Abstract
The origins of adult disease are considered to relate to fetal undernutrition, and this concept is termed “developmental origins of adult health and disease” (DOHaD). Here, we describe several epidemiological studies performed in Japan and discuss whether DOHaD is applicable to children in present day Japan. In a study of healthy children and young adults, it was found that systolic blood pressure, total cholesterol and adiponectin were associated with birth weight. Hyperinsulinemia, high blood pressure, elevated transaminase levels and prevalence of metabolic syndrome in obese children were inversely correlated with birth weight and positively correlated with current weight and waist circumference. Birth weight was related to the development of type 2 diabetes in children. DOHaD is therefore considered to be applicable in Japan. The key considerations of DOHaD are the following two mismatches. The first mismatch pertains to growth and development in response to environmental influences, especially those of nutrition. The second mismatch pertains to the prenatal versus postnatal environment. We consider that the chance of children in present day Japan developing adult diseases is determined by the above mismatches. Pediatricians and schoolteachers should therefore understand the concept of DOHaD, so that they can educate both children and their families regarding an appropriate diet to reduce the likelihood of developing adult diseases in later life.
Keywords: birth weight, obesity, blood pressure, insulin, adiponectin
Introduction
The prevalence of obesity in Japanese children and adolescents has increased from 5% to more than 10% over the last two decades. This has become a serious public health concern, as childhood obesity, which is the leading cause of hyperinsulinemia and insulin resistance, is associated with adult diseases such as hypertension (HT), dyslipidemia, type 2 diabetes mellitus (T2DM) and metabolic syndrome (MS) in adulthood. These diseases are caused by both genetic factors and postnatal environmental factors. The latter factors, the so-called “lifestyle factors”, are more closely related to the development of adult diseases than genetic factors. This has been demonstrated by the recent rapid increase in fat consumption in Japan. Leading an adequately healthy lifestyle from childhood will reduce the likelihood of developing obesity and prevent certain adult diseases. Therefore, pediatricians should be concerned with the health education of children and adolescents in order to prevent the possibility of obesity in later life.
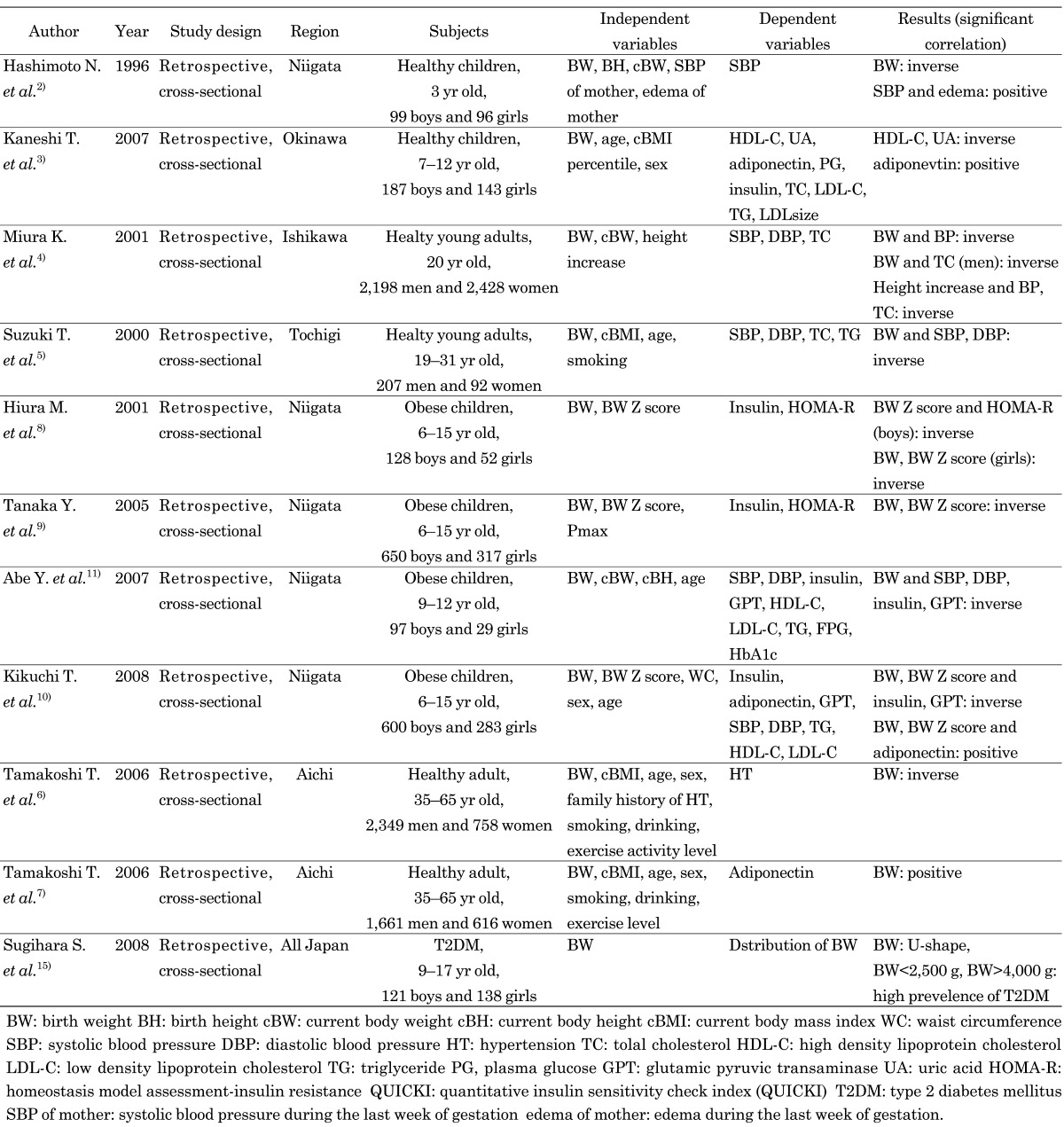
In 2004, Barker et al. proposed the concept of “developmental origins of adult health and disease” (DOHaD), which considers that intrauterine growth restriction (IUGR) is associated with an increased risk of developing MS and its related diseases in later life (1). The supply of nutrients to the fetus is the major determinant of fetal growth and is dependent on the mother’s size, body composition, nutrient store, diet during pregnancy, and the transport of nutrients to the placenta and their subsequent transfer across the placental membrane. DOHaD suggests that health education for children and adolescents is important to prevent them from bearing offspring who will be at risk of developing MS and its related diseases because maintaining a healthy lifestyle is necessary for mothers to prevent IUGR. In this paper, we briefly review several epidemiological studies of Japanese children, adolescents and adults and discuss the applicability of DOHaD in present day Japan (Table 1). As DOHaD was shown to be applicable in Japan, the need for appropriate health education for both children and adolescents is emphasized.
Table 1. Epidemiological studies of the relation of birth weight and risks factors to cardiovascular disease in Japan.
DOHaD in healthy Japanese children and young adults
Previously, we reported the relationship of birth weight and current body weight with blood pressure (BP) in 195 healthy 3-yr-old Japanese children from Niigata, Japan (2). Systolic blood pressure (SBP) was inversely correlated with weight at birth and positively correlated to weight at 3 yr of age. Children at 3 yr of age whose birth weights were more than 3,520 g had a mean SBP of 3.0 mmHg below that of those whose birth weight was 2,999 g or less. Mean SBP at 3 yr of age for children whose weight at 3 yr exceeded 16.8 kg was 9.4 mmHg higher than that of age-matched children whose weight was 14.2 kg or less. We also found an increase of 0.12 mmHg in the SBP of children for each increment of 1 mmHg in the SBP of their mothers. The SBP at 3 yr of age in children of mothers who had experienced pretibial edema during pregnancy (101.0 ± 8.8 mmHg) was significantly higher than that in children whose mothers did not have edema (96.6 ± 9.6 mmHg).
Kaneshi et al. reported the relationship of birth weight or weight velocity (weight gain/year) with risk factors of atherosclerosis in 330 Japanese children (187 boys, 143 girls) between 7 and 12 yr of age who underwent screening for lifestyle-related diseases in Okinawa, Japan (3). Birth weight was significantly correlated with serum levels of adiponectin (r=0.239, p=0.000), uric acid (r=–0.247, p=0.000) and high-density lipoprotein cholesterol (HDL-C; r=0.117, p=0.034) after adjusting for age, sex and body mass index (BMI) percentile. However, weight velocity was a stronger predictive variable than birth weight for both adiponectin and uric acid.
Miura et al. reported the relationship of birth weight, current weight, rate of height increase from 3 yr to 20 yr of age and BP with serum total cholesterol (TC) level in 4,626 Japanese (2,198 men, 2,428 women) at 20 yr of age and born between 1965 and 1974 in Ishikawa, Japan (4). Using multiple linear regression analysis, the authors estimated that a higher birth weight (+1 standard deviation) was significantly associated with SBP (lower by 1.6 mmHg in men and by 1.0 mmHg in women) and serum TC (lower by 0.07 mmol/l in men and by 0.04 mmol/l in women) after adjusting for current weight and rate of height increase.
Suzuki et al. reported the relationship of birth weight and BP with serum lipid levels in 299 (207 men, 92 women) medical students of Dokkyo University School of Medicine who had a mean age of 23 yr (5). In this case, male birth weight was inversely correlated with serum TC and triglyceride (TG) levels in young adulthood and was independent of current BMI. However, the birth weight showed no relation with BP in this study.
These findings suggest the relation of birth weight with BP, TC, HDL-C, uric acid and adiponectin. However, a study reported that birth weight was not associated with these risk factors of cardiovascular disease (5). To reveal the relationship of fetal and infant growth with these risk factors, further epidemiological study should be conducted in Japan.
DOHaD in middle-aged Japanese adults
Tamakoshi et al. reported the relationship of birth weight with adult HT in a Japanese workplace population (2,303 males, 804 females) aged 35 to 66 yr (6). Multiple logistic regression analysis adjusted for age, sex, BMI, parental history, and lifestyle revealed that the adjusted odds ratios for HT were 1.26 (95% confidence interval (CI): 0.88–1.80), 1.00 (reference), 0.89 (95%CI: 0.73–1.08) and 0.70 (95%CI: 0.49–1.00) for subjects who were in the birth weight categories of < 2,500 g, 2,500 ≤ 3,000 g, 3,000 ≤ 3,500 g, and > 3,500 g, respectively (p-value=0.009).
Tamakoshi et al. reported the relationship of birth weight with serum adiponectin levels in 2,277 subjects (1,661 men, 616 women) aged 35 to 66 yr (7). After adjusting for potential confounders, including age, sex, current BMI, smoking status, alcohol consumption and exercise activity level, the geometric mean adiponectin levels were 6.63, 6.45, 6.86, 7.05, 6.75 and 7.22 mg/ml for subjects with birth weights that were < 2,500, 2,500 to < 2,800, 2,800 to < 3,000, 3,000 to < 3,200, 3,200 to < 3,500 and > 3,500 g, respectively. Consequently, a positive association was found between birth weight and adiponectin concentration (p<0.002).
These findings suggest that the relations of weight and height at birth and postnatal weight increases with the risk factors of cardiovascular disease in middle-aged Japanese adults.
DOHaD in obese Japanese children and adolescents
We investigated the association of birth weight with metabolic derangements in obese children in Niigata, Japan (8,9,10,11). We reported the relationships of birth weight and current visceral fat accumulation with hyperinsulinemia and insulin resistance in 967 obese Japanese children and adolescents (650 boys, 317 girls) aged 6 to 15 yr (9). We divided the subjects into 4 groups on the basis of their birth weight or standard deviation (SD) score and compared the following anthropometric measurements: maximum preperitoneal fat thickness of the abdominal wall (Pmax), BP, serum insulin levels, homeostasis model assessment-insulin resistance (HOMA-R) and quantitative insulin sensitivity check index (QUICKI) among the quartiles. The fasting serum insulin levels and HOMA-R were highest in the quartile with the lowest birth weight or SD score. Birth weight and SD score were inversely related to the serum insulin levels and HOMA-R but positively related to QUICKI after adjusting for Pmax. These findings suggest that both the intrauterine environment and current visceral fat accumulation are related to hyperinsulinemia, insulin resistance and the subsequent development of MS in obese Japanese children.
We also reported the relationship of birth weight with serum insulin, adiponectin, glutamic pyruvic transaminase (GPT), TG, HDL-C and low density lipoprotein cholesterol (LDL-C) levels (10). Multiple linear regression analyses adjusted for sex, age, and current waist circumference revealed a correlation of birth weight with serum adiponectin, insulin and GPT levels (Table 2). On the other hand, the serum TG, HDL-C, and LDL-C levels showed no relation to birth weight.
Table 2. Multiple regression analyses of adiponectin, insulin and GPT with birth weight and waist circumference adjusted for sex and age among 600 obese boys and 283 obese girls from Japan.
| Independent variables | Dependent variables | Adiponectin | Insulin | GPT | |||
| β | p | β | p | β | p | ||
| Model 1 | Waist circumference | –0.235 | <0.0001 | 0.591 | <0.0001 | 0.453 | <0.0001 |
| Birth weight | 0.09 | <0.01 | –0.139 | <0.0001 | –0.131 | <0.0001 | |
| Model 2 | Waist circumference | –0.236 | <0.0001 | 0.595 | <0.0001 | 0.457 | <0.0001 |
| Birth weight SD score | 0.087 | <0.01 | –0.150 | <0.0001 | –0.14 | <0.0001 | |
GPT, glutamic pyruvic transaminase.
Moreover, we have reported on the relationships of current weight-to-birth weight ratio (WBWR) with BP, elevated GPT and hyperinsulinemia in 126 obese Japanese children and adolescents (97 boys, 29 girls; age range 9–12 yr) (11). The subjects were divided into an MS group and a non-MS group on the basis of criteria proposed for diagnosing Japanese children with MS. Although there were no significant differences in age or anthropometric measurements between the two groups, the birth weight of the MS group was lower than that of the non-MS group, whereas the WBWR of the MS group was higher than that of the non-MS group. Systolic and diastolic blood pressure, serum insulin and GPT levels correlated positively with birth weight after adjusting for sex, current height and weight.
We then investigated the association of birth weight and current waist circumference with the prevalence of MS and serum insulin levels in obese children and adolescents. We divided 416 obese children (261 boys, 125 girls) into 9 groups on the basis of low, medium or heavy birth weight, or small, medium or large waist circumference. The group with the low birth weight and large waist circumference had the highest prevalence of MS and mean serum insulin level among the 9 groups (Tables 3 and 4).
Table 3. Prevalence of metabolic syndrome and the mean levels of fasting serum insulin in 261 Japanese obese boys according to birth weight and waist circumference after being divided into 3 groups.
| Waist circumference (cm) | Birth weight (g) | |||
| 1,740–3,120 | 3,130–3,425 | 3,430–4,875 | Total | |
| 64.0–82.0 | 4 (10.8%) | 0 (0.0%) | 1 (3.8%) | 5 (5.6%) |
| 12.7 | 11.4 | 11.4 | 11.9 | |
| 37 | 27 | 26 | 90 | |
| 82.5–88.5 | 7 (29.2%) | 3 (10.3%) | 6 (18.2%) | 16 (18.6%) |
| 17.4 | 13.4 | 12.8 | 14.3 | |
| 24 | 29 | 33 | 86 | |
| 89.0–116.0 | 9 (33.3%) | 8 (26.7%) | 5 (17.9%) | 22 (25.9%) |
| 30.8 | 22.5 | 20.2 | 24.4 | |
| 27 | 30 | 28 | 85 | |
| Total | 20 (22.7%) | 11 (12.8%) | 12 (13.8%) | 43 (16.5%) |
| 19.5 | 16 | 14.7 | 16.8 | |
| 88 | 86 | 87 | 261 | |
Upper stand: number with metabolic syndrome (%). Middle stand: the mean level of fasting serum insulin (µU/ml). Lower stand: total number in each group.
Table 4. Prevalence of metabolic syndrome and the mean levels of fasting serum insulin in 125 Japanese obese girls according to birth weight and waist circumference after being divided into 3 groups.
| Waist circumference (cm) | Birth weight (g) | |||
| 1,845–3,040 | 3,044–3,375 | 3,390–4,000 | Total | |
| 69.0–80.5 | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) |
| 15 | 16.4 | 17.8 | 16.4 | |
| 12 | 19 | 11 | 42 | |
| 86.0–85.5 | 3 (20.0%) | 1 (11.1%) | 0 (0.0%) | 4 (10.0%) |
| 20.5 | 20.3 | 19.6 | 20.1 | |
| 15 | 9 | 16 | 40 | |
| 86.0–114.5 | 11 (73.3%) | 1 (7.7%) | 2 (13.3%) | 14 (32.6%) |
| 32.8 | 23.7 | 21.5 | 26.1 | |
| 15 | 13 | 15 | 43 | |
| Total | 14 (33.3%) | 2 (4.9%) | 2 (4.8%) | 18 (14.4%) |
| 23.3 | 19.6 | 19.8 | 20.9 | |
| 42 | 41 | 42 | 125 | |
Upper stand: number with metabolic syndrome (%). Middle stand: the mean level of fasting serum insulin (µU/ml). Lower stand: total number in each group.
These findings suggest that birth weight is related to metabolic derangements in obese Japanese children and adolescents. Ideally, epidemiological studies should be performed in other regions of Japan, because the presented studies have only performed in some regions.
DOHaD in Japanese children and adolescents with T2DM
According to epidemiological studies, interactions between birth weight and early postnatal growth have been associated with the development of diabetes in later life (12). Recent studies of Pima Indians and schoolchildren in Taiwan revealed a U-shaped relationship between birth weight and the risk of developing T2DM (13, 14). Sugihara et al. reported the associations of birth weight and clinical characteristics with childhood-onset T2DM (15, 16). The frequencies of low and high birth weights were higher among patients with T2DM than among those in a control group, producing a U-shaped distribution (p<0.05). Low-birth-weight patients had a low prevalence of a family history of diabetes. In contrast, high-birth-weight patients had a higher prevalence of diabetic mothers who used medication that included insulin therapy (p<0.05). These findings supported the notion that fetal growth is related to the development of T2DM in Japanese children and adolescents.
Key considerations and mechanisms of DOHaD
Fetal growth is constrained by the nutrients and oxygen provided by the mother. A poor intrauterine environment, such as that of a mother with malnutrition, a smoking habit or an inappropriate diet, will result in fetal growth retardation. When the maternal-placental nutrient supply fails to match the fetal nutrient demand, the fetus adapts to the poor nutrition by changing its metabolism, altering its secretion of hormones and the sensitivity of tissues to these hormones, redistributing its blood flow to protect key organs, especially the brain, and slowing its growth rate. Although this adaptation called “programming” is beneficial for fetal survival, it permanently alters the structure and function of both the tissues and the body of the newborn.
The downstream effects of poor fetal nutrition include insulin resistance in muscle, liver and adipose tissue, poor development of pancreatic β-cell mass and function, decreased replication of kidney cells and reduced activity of placental 11β-hydroxysteroid dehydrogenase (11β-HSD) type 2 (17). This programming is considered to be the individual’s adaptation to the mismatch of nutrition during growth and development in the fetal stage. Moreover, the second mismatch of the prenatal versus the postnatal environment will contribute to an increase in risk factors for developing adult disease. The underlying mechanisms of this innate programming involve epigenetic modifications to the non-imprinted genes and are induced by aspects of the developmental environment, which modify gene expression without altering the DNA sequence (18).
A pediatric perspective for DOHaD in present day Japan
In Japan, as of 2005, the average birth weight has decreased to <3,000 g, while the incidence of low-birth-weight infants has increased to 9.5%. The maternal diet has become insufficient, as the average daily energy intake is around 1,700–1,880 kcal and is not increased during pregnancy. Such a poor nutritional condition, which is often associated with a western lifestyle, is expected to result in a trend of increased risk for present day Japanese children developing adult diseases in later life. Pediatricians and schoolteachers should therefore understand the concept and importance of DOHaD and educate both children and their families regarding appropriate diet to reduce the likelihood of developing adult diseases in later life.
Acknowledgments
We appreciated the following doctors from the Division of Pediatrics, Niigata University Graduate School of Medicine and Dental Sciences, who participated in our studies on DOHaD: Naoshi Hashimoto, Takuya Kawasaki, Keisuke Nagasaki, Yuki Abe, Makoto Hiura, Yukie Tanaka, Yohei Ogawa, Hideo Takahashi, Hisashi Yamazaki, Masahiro Nishina, Kazuhiro Kameda and Hidetoshi Sato.
References
- 1.Barker DJP. The development origins of adult disease. J Am College Nutrition 2004;23: 588S–98S [DOI] [PubMed] [Google Scholar]
- 2.Hashimoto N, Kawasaki T, Kikuchi T, Takahashi H, Uchiyama M. The relationship between the intrauterine environment and blood pressure in 3-year-old Japanese children. Acta Peadiatr 1996;85: 132–8 [DOI] [PubMed] [Google Scholar]
- 3.Kaneshi T, Yoshida T, Ohshiro T, Nagasaki H, Asato Y, Ohta T. Birthweight and risk factors for cardiovascular diseases in Japanese schoolchildren. Pediatr Int 2007;49: 138–43 [DOI] [PubMed] [Google Scholar]
- 4.Miura K, Nakagawa H, Tabata M, Morikawa Y, Nishijo M, Kagamimori S. Birth weight, childhood growth, and cardiovasulular disease risk factors in Japanese aged 20 years. Am J Epidemiol 2001;153: 783–9 [DOI] [PubMed] [Google Scholar]
- 5.Suzuki T, Minami J, Ohrui M, Ishimitsu T, Matsuoka H. Relationship between birth weight and cardiovascular risk factors in Japanese young adults. Am J Hypertens 2000;13: 907–13 [DOI] [PubMed] [Google Scholar]
- 6.Tamakoshi K, Yatsuya H, Wada K, Matsushita K, Otsuka R, Yang PO, et al. Birth weight and adult hypertension: cross-sectional study in a Japanese workplace population. Circ J 2006;70: 262–7 [DOI] [PubMed] [Google Scholar]
- 7.Tamakoshi K, Yatsuya H, Wada K, Matsushita K, Otsuka R, Sugiura K, et al. Low birth weight is associated with reduced adiponectin concentration in adult. Ann Epidemiol 2006;16: 669–74 [DOI] [PubMed] [Google Scholar]
- 8.Hiura M, Kikuchi T, Kameda K, Yamazaki H, Nishina M, Uchiyama M. The relationship between birth weight and serum insulin in obese children. Clin Pediatr Endocrinol 2002;11: 49–54 [Google Scholar]
- 9.Tanaka Y, Kikuchi T, Nagasaki K, Hiura M, Ogawa Y, Uchiyama M. Lower birth weight and visceral fat accumulation are related to hyperinsulinemia and insulin resistance in obese Japanese children. Hypertens Res 2005;28: 529–36 [DOI] [PubMed] [Google Scholar]
- 10.Kikuchi T, Nagasaki K, Hiura M, Tanaka Y, Ogawa Y, Abe Y, et al. The association of birth weight to metabolic derangements and the serum adiponectin levels in Japanese obese children and adolescence. Clinical Endocrinology (Horumon to Rinsho) 2008;56: 69–74(in Japanese). [Google Scholar]
- 11.Abe Y, Kikuchi T, Nagasaki K, Hiura M, Tanaka Y, Ogawa Y, et al. Lower birth weight associated with current overweight status is related with the metabolic syndrome in obese Japanese children. Hypertens Res 2007;30: 627–34 [DOI] [PubMed] [Google Scholar]
- 12.Law CM, Gordon GS, Shlell AW, Barker DJ, Hales CN. Thinness at birth and glucose tolerance in seven year-old children. Diabet Med 1995;12: 24–9 [DOI] [PubMed] [Google Scholar]
- 13.MaCane DR, Pettitt DJ, Hanson RL, Jacobsson LT, Knowler WC, Bennett PH. Birth weight and noninsulin dependent diabetes: thrifty genotype, thrifty phenotype, or surviving small baby genotype? BMJ 1994;308: 942–5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wei JN, Sung FC, Li CY, Chang CH, Lin RS, Lin CC, et al. Low birth weight and high birth weight infants are both at an increased risk to have type 2 diabetes among school children in Taiwan. Diabetes Care 2003;26: 343–8 [DOI] [PubMed] [Google Scholar]
- 15.Sugihara S, Sasaki N, Amemiya S, Kohno H, Tanaka T, Matsuura N. Analysis of weight at birth and at diagnosis of childhood-onset type 2 diabetes mellitus in Japan. Pediatr Diabetes 2008;9: 285–90 [DOI] [PubMed] [Google Scholar]
- 16.Sugihara S, Sasaki N, Kohno H, Amemiya S, Tanaka T, Matsuura N. Survey of current medical treatmentsfor childhood-onset type 2 diabetes mellitus in Japan. Clin Pediatr Endocrinol 2005;14: 65–75 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Saegusa H, Nakagawa Y, Liu YJ, Ohzeki T. Influence of placental 11beta-hydroxysteroid dehydrogenase (11beta-HSD) inhibition on glucose metabolism and 11beta-HSD regulation in adult offspring of rats. Metabolism 1999;48: 1584–8 [DOI] [PubMed] [Google Scholar]
- 18.Godfrey KM, Lillycrop KA, Burdge GC, Gluckman PD, Hanson MA. Epigenetic mechanisms and the mismatch concept of the developmental origins of health and disease. Pediatr Res 2007;61: 5R–10R [DOI] [PubMed] [Google Scholar]


