Abstract
Background:
The national policy on malaria control recommends use of intermittent preventive treatment with sulfadoxine/pyrimethamine (IPT-SP) for chemoprophylaxis against malaria in pregnancy; and use of quinine and arthemisinin-based combination therapy (ACT) for acute treatment of malaria in the first, and second/third trimesters, respectively. In Nigeria, a large proportion of pregnant women are seen by the general practitioners (GPs).
Objective:
To determine the pattern of anti-malaria prescription in pregnancy among GPs in Enugu state, and access the level of conformity with the national policy on malaria control.
Materials and Methods:
Questionnaires were administered to a cross-section of 147 GPs that attended the 2010 Enugu state branch of the Nigeria Medical Association Scientific Conference/Annual General Meeting/Election.
Results:
The mean age of the GPs was 37 ± 3.6 (range 27-70) years. Quinine was the commonly (45.6% (n = 67)) prescribed anti-malaria drug in the first trimester while in the second/third trimester ACT was commonly (48.3% (n = 71)) prescribed. Seventy-six (51.7%) practitioners prescribed IPT-SP for chemoprophylaxis against malaria while the rest (48.3%) prescribed other drugs. GPs who obtained MBBS qualification less than or equal to 5 years prior to the survey were more likely to comply with the national policy on malaria control in their prescriptions (P < 0.05).
Conclusion:
The pattern of anti-malaria prescription among GPs in Enugu state is varied, and conformed poorly to the evidence-based national policy on malaria control. There is need for continuing professional development to keep the GPs abreast with current trends in malaria treatment during pregnancy.
Keywords: Anti-malaria prescription, Enugu state, general practitioners, pregnancy
INTRODUCTION
Malaria infection in pregnant women is associated with high risk of both maternal and perinatal morbidity and mortality. The disease often results from infection with Plasmodium falciparum, which accounts for over 80% of the world malaria burden.1
Pregnant women have reduced immune response and therefore less effectively clear malaria infections.2 Consequently, they are three times more likely to develop severe disease than non-pregnant women acquiring infections from the same area.2 Furthermore, because the malaria parasites sequester and replicate in the placenta,3 the malaria infection during pregnancy can lead to miscarriage, premature delivery, low birth weight, congenital malaria infection and perinatal death amongst others.4
In view of these complications, the Roll Back malaria partnership recommended a three pronged approach for reducing the burden of malaria among pregnant women.5 These interventions included use of insecticide treated bed nets (ITNs), intermittent preventive treatment with sulfadoxine/pyrimethamine (IPT-SP), and effective case management. The National malaria control program,6,7 recommends two doses of IPT-SP during normal pregnancy; the first dose to be administered at quickening, which ensures that the woman is in the second trimester, and the second dose given at least one month from the first. A third dose is recommended for human immunodeficiency virus (HIV)-positive women. The use of drugs such as proguanil, pyrimethamine or chloroquine for chemoprophylaxis is no longer recommended because of the demonstrable resistance of malaria parasites to these drugs.6,7 Effective case management of malaria entails early diagnosis and prompt treatment of acute cases using effective anti-malaria drugs. The National malaria control program recommends the use of quinine for acute treatment of cases in the first trimester, and artemsinin-based combination therapy (ACT) for acute cases in the second and third trimesters.6,7 The ACT recommended in pregnancy is the Arthemeter/lumefantrine or Artemisinin/amodiaquine combinations.6,7 Anti-malaria drugs such as primaquine, halofantine, mefloquine, etc., are contraindicated in pregnancies and thus not recommended.8
A far majority of pregnant Nigerian women attending antenatal care are seen by non-obstetricians, who prescribe various forms of anti-malaria drugs during pregnancy. General practitioners (GPs) no doubt attend to a large proportion of our pregnant women. It is therefore pertinent that the pattern of anti-malaria prescription by the GPs is periodically analyzed as this will help determine the conformity with the evidence-based recommendation by the National malaria control program. These underscored the need for this study which aims at determining the pattern of anti-malaria prescription in pregnancy among the GPs and to access the level of conformity with the national policy on malaria control as the prescription pattern may impact positively or negatively on the foetal and maternal outcome of pregnancies afflicted with malaria.
MATERIALS AND METHODS
This was a cross-sectional survey of all the GPs that attended the 2010 Enugu state branch of the Nigeria Medical Association Scientific Conference/Annual General Meeting (AGM)/Election held on 26th July at Danic Hotel, Enugu. Enugu is located in the hilly tropical rain forest about 230 m above sea level. The average annual temperature is between 23.1°C and 31°C with a rainfall of 1520-2030 mm. There are two major seasons; rainy season (March to October) and dry season (November to February). It has a mixed rural and urban population of 722,664 inhabitants of which 52.1% are female.9 The area is hyper-endemic for malaria and Plasmodium falciparum is predominantly implicated. Further details of the study area have been described in a recent study.10
Enugu state has a record of 302 GPs according to information available at the state ministry of health and NMA secretariat. The state NMA secretary provided a ‘book register’ for the registration of every doctor that attended the scientific conference/AGM/election. The register contained provisions for the names of the doctors, status of the doctors, e.g., house officer, GP or specialist, and the name/location of the hospitals where the doctors were working. The doctors that attended the scientific conference/AGM/election registered one after the order as they came. A total of 509 doctors attended the conference/AGM/election out of which 160 were GPs, representing 31.4% of all the doctors in attendance and 53% of all the GPs in the state. All the 160 GPs in attendance were included in the study following individual counselling and all those that consented were given self-administered, structured and pre-tested questionnaires. Ethical clearance for the study was obtained from the Institutional Review Board of the UNTH, Enugu. The questionnaires were designed to cover the GPs’ socio-demographic characteristics and the various anti-malaria drugs prescribed by them for acute uncomplicated treatment of malaria infection and for chemoprophylaxis. Statistical analysis was both descriptive and inferential at 95% confidence level using Statistical Package for Social Sciences (SPSS) computer software version 16 (SPSS Inc. Chicago, IL, USA). Frequency tables were generated for relevant variables. Proportions were compared with Pearson's Chi-square. Relationships were expressed using odd ratio and confidence intervals. P value of less than 0.05 was considered statistically significant. GP in this study was defined as medical doctor with MBBS degree or its equivalent but without any post-graduate fellowship qualification.
RESULTS
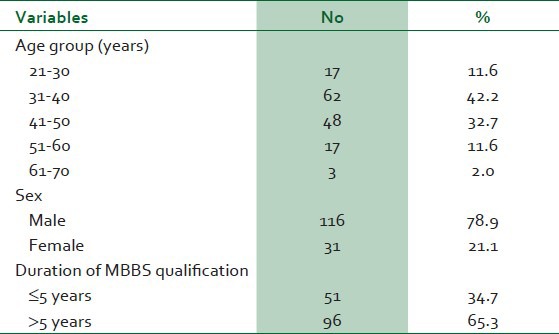
One hundred and sixty (160) questionnaires were distributed, however, I47 were correctly filled and retrieved giving a response rate of 92%. The mean age of the GPs was 37 ± 3.6 (range: 27-70) years. One hundred and sixteen (78.9%) were males while 31 (21.1%) were females. The number of years of practice ranged between 1 and 43 years. Fifty-one GPs obtained MBBS qualification less than or equal to 5 years prior to the survey while the rest (n = 96) obtained MBBS qualification more than 5 years before the survey [Table 1].
Table 1.
Socio-demographic characteristics of the respondents
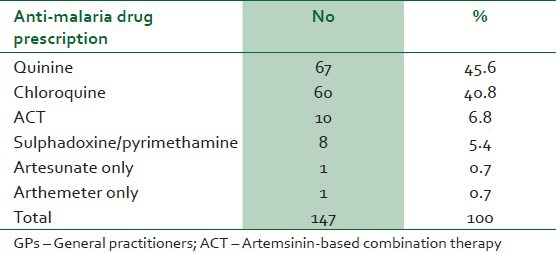
In the first trimester of pregnancy, 67 (45.6%) of the GPs prescribed quinine for their patients who presented with acute malaria attack, while 60 (40.8%) prescribed chloroquine. Other anti-malaria drugs prescribed in the first trimester for acute treatment of malaria infection were as shown in Table 2.
Table 2.
Pattern of anti-malaria prescription for acute treatment of malaria in the first trimester of pregnancy by the GPs
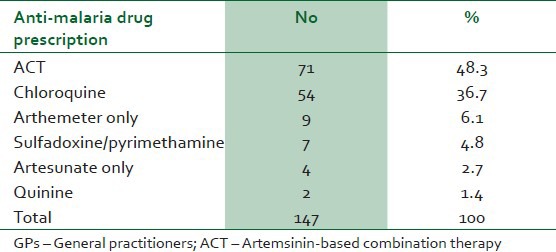
In the second/third trimesters, 71 (48.3%) prescribed ACT for acute treatment of malaria infection, while 54 (36.7%) prescribed chloroquine. Other anti-malaria drugs prescribed by the practitioners for acute treatment of malaria infection in the second and third trimesters were as shown in Table 3.
Table 3.
Pattern of anti-malaria prescription for acute treatment of malaria in the second/third trimester by the GPs
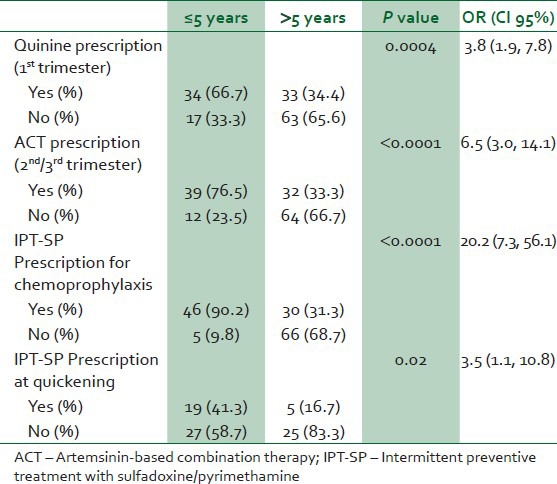
Seventy-six (51.7%) of the GPs prescribed IPT-SP for chemoprophylaxis. Other drugs prescribed for chemoprophylaxis were as shown in Table 4. Of the 51.7% (n = 76) GPs that prescribed IPT-SP for chemoprophylaxis, 71 (48.3%) prescribed correctly two doses for pregnant women without HIV infection and 45 (30.6%) prescribed correctly three doses for HIV-positive pregnant women. The time of commencement of IPT-SP chemoprophylaxis prescription varied among the GPs that prescribed it; 24 (31.6%) commenced prescription at quickening (16 weeks gestation), 35 (46.1%) commenced at mid-half of pregnancy (20 weeks gestation), 10 (13.2%) commenced at first trimester and 7 (9.2%) commenced at the third trimester. GPs who obtained MBBS qualification less than or equal to 5 years prior to the survey were significantly more likely to adopt the treatment protocol for malaria in pregnancy in the national malaria control program than those that obtained the qualification more than 5 years prior to the survey (<0.05) as shown in Table 5.
Table 4.
Pattern of anti-malaria prescription for chemoprophylaxis by the GPs
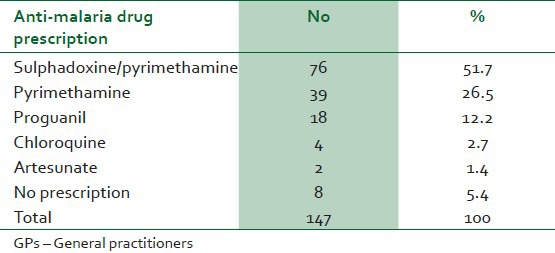
Table 5.
Association between duration of MBBS qualification (years) and Federal Ministry of Health recommended anti-malaria prescription in pregnancy
DISCUSSION
The pattern of anti-malaria prescription amongst the GPs in Enugu state is varied. Most prescriptions are not consistent with the evidence-based approach, as recommended by the World Health Organization5,11 and the national malaria control programme of the Federal Ministry of Health (FMOH).6,7 The fact that only 45.6% of the GPs prescribed quinine for acute treatment of malaria in the first trimester with majority (54.4%) prescribing other anti-malaria drugs, shows that the GPs may not be abreast with the new concept of treatment of acute malaria in the first trimester where quinine is drug of choice and is also currently the only anti-malaria drug that is effective and safe for use in the first trimester of pregnancy.6,11 The continued prescription of chloroquine to treat malaria in pregnancy showed that they were unaware of the documented evidence of wide spread chloroquine resistance in the region and in sub-Sahara Africa in general.12,13 Again, the FMOH has for over 5 years now banned the use of chloroquine for prophylaxis or treatment of malaria in pregnancy.6,7
In the second/third trimesters, less than half (48.3%) of the GPs prescribed ACT drugs for acute treatment of malaria. It is unfortunate that despite the demonstrated effectiveness and safety of ACT in acute treatment of malaria in second/third trimester, most GPs could not avail the pregnant women in their care of this effective anti-malaria treatment probably because of ignorance. Nevertheless, the ACT prescription obtained in this study is much higher than the 18.6% and 3.0% obtained in previous studies from Osogbo and Calabar in 2005 and 2007, respectively.14,15 The higher rate of prescription in this study may not be unconnected with the recent aggressive advertisement and marketing of ACT by some pharmaceutical companies, FMOH and recently introduced continuing professional development (CPD) in Nigeria.
That only 51.7% of the practitioners prescribed IPT-SP of malaria revealed again that many GPs in the study area are yet to be abreast with the new concept of chemoprophylaxis for the prevention of malaria attack in pregnancy. This was corroborated by the finding that only 31.6% of the GPs that even prescribed IPT-SP commenced the prescription at the appropriate time at quickening. The implications of not conforming to current practices in treating acute malaria and chemoprophylaxis in pregnancy included increased foetal, perinatal and maternal morbidity and mortality from malaria.
The limitation of the survey include the fact that the reported practice may have over-estimated the actual clinical practices as some of the respondents may be aware of the current guidelines and therefore be inclined to state so despite practicing the contrary. This implies that the level of practice reported from this survey is conservative and in fact may be poorer than estimated. Furthermore the survey was conducted among attendees of scientific conference/annual general meeting of the medical association who were possibly more of a motivated group and more up to date with their clinical practice compared to those not attending the scientific session and the annual general meeting.
In conclusion, the pattern of anti-malaria prescription among GPs in Enugu state varied widely among the practitioners and was not in accordance with the new evidence-based recommendation by the World Health Organization and the national malaria control unit of the FMOH. There is need for CPD as this will reduce maternal and perinatal morbidity and mortality associated with malaria in pregnancy.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Breman JG, Alilio MS, Mills A. Conquering the intolerable burden of malaria: What's new? What's needed? Am J Trop Med Hyg. 2004;7:1–15. [PubMed] [Google Scholar]
- 2.Elliot SR, Brennan AK, Beeson JG, Tadesse E, Molyneux ME, Brown GV, et al. Placental malaria induces variant-specific antibiotics of the cytophilic subtypes immunoglobulin G 1 (IgG 1) and IgG 3 that correlate with adhesion inhibitory activity. Infect Immun. 2005;73:5903–7. doi: 10.1128/IAI.73.9.5903-5907.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Luxemburger C. The epidemiology of severe malaria in the area of low transmission in Thailand. Trans R Soc Trop Med Hyg. 1997;91:256–62. doi: 10.1016/s0035-9203(97)90066-3. [DOI] [PubMed] [Google Scholar]
- 4.Mutabingwa TK, Bolla MC, Li JL. Maternal malaria and gravidity interest to modify infant susceptibility to malaria. PLoS Med. 2005;2:e407. doi: 10.1371/journal.pmed.0020407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.World Health Organization. Brazzaville: WHO Regional Office for Africa. A strategic framework for malaria prevention and control during pregnancy in the African region. 2004. [Last assessed on 2012 May 28]. p. 115. AFR/MAL/04/09. Available from: http://afro.who.int/malaria/publications/malari a_in_pregnancy_09/2004 .
- 6.Federal Ministry of Health, National Malaria Control Programme, Abuja, Nigeria. Strategic Plan. 2009-2013. [Last assessed on 2012 May 30]. pp. 24–28. Available from: http://nmcpnigeria.org/f/Nigeria Annex 1_National Malaria Control Strategy Plan 2009-2013 .
- 7.FMOH. National Antimalaria Treatment Policy. Abuja: Federal Ministry of Health; 2005. Federal Republic of Nigeria; pp. 6–31. [Google Scholar]
- 8.Mokuolu OA, Okoro EO, Ayetoro SO, Adewara AA. Effect of artemisinin-based treatment policy on consumption pattern of antimalarials. Am J Trop Med Hyg. 2007;1:7–11. [PubMed] [Google Scholar]
- 9.Federal Republic of Nigeria. Population Census. 2006. [Last assessed on 2012 Feb 18]. Available from: http://www.nigerianstat.gov.ng/nbsapps/Connections/Pop2006.pdf .
- 10.Umeh UA, Obi SN, Onah HE, Ugwu EO, Ajah LO, Umeh CR. The impact of intermittent preventive treatment with sulphadoxine-pyrimethamine on the prevalence of malaria parasitaemia in pregnancy. Trop Doct. 2012;42:133–5. doi: 10.1258/td.2011.110402. [DOI] [PubMed] [Google Scholar]
- 11.World Health Organization. Guidelines for treatment of malaria. Second edition. 2010. [Last assessed on 2012 Jun 6]. pp. 26–28. Available from: http://www.who.int/publications/atoz/9789241547925/en/index.html .
- 12.Briand V, Cottrell G, Massougbodji A, Cot M. Intermittent preventive treatment for the prevention of malaria during pregnancy in high transmission areas. Malar J. 2007;6:160. doi: 10.1186/1475-2875-6-160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nwagha UI, Ugwu VO, Nwagha TU, Anyaechie BU. Asymptomatic plasmodium parasitaemia in pregnant Nigeria women; Almost a decade after Role Back Malaria. Trans R Soc Trop Med Hyp. 2009;103:16–20. doi: 10.1016/j.trstmh.2008.07.016. [DOI] [PubMed] [Google Scholar]
- 14.Elemile PO, Egbewale BE, Olowu OA, Abiodun OV. Prescription pattern of antimalaria drugs among medical practitioners in Osogbo Metropolis, South-west Nigeria. Trop Med Health. 2005;33:201–8. [Google Scholar]
- 15.Meremikwu M, Okomo U, Nwachukwu C, Oyo-Ita A, Eke-Njoku J, Okebe J, et al. Antimalarial drug prescribing practice in private and public health facilities in South-Nigeria: A descriptive study. Malar J. 2007;6:55. doi: 10.1186/1475-2875-6-55. [DOI] [PMC free article] [PubMed] [Google Scholar]


