Abstract
Objective:
To assess the impact of gender and living area on cardiovascular risk factors in the context of a comprehensive lifestyle intervention program.
Design:
Data from independent sample surveys before (2000--2001) and after (2007) a community trial, entitled the Isfahan Healthy Heart Program (IHHP) were used to compare differences in the intervention area (IA) and reference area (RA) by gender and living area.
Setting:
The interventions targeted the population living in Isfahan and Najaf-Abad counties as IA and Arak as RA.
Participants:
Overall, 12 514 individuals who were more than 19 years of age were studied at baseline, and 9570 were studied in postintervention phase.
Interventions:
Multiple activities were conducted in connection with each of the four main strategies of healthy nutrition, increasing physical activity, tobacco control, and coping with stress.
Main Outcomes:
Comparing serum lipids levels, blood pressure, blood glucose and obesity indices changes between IA and RA based on sex and living areas during the study.
Results:
In IA, while the prevalence of hypertension declined in urban and rural females (P < 0.05). In IA, the prevalence of hypercholesterolemia and hypertriglyceridemia decreased in both females and males of urban and rural areas except for hypercholesterolemia in rural males (P < 0.01). In RA, the significant changes include both decrease in the hypercholesterolemia among rural males (P < 0.001) and hypertriglyceridemia in urban females (P < 0.01), while hypertriglyceridemia was significantly increased in rural females (P < 0.01).
Conclusions:
This comprehensive community trial was effective in controlling many risk factors in both sexes in urban and rural areas. These findings also reflect the transitional status of rural population in adopting urban lifestyle behaviors.
Keywords: Age, cardiovascular risk factor, community health program, health promotion, rural, sex, urban
INTRODUCTION
Noncommunicable diseases (NCDs) are expected to account for 60% of the disease burden and 73% of all deaths in the world by 2020.[1] Atherosclerotic cardiovascular disease (ACVD) can no longer be considered a disease of developed world because myocardial infarction and stroke are increasingly prevalent worldwide across all socioeconomic strata.[2]
From an epidemiological perspective, a risk factor is a characteristic or feature associated with an increased risk of developing future disease; although conventional risk factors for most NCDs, notably ACVDs, are smoking, hypertension, hyperlipidemia, diabetes and obesity but the global inequalities access of health care[3] and the exiting disparities of health between males and females and between urban and rural residents have led to considerable differences in the prevalence of these risk factors according to gender and living area. For instance, we have previously documented that overweight and metabolic syndrome are emerging health problems in Iranian women and urban residents.[4] Most existing data are from cross-sectional studies; however community-based interventions are considered as a means of decreasing risk factors at population level and in turn providing information to health policy-makers beyond that obtained by individual-based clinical trials. Very limited reports exist about community trials in developing countries; consequently the “Isfahan Healthy Heart Program” (IHHP) was launched as a comprehensive public health response to the high prevalence of NCDs in Iran. This community-based program aimed to promote healthy lifestyle behaviors, and ultimately to prevent NCDs in a developing country.[5,6]
Although it is of special concern for policy makers to have evidence- based information about the differences in the impact of community-based interventions in urban and rural areas, as most community trials have been conducted only in urban areas, very limited experience exists on the differences in the impact of lifestyle interventions in urban versus rural areas. As the first study of its kind, not only in Iran but also in the Eastern Mediterranean region (EMR), the current report from IHHP presents the variation in the impact of gender and living area on ACVD cardio-metabolic risk factors in the context of a comprehensive community-based lifestyle intervention program.
MATERIALS AND METHODS
IHHP was developed as an action-oriented demonstration program targeted to the general population in urban and rural areas of three counties in central Iran. We have previously explained its design and detailed interventions,[5,6] and here we describe it in brief. The baseline survey was conducted in 2000--2001 in three counties with similar sociodemographic and cultural characteristics. Furthermore, both areas were industrial without any contaminations and mass media coverage as well as good cooperation. Subjects were chosen with multistage random sampling method form clusters of health center. The survey consisted of assessment of questionnaire-based lifestyle behaviors, physical examination, and blood collection. Then, while routine national health programs continued in intervention and the reference areas, comprehensive and integrated community-based interventions were implemented in two counties, Isfahan and Najaf-Abad, with populations of 1 895 856 and 275 084, respectively, in comparison with another county, Arak, located 375 km northwest of Isfahan with a population of 668 531. The urban-to-rural population ratios in the counties of Isfahan, Najaf-Abad and Arak were 90/10, 60/40, and 66/34, respectively. Approval was obtained from Ethical Committee of Isfahan Cardiovascular Research Center (ICRC), which is a collaborating center in the Eastern Mediterranean region. Written informed consent was obtained from all participants after full explanation of the study protocol. Lifestyle behaviors were measured by annual questionnaire-based surveys in independent samples in the three counties under study. In 2007, the whole baseline survey was repeated on an independent random sample in both the intervention and reference communities. Overall, 12 514 individuals with more than 19 years of age were studied at baseline, and 9 570 were studied in postintervention phase. IHHP had a quasi-experimental design, and the impact of its interventions by gender and living area was evaluated in a repeat [2000--2001 vs. 2007] cross-sectional survey method.
In both surveys, participants were invited to survey centers for interview, physical examination and blood sampling. Trained physicians and nurses conducted the clinical examinations and fasting blood sampling by using standardized and zero calibrated instruments standard protocols.
Blood samples obtained from participants in both surveys were assayed in ICRC central laboratory, with adherence to external national and international standardization.
Cardio-metabolic risk factors were defined according to standard classifications, i.e. participants were considered to have diabetes if their fasting blood glucose (FBG) level was ≥126 mg/dl, or they were taking glucose-lowering medications,[7] hypertension was defined in accordance with the Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC 7) as SBP ≥140 mm Hg, or DBP ≥90 mm Hg, or being on antihypertensive medication,[8] abnormal serum lipid profiles were defined based on the National Cholesterol Education Panel Adult Treatment Panel III (NCEP-ATP III) as total cholesterol >240 mg/dl; triglycerides >200 mg/dl; HDL <40 mg/dl for males and <50 mg/dl for females; and LDL-C >160 mg/dl.[9]
IHHP interventions were implemented based on the data from obtained the baseline survey and a needs assessment on existing health and human resources. Details of the interventional activities were are described before,[10] briefly they targeted individuals, populations and the environment by considering the four main strategies of healthy nutrition, increasing physical activity, tobacco control, and coping with stress.
Various measures were considered for maximizing the quality of the data collection through quality assurance programs. Different levels of evaluation were taken into account to assess the process of program development and performance, as well as the extent to which the program attained its objectives,[6] process evaluation comprising both qualitative and quantitative methods was conducted in the intervention areas.[11] Moreover, the Isfahan University of Medical Sciences undertook an external evaluation of the whole IHHP study, including its implementation and evaluation components, by international experts and submitted it's report to the university officials and the WHO office in Iran.[12]
Statistical analysis
Continuous data are presented as means + standard errors of mean (SEM), and frequencies as percent. All statistical analyses controlled for age, education level and income. Differences between mean (SEM) risk factor values were compared between years (2000--201 and 2007), areas (intervention and reference communities)-based sex, residency as well as interaction terms of area (intervention versus reference) × time (2000--2001 versus 2007) using ANCOVA test.
Chi square test was used to compare categorical variables containing frequency of risk factors between areas and years. Area (intervention versus reference) × time (2000--201 versus 2007) interaction terms in categorical variables were tested using logistic regression analysis. Data were analyzed using the SPSS statistical package version 15.0 for windows (SPSS Inc., Chicago, USA). The significance level was set at P < 0.05.
RESULTS
The baseline survey comprised 6175 participants (48.7% male, 78.9% urban resident) in the intervention area, and 6339 participants (49.2% male, 66.6% urban resident) in the reference area. In 2007, the sample included 4719 participants (49.2% male, 82.6% urban resident) in the intervention area and 4853 participants (50.6% male, 57.6%urban resident) in the reference area. The mean age of participants was not significantly different in the two surveys (38.8 ± 14.6 years in 2000--2001; 39.1 ± 15.3 years in 2007).
The mean values of variables studied in 2001 and 2007 among males and females living in urban and rural areas are presented in Tables 1 and 2, respectively. The prevalence of cardio-metabolic risk factors in the abovementioned populations is presented in Tables 3 and 4, respectively. While body mass index (BMI) decreased significantly in urban females living in the intervention areas, it had no significant change in other groups. In the intervention areas, waist circumference (WC) had significant decrease in females of both urban and rural areas and males of urban areas, whereas in the reference area, it had significant increase in males and females of both urban and rural areas [Tables 1 and 2]. The prevalence of overweight and obesity (BMI >25 kg/m2) had a nonsignificant decrease in urban females of the intervention area, while the corresponding figure increased significantly in the reference area (P for interaction <0.0001). Among the rural male residents, this prevalence had a nonsignificant increase in the intervention area and a significant increase in the reference area (P for interaction <0.0001). The prevalence of abdominal obesity decreased significantly in female urban and rural residents of the intervention area, whereas the corresponding figure had significant increase in the reference area (P for interaction <0.0001). As presented in Tables 3 and 4, among males, this prevalence had significant decrease in urban residents of the intervention area and nonsignificant increase in the reference area; while this change was not significant in rural residents of the intervention area, it had a significant increase in the reference area (P for interaction <0.0001).
Table 1.
Comparing the mean change of cardio-metabolic risk factors in intervention vs. reference urban area based on sex, 2001--2007
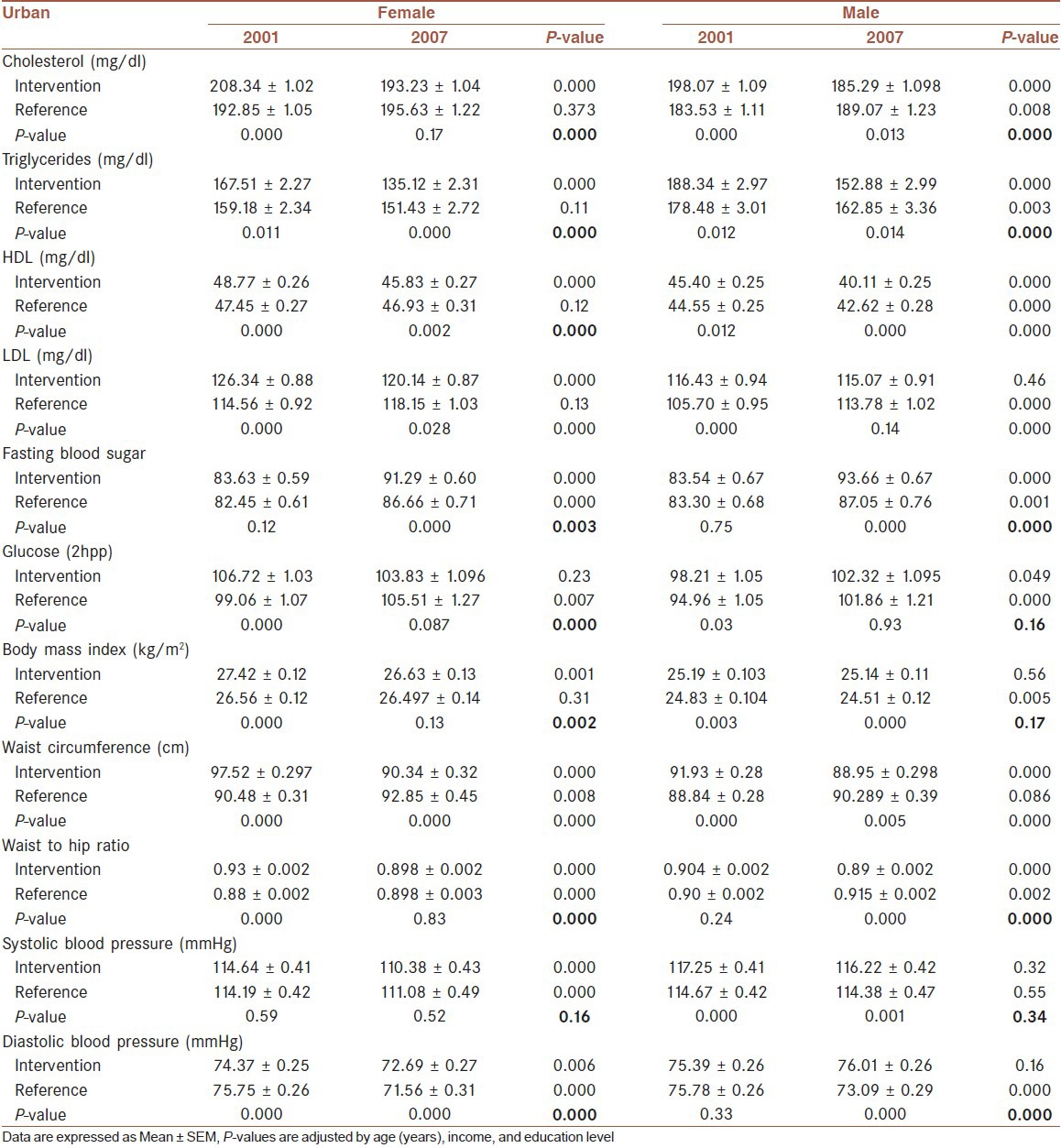
Table 2.
Comparing the mean change of cardio-metabolic risk factors in intervention vs. reference rural area based on sex, 2001-2007
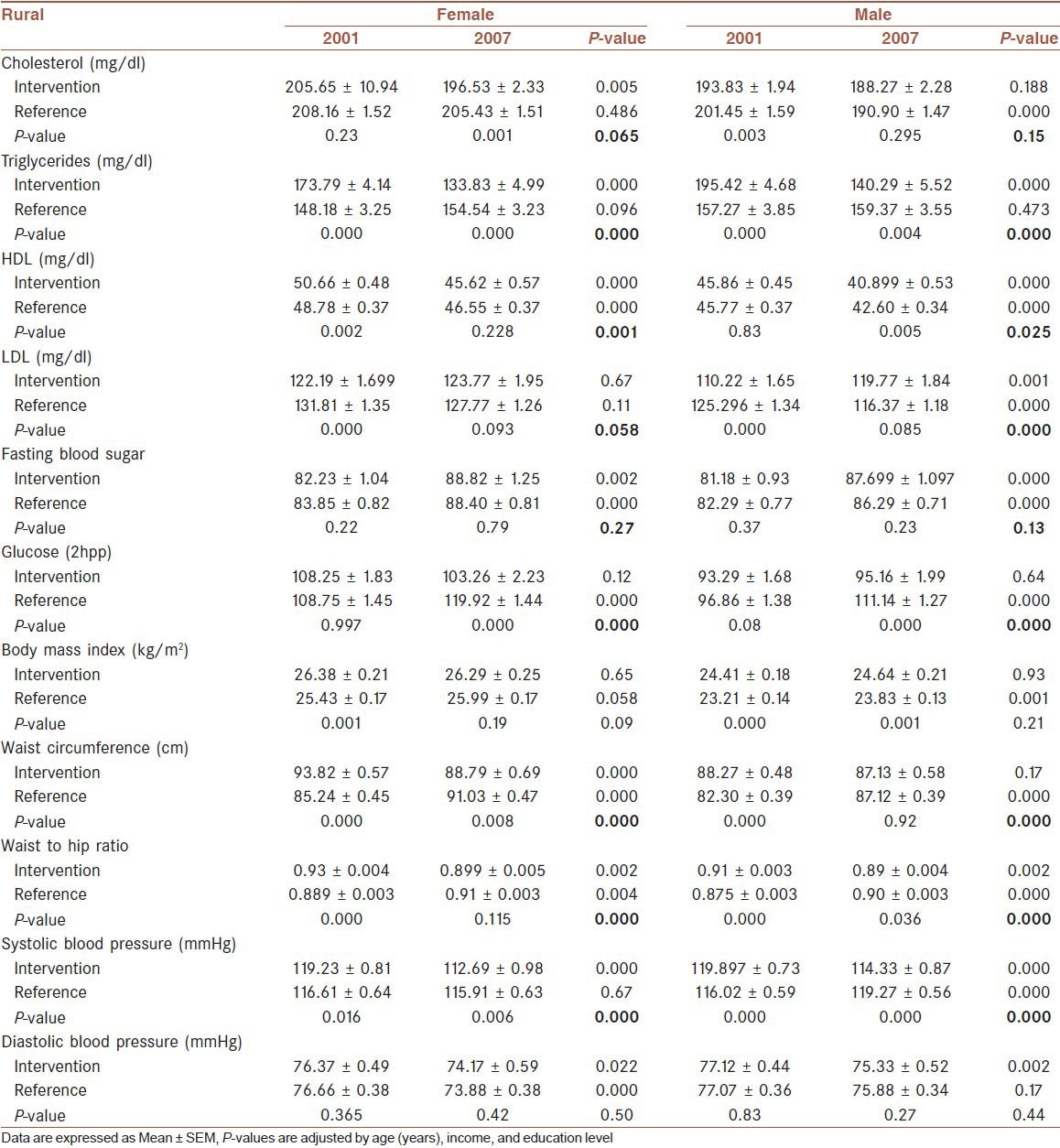
Table 3.
Comparing the prevalence change of cardio-metabolic risk factors in intervention vs. reference urban area based on sex, 2001-2007
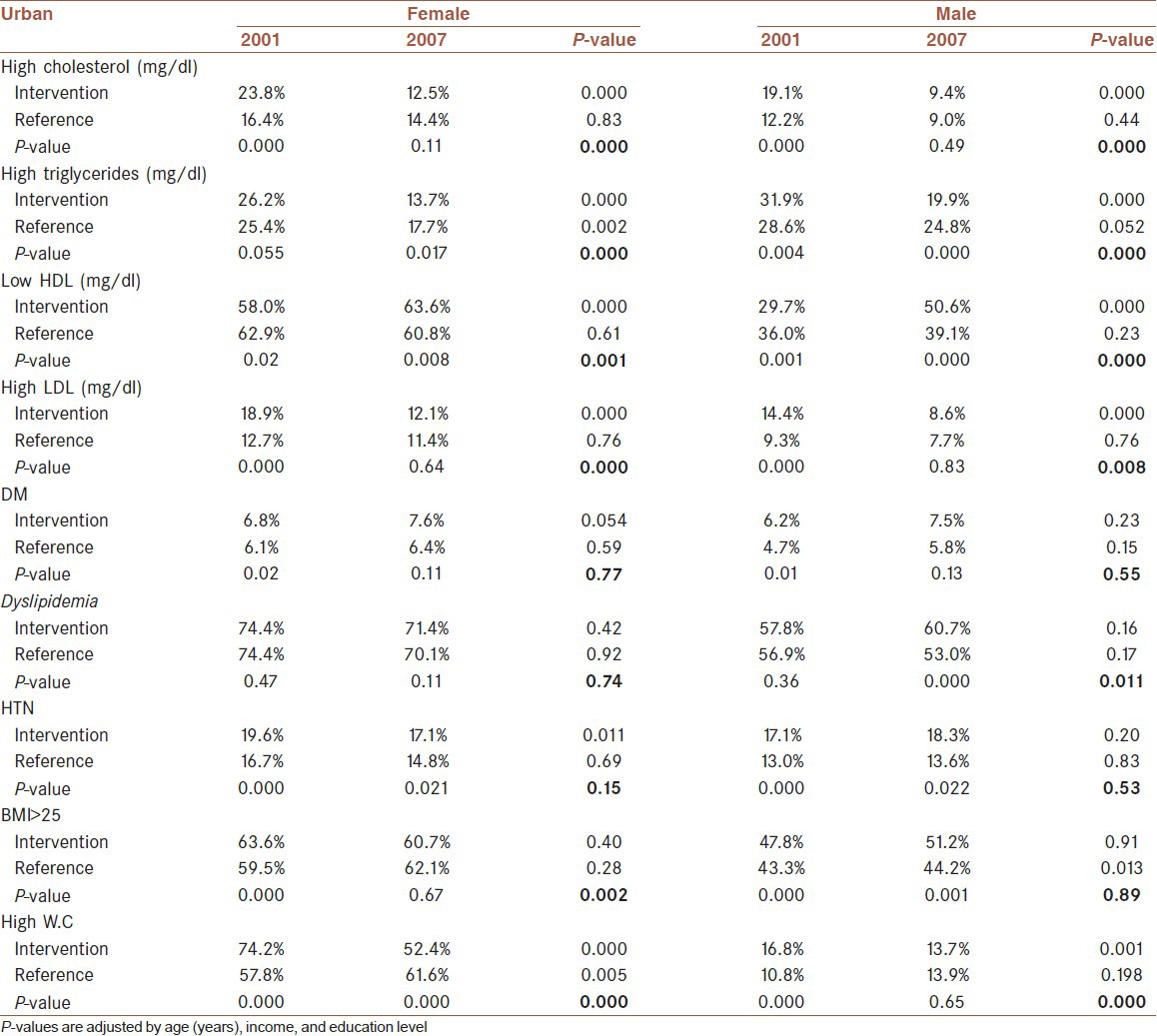
Table 4.
Comparing the prevalence change of cardio-metabolic risk factors in intervention vs. reference rural area based on sex, 2001-2007
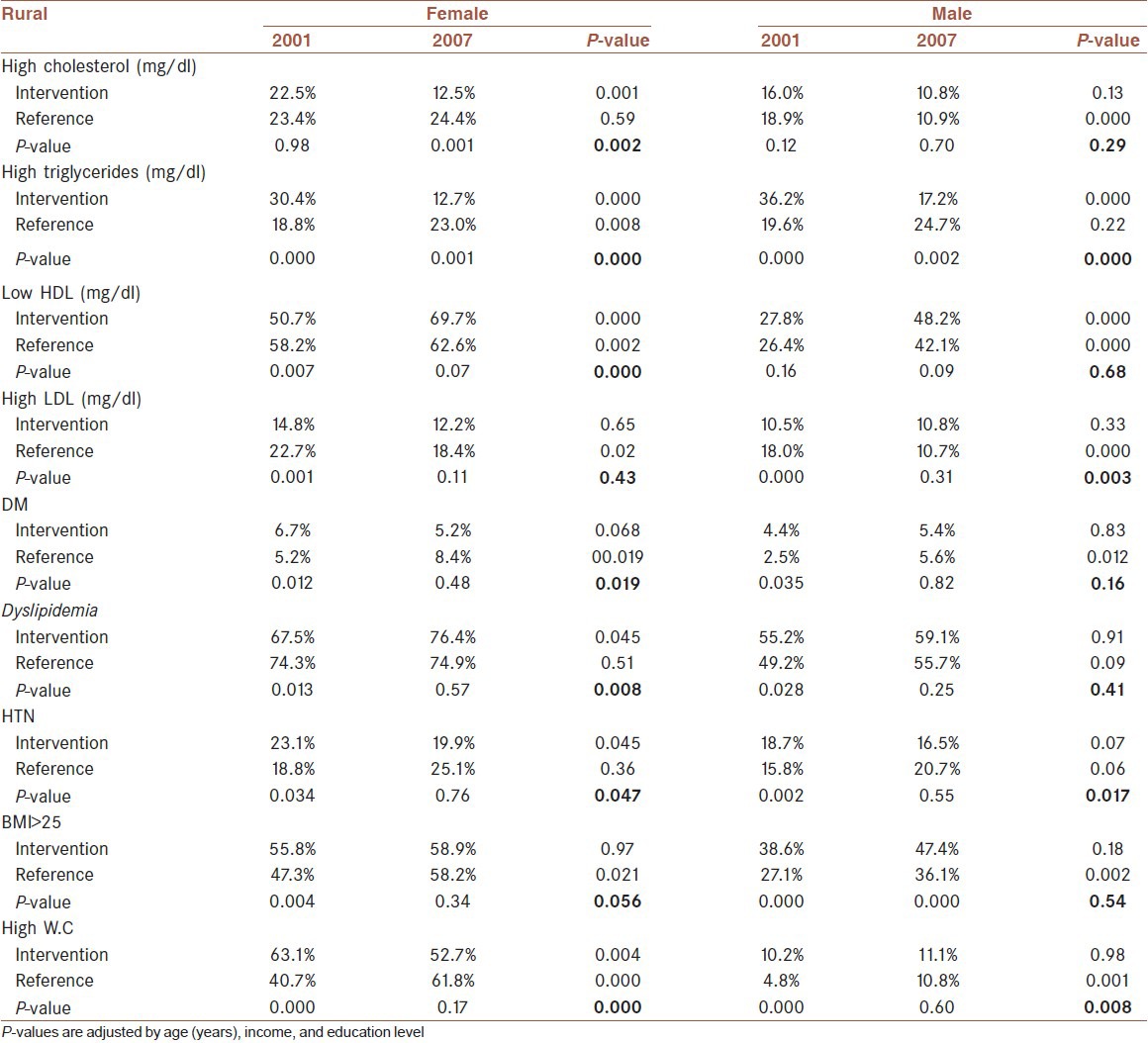
In urban areas, the mean systolic and diastolic blood pressures decreased significantly in females of both intervention and reference areas, without significant change in males of both areas. In rural areas, it decreased significantly in females of both areas and males in the intervention area, whereas it had significant increase in males of the reference area (P for interaction <0.0001). The diastolic blood pressure decreased significantly in all groups, with the exception of male rural residents of the reference area in whom this decrease was not significant [Tables 1 and 2]. In the intervention area, the prevalence of hypertension decreased significantly in female residents of urban and rural areas. While this prevalence did not differ significantly among male urban residents of both areas under study, it had significant decrease in rural male residents of the intervention area and significant increase in their counterparts in the reference area (P for interaction <0.0001) [Tables 3 and 4].
Among urban residents of both sexes, the mean total cholesterol had significant decrease in the intervention area, and significant increase in the reference area (P for interaction <0.0001). In rural residents, it had significant decrease in females of the intervention areas, and nonsignificant decreases in other groups [Tables 1 and 2]. In the intervention areas, the prevalence of hypercholesterolemia decreased significantly in females of both urban and rural areas, and males of urban areas. In the reference area, the only significant change was the decrease in this prevalence among males of rural areas [Tables 3 and 4].
The mean level of LDL-C decreased significantly in female urban residents of the intervention area. In the reference area, it had significant increase in male urban residents and significant decrease in male rural residents. Except than the female rural residents, the P for interaction was less than 0.0001 for all these comparisons between the intervention vs. reference areas. In general, HDL-C decreased in urban and rural residents of both males and females in the intervention and reference areas.
The mean triglycerides level decreased significantly in both sexes in urban and rural residents of the intervention areas. In the reference area, it had nonsignificant decrease in both sexes in urban residents, and nonsignificant increase in rural residents (P < 0.0001 for all these comparison in intervention vs. reference area). In urban residents, the prevalence of hypertriglyceridemia decreased significantly in females of the intervention and reference areas, and males of the intervention area. Among rural residents, this prevalence decreased significantly in both sexes in the intervention area; it had a significant increase in females and a nonsignificant increase in males of the reference area (P < 0.0001 for all these comparisons between intervention and reference areas) [Tables 3 and 4].
In urban areas, the prevalence of diabetes mellitus had a nonsignificant rise in both genders, whereas in rural areas, while there was no significant change in IA, it increased significantly among both genders in RA [Tables 3 and 4].
DISCUSSION
The findings of the current study provide evidence-based information about the efficient and favorable impacts of a comprehensive healthy lifestyle intervention program on improving cardio-metabolic risk factors in urban and rural population of both genders in a developing country. By using clinical models targeting only high-risk individuals, most previous studies have documented the beneficial effects of lifestyle modification on risk reduction.[13,14] There are, however, several inadequacies to translating this traditional clinical model into public health interventions.
As stated by Rose, “A large number of people exposed to a small risk may generate more cases than a small number exposed to a high risk.”[15] Therefore, small changes in behaviors of the population are likely to yield larger improvements in risk factors in the population than larger changes among a smaller number of high-risk individuals.[16] Although the rapid urbanization in many low- and middle-income countries over the past decades have been accompanied by lifestyle change and increase in NCD risk factors, the evidence of such beneficial effects is scarce and of uncertain clinical significance in these countries. As a demonstration program, the current findings showed that a comprehensive community trial with strategies integrated to existing facilities and directed at targets of both primary and secondary prevention can be effective in reducing cardio-metabolic risk factors among both genders in urban and rural areas.
In the current study, the mean values of most variables and the prevalence of most risk factors decreased in both urban and rural residents of intervention areas, in some cases although significant improvement was not documented in intervention areas, but that risk factor had significant increase in the reference area, e.g., abdominal obesity in rural males. These findings and the comparable prevalence of risk factors in urban and rural residents might reflect the transitional status of rural population in adopting urban lifestyle behaviors.[17] On the other hand, the favorable changes in some risk factors in both genders in urban and rural inhabitants in the intervention and reference areas with greater improvement in the intervention areas can be a confirmatory evidence of appropriate coverage of the national health system reducing socio-demographic disparities in health and health care that has been intensified by simple and sustainable interventions with appropriate dose of intervention of this community trial, which have been integrated to existing facilities and health services. In turn, these findings suggest the feasibility of integrating the interventions of this demonstration program to the current health system at national, and even at regional levels.
Limited experience exists from developing countries on the variations of the impact of community trials by gender and living area. An 8-year-community-based comprehensive intervention study in a suburb area in China (1991--2000) resulted in reducing mean systolic and diastolic blood pressure but not serum lipids and BMI.[18] Some other lifestyle trials conducted in developing countries have been limited to high-risk individuals like diabetic patients or could only show their effectiveness in increasing public awareness mostly by peer-education or were limited to urban areas.[19,20,21,22]
Investigators of the North-Karelia study, as one of the first and most successful community trials have suggested that their experience, notably on nutrition intervention programs can be useful in developing countries. They suggested that although Finland is an industrialized country; North Karelia was a rural area with low socioeconomic level and with many social problems in the 1970s and 1980s. The project was based on low-cost intervention activities, where people's participation and community organizations played a key role. In turn, comprehensive interventions in the community were ultimately supported by national activities in terms of expert guidelines and media actions to industry collaboration and policy. Therefore, they suggested that after tailoring to the local conditions, similar principles for nutrition intervention programs could be used in low- and middle-income countries.[23]
The baseline differences in cardio-metabolic risk factors between IA and RA in our study can be considered as one of our limitations; however it is not easy for large community based trials to match most of the studied characteristics between IA and RA.
The magnitude of the risk reduction observed in this demonstration community trial is likely to have considerable public health implications when assessed in terms of overall impact, not only efficacy. Having reference area, various levels of evaluation considered in this program,[5,6] and high-quality results of external evaluation of the interventions and outcomes by international external evaluators[12] support the strength of the program. Its favorable impact not only on lifestyle behaviors, but also on most NCD risk factors in both genders living in urban and rural areas is promising to be replicable in other countries with similar sociodemographic situation.
ACKNOWLEDGMENTS
This program was conducted by the Isfahan Cardiovascular Research Center (ICRC) (a WHO Collaborating Center) with the collaboration of Isfahan Provincial Health Office, both of which are affiliated with the Isfahan University of Medical Sciences. The program was supported by a grant (No. 31309304) from the Iranian Budget and Planning Organization, as well as the Deputy for Health of the Iranian Ministry of Health and Medical Education and the Iranian Heart Foundation. We are thankful to the team of ICRC and Isfahan Provincial Health Office as well as collaborators from Najaf-Abad Health Office and Arak University of Medical Sciences.
Footnotes
Source of Support: a grant (No. 31309304) from the Iranian Budget and Planning Organization, as well as the Deputy for Health of the Iranian Ministry of Health and Medical Education and the Iranian Heart Foundation
Conflict of Interest: None declared.
REFERENCES
- 1.Stuckler D, King L, Robinson H, McKee M. WHO's budgetary allocations and burden of disease: a comparative analysis. Lancet. 2008;372:1563–9. doi: 10.1016/S0140-6736(08)61656-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mendis S, Lindholm LH, Mancia G, Whitworth J, Alderman M, Lim S, et al. World Health Organization (WHO) and International Society of Hypertension (ISH) risk prediction charts: assessment of cardiovascular risk for prevention and control of cardiovascular disease in low and middle-income countries. J Hypertens. 2007;25:1578–82. doi: 10.1097/HJH.0b013e3282861fd3. [DOI] [PubMed] [Google Scholar]
- 3.Boutayeb A. The double burden of communicable and non-communicable diseases in developing countries. Trans R Soc Trop Med Hyg. 2006;100:191–9. doi: 10.1016/j.trstmh.2005.07.021. [DOI] [PubMed] [Google Scholar]
- 4.Sarrafzadegan N, Kelishadi R, Baghaei A, Hussein Sadri G, Malekafzali H, Mohammadifard N, et al. Metabolic syndrome: an emerging public health problem in Iranian women: Isfahan Healthy Heart Program. Int J Cardiol. 2008;131:90–6. doi: 10.1016/j.ijcard.2007.10.049. [DOI] [PubMed] [Google Scholar]
- 5.Sarraf-Zadegan N, Sadri G, Malek Afzali H, Baghaei M, Mohammadi Fard N, Shahrokhi S, et al. Isfahan Healthy Heart Program: A comprehensive integrated community-based program for cardiovascular disease prevention and control. Design, methods and initial experience. Acta Cardiol. 2003;58:309–20. doi: 10.2143/AC.58.4.2005288. [DOI] [PubMed] [Google Scholar]
- 6.Sarrafzadegan N, Baghaei A, Sadri Gh, Kelishadi R, Malekafzali H, Boshtam M. Isfahan healthy heart program: Evaluation of comprehensive, community-based interventions for non-communicable disease prevention. Prev Control. 2006;2:73–84. [Google Scholar]
- 7.Report of the Expert Committee on the Diagnosis and Classification of Diabetes Mellitus. Diabetes Care. 2003;26:S5–20. doi: 10.2337/diacare.26.2007.s5. [DOI] [PubMed] [Google Scholar]
- 8.Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL., Jr Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension. 2003;42:1206–52. doi: 10.1161/01.HYP.0000107251.49515.c2. [DOI] [PubMed] [Google Scholar]
- 9.Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). Executive Summary of The Third Report of The National Cholesterol Education Program (NCEP) JAMA. 2001;285:2486–97. doi: 10.1001/jama.285.19.2486. [DOI] [PubMed] [Google Scholar]
- 10.Sarrafzadegan N, Kelishadi R, Esmaillzadeh A, Mohammadifard N, Rabiei K, Roohafza H, et al. Do lifestyle interventions work in developing countries? Findings from the Isfahan Healthy Heart Program in the Islamic Republic of Iran. Bull World Health Organ. 2009;87:39–50. doi: 10.2471/BLT.07.049841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rabiei K, Kelishadi R, Sarrafzadegan N, Abedi HA, Alavi M, Heidari K, et al. Process evaluation of a community-based program for prevention and control of non-communicable disease in a developing country: The Isfahan Healthy Heart Program, Iran. BMC Public Health. 2009;9:57. doi: 10.1186/1471-2458-9-57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Vartiainen E, Laatikainen T. Isfahan Healthy Heart Program: External Evaluation. 2009. [Last accessed on 20-11-2011]. Available from: http://www.ihhp.ir/IHHP/display.aspxid=1656 .
- 13.Goldhaber-Fiebert JD, Goldhaber-Fiebert SN, Tristán ML, Nathan DM. Randomized controlled community-based nutrition and exercise intervention improves glycemia and cardiovascular risk factors in type 2 diabetic patients in rural Costa Rica. Diabetes Care. 2003;26:24–9. doi: 10.2337/diacare.26.1.24. [DOI] [PubMed] [Google Scholar]
- 14.Fortmann SP, Varady AN. Effects of a community-wide health education program on cardiovascular disease morbidity and mortality: the Stanford Five-City Project. Am J Epidemiol. 2000;152:316–23. doi: 10.1093/aje/152.4.316. [DOI] [PubMed] [Google Scholar]
- 15.Rose G. Oxford: Oxford University Press; 1992. The Strategy of preventive medicine. [Google Scholar]
- 16.Saunders SA, Wallymhamed M, Macfarlane IA. Improvements in glycaemic control and cardiovascular risk factors in a cohort of patients with type 1 diabetes over a 5-year period. QJM. 2009;102:29–34. doi: 10.1093/qjmed/hcn125. [DOI] [PubMed] [Google Scholar]
- 17.Ntandou G, Delisle H, Agueh V, Fayomi B. Abdominal obesity explain s the positive rural-urban gradient in the prevalence of the metabolic syndrome in Benin, West Africa. Nutr Res. 2009;29:180–9. doi: 10.1016/j.nutres.2009.02.001. [DOI] [PubMed] [Google Scholar]
- 18.Huang GY, Gu DF, Duan XF, Xu XS, Gan WQ, Chen JC, et al. Effects of 8 years community intervention on risk factors of cardiovascular diseases in Fangshan Beijing. Zhongguo Yi Xue Ke Xue Yuan Xue Bao. 2001;23:15–8. [PubMed] [Google Scholar]
- 19.Vincent D. Culturally tailored education to promote lifestyle change in Mexican Americans with type 2 diabetes. J Am Acad Nurse Pract. 2009;21:520–7. doi: 10.1111/j.1745-7599.2009.00439.x. [DOI] [PubMed] [Google Scholar]
- 20.Makrilakis K, Liatis S, Grammatikou S, Perrea D, Katsilambros N. Implementation and effectiveness of the first community lifestyle intervention programme to prevent Type 2 diabetes in Greece. The DE-PLAN study. Diabet Med. 2010;27:459–65. doi: 10.1111/j.1464-5491.2010.02918.x. [DOI] [PubMed] [Google Scholar]
- 21.Damião R, Sartorelli DS, Hirai A, Massimino F, Poletto J, Bevilacqua MR, et al. Japanese-Brazilians Diabetes Study Group. Nutritional intervention programme among a Japanese-Brazilian community: procedures and results according to gender. Public Health Nutr. 2010;13:1453–61. doi: 10.1017/S1368980010000935. [DOI] [PubMed] [Google Scholar]
- 22.Horton ES. Effects of lifestyle changes to reduce risks of diabetes and associated cardiovascular risks: results from large scale efficacy trials. Obesity (Silver Spring) 2009;17(Suppl 3):S43–8. doi: 10.1038/oby.2009.388. [DOI] [PubMed] [Google Scholar]
- 23.Nissinen A, Berrios X, Puska P. Community-based noncommunicable disease interventions: lessons from developed countries for developing ones. Bull World Health Organ. 2001;79:963–70. [PMC free article] [PubMed] [Google Scholar]


