Abstract
Research on the psychological development of persons with Disorders of Sex Development (DSD) has focused on understanding the influence of atypical sex hormone exposure during steroid-sensitive periods of prenatal brain development on the process of psychosexual differentiation (i.e., gender identity, gender role, and sexual orientation). In contrast, analysis of clinical management strategies has focused on gender assignment and the desirability and timing of genital surgery.
This review focuses on the psychological issues that confront clinicians managing the care of persons born with DSD and their families. Particular attention is paid to processes and factors that potentially mediate or moderate psychosocial and psychosexual outcomes within and across developmental stages.
Keywords: disorders of sex development, DSD, psychosocial, psychosexual, gender identity, gender role, sexual orientation
As in other chronic pediatric conditions, accurate diagnosis and delivering appropriate medical and surgical treatment are central aspects of best practices in the clinical management of disorders of sex development (DSD); nevertheless, and potentially more than in other congenital conditions, the affected person’s health-related quality of life (HRQoL) and adaptation of the family will also depend on the extent to which healthcare providers attend to psychosocial aspects of the condition. Psychology, particularly research in developmental psychology, guides our approach.
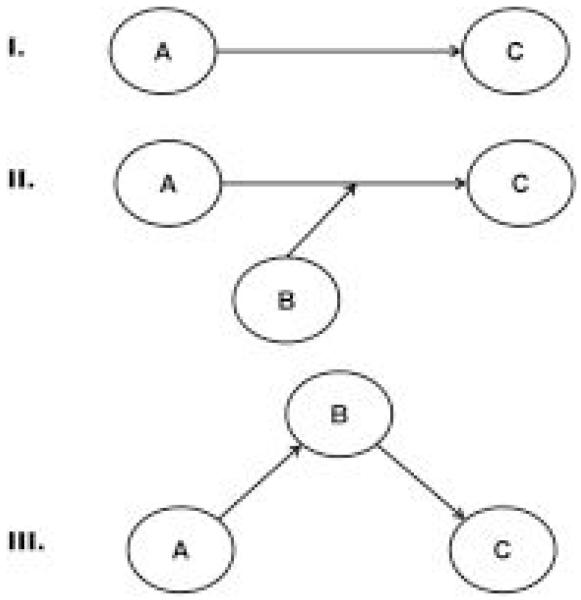
A commonly adopted model for understanding HRQoL outcomes in DSD is one in which assigning the “right” diagnosis and providing the “best” medical or surgical treatment(s) are viewed as the exclusive predictors of positive HRQoL ([Fig. 1: I]). Ultimately, a linear model in which outcomes are hypothesized to be directly determined by biological factors and/or medical/surgical interventions proves to be an oversimplification that leaves substantial variability in endpoints unaccounted for. Moreover, an exclusive focus on biological and medical/surgical aspects of DSD limits theory development and impedes innovation in clinical management strategies. Instead, and consistent with commonly adopted paradigms in developmental psychology, psychopathology and theory in gender development,[1][2] we propose adopting conceptual models that consider the potential influences of moderating ([Fig. 1: II]) and mediating variables ([Fig. 1: III]). In addition to this approach more accurately reflecting the complexity of psychological development, it offers the benefit of studying DSD within the mainstream of clinical research and theory development in pediatric psychology.
Figure 1.
Conceptual models for direct, mediated and moderated developmental effects.
I. Simple or direct effect model: single predictor (A) directly related to a single outcome (C) II. When the relationship between predictor (A) and outcome (C) is thought to be either buffered or intensified by another factor (C), then a suitable model is one that tests for moderation. III. A mediation model posits that the predictor (A) influences another variable (B) which, in turn, is more directly responsible for the outcome (C).
In cases in which gender assignment is in question, or gender reassignment is under consideration, decision making needs to be informed by both developmental and clinical psychology. The necessity of psychological counseling also emerges in the context of decisions about the timing of interventions, education of the patient and others about medical history (i.e., disclosure), management of potential psychosocial or educational problems that emerge for the child, or when parents need support in understanding the etiology of the child’s condition and its implications. The importance of these aspects of care is reflected by the increasing participation of mental health professionals in multidisciplinary DSD teams.[3][4][5]
This paper focuses on the psychological issues that confront clinicians managing the care of persons born with DSD and their families. Particular attention is paid to processes and factors that potentially mediate or moderate outcomes (broadly defined) within and across developmental stages.
Prenatal Period
Identifying and clinically managing DSD can begin before a child is born. Expectations of the family and healthcare providers regarding the somatic sex of the child are increasingly driven by advances in technology; for example, remarkably clear ultrasound images[6] and genetic testing that can noninvasively and reliably ascertain fetal chromosomal sex between 7 and 12 weeks[7] are widely available in industrialized countries. Discordance between prenatal test findings (e.g., genital appearance by ultrasound and karyotype) can initiate the DSD counseling process even at this early stage. Evidence from studies of prenatal diagnostic counseling suggests that termination of a pregnancy is dependent upon the professional background of the healthcare provider delivering post-diagnostic counseling.[8][9][10] There is substantial variation in healthcare providers’ knowledge regarding DSD. Because these conditions are rare and, historically, understudied and misunderstood, parents are at risk of receiving outdated or incomplete information unless major efforts are made in the context of interdisciplinary care teams.
Beyond diagnosis, the prenatal period has seen efforts at medical intervention to avert phenotypic changes associated with DSD; a case in point is prenatal suppression of adrenal androgens that masculinize the genitalia in 46, XX congenital adrenal hyperplasia (CAH). CAH comprises a family of autosomal recessive disorders involving impaired synthesis of cortisol. In 21-hydroxylase deficiency (21-OH CAH), the most common form comprising as many as 95% of new cases, excessive adrenal androgen biosynthesis results in masculinization of the genitals of 46, XX offspring.[11] If a woman has previously had a child with CAH and again becomes pregnant with the same partner (assuming both are carriers), the fetus has a one in four chance of acquiring the genotype associated with CAH. Suppression of fetal adrenal androgens in CAH is achievable by administering glucocorticoids (dexamethasone, DEX) during the pregnancy.[12] The goal is to reduce genital masculinization of female offspring and obviate the need for reconstructive surgery and presumed distress associated with the birth of a child with atypical genitalia.
Criticism of this intervention centers around several issues: first, the treatment is experimental and, yet, not characteristically delivered in the context of a clinical trial with necessary human subject oversight as called for in CAH practice guidelines[13][14]; second, to be effective, DEX treatment must be initiated between gestational weeks 6 to 7 and before it can be determined whether the fetus carries the CAH gene mutation. Treatment continues until chorionic villi sampling can be employed for genotyping. If the fetus is 46, XY or 46, XX without the CAH genotype, then treatment is discontinued. Accordingly, 7 out of 8 fetuses (all 46, XY and three out of four 46, XX) gain no benefit from the treatment but are exposed to potential risks; third, the safety of prenatal DEX for outcomes such as metabolism, cognitive function and behavioral-emotional adaptation is in question based on animal experimental and human clinical research[15][16][17][18][19][20][21]; fourth, prenatal treatment does not change the need for lifelong glucocorticoid replacement therapy, the need for careful medical monitoring, or the risk of life-threatening salt-losing crises if treatment adherence is poor. Finally, concern over prenatal DEX treatment has been expressed by bioethicists who have questioned whether treatment introduced to “normalize” genital anatomy is confounded with the goal of making gender-role behavior and sexual orientation more typical.[13]
Opportunities for systematic research and theory development that examine the influence of timing of diagnosis (prenatal versus later) on treatment choices (e.g., gender assignment, genital surgery, etc.) and HRQoL outcomes for patients and families are as yet untapped.
The Neonatal Period and Infancy
The presence at birth of a congenital anomaly affecting a child’s genital appearance or future reproductive function can engender a “psychosocial emergency” for parents and healthcare providers. Atypical genital anatomy may represent, for both the clinician and family, the most challenging aspect of otherwise complex and even life-threatening conditions (most notably classic CAH). It is in this context, shortly following birth, that major (some irreversible) decisions are made, including gender assignment and urogenital surgery.
Family-centered strategies for clinical care are particularly important as family attitude and function are widely acknowledged to affect medical and surgical decisions as well as the psychosocial development of children diagnosed with a variety of medical conditions.[22] To optimally counsel parents, mental health providers need to take into account parents’ capacity to manage uncertainty regarding psychosocial and psychosexual outcomes as the child develops. Family and cultural factors[3][23] will also likely play an important role in the perceptions of the child’s condition and interpretation of complex medical and genetic information. The challenge for mental health providers is to educate parents in a balanced manner about the genetic and biologic origins of the DSD and its implications for their child’s physical health and HRQoL that positions them to make informed decisions regarding elective interventions, for example, genital surgery.
Psychological Aspects of Gender Assignment
Parents may experience shock if the biological sex of their newborn is not immediately apparent. This is, in part, related to parents experiencing difficulty in coping with uncertainties of the child’s development. The consensus recommendation not to use gendered pronouns (“he” or “she”) as long as the gender assignment has not yet been decided, adds to this uncertainty. However, referring to the child in a way that has to be changed after the diagnosis has been made is considered even less desirable.
The 2006 DSD consensus statement,[3] states that all newborns should receive a gender assignment with the decision being informed by expert evaluation delivered by an interdisciplinary team working closely with the parents. Gender assignment decisions are typically guided by a combination of diagnosis and long-term, adult follow-up studies that focus on gender identity stability and other psychosexual outcomes (e.g.,[24][25][26][27]). “Gender identity” refers to a person’s inner sense of being a boy/man or girl/woman.[28] Unfortunately, for some DSD, adult gender identity cannot confidently be predicted.[29][30][31][32] This is because there is still little known about the relative contribution of biological (e.g., genes, prenatal sex hormone exposure) and non-biological influences (e.g., parental attitude, peer influences, cultural context) on gender identity development and stability. Critical stages in the development or potential interactions of the various factors are also unclear.
Psychosexual outcomes in DSD have been most extensively studied in 46, XX CAH.[33] These studies show that the vast majority of those raised as girls develop and maintain a gender identity as girls/women across the lifespan. However, a less strong female identification, some gender discomfort, and even gender dysphoria occur more often in this group than in women without CAH. Reviewing studies on psychosexual outcome in DSD up to 2007, de Vries and colleagues reported that 10 of 217 (5%) of female-reared adolescent and adult women with CAH experienced some form of gender dysphoria and made a complete social gender transition (i.e., lived completely and permanently in the male role).[32] Masculine gender-role behavior among adult women was fairly common. Similarly, prepubertal girls with CAH exhibited more masculine and less feminine interests, behaviors and preferences than girls without CAH. Gender-atypical behavior is more pronounced among CAH girls and women with the salt-wasting form of CAH than those categorized as simple virilizers.[34][35][36]
DSD that are a consequence of errors of androgen biosynthesis have historically been particularly challenging from the standpoint of gender assignment. Long-term outcome studies of persons with 46, XY 5-α-reductase type 2 deficiency (5α-RD-2) and 17β-hydroxysteroid dehydrogenase 3 (17β-HSD-3), suggest that large proportions of those reared as girls, subsequently identify as men if they are allowed to experience a spontaneous masculinizing puberty. Following the first observations of gender change among 5α-RD-2 individuals reared as girls in the Dominican Republic,[37] gender change was reported in 17β-HSD-3 and in other societies.[26] Gender change, however, does not always occur, even in societies that highly value the male role. In the review by de Vries et al.,[32] 69 of 117 5α-RD-2 (59%), and 20 of 51 17β-HSD-3 (39%) persons reared as girls, and all older than 12 years, experienced gender dysphoria to the extent that they decided to live as boys/men. In one study by Richter-Appelt et al,[38] five persons with 5α-RD-2 and 17β-HSD-3 reared as girls, scored significantly lower on a “female gender identity scale” than a female comparison group and one of the five also had a significantly higher male gender identity score than the female comparison group on a “male gender identity scale.”
In contrast to the common pattern of gender change from female to male in persons with 46, XY DSD secondary to errors in androgen biosynthesis, a recent report suggests a markedly different outcome. In addition to demonstrating marked variability in genital phenotype associated with alterations in the 5α-reductase type 2 gene (SRD5A2) responsible for 5α-RD-2, Maimoun and colleagues[39] reported that only 5 of 40 patients assigned female (12.5%) subsequently changed their gender to male. This proportion is remarkably lower than the 59% reported by de Vries et al.[32] Unfortunately, gaps in details provided, in particular the age of patients at the time of recording gender assignment, make it difficult to reconcile these highly discrepant observations. Whether the proportion of those affected with 5α-RD-2 that ultimately change identity from female to male is relatively large or small, information on parental rearing styles, psychosexual development, or more subtle signs of gender discomfort are essential for an understanding of the variability in gender identity outcome. Unfortunately, virtually no reports provide such information.
Persons with complete androgen insensitivity syndrome (CAIS) reared as girls, with limited exceptions,[40] develop and maintain a female gender identity throughout their lives.[25] However, there may be more variability in their gender behavior than commonly assumed: women with CAIS recruited through the United Kingdom Database of Ambiguous Genitalia and Intersex Disorders recalled more male-typical childhood toy and activity preferences than women recruited through an AIS support group. In contrast, the same registry-recruited group was more strongly heterosexual in the previous 12-month period than the AIS support group.[41] In a second study possibly signaling greater gender-atypical gender development in CAIS women than previously reported, two of five women with CAIS scored low in terms of a female gender identity.[38] Despite these greater than expected masculine interests and behavior, not one of 98 women with CAIS in the de Vries et al. review[32] reported gender dysphoria or made a social gender transition.
Gender identity shows considerably greater fluidity among persons born with partial androgen insensitivity syndrome (PAIS). In 46 female-reared adolescents and adults, 5 (11%) were gender dysphoric or started to live in the male role later in life. This percentage was even higher in the male-reared group; 5 of 35 (14%) was gender dysphoric or made a social gender transition. All gender changes took place in adulthood. In Richter-Appelt et al’s study,[31] one of three PAIS individuals reared female scored significantly lower than female controls on the “female gender identity scale.” From these studies and studies on other conditions such as penile agenesis, penile ablation, cloacal exstrophy of the bladder and micropenis,[25][27] it appears that testosterone influences the development of a male gender role and probably increases the chance of a male gender identity development. However, even in circumstances in which the person has been prenatally exposed to high levels of testosterone and reared as girls from birth, a female adult gender identity is the rule rather than the exception.[24]
Gender assignment does not pose insurmountable problems in most DSD. However, in some conditions (e.g., PAIS, 17β-HSD-3, or 5α- RD-2), the choice may be a difficult one because so little is known about postnatal events in the social environment that potentially intervene between early biological events to modulate gender identity outcomes ([Fig. 1]). For instance, should a child with 5α-RD-2 who has a complete absence of virilized external genitals be gonadectomized early to prevent a masculinizing puberty and reared as a girl? This choice would be associated with lost capacity for a spontaneous puberty, potential fertility[42] and need for lifelong androgen replacement therapy. Alternatively, if gender assigned and reared as a boy, what would be the person’s experience living with very atypical external genitals? In the decision, non-medical factors such as healthy psychological development and the potential for a good quality of life as boy/man or girl/woman, the ability of parents to cope with uncertainties, and medical factors such as surgical possibilities, potential for fertility, and need for hormone replacement need to be included. Even considering all these factors, one cannot always be completely certain that the chosen gender assignment will result in a good quality of life. Unfortunately, the evidence on quality of life outcome of adults with DSD that could be used to inform such decisions is currently scarce (e.g.,[43]).
Gender Development
Under normal circumstances, few give much thought to their gender development, as somatic sex, gender identity, and gender role typically develop in accordance with each other. A newborn does not immediately have self-awareness of his or her sex and gender. Such self-awareness evolves gradually during infancy and childhood. In the absence of discordance between aspects of sex and gender, few will reflect on their gender identity or gender role. Developmental psychology theories have attempted to account for the process of gender development, emphasizing the influences of cognitive and affective learning in interaction with parents, peers, and other aspects of the social environment.[28] Gender role refers to the pattern of masculine or feminine behavior and interests of the person that is conditioned by culture and upbringing. Long before children make consistent and systematic use of genital information as a criterion for sex classification, they have knowledge about gender stereotypes and display gender-role behavior characterized as either feminine or masculine. Adults and peers influence gender development directly by reinforcing or discouraging gender-role behaviors and indirectly by serving as role models.
Biology, however, also plays a role in the shaping of gender-role behavior. There is substantial evidence from animal and human research that sex hormones, androgens in particular, play an important role in the differentiation of gender-role behavior, gender-typed preferences, and even aspects of personality. Studies of sex-steroid levels in the blood or amniotic fluid of pregnant women and gender-related behaviors of their children have demonstrated positive associations between androgen exposure and male-typical behavior in healthy girls.[44][45][46][47] Timing, dose and type of androgen exposure seem to be important.[48] Similarly, studies of gender-role behavior in persons with DSD also suggest that sex hormone exposure during sensitive development periods play a role in the formation of behaviors exhibiting sex-related variability.[35][36][49] The influence of early sex hormone exposure on the formation of gender identity is less clear.
Genital Surgery
Questions about surgery to “normalize” genital appearance and function can arise shortly after birth. Surgeons have the responsibility to describe to families surgical options and the range of possible consequences from infancy to adulthood.[3] Although there appears to be consensus on some types of genital surgery (e.g., neonatal surgery in case of severe virilization in female-assigned children or gonadectomy in female-reared children with PAIS and CAIS[3]), decisions remain that are not obvious. Controversies regarding types of surgery and their timing remain unresolved. This is readily apparent in conditions commonly diagnosed late, such as Mayer-Rokitansky-Küster-Hauser syndrome[50] or CAIS,[51] in which older girls/women need to decide whether they will opt for vaginal surgery or dilation to create a vagina and when it is optimal to proceed based on psychological readiness. If there is not enough evidence from outcome studies that unequivocally demonstrate superiority of one approach over another, then choices depend on individual characteristics and detailed discussions with the patient (and, as applicable, the parents) regarding perceptions of advantages and disadvantages of the various choices. The goals of genital surgery and, in particular their consequences for sexual function and satisfaction need to be explicitly addressed. Naturally, the clinician who provides this counseling should feel comfortable when speaking about sexuality. Systematic decision-making aids, as developed for some conditions (see The Foundation for Informed Medical Decision Making),[52] would be very valuable, but have yet to be developed for DSD.
Information Management
Information management refers to two processes: first, the sharing of information about the DSD between clinicians, the parents and the child and second, the sharing of information about the condition by the child or family with the wider social environment. Both processes are activated to varying degrees once families are aware that their child has a DSD; this may begin with a prenatal diagnosis.
The first process often requires more than just presenting information in a clear manner. Some of the information potentially carries strong emotional implications. This is commonly the case with information about karyotype and gonadal status, especially when these results are discordant with the gender of assignment. To learn that the condition implies infertility may also pose challenges for coping. The second process, involving education of those beyond the affected person and parents, requires careful balancing of the potential advantages and disadvantages. It is still an open question whether sharing information about the DSD with the wider social environment will have positive or negative consequences for the child. Living a “normal” life with a secret could be harmful, just as living a life without secrets but with an increased risk of stigmatization or rejection. The advice currently given to parents remains largely based on clinicians’ personal opinions on what would be preferable, considering their evaluation of the family, the child, and their wider social and cultural context. Research on the effects of timing, type of information (and a potential interaction of the two), the way of conveying information, and the influence of cultural, family and child factors on how the information is managed is virtually nonexistent. Nevertheless, clinicians can find guidance in the general pediatric literature concerning physician-parent communication, especially as it relates to the sharing of “bad news.”[53]
Initial statements to parents should provide support and information. With regard to gender, healthcare providers should counsel families on differences between “gender identity,” “gender-role,” and “sexual orientation,” including general, evidence-based statements on the psychosexual development of individuals born with the child’s particular condition. The process (and not a single event) of educating the parents and the affected person requires a flexible individualized approach. Medical education and counseling for children and their families is a continuing process of gradually increasing complexity that takes into account health literacy[54] and emotional readiness. Fostering open communication between the parents and child is a high priority.[55][56][57] This iterative process should be planned with the parents from the time of diagnosis.[58]
Childhood
Major psychosocial and social-environmental aspects of DSD and its management, identified in earlier developmental stages, can re-emerge during childhood. Gender assignment and possible early reassignment will have taken place previously; however, parental questions and uncertainties may emerge if they observe their child engaging in gender-atypical play (e.g., boys playing with baby dolls or girls rough-housing). If there is a need to perform urogenital surgery beyond infancy, children require adequate preparation. The specialties of pediatric psychology[59] and child life[60] are highly useful in this context. Guidance from these members of the interdisciplinary team should be sought regarding preparation of the child and parents for genital examinations during childhood. In general, genital examinations should be kept to a minimum because of the risk that the child will recall these experiences as traumatic or contributing to a negative body image.[61][62][63]
Gender Reassignment
The age that healthcare provider/parent-imposed gender reassignment can take place without harming the child’s gender and general psychological development remains an open question. Although it is clear from developmental psychology studies in normative samples[28] that the person’s ability to cognitively identify one’s gender occurs around 30 months of age, it is not precisely known when affective aspects of gender identity develop and until what age do they remain flexible. As already noted, the process of gender development in children with DSD may follow a different pathway than in children without a DSD. Accordingly, the often mentioned age limit of 18 months is still much debated.[3]
From previously described studies, it is evident that atypical gender-role behavior is not a sign of gender identity problems. Yet, parents and healthcare providers may regard gender-role behavior that is inconsistent with the gender of rearing as an indication of gender dysphoria, causing them to question whether the gender assignment decision at birth might have been incorrect. An assessment by experienced mental health providers is indicated only if there are persistent and strong indications that gender dysphoria is present. Gender reassignment should not occur without such an assessment. The Standards of Care of the World Professional Association of Transgender Health (WPATH), a professional organization in the field of gender dysphoria, is potentially useful in guiding the assessment and treatment process.[64][65]
In the case of experienced gender dysphoria, the clinical approach includes an assessment of the gender dysphoria itself as well as an assessment of the general functioning of the child and the family. As gender-atypical behavior may be more disturbing to the social environment than to the child, the clinician needs to understand what factors (in the past or at the time of referral) may have influenced the gender-variant behavior and preferences of the child. Several standardized instruments, such as cognitive tests, parent and child questionnaires, child interviews, play observations, and projective methods are available to assess understanding of the child’s gender, behavior, and feelings.[66] Nearly all diagnostic tools and procedures, as well as the psychological interventions used in the management of gender identity disorder in physically typical children[67][68] are modifiable, with some caveats,[69] to gender-dysphoric children with DSD.
Information Management
Children will require explanations for multiple aspects of the DSD and associated clinical management. For instance, they may wonder why they need medication in childhood or hormone replacement at the beginning of puberty; why they have scars in their genital area; or why they have to visit the clinic and receive physical examinations more frequently than peers. If the child has not been adequately and timely informed, atypical gender-role behavior or sexual feelings (e.g., sexual attraction to same-gender peers) may create anxieties. They may incorrectly make inferences about their “true” sex. In circumstances in which clinical management of the DSD is associated with strong emotional responses, cognitive processing by the child of factual information provided is often less than optimal. The information is complex and not every child or parent is able to understand and recall what had been presented. Also, children’s understanding of the DSD and its personal meaning will change with each developmental stage. This suggests that the affected child (and parents) will benefit from repeated review of the facts and their implications as the child matures. By the time they reach adulthood the children should be fully informed about their condition. Unfortunately, too often patients transition to adult care without a complete understanding of their medical condition.
Developing a plan early in the course of treatment for staged, but ultimately complete sharing of information with the child is a key aspect of optimal care.[58] The plan takes into account the developmental stage of the child and opportunities which naturally present themselves in preparation for clinic visits and the questions which children inevitably ask if they perceive openness on the part of parents. Informing the child sometimes meets with resistance from parents who mistakenly believe that concealment of details will protect the children from knowledge they consider harmful. In some cultures, disclosure may be even harder to address, as conceptualizations and values regarding gender and sexuality vary greatly between cultures (e.g.,[23][70]). Yet, from other areas in medicine, it is known that being informed about one’s medical condition is associated with psychological adjustment.[54][64][70]
In comparison to children who remain uninformed, or misinformed about their condition, children who are educated in a timely manner will have better opportunities to develop adaptive coping skills, including development of a positive self-image and expectations for a fulfilling adult life despite somatic limitations (such as infertility). The requirement for older children to fully understand relevant aspects of their condition and give proper informed consent is especially important when they are required to provide assent for medical interventions.
Adolescence
In adolescence, questions may emerge or re-emerge about gender identity, gender re-assignment, and surgical intervention (e.g., some may need to know why they have to dilate the vagina or have to make decisions about genital surgery). The sharing of more detailed information with the child is an imperative during this stage which leads to transition to adult care and the need for the DSD-affected person to take responsibility for their own healthcare. Sexuality, sexual orientation and fertility are important and sensitive topics that emerge during this phase.
Gender Reassignment
In transgender (i.e., physically typical at birth) adolescents and adults experiencing gender dysphoria, the gender reassignment decision is taken in phases. In the first, diagnostic phase, it has to be established that the person fulfills DSM or ICD criteria for the diagnoses “gender identity disorder” or “transsexualism” and that the person is physically and psychologically ready to undergo gender reassignment. The next phase usually consists of receiving hormones of the desired gender and social transitioning. Undergoing surgery to change the genitals and sometimes other somatic sex characteristics is typically the last phase of the treatment. In some cases, however, the sequence may be changed, depending on the needs of the individual (e.g., large breasts of a person who is going to live in the male role). In case of gender dysphoric individuals with DSD, specific attention has to be paid to limitations of the treatment. In cases of female-reared individuals who choose to live as males, the hormones may not be completely virilizing and previous operations may limit surgical options. If the person is confused about their gender or seeks gender reassignment for reasons other than a gender identity that does not match their assigned gender, psychological interventions in lieu of hormonal or surgical gender reassignment are indicated. In either case, persons with DSD will benefit from the opportunity to engage in psychological counseling to address commonly experienced apprehensiveness over the ability to form romantic and satisfying sexual relationships.
A very useful part of the gender reassignment procedure is what was previously called the “real-life experience” phase. In this phase, one lives full-time in the desired gender role to tryout, on a daily basis, what it is like to live in the desired gender before one makes irreversible change.[64] In this phase the person’s feelings about the social transition, including coping with the responses of others, is a major focus of the discussions and counseling. In gender dysphoric adolescents without DSD, one option is to suppress puberty by using gonadotropin-releasing hormone analogues. This reversible treatment is meant to provide the adolescent time to consider gender reassignment without experiencing development of secondary sex characteristics (see[64] for a review). In contrast to these adolescents, agonadal adolescents with DSD do not need suppression of puberty. If they are gender dysphoric but not yet certain on whether want to pursue a gender reassignment, they may profit from a delay in the start of hormone replacement therapy.
Feminizing/masculinizing hormone therapy (estrogens/anti-androgens/progestins for male-to-females, androgens for female-to-males) is considered only partially reversible, as some of the changes persist even if hormone therapy is discontinued. Some changes (breast growth in natal males, low pitched voice and facial hair growth in natal females) require surgery or other treatment to “reverse.” Feminizing/masculinizing hormone therapy typically does not begin until a gender-dysphoric adolescent without DSD is 16 years or older.[64] Because of the differences between DSD and non-DSD conditions, and the wide variation in DSD conditions, general age requirements for initiating these hormones do not exist for adolescents with DSD who seek to change gender.
Gender reassignment surgery is rarely performed prior to adulthood in non-DSD children and adolescents. There is international clinical consensus that the risks of early surgical intervention outweigh the potential benefits in most cases. Surgical feminization/masculinization procedures are explained in detail in a document, “Care of the Patient Undergoing Sex Reassignment Surgery.”[64] Again, considering the differences between the conditions, this age restriction is not necessarily directly applicable to adolescents with DSD.
Sexuality
When entering puberty, some adolescents with DSD may develop anxieties. Repeated genital exams and medical photography, treatment by clinicians experienced as disrespectful, or an atypical genital appearance are particularly anxiety provoking. After entering puberty, some feel increasingly uncertain about their masculinity/femininity, sexual adequacy, or sexual orientation. They often postpone initiating intimate relationships because of such insecurities and fear of rejection. Sexual problems indeed occur more often in DSD than non-DSD groups.[64][71][72] For instance, the sexual lives of women with CAH differ from control groups in terms of timing of psychosexual milestones (delayed), sexual experiences (less), sexual activity and imagery (less), sexual motivation (less), partnership and marriage (less), and sexual self-image (less favorable)[73][74][75] and the sexual orientation of women with CAH is more often homosexual as compared with the general population.[75][76] Various sexual problems and an elevated percentage of non-heterosexuality were reported in women with enzyme deficiencies,[72] but systematic studies in larger groups are lacking. In one study, sexual problems, primarily low sexual desire and inability to become sexually aroused and experience orgasm, were reported by women with CAIS, whereas most women with PAIS feared to have sexual contact and had experienced dyspareunia or fear of becoming hurt through sexual contact. In the latter group, an elevation of non-heterosexuality was also found.[72]
Comprehensive sex education together with timely preparation for romantic and sexual relationships can contribute to a positive HRQoL. Adolescents should have the opportunity to discuss their concerns repeatedly, and in private, with a mental health clinician.
Summary
It has hopefully become apparent to the reader of this review that direct effect conceptual models ([Fig. 1.I]) designed to account for the course of psychological development of persons born with DSD are certain to oversimplify the process and mislead both researchers and healthcare providers. Instead, more complex models—developmental pathways—reflecting the sorts of influences and choices described in the sections above will hopefully generate novel ideas and strategies to enhance HRQoL outcomes in DSD. As noted by Pickles and Hill[2]:
The developmental pathway is a remarkably productive metaphor. … At its simplest, the idea of a pathway suggests a route that is traveled over time, in which there are constraints over the directions the traveler can take, and there is an ordered sequence of events or experiences… if we envisage a traveler (walker) taking one of a number of possible pathways over a changing terrain, for example, encompassing relatively easy walking before climbing up steep mountain paths… If developmental pathways resemble such physical paths, we can make predictions, such as that there will be phases of the journey where the path taken by an individual is highly predictable but punctuated by points at which choices are made among different paths…. The pathway metaphor also provokes ideas regarding mechanisms in development. For example, there are multiple ways in which decisions regarding which path to take can be made. They can be based on an overview of the ultimate aim or destination of the journey…or they may be determined by immediate factors, such as whether the visible path looks easy or difficult. A path may be chosen because it is desirable, or because it is the only one remaining after others have been rejected, for example, because they seem too risky. Decisions at any one point are also influenced by the cumulative effects of the journey on the traveler. The weary walker is likely to choose the easier path! Furthermore, the choice of path may be the result of the joint effects of such different mechanisms and may vary as the path is traversed. (pp. 212-13).
The “pathway” metaphor can be as productive for studying the psychological development of persons with DSD as it has been in the much broader field of child development and developmental psychopathology. It is easy to imagine how decisions made by parents for or against early surgery, for example, might alter the path the person with a DSD takes on their personal journey. By studying a large number of people with DSD for whom different decisions were made, or who themselves made varying choices when older, it may be possible to create a “taxonomy of travelers.”[2]
Finally, an additional thought about the role of the mental health provider member of the healthcare team: in addition to their contribution as educator and counselor regarding the psychological aspects of DSD, the mental health provider is potentially in a unique position among all the members of the team to facilitate the group process within the team and between the team and the family. The extensive business literature on team performance and organizational development has been extended to healthcare and the function of interdisciplinary teams.[77][78][79][80] Among all the healthcare specialists on the DSD, the mental health provider is most likely the one who has been exposed to the concepts and received training in managing these processes.
Acknowledgments
This work was supported, in part, by grants from the Eunice Kennedy Shriver National Institute of Child Health and Human Development (R01HD053637 and R01HD068138). The content is solely the responsibility of the author and does not necessarily represent the official views of the Eunice Kennedy Shriver National Institute of Child Health and Human Development of the National Institutes of Health.
Contributor Information
David E. Sandberg, Division of Child Behavioral Health, Department of Pediatrics & Communicable Diseases, University of Michigan, Ann Arbor, MI
Melissa Gardner, Division of Child Behavioral Health, Department of Pediatrics & Communicable Diseases, University of Michigan, Ann Arbor, MI.
Peggy T. Cohen-Kettenis, Division of Gender and Sexuality, Department of Medical Psychology and Medical Social Work, VU University medical Center, Amsterdam, the Netherlands
References
- 1.Crouter AC, Manke BA, McHale SM. The family context of gender intensification in early adolescence. Child Dev. 1995;66(2):317–329. doi: 10.1111/j.1467-8624.1995.tb00873.x. [DOI] [PubMed] [Google Scholar]
- 2.Pickles A, Hill J. Developmental psychopathology. In: Cicchetti D, Cohen D, editors. Developmental psychopathology Theory and method. 2nd ed. John Wiley & Sons, Inc; Hoboken, New Jersey: 2006. pp. 211–43. [Google Scholar]
- 3.Lee PA, Houk CP, Ahmed SF, Hughes IA. International Consensus Conference on Intersex organized by the Lawson Wilkins Pediatric Endocrine Society and the European Society for Paediatric Endocrinology. Consensus statement on management of intersex disorders. Pediatrics. 2006;118(2):e488–e500. doi: 10.1542/peds.2006-0738. [DOI] [PubMed] [Google Scholar]
- 4.Pasterski V, Prentice P, Hughes IA. Consequences of the Chicago consensus on disorders of sex development (DSD): current practices in Europe. Arch Dis Child. 2010;95(8):618–623. doi: 10.1136/adc.2009.163840. [DOI] [PubMed] [Google Scholar]
- 5.Ahmed SF, Achermann JC, Arlt W, et al. UK guidance on the initial evaluation of an infant or an adolescent with a suspected disorder of sex development. Clinical Endocrinology (Oxf.) 2011;75:12–26. doi: 10.1111/j.1365-2265.2011.04076.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chitayat D, Glanc P. Diagnostic approach in prenatally detected genital abnormalities. Ultrasound Obstet Gynecol. 2010;35(6):637–646. doi: 10.1002/uog.7679. [DOI] [PubMed] [Google Scholar]
- 7.Devaney SA, Palomaki GE, Scott JA, Bianchi DW. Noninvasive fetal sex determination using cell-free fetal DNA: a systematic review and meta-analysis. JAMA. 2011;306(6):627–636. doi: 10.1001/jama.2011.1114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Marteau TM, Nippert I, Hall S, et al. DADA Study Group Decision-making after diagnosis of fetal abnormality.Outcomes of pregnancies diagnosed with Klinefelter syndrome: the possible influence of health professionals. Prenat Diagn. 2002;22(7):562–566. doi: 10.1002/pd.374. [DOI] [PubMed] [Google Scholar]
- 9.Abramsky L, Hall S, Levitan J, Marteau TM. What parents are told after prenatal diagnosis of a sex chromosome abnormality: interview and questionnaire study. BMJ. 2001;322(7284):463–466. doi: 10.1136/bmj.322.7284.463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Girardin CM, Van Vliet G. Counselling of a couple faced with a prenatal diagnosis of Klinefelter syndrome. Acta Paediatr. 2011;100(6):917–922. doi: 10.1111/j.1651-2227.2011.02156.x. [DOI] [PubMed] [Google Scholar]
- 11.Speiser PW, White PC. Congenital adrenal hyperplasia. N Engl J Med. 2003;349(8):776–788. doi: 10.1056/NEJMra021561. [DOI] [PubMed] [Google Scholar]
- 12.Evans MI, Chrousos GP, Mann DW, et al. Pharmacologic suppression of the fetal adrenal gland in utero. Attempted prevention of abnormal external genital masculinization in suspected congenital adrenal hyperplasia. JAMA. 1985;253(7):1015–1020. [PubMed] [Google Scholar]
- 13.Dreger A, Feder E, Tamar-Mattis A. [Accessed July 15, 2010];Preventing Homosexuality (and Uppity Women) in the Womb? Bioethics Forum. 2010 http://www.thehastingscenter.org/Bioethicsforum/Post.aspx?id=4754&blogid=140&terms=dreger+and+%23filename+*.html.
- 14.Speiser PW, Azziz R, Baskin LS, et al. Endocrine Society. Congenital adrenal hyperplasia due to steroid 21-hydroxylase deficiency: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2010;95(9):4133–4160. doi: 10.1210/jc.2009-2631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Matthews SG. Antenatal glucocorticoids and the developing brain: mechanisms of action. Semin Neonatol. 2001;6(4):309–317. doi: 10.1053/siny.2001.0066. [DOI] [PubMed] [Google Scholar]
- 16.Murphy KE, Hannah ME, Willan AR, et al. MACS Collaborative Group. Multiple courses of antenatal corticosteroids for preterm birth (MACS): a randomised controlled trial. Lancet. 2008;372(9656):2143–2151. doi: 10.1016/S0140-6736(08)61929-7. [DOI] [PubMed] [Google Scholar]
- 17.Lajic S, Nordenström A, Hirvikoski T. Long-Term Outcome of Prenatal Treatment of Congenital Adrenal Hyperplasia. Endocrine Development. In: Flück C, Miller W, editors. Disorders of the Human Adrenal Cortex. Karger; Basel: 2008. pp. 82–98. [DOI] [PubMed] [Google Scholar]
- 18.Huang WL, Beazley LD, Quinlivan JA, Evans SF, Newnham JP, Dunlop SA. Effect of corticosteroids on brain growth in fetal sheep. Obstet Gynecol. 1999;94(2):213–218. doi: 10.1016/s0029-7844(99)00265-3. [DOI] [PubMed] [Google Scholar]
- 19.Hirvikoski T, Lindholm T, Lajic S, Nordenström A. Gender role behaviour in prenatally dexamethasone-treated children at risk for congenital adrenal hyperplasia—a pilot study. Acta Paediatr. 2011;100(9):e112–e119. doi: 10.1111/j.1651-2227.2011.02260.x. [DOI] [PubMed] [Google Scholar]
- 20.Hirvikoski T, Nordenström A, Lindholm T, et al. Cognitive functions in children at risk for congenital adrenal hyperplasia treated prenatally with dexamethasone. J Clin Endocrinol Metab. 2007;92(2):542–548. doi: 10.1210/jc.2006-1340. [DOI] [PubMed] [Google Scholar]
- 21.Trautman PD, Meyer-Bahlburg HF, Postelnek J, New MI. Effects of early prenatal dexamethasone on the cognitive and behavioral development of young children: results of a pilot study. Psychoneuroendocrinology. 1995;20(4):439–449. doi: 10.1016/0306-4530(94)00070-0. [DOI] [PubMed] [Google Scholar]
- 22.Kazak AE, Rourke MT, Crump TA, Roberts MC. Handbook of pediatric psychology. Guildford Press; New York, NY: 2003. Families and other systems in pediatric psychology; pp. 159–75. [Google Scholar]
- 23.Warne GL, Raza J. Disorders of sex development (DSDs), their presentation and management in different cultures. Rev Endocr Metab Disord. 2008;9(3):227–236. doi: 10.1007/s11154-008-9084-2. [DOI] [PubMed] [Google Scholar]
- 24.Dessens AB, Slijper FME, Drop SLS. Gender dysphoria and gender change in chromosomal females with congenital adrenal hyperplasia. Arch Sex Behav. 2005;34(4):389–397. doi: 10.1007/s10508-005-4338-5. [DOI] [PubMed] [Google Scholar]
- 25.Mazur T. Gender dysphoria and gender change in androgen insensitivity or micropenis. Arch Sex Behav. 2005;34(4):411–421. doi: 10.1007/s10508-005-4341-x. [DOI] [PubMed] [Google Scholar]
- 26.Cohen-Kettenis PT. Gender change in 46,XY persons with 5α-reductase-2 deficiency and 17β-hydroxysteroid dehydrogenase-3 deficiency. Arch Sex Behav. 2005;34(4):399–410. doi: 10.1007/s10508-005-4339-4. [DOI] [PubMed] [Google Scholar]
- 27.Meyer-Bahlburg HFL. Gender identity outcome in female-raised 46,XY persons with penile agenesis, cloacal exstrophy of the bladder, or penile ablation. Arch Sex Behav. 2005;34(4):423–438. doi: 10.1007/s10508-005-4342-9. [DOI] [PubMed] [Google Scholar]
- 28.Ruble D, Martin C, Berenbaum S. Gender development. In: Damon W, Lerner R, Eisenberg N, editors. Handbook of child psychology: Social, emotional, and personality. 6ed. Wiley; New York: 2006. pp. 858–932. [Google Scholar]
- 29.Berenbaum SA. Psychological outcome in children with disorders of sex development: implications for treatment and understanding typical development. Annu Rev Sex Res. 2006;17:1–38. [Google Scholar]
- 30.Cohen-Kettenis P. Psychological long-term outcome in intersex conditions. Horm Res. 2005;64(Suppl. 02):27–30. doi: 10.1159/000087750. [DOI] [PubMed] [Google Scholar]
- 31.Richter-Appelt H, Discher C, Gedrose B. Gender identity and recalled gender related childhood play-behaviour in adult individuals with different forms of intersexuality. Anthropol Anz. 2005;63(3):241–256. [PubMed] [Google Scholar]
- 32.de Vries AL, Doreleijers TA, Cohen-Kettenis PT. Disorders of sex development and gender identity outcome in adolescence and adulthood: understanding gender identity development and its clinical implications. Pediatr Endocrinol Rev. 2007;4(4):343–351. [PubMed] [Google Scholar]
- 33.Stout SA, Litvak M, Robbins NM, Sandberg DE. Congenital Adrenal Hyperplasia: Classification of studies employing psychological endpoints. International Journal of Pediatric Endocrinology. 2010 doi: 10.1155/2010/191520. 2010(doi:10.1155/2010/191520):11 pages. http://www.hindawi.com/journals/ijpe/2010/191520/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Meyer-Bahlburg HF, Dolezal C, Baker SW, Ehrhardt AA, New MI. Gender development in women with congenital adrenal hyperplasia as a function of disorder severity. Arch Sex Behav. 2006;35(6):667–684. doi: 10.1007/s10508-006-9068-9. [DOI] [PubMed] [Google Scholar]
- 35.Frisén L, Nordenström A, Falhammar H, et al. Gender role behavior, sexuality, and psychosocial adaptation in women with congenital adrenal hyperplasia due to CYP21A2 deficiency. J Clin Endocrinol Metab. 2009;94(9):3432–3439. doi: 10.1210/jc.2009-0636. [DOI] [PubMed] [Google Scholar]
- 36.Nordenström A, Servin A, Bohlin G, Larsson A, Wedell A. Sex-typed toy play behavior correlates with the degree of prenatal androgen exposure assessed by CYP21 genotype in girls with congenital adrenal hyperplasia. J Clin Endocrinol Metab. 2002;87(11):5119–5124. doi: 10.1210/jc.2001-011531. [DOI] [PubMed] [Google Scholar]
- 37.Imperato-McGinley J, Guerrero L, Gautier T, Peterson RE. Steroid 5alpha-reductase deficiency in man: an inherited form of male pseudohermaphroditism. Science. 1974;186(4170):1213–1215. doi: 10.1126/science.186.4170.1213. [DOI] [PubMed] [Google Scholar]
- 38.Richter-Appelt H, Discher C, Gedrose B. Gender identity and recalled gender related childhood play-behaviour in adult individuals with different forms of intersexuality. Anthropol Anz. 2005;63:241–256. [PubMed] [Google Scholar]
- 39.Maimoun L, Philibert P, Cammas B, et al. Phenotypical, biological, and molecular heterogeneity of 5α-reductase deficiency: an extensive international experience of 55 patients. J Clin Endocrinol Metab. 2011;96(2):296–307. doi: 10.1210/jc.2010-1024. [DOI] [PubMed] [Google Scholar]
- 40.T’Sjoen G, De Cuypere G, Monstrey S, et al. Male gender identity in complete androgen insensitivity syndrome. Archives of Sexual Behavior. 2011;40(3):635–638. doi: 10.1007/s10508-010-9624-1. [DOI] [PubMed] [Google Scholar]
- 41.Hines M, Ahmed SF, Hughes IA. Psychological outcomes and gender-related development in complete androgen insensitivity syndrome. Arch Sex Behav. 2003;32(2):93–101. doi: 10.1023/a:1022492106974. [DOI] [PubMed] [Google Scholar]
- 42.Matsubara K, Iwamoto H, Yoshida A, Ogata T. Semen analysis and successful paternity by intracytoplasmic sperm injection in a man with steroid 5α-reductase-2 deficiency. Fertil Steril. 2010;94(7):2770–10. e7–e10. doi: 10.1016/j.fertnstert.2010.04.013. [DOI] [PubMed] [Google Scholar]
- 43.Thyen U, Krege S. DSD/intersexuality network. A project in the BMBF program for rare diseases. Urologe A. 2007;46(9):1304–1306. doi: 10.1007/s00120-007-1505-4. [DOI] [PubMed] [Google Scholar]
- 44.Auyeung B, Baron-Cohen S, Ashwin E, et al. Fetal testosterone predicts sexually differentiated childhood behavior in girls and in boys. Psychol Sci. 2009;20(2):144–148. doi: 10.1111/j.1467-9280.2009.02279.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Hines M, Golombok S, Rust J, Johnston KJ, Golding J, Avon Longitudinal Study of Parents and Children Study Team Testosterone during pregnancy and gender role behavior of preschool children: a longitudinal, population study. Child Dev. 2002;73(6):1678–1687. doi: 10.1111/1467-8624.00498. [DOI] [PubMed] [Google Scholar]
- 46.Hines M. Prenatal testosterone and gender-related behaviour. Eur J Endocrinol. 2006;155(Suppl. 01):S115–S121. doi: 10.1530/eje.1.02236. [DOI] [PubMed] [Google Scholar]
- 47.Knickmeyer RC, Wheelwright S, Taylor K, Raggatt P, Hackett G, Baron-Cohen S. Gender-typed play and amniotic testosterone. Dev Psychol. 2005;41(3):517–528. doi: 10.1037/0012-1649.41.3.517. [DOI] [PubMed] [Google Scholar]
- 48.Cohen-Bendahan CC, van de Beek C, Berenbaum SA. Prenatal sex hormone effects on child and adult sex-typed behavior: methods and findings. Neurosci Biobehav Rev. 2005;29(2):353–384. doi: 10.1016/j.neubiorev.2004.11.004. [DOI] [PubMed] [Google Scholar]
- 49.Servin A, Nordenström A, Larsson A, Bohlin G. Prenatal androgens and gender-typed behavior: a study of girls with mild and severe forms of congenital adrenal hyperplasia. Dev Psychol. 2003;39(3):440–450. doi: 10.1037/0012-1649.39.3.440. [DOI] [PubMed] [Google Scholar]
- 50.Liao LM, Doyle J, Crouch NS, Creighton SM. Dilation as treatment for vaginal agenesis and hypoplasia: a pilot exploration of benefits and barriers as perceived by patients. J Obstet Gynaecol. 2006;26(2):144–148. doi: 10.1080/01443610500443527. [DOI] [PubMed] [Google Scholar]
- 51.Ismail-Pratt IS, Bikoo M, Liao L-M, Conway GS, Creighton SM. Normalization of the vagina by dilator treatment alone in Complete Androgen Insensitivity Syndrome and Mayer-Rokitansky-Kuster-Hauser Syndrome. Hum Reprod. 2007;22(7):2020–2024. doi: 10.1093/humrep/dem074. [DOI] [PubMed] [Google Scholar]
- 52.Foundation for Informed Medical Decision Making [Accessed October 9, 2011];2011 http://www.informedmedicaldecisions.org/
- 53.Strauss RP, Sharp MC, Lorch SC, Kachalia B. Physicians and the communication of “bad news”: parent experiences of being informed of their child’s cleft lip and/or palate. Pediatrics. 1995;96(1 Pt 1):82–89. [PubMed] [Google Scholar]
- 54.Committee on Health Literacy. Nielsen-Bohlman L, Panzer AM, Kindig DA. Health literacy: A prescription to end confusion. The National Academies Press; Washington, DC: 2004. Institute of Medicine. [PubMed] [Google Scholar]
- 55.Money J. Sex errors of the body and related syndromes: a guide to counseling children, adolescents, and their families. Paul H. Brookes Publishing Co; Baltimore, MD: 1994. [Google Scholar]
- 56.Money J. Sex Errors of the Body: Dilemmas, Education, Counseling. The Johns Hopkins Press; Baltimore: 1968. [Google Scholar]
- 57.Meyer-Bahlburg HFL, Martini L. Encyclopedia of Endocrine Diseases. Elsevier, Inc; 2004. Gender assignment and psychosocial management; pp. 125–34. [Google Scholar]
- 58.Carmichael P, Ransley P. Telling children about a physical intersex condition. Dialogues in Pediatric Urology. 2002;25:7–8. [Google Scholar]
- 59.Harbeck-Weber C, Fisher J, Dittner C. Promoting coping and enhancing adaptation to illness. In: Roberts M, editor. Handbook of Pediatric Psychology. 3rd ed. Guilford Press; ew York, NY: 2003. pp. 99–118. [Google Scholar]
- 60.Brewer S, Gleditsch SL, Syblik D, Tietjens ME, Vacik HW. Pediatric anxiety: child life intervention in day surgery. J Pediatr Nurs. 2006;21(1):13–22. doi: 10.1016/j.pedn.2005.06.004. [DOI] [PubMed] [Google Scholar]
- 61.Money J, Lamacz M. Genital examination and exposure experienced as nosocomial sexual abuse in childhood. J Nerv Ment Dis. 1987;175(12):713–721. doi: 10.1097/00005053-198712000-00002. [DOI] [PubMed] [Google Scholar]
- 62.Chase C. What is the agenda of the intersex patient advocacy movement? Endocrinologist. 2003;13:240–242. [Google Scholar]
- 63.Crissman H, Warner L, Gardner M, et al. Children with disorders of sex development: a qualitative study of early parental experience. International Journal of Pediatric Endocrinology. 2011:10. doi: 10.1186/1687-9856-2011-10. 2011. http://www.ijpeonline.com/content/2011/1/10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. [Accessed August 20, 2012];Standards of Care for the Health of Transsexual, Transgender, and Gender Nonconforming People. 2011 at http://www.wpath.org/documents/SOC%20V7%2003-17-12.pdf.
- 65.Meyer-Bahlburg HFL. Variants of gender differentiation in somatic disorders of sex development: recommendations for Version 7 of the World Professional Association for Transgender Health’s Standards of Care. Int J Transgenderism. 2009;11:226–237. [Google Scholar]
- 66.Zucker KJ. Measurement of psychosexual differentiation. Arch Sex Behav. 2005;34(4):375–388. doi: 10.1007/s10508-005-4336-7. [DOI] [PubMed] [Google Scholar]
- 67.Zucker K, Cohen-Kettinis P. Gender identity disorder in children and adolescents. In: Rowland D, Incrocci L, editors. Handbook of Sexual and Gender Identity Disorders. Wiley & Sons; New York, NY: 2008. pp. 376–422. [Google Scholar]
- 68.Menvielle EJ, Tuerk C, Jellinek MS. A support group for parents of gender-nonconforming boys. J Am Acad Child Adolesc Psychiatry. 2002;41(8):1010–1013. doi: 10.1097/00004583-200208000-00021. [DOI] [PubMed] [Google Scholar]
- 69.Mazur T, Colsman M, Sandberg D. Intersex: definition, examples, gender stability, and the case against merging with transsexualism. In: Ettner R, Monstrey S, Eyler AE, editors. Principles of Transgender Medicine and Surgery. Haworth Press; Binghamton, NY: 2007. pp. 235–259. [Google Scholar]
- 70.Lang C, Kuhnle U. Intersexuality and alternative gender categories in non-Western cultures. Horm Res. 2008;69(4):240–250. doi: 10.1159/000113025. [DOI] [PubMed] [Google Scholar]
- 71.Ismail I, Creighton S. Surgery for intersex. Rev Gynaecol Pract. 2005;5:57–64. [Google Scholar]
- 72.Schönbucher V, Schweizer K, Rustige L, Schützmann K, Brunner F, Richter-Appelt H. Sexual quality of life of individuals with 46,XY disorders of sex development. Journal of Sexual Medicine. 2010 Jan 6; doi: 10.1111/j.1743-6109.2009.01639.x. Epub. [DOI] [PubMed] [Google Scholar]
- 73.Kuhnle U, Bullinger M, Schwarz HP. The quality of life in adult female patients with congenital adrenal hyperplasia: a comprehensive study of the impact of genital malformations and chronic disease on female patients life. Eur J Pediatr. 1995;154(9):708–716. doi: 10.1007/BF02276713. [DOI] [PubMed] [Google Scholar]
- 74.Slijper F, van der Kamp H, Brandenbrug H, de Muinck Keizer-Schrama S, Drop S, Molenaar J. Evaluation of psychosexual development of young women with congenital adrenal hyperplasia: A pilot study. J Sex Educ Ther. 1992;18:200–207. doi: 10.1159/000182400. [DOI] [PubMed] [Google Scholar]
- 75.Zucker KJ, Bradley SJ, Oliver G, Blake J, Fleming S, Hood J. Psychosexual development of women with congenital adrenal hyperplasia. Horm Behav. 1996;30(4):300–318. doi: 10.1006/hbeh.1996.0038. [DOI] [PubMed] [Google Scholar]
- 76.Hines M, Brook C, Conway GS. Androgen and psychosexual development: core gender identity, sexual orientation and recalled childhood gender role behavior in women and men with congenital adrenal hyperplasia (CAH) J Sex Res. 2004;41(1):75–81. doi: 10.1080/00224490409552215. [DOI] [PubMed] [Google Scholar]
- 77.Reader TW, Flin R, Mearns K, Cuthbertson BH. Developing a team performance framework for the intensive care unit. Crit Care Med. 2009;37(5):1787–1793. doi: 10.1097/CCM.0b013e31819f0451. [DOI] [PubMed] [Google Scholar]
- 78.Salas E, DiazGranados D, Weaver SJ, King H. Does team training work? Principles for health care. Acad Emerg Med. 2008;15(11):1002–1009. doi: 10.1111/j.1553-2712.2008.00254.x. [DOI] [PubMed] [Google Scholar]
- 79.Lemieux-Charles L, McGuire WL. What do we know about health care team effectiveness? A review of the literature. Med Care Res Rev. 2006;63(3):263–300. doi: 10.1177/1077558706287003. [DOI] [PubMed] [Google Scholar]
- 80.Bell ST. Deep-level composition variables as predictors of team performance: a meta-analysis. J Appl Psychol. 2007;92(3):595–615. doi: 10.1037/0021-9010.92.3.595. [DOI] [PubMed] [Google Scholar]