remitted after an initial course of individual psychotherapy and/or pharmacotherapy. This approach is consistent with the recommendation of Whisman (2001b) that patients with dyadic discord at the completion of depression treatment might be best served by a referral for couple therapy, although this recommendation has not been empirically evaluated. These results suggest the need to evaluate this recommendation.
Acknowledgements
The present study was supported by Bristol–Myers Squibb.
Declaration of Interest
A.J.R. has received research support from the National Institute of Mental Health, the Robert Wood Johnson Foundation and the Stanley Medical Research Institute. He has been on the advisory boards and/or consultant for Advanced Neuromodulation Systems, Inc., AstraZeneca, Best Practice Project Management, Inc., Bristol–Myers Squibb Company, Cyberonics, Inc., Eli Lilly and Company, Gerson Lehman Group, GlaxoSmithKline, Jazz Pharmaceuticals, Magellan Health Services, Merck & Co, Inc., Neuronetics, Ono Pharmaceutical, Organon USA Inc., Pam Lab, Personality Disorder Research Corp., Pfizer Inc., The Urban Institute and Wyeth–Ayerst Laboratories Inc. He has been on the speakers’ bureau for Cyberonics, Inc., Forest Pharmaceuticals, Inc. and GlaxoSmithKline. He has equity holdings (excluding mutual funds/blinded trusts) in Pfizer Inc. and has royalty income affiliations with Guilford Publications and Healthcare Technology Systems, Inc.
M.E.T. has served in an advisory or consulting capacity to, or received speakers’ honoraria from, AstraZeneca, Bristol–Myers Squibb, Cephalon, Cyberonics, Inc., Eli Lilly and Company, GlaxoSmithKline, Janssen Pharmaceutica, MedAvante, Inc., Neuronetics, Inc., Novartis, Organon, Inc., Sanofi-Aventis, Sepracor, Inc., Shire US, Inc. and Wyeth Pharmaceuticals. He has equity holdings in MedAvante, Inc. He has received royalty/patent or other income from American Psychiatric Publishing, Inc., Guilford Publications and Herald House.
M.H.T. has been a consultant for Abbott Laboratories, Inc., Akzo (Organon Pharmaceuticals Inc.), AstraZeneca, Bayer, Bristol–Myers Squibb Company, Cephalon, Inc., Cyberonics, Inc., Eli Lilly & Company, Fabre-Kramer Pharmaceuticals, Inc., Forest Pharmaceuticals, GlaxoSmithKline, Janssen Pharmaceutica Products, LP, Johnson & Johnson PRD, Eli Lilly & Company, Meade Johnson, Neuronetics, Parke-Davis Pharmaceuticals, Inc., Pfizer, Inc., Pharmacia & Upjohn, Sepracor, Solvay Pharmaceuticals, Inc., Vantage-Point and Wyeth-Ayerst Laboratories. He has served on speakers’ bureaus for Abdi Brahim, Akzo (Organon Pharmaceuticals Inc.), Bristol–Myers Squibb Company, Cephalon, Inc., Cyberonics, Inc., Forest Pharmaceuticals, GlaxoSmithKline, Janssen Pharmaceutica Products, LP, Eli Lilly & Company, Pharmacia & Upjohn, Solvay Pharmaceuticals, Inc. and Wyeth–Ayerst Laboratories. He has also received grant support from Bristol–Myers Squibb Company, Cephalon, Inc., Corcept Therapeutics, Inc., Cyberonics, Inc., Eli Lilly & Company, Forest Pharmaceuticals, GlaxoSmithKline, Janssen Pharmaceutica, Merck, National Institute of Mental Health, National Alliance for Research in Schizophrenia and Depression, Novartis, Pfizer Inc., Pharmacia & Upjohn, Predix Pharmaceuticals, Solvay Pharmaceuticals, Inc. and Wyeth–Ayerst Laboratories.
M.B.K. has been a consultant and/or received honoraria from Cenerex, Cephalon, Cypress Bioscience, Cyberonics, Forest Laboratories, Janssen, JDS, Organon, Novartis, Pfizer and Wyeth. He has received a research grant from Pfizer. He serves on the advisory boards of Abbot Laboratories, Bristol–Myers Squibb, Cenerex, Cyberonics, Cypress Bioscience, Forest Laboratories, Janssen, Novartis, Organon and Pfizer.
Footnotes
The notes appear after the main text.
There were 76 subjects who did not complete one or both of the sexuality questions who completed the MAS at both baseline and exit. Those 76 subjects had a mean age of 48.8 years v. a mean age of 42.8 years for the 178 who completed the entire MAS (p<0.0001). The two groups did not differ on baseline IDS-SR [40.7 (n=76) v. 39.6 (n=178), p=0.3426] but did differ on scores for the abbreviated MAS [3.1 (n=76) v. 2.6 (n=178), p<0.0001]. They did not differ on race [94.7% white (n=76) v. 91.0% white (n=178), p=0.3127] but did differ on gender [80.3% female (n=76) v. 64.0% female (n=178), p=0.0106]. Thus, the group that did not answer the two questions tended to be older, female and have higher levels of dyadic discord than those who did answer the last two questions. The continuous outcome analyses were recalculated including these 76 subjects. Results of the new analyses were found to be substantially the same, so only results from subjects who fully completed the MAS at both administrations are presented in the text.
References
- Barbato A, D’Avanzo B. Efficacy of couple therapy as a treatment for depression : a meta-analysis. Psychiatric Quarterly. 2008;79:121–132. doi: 10.1007/s11126-008-9068-0. [DOI] [PubMed] [Google Scholar]
- Broadhead WE, Blazer DG, George LK, Tse CK. Depression, disability days, and days lost from work in a prospective epidemiologic survey. Journal of the American Medical Association. 1990;264:2524–2528. [PubMed] [Google Scholar]
- Christian-Herman JL, O’Leary KD, Avery-Leaf S. The impact of severe negative events in marriage on depression. Journal of Social and Clinical Psychology. 2001;20:24–40. [Google Scholar]
- Davila J, Bradbury TN, Cohan CL, Tochluk S. Marital functioning and depressive symptoms: evidence for a stress generation model. Journal of Personality and Social Psychology. 1997;73:849–861. doi: 10.1037//0022-3514.73.4.849. [DOI] [PubMed] [Google Scholar]
- Dessaulles A, Johnson SM, Denton WH. Emotion-focused therapy for couples in the treatment of depression : a pilot study. American Journal of Family Therapy. 2003;31:345–353. [Google Scholar]
- Fredman L, Weissman MM, Leaf PJ, Bruce ML. Social functioning in community residents with depression and other psychiatric disorders : results of the New Haven Epidemiologic Catchment Area study. Journal of Affective Disorders. 1988;15:103–112. doi: 10.1016/0165-0327(88)90077-8. [DOI] [PubMed] [Google Scholar]
- Friedman RA. Social impairment in dysthymia. Psychiatric Annals. 1993;23:632–637. [Google Scholar]
- Friedman RA, Markowitz JC, Parides M, Kocsis JH. Acute response of social functioning in dysthymic patients with desipramine. Journal of Affective Disorders. 1995;34:85–88. doi: 10.1016/0165-0327(95)00003-6. [DOI] [PubMed] [Google Scholar]
- Hammen C. Generation of stress in the course of unipolar depression. Journal of Abnormal Psychology. 1991;100:555–561. doi: 10.1037//0021-843x.100.4.555. [DOI] [PubMed] [Google Scholar]
- Herr NR, Hammen C, Brennan PA. Current and past depression as predictors of family functioning : a comparison of men and women in a community sample. Journal of Family Psychology. 2007;21:694–702. doi: 10.1037/0893-3200.21.4.694. [DOI] [PubMed] [Google Scholar]
- Hickie I, Parker G. The impact of an uncaring partner on improvement in non-melancholic depression. Journal of Affective Disorders. 1992;25:147–160. doi: 10.1016/0165-0327(92)90077-j. [DOI] [PubMed] [Google Scholar]
- Hirschfeld RM, Dunner DL, Keitner G, Klein DN, Koran LM, Kornstein SG, Markowitz JC, Miller I, Nemeroff CB, Ninan PT, Rush AJ, Schatzberg AF, Thase ME, Trivedi MH, Borian FE, Crits-Christoph P, Keller MB. Does psychosocial functioning improve independent of depressive symptoms? A comparison of nefazodone, psychotherapy, and their combination. Biological Psychiatry. 2002;51:123–133. doi: 10.1016/s0006-3223(01)01291-4. [DOI] [PubMed] [Google Scholar]
- Hollon SD, Shelton RC, Wisniewski S, Warden D, Biggs MM, Friedman ES, Husain M, Kupfer DJ, Nierenberg AA, Petersen TJ, Shores-Wilson K, Rush AJ. Presenting characteristics of depressed outpatients as a function of recurrence : preliminary findings from the STAR*D clinical trial. Journal of Psychiatric Research. 2006;40:59–69. doi: 10.1016/j.jpsychires.2005.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacobson NS, Fruzzetti AE, Dobson K, Schmaling KB, Salusky S. Marital therapy as a treatment for depression. Journal of Consulting and Clinical Psychology. 1991;59:547–557. doi: 10.1037//0022-006x.59.4.547. [DOI] [PubMed] [Google Scholar]
- Jacobson NS, Truax P. Clinical significance : a statistical approach to defining meaningful change in psychotherapy research. Journal of Consulting and Clinical Psychology. 1991;59:12–19. doi: 10.1037//0022-006x.59.1.12. [DOI] [PubMed] [Google Scholar]
- Kalmijn M. Shared friendship networks and the life course : an analysis of survey data on married and cohabiting couples. Social Networks. 2003;25:231–249. [Google Scholar]
- Kashner TM, Carmody TJ, Suppes T, Rush AJ, Crismon ML, Miller AL, Toprac M, Trivedi M. Catching up on health outcomes : The Texas Medication Algorithm Project. Health Services Research. 2003;38:311–331. doi: 10.1111/1475-6773.00117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaslow N, Warner V, John K, Brown R. Intrainformant agreement and family functioning in depressed and nondepressed parents and their children. American Journal of Family Therapy. 1992;20:204–217. [Google Scholar]
- Keller MB, Lavori PW, Mueller TI, Endicott J, Coryell W, Hirschfeld RMA, Shea T. Time to recovery, chronicity, and levels of psychopathology in major depression – a 5-year prospective follow-up of 431 subjects. Archives of General Psychiatry. 1992;49:809–816. doi: 10.1001/archpsyc.1992.01820100053010. [DOI] [PubMed] [Google Scholar]
- Keller MB, McCullough JP, Klein DN, Arnow B, Dunner DL, Gelenberg AJ, Markowitz JC, Nemeroff CB, Russell JM, Thase ME, Trivedi MH, Zajecka J, Blalock JA, Borian FE, Jody DN, DeBattista C, Koran LM, Schatzberg AF, Fawcett J, Hirschfeld RMA, Keitner G, Miller I, Kocsis JH, Kornstein SG, Manber R, Ninan PT, Rothbaum B, Rush AJ, Vivian D, Rothbaum B. A comparison of nefazodone, the cognitive behavioral-analysis system of psychotherapy, and their combination for the treatment of chronic depression. New England Journal of Medicine. 2000;342:1462–1470. doi: 10.1056/NEJM200005183422001. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Berglund P, Demler O, Jin R, Koretz D, Merikangas KR, Rush AJ, Walters EE, Wang PS. The epidemiology of major depressive disorder : results from the National Comorbidity Survey Replication (NCS-R) JAMA. 2003;289:3095–3105. doi: 10.1001/jama.289.23.3095. [DOI] [PubMed] [Google Scholar]
- Kocsis JH, Frances AJ, Voss C, Mason BJ, Mann JJ, Sweeney J. Imipramine and social-vocational adjustment in chronic depression. American Journal of Psychiatry. 1988;145:997–999. doi: 10.1176/ajp.145.8.997. [DOI] [PubMed] [Google Scholar]
- Leff J, Vearnals S, Brewin CR, Wolff G, Alexander B, Asen E, Dayson D, Jones E, Chisholm D, Everitt B. The London Depression Intervention Trial. Randomised controlled trial of antidepressants v. couple therapy in the treatment and maintenance of people with depression living with a partner : clinical outcome and costs. British Journal of Psychiatry. 2000;177:95–100. doi: 10.1192/bjp.177.2.95. [DOI] [PubMed] [Google Scholar]
- Logsdon MC, Wisner K, Hanusa BH, Phillips A. Role functioning and symptom remission in women with postpartum depression after antidepressant treatment. Archives of Psychiatric Nursing. 2003;17:276–283. doi: 10.1053/j.apnu.2003.10.004. [DOI] [PubMed] [Google Scholar]
- McCullough JP. Treatment for Chronic Depression : Cognitive Behavioral Analysis System of Psychotherapy (CBASP) New York: Guilford Press; 2000. [DOI] [PubMed] [Google Scholar]
- McLeod JD. Spouse concordance for depressive disorders in a community sample. Journal of Affective Disorders. 1993;27:43–52. doi: 10.1016/0165-0327(93)90096-3. [DOI] [PubMed] [Google Scholar]
- Miller IW, Keitner GI, Schatzberg AF, Klein DN, Thase ME, Rush AJ, Markowitz JC, Schlager DS, Kornstein SG, Davis SM, Harrison WM, Keller MB. The treatment of chronic depression, part 3: Psychosocial functioning before and after treatment with sertraline or imipramine. Journal of Clinical Psychiatry. 1998;59:608–619. doi: 10.4088/jcp.v59n1108. [DOI] [PubMed] [Google Scholar]
- Murphy SA, Oslin DW, Rush AJ, Zhu J. Methodological challenges in constructing effective treatment sequences for chronic psychiatric disorders. Neuropsychopharmacology. 2007;32:257–262. doi: 10.1038/sj.npp.1301241. [DOI] [PubMed] [Google Scholar]
- O’Leary KD, Beach SR. Marital therapy : a viable treatment for depression and marital discord. American Journal of Psychiatry. 1990;147:183–186. doi: 10.1176/ajp.147.2.183. [DOI] [PubMed] [Google Scholar]
- Papakostas GT, Petersen T, Denninger JW, Tossani E, Pava JA, Alpert JE, Nierenberg AA, Fava M. Psychosocial functioning during the treatment of major depressive disorder with fluoxetine. Journal of Clinical Psychopharmacology. 2004;24:507–511. doi: 10.1097/01.jcp.0000138761.85363.d5. [DOI] [PubMed] [Google Scholar]
- Reimherr FW, Strong RE, Marchant BK, Hedges DW, Wender PH. Factors affecting return of symptoms 1 year after treatment in a 62-week controlled study of fluoxetine in major depression. Journal of Clinical Psychiatry. 2001;62:16–23. [PubMed] [Google Scholar]
- Rush AJ, Bernstein IH, Trivedi MH, Carmody TJ, Wisniewski S, Mundt JC, Shores-Wilson K, Biggs MM, Woo A, Nierenberg AA, Fava M. An evaluation of the quick inventory of depressive symptomatology and the Hamilton rating scale for depression : a Sequenced Treatment Alternatives to Relieve Depression Trial report. Biological Psychiatry. 2006a;59:493–501. doi: 10.1016/j.biopsych.2005.08.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rush AJ, Blacker D, First MB. Handbook of Psychiatric Measures. Washington, DC: American Psychiatric Association; 2007. [Google Scholar]
- Rush AJ, Gullion CM, Basco MR, Jarrett RB, Trivedi MH. The Inventory of Depressive Symptomatology (IDS) : psychometric properties. Psychological Medicine. 1996;26:477–486. doi: 10.1017/s0033291700035558. [DOI] [PubMed] [Google Scholar]
- Rush AJ, Trivedi MH, Ibrahim HM, Carmody TJ, Arnow B, Klein DN, Markowitz JC, Ninan PT, Kornstein S, Manber R, Thase ME, Kocsis JH, Keller MB. The 16-item Quick Inventory of Depressive Symptomatology (QIDS), clinician rating (QIDS-C), and self-report (QIDS-SR) : a psychometric evaluation in patients with chronic major depression. Biological Psychiatry. 2003;54:573–583. doi: 10.1016/s0006-3223(02)01866-8. erratum 585. [DOI] [PubMed] [Google Scholar]
- Rush AJ, Trivedi MH, Wisniewski SR, Nierenberg AA, Stewart JW, Warden D, Niederehe G, Thase ME, Lavori PW, Lebowitz BD, McGrath PJ, Rosenbaum JF, Sackeim HA, Kupfer DJ, Luther J, Fava M. Acute and longer-term outcomes in depressed outpatients requiring one or several treatment steps : a STAR*D report. American Journal of Psychiatry. 2006b;163:1905–1917. doi: 10.1176/ajp.2006.163.11.1905. [DOI] [PubMed] [Google Scholar]
- Trivedi MH, Rush AJ, Ibrahim HM, Carmody TJ, Biggs MM, Suppes T, Crismon ML, Shores-Wilson K, Toprac MG, Dennehy EB, Witte B, Kashner TM. The Inventory of Depressive Symptomatology, Clinician Rating (IDS-C) and Self-Report (IDS-SR), and the Quick Inventory of Depressive Symptomatology, Clinician Rating (QIDS-C) and Self-Report (QIDS-SR) in public sector patients with mood disorders : a psychometric evaluation. Psychological Medicine. 2004;34:73–82. doi: 10.1017/s0033291703001107. [DOI] [PubMed] [Google Scholar]
- Vittengl JR, Clark LA, Jarrett RB. Improvement in social-interpersonal functioning after cognitive therapy for recurrent depression. Psychological Medicine. 2004;34:643–658. doi: 10.1017/S0033291703001478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weissman MM, Paykel ES. The Depressed Woman: A Study of Social Relationships. Chicago: University of Chicago Press; 1974. [Google Scholar]
- Weissman MM, Prusoff BA, Thompson WD, Harding PS, Myers JK. Social adjustment by self-report in a community sample and in psychiatric outpatients. Journal of Nervous and Mental Disease. 1978;166:317–326. doi: 10.1097/00005053-197805000-00002. [DOI] [PubMed] [Google Scholar]
- Wells KB, Burnam MA, Rogers W, Hays R, Camp P. The course of depression in adult outpatients : results from the Medical Outcomes Study. Archives of General Psychiatry. 1992;49:788–794. doi: 10.1001/archpsyc.1992.01820100032007. [DOI] [PubMed] [Google Scholar]
- Whisman MA. The association between depression and marital dissatisfaction. In: Beach SRH, editor. Marital and Family Processes in Depression : A Scientific Foundation for Clinical Practice. Washington, DC: American Psychological Association; 2001a. pp. 3–24. [Google Scholar]
- Whisman MA. Marital adjustment and outcome following treatments for depression. Journal of Consulting and Clinical Psychology. 2001b;69:125–129. doi: 10.1037//0022-006x.69.1.125. [DOI] [PubMed] [Google Scholar]
- Whisman MA, Uebelacker LA, Weinstock LM. Psychopathology and marital satisfaction : the importance of evaluating both partners. Journal of Consulting and Clinical Psychology. 2004;72:830–838. doi: 10.1037/0022-006X.72.5.830. [DOI] [PubMed] [Google Scholar]
- Wolfinger R, O’Connell M. Generalized linear mixed models: a pseudo-likelihood approach. Journal of Statistical Computation and Simulation. 1993;48:233–243. [Google Scholar]