Abstract
Background:
Hemoglobinopathies are a group of inherited disorders of hemoglobin synthesis. It could be formed a fatal scenario in concern of lacking of actual information. Beside this, ABO and Rh blood grouping are also important matter in transfusion and forensic medicine and to reduce new born hemolytic disease (NHD).
Materials and Methods:
The spectrum and prevalence of various hemoglobinopathies, ABO and rhesus (Rh) blood groups was screened among patients who visited B.S. Medical College and Hospital, Bankura, West Bengal, India. This study was carried out on 958 patients of different ages ranging from child to adults from January to June 2011. High-performance liquid chromatography (HPLC), complete blood count (CBC) and hemagglutination technique were performed for the assessment of abnormal hemoglobin variants, ABO and Rh blood groups, respectively.
Results:
Results from this study had been shown that there was high prevalence of hemoglobinpathies (27.35%) where β-thalassemia in heterozygous state occurred more frequent than other hemoglobinopathies. Out of 958 patients, 72.65% were HbAA and 27.35% were hemoglobinopathies individuals where 17.64% β-thalassemia heterozygous, 2.92% β-thalassemia homozygous, 3.86% HbAE, 1.15% HbAS trait, 1.25% HbE-β thalassemia trait and 0.52% HbS-β thalassemia trait were found. No incidence of HbSS, HbSC, HbCC, HbD and other variants of hemoglobinpathies were observed. The gene frequencies with respect to ABO systems had been shown as O > B > A > AB. Blood group O was the highest (35.8%) and the least percentage distribution was blood group AB (6.68%). Rhesus positive (Rh+) were 97.7%, while the remaining was 2.3% Rhesus negative (Rh-). The frequencies of A+, B+, AB+, and O+ blood groups were 22.44%, 33.61%, 6.58%, and 35.07%, respectively.
Conclusions:
Remarkable percentages of hemoglobinopathies were prevalent from the present study. An extensive screening of the population is needed to assess the prevalence of hemoglobinopathies, which will help in identification of carriers of hemoglobinopathies and further it will be of assistance in taking adequate therapeutic and preventive measures.
Keywords: ABO, blood groups, hemoglobinopathy, HPLC, rhesus, West Bengal
INTRODUCTION
The hemoglobinopathies are characterized by the production of structurally defective hemoglobin due to abnormalities in the formation of the globin moiety of the molecule. When biological function is altered owing to a mutation in the hemoglobin, the condition is known as a hemoglobinopathy.[1] Abnormal hemoglobin variants are a group of autosomal recessive disorders characterized by the synthesis of a structurally abnormal globin chain. Inherited disorders of hemoglobin are the most common gene disorders with 7% of the world's population being carriers with as many as 40% carriers in some regional populations.[2]
The inherited disorders of blood include hemoglobinopathies produce a massive public health problem in many countries including India.[3] The carrier frequency of hemoglobinopathy varies from 3 to 17% in different population groups of India.[4] It was reported that there were about 65,000-67,000 β-thalassemia patients in India with around 9,000-10,000 cases being added every year. The prevalence of carrier β-thalassemia gene varies from 1 to 3% in Southern India to 3 to 15% in Northern India.[5] The cumulative gene frequency of the three most predominant abnormal hemoglobins, i.e., sickle cell, hemoglobin D and hemoglobin E has been estimated to be 5.35% in India.[6] But the exact magnitude of the problem in rural India is still obscure. Several methods are applied for the assessment of hemoglobinopathies among them cation exchange high-performance liquid chromatography (HPLC) offers a reliable tool for early, accurate detection of various hemoglobinopathies.[7]
The membrane of the human red blood cell (RBC) is complex and contains a variety of blood group antigens.[8] The ABO blood group system is the most clinically important blood group system because antibodies against A or B or both antigens of RBCs are naturally present in the serum of persons whose red cells express blood group B, A, or O. The ABO incompatible transfusions are potentially fatal. In addition, human red blood cells that contain antigen D are known as Rhesus positive, while those without antigen D in their RBC's are Rhesus negative.[9] Rh incompatible transfusions are also potentially fatal to health.[10]
The knowledge of prevalence and distribution of the hemoglobin variants and blood groups aiding in prevention and management of various hemoglobinopathies plays a vital role in the hospital blood bank as well as in the formulation of transfusion policies.[8] The frequencies of these inherited characters have been extensively reported in various populations and ethnic groups around the world. [9,10,11] In India, few published data have been encountered.[5,6,12] There has been no known data of the distribution pattern and frequency of hemoglobin variants, ABO and Rh blood group from western region of West Bengal. Therefore, this study aimed for providing information on the distribution pattern of hemoglobinopathies, ABO and Rh blood groups in the rural population of this area from the visited patients at B.S. Medical College & Hospital (BSMCH), Bankura, West Bengal, India.
MATERIALS AND METHODS
Subjects
The participants were enrolled as a screening programme for the evaluation of spectrum of abnormal hemoglobin, grouping and rhesus typing for those who visited to the Bankura Smmilani Medical College and Hospital (BSMCH), Bankura, West Bengal, India. Total 958 participants were studied; their address are kept and stored in this screening programme. They were with different ages ranging from child to adults (3 years to 55 years) for a period of January to June 2011. These participants include pre-marital candidates, pregnant mother with known suspicious or unknown family history, clinically suspicious or haemoglobin fall patients referred by the home institute physician and few of self participants. But all participants were represented from western region of West Bengal state, India which covers distinctively Bankura, Purulia, Burdwan and Paschim Medinipur district. These districts are known as ‘backward districts’ of this state and large percentage of people of this community belongs in schedule caste or in tribe. This study covers mainly in rural population of these districts where Bauri group, one of ethnic group (native residents of Bankura) were showed dominantly.
Sample collection
Blood samples were collected by venipuncture into ethylene diamine tetra acetic acid (EDTA) anticoagulated tubes used for the determination of haemoglobin variants, complete blood count (CBC) and red cell phenotyping. Peripheral blood smear (PBS) was also collected for the microscopic observation.
Laboratory methods
Hemoglobin variants were determined using cationic-exchange HPLC method (BIO RAD ‘VARIANT’, BIO RAD Laboratories, USA). At first, prior to sample application, the instruments had been primed and calibrated followed by use of controls and then prepared hemolysate from EDTA blood was run by that instrument. CBC was assessed by cell counter (Sysmax Kx-21, Sysmax Corporation, Japan) and PBS with Leishman's staining was observed microscopically for red cells morphology for the supporting of diagnosis of hemoglobinopathies.
ABO and Rhesus blood grouping were carried out using the tile method while a drop of EDTA blood of each subject are mixed with respective antisera, anti A, anti B, anti D reagents (Tulip Diagnostics (P) Ltd., Goa, India) in separate places on a clean white tile and blood groups were determined on the basis of agglutination and parallaly control was run separately. Agglutination was read macroscopically and microscopically in doubtful cases. All negative results were confirmed using the indirect antiglobulin test (IAT) procedure for confirmation of the weak D.
Patient history and family history were recorded by the counselling for the confirmation of diagnosis of hemoglobinopathy. Family screening was also conducted in abnormal hemoglobin cases. In few cases mutation study are done by a referral institute, Institute of Haematology and Transfusion Medicine, Kolkata, for the conformation of types of hemoglobinopathy.
Ethical consideration
The medical and ethical committee of B.S. Medical College and Hospital approved this research study.
RESULTS
A total of 958 participants were screened for abnormal hemoglobin variants, ABO, and Rhesus blood groups. Of these, 301 were male (31.42%) and 657 (68.58%) were female subjects. Overall and sex wise prevalence of hemoglobinopathies is depicted in Figure 1. This study showed the over-all prevalence of hemoglobinopathies was 27.35% where male (38.54%) was more suffer with hemoglobinopathies than female (22.22%).
Figure 1.
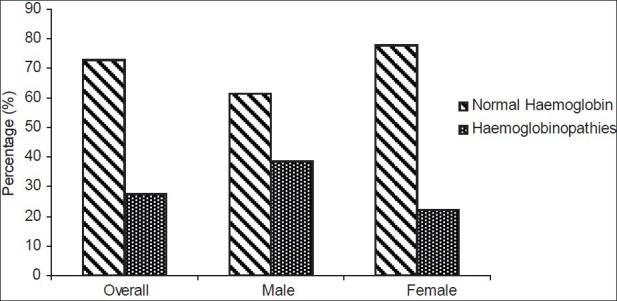
Overall and sex-wise prevalence of hemoglobinopathy among the study participants
Sex wise different hemoglobinopathies detected during the study are presented in Table 1 where β-thalassemia heterozygous (trait) was the most frequently encountered hemoglobinopathies (17.64%) and β-thalassemia homozygous (major and intermediate) was 2.92%. In this study, the frequencies of HbAA, HbAE, and HbAS were 72.65%, 3.86%, and 1.15%, respectively. Only eleven cases of sickle cell trait were found. Besides, 12 (1.25%) and 5 (0.52%) were observed Hb-E- β-thalassemia trait and Hb-S- β-thalassemia trait, respectively. None of the participants had abnormal pattern of HbSS or HbSC in the present study.
Table 1.
Sex-wise distribution of patients with different hemoglobinopathies (n = 958)
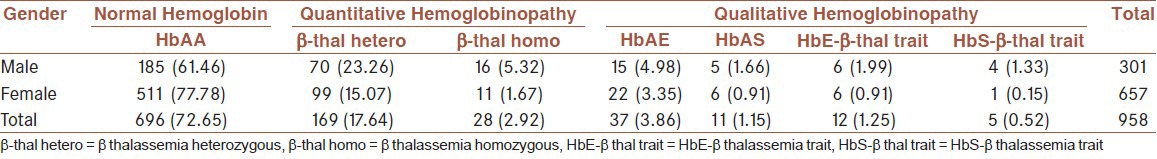
The prevalence of hemoglobinopathies was higher among the male than female participants. The frequency of β-thalassemia heterozygous was 23.26% and β-thalassemia homozygous was 5.32% among male. Fifteen (4.98%) males and 22 (3.35%) females had HbAE, 5 (1.66%) male and 6 (0.91%) female had HbAS, while 6 (1.99%) male and 6 (0.91%) female had Hb-E- β-thalassemia trait. Besides this, 4 (1.33%) in male and 1 (0.15%) in female had Hb-S- β-thalassemia trait.
Table 2 revealed the distribution of the ABO and Rhesus (D) blood groups among study subjects. Blood group O was found to be the most frequent (35.8%) among the study population, while blood group AB was least prevalent (6.68%). The gene frequencies with respect to ABO can be shown as O > B > A > AB. The frequency of blood group B showed preponderance over blood group A. The distribution of ABO groups among the gender showed that O (39.20%) and B (35.22) group were more frequent among the male. In contrast, A (24.35%) and AB (6.68) group were higher prevalent among female.
Table 2.
Prevalence of blood groups in the study population (n = 958)
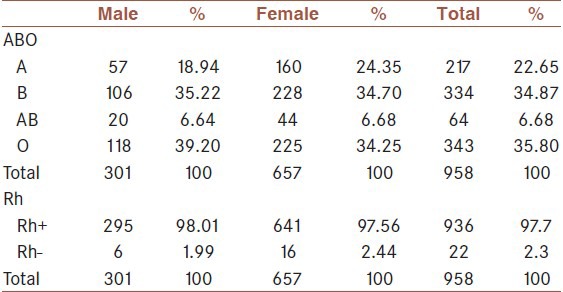
In Rh blood typing, 97.7% of the subject was Rh+ while the remaining 2.3% was Rh- [Table 2]. The percentages of female (2.44%) of Rh- type are more than the males.
There were no significant differences in both ABO and Rh blood groups in male and female.
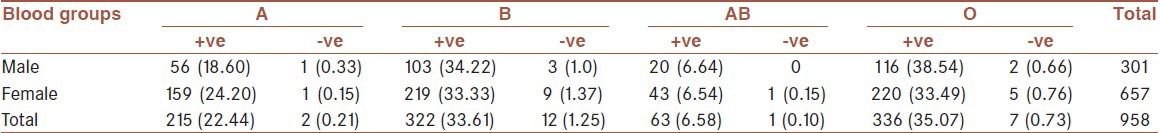
With respect to both ABO and Rhesus blood grouping systems, the prevalence of blood group A+, A-, B+, B-, AB+, AB-, O+ and O- were 22.44, 0.21, 33.61, 1.25, 6.58, 0.10, 35.07, and 0.73%, respectively. The gene frequencies with respect to ABO and Rhesus systems can be shown as O+ > B+ > A+ > AB+ > B- > O- > A- > AB- [Table 3].
Table 3.
Distribution of various blood groups (ABO and Rh) in the study population (n = 958)
DISCUSSION
Hemoglobinopathies are of worldwide occurrence, though some geographical areas have high prevalence of these disorders. The inherited disorders of hemoglobin synthesis are one of the important public health problems in various part of India.[5]
The present study revealed that large numbers of people were encountered with hemoglobinopathies (27.35%) in the rural areas of Bankura, West Bengal. In our study, β-thalassemia heterozygous individuals (17.64%) was the most frequently encountered quantitative hemoglobinopathies, followed by HbAE (3.86%), β-thalassemia homozygous state (2.92%), HbE β-thalassemia trait (1.25%), HbAS (1.15%) and HbS β-thalassemia trait (0.52%). This compares with previous studies from Kolkata (26%)[13] and Gujarat (16.35%)[12] where β-thalassemia heterozygous was the commonest disorder. In a study by Balgir,[14] sickle cell trait was reported common disorders from Orissa where sickle cell trait and β-thalassemia trait were the most frequently encountered hemoglobinopathies. Different variants of hemoglobinopathy manifest variable clinical and hematological profile in India. The highest frequency of β-thalassemia trait is reported in Gujarat (10-15%), followed by Sindh (10%), Punjab (6.5%), Tamil Nadu (8.4%), and Maharashtra.[3,5,14] We also observed a gender associated risk for where β-thalassemia of 23.26% and 5.32% for males versus 15.07% and 1.67% for females in respect of heterozygous and homozygous status. The reason for this male gender susceptibility for abnormal β-thalassemia is unknown.
The frequency of HbAS detected in this study is consistent with previous studies in Gujarat.[12] In India, average frequency of sickle cell gene is around 5%.[5]
On comparing HbE β-thalassemia trait and HbS β-thalassemia trait disorders, it was seen that the frequency of abnormal hemoglobin was more in HbE β-thalassemia trait (1.25%) than HbS β-thalassemia trait (0.52%).
Gene frequencies with respect to ABO system for the present study can be shown with a general formula O > B > A > AB. The preponderance of the allele B of the ABO blood groups over allele A had been observed in the present study. Previous reports are in agreement with the present study and confirm that group O was the predominant in ABO blood groups.[8,11] Previously in a survey conducted in Nigeria the frequency of blood group O was 46%, A was 26.6%, and B was 3.8%.[8]
Rhesus D distribution also varies within any group of human population. This study showed that total percentage of RhD positive distribution was 97.7% and RhD negative distribution was 2.3%. Similar pattern of distribution is also observed in other studies.[9] It was also revealed that blood group O RhD positive was the highest with frequency of 35.07%, followed by group B RhD positive 33.61%, blood group A RhD positive 22.44%, and AB RhD positive was 6.58%. In this study, we have observed higher prevalence of O RhD positive blood group compared to other frequencies. Similar frequencies was reported among university students from Oyo state of Nigeria.[10]
Knowledge of the prevalence and distribution of hemoglobinopathies, ABO and Rh blood groups among any population is useful in health care planning and appropriate allocation of resources.[8,12] Hemoglobinopathy screening and identification can become the cornerstone to reduce this burden specially in developing countries. Adequate measures and screening procedures should be performed concurrently. On the another hand, knowledge on the distribution of the various blood groups is also vital in the safe rendering of transfusion service, civic registration, forensic medicine and to reduce hemolytic disease of newborn associated with Rhesus-mismatched marriages among couples.
ACKNOWLEDGMENTS
We are grateful to Prof. Manoj Kr. Choudhuri, Principal of the B. S. Medical College and Hospital, Bankura, West Bengal, for his continuous encouragement and providing the necessary permission to carry out the study. Technical help by Mrs. Kasturi Maji, Medical Laboratory Technologist is gratefully acknowledged. We are also grateful to the Govt. of West Bengal for the conduction of State Thalassaemia Control Programme.
Footnotes
Source of Support: Nil
Conflict of Interest: The authors have no conflicts of interest
REFERENCES
- 1.Rodwell VW. Harper's Biochemistry. In: Murray RK, Granner DK, Mayes PA, Rodwell VW, editors. 25th ed. Stamford: Appleto and Lange; 2000. pp. 63–73. [Google Scholar]
- 2.Weatheral DJ. Genetic disorders of hemoglobin. In: Hoffbrand AV, Lewis SM, Tuddenham EG, editors. Postgraduate haematology. 4th ed. London, UK: Arnold Publishers; 2001. pp. 91–119. [Google Scholar]
- 3.Balgir RS. The burden of haemoglobinopathies in India and the challenges ahead. Curr Sci. 2000;79:1536–47. [Google Scholar]
- 4.Balgir RS. Control and prevention of the genetic load of haemoglobinopathies in India. Natl Med J India. 1999;12:234–8. [PubMed] [Google Scholar]
- 5.Shivashankara AR, Jailkhani R, Kini A. Hemoglobinopathies in Dharwad, North Karnataka: A hospital-based study. J Clin Diagnostic Res. 2008:593–9. [Google Scholar]
- 6.Balgir RS. Genetic epidemiology of the three predominant abnormal hemoglobins in India. J Assoc Physicians India. 1996;44:25–8. [PubMed] [Google Scholar]
- 7.Sachdev R, Dam AR, Tyagi G. Detection of Hb variants and hemoglobinopathies in Indian population using HPLC: Report of 2600 cases. Indian J Pathol Microbiol. 2010;53:57–62. doi: 10.4103/0377-4929.59185. [DOI] [PubMed] [Google Scholar]
- 8.Erhabor O, Adias TC, Jeremiah ZA, Hart ML. Abnormal hemoglobin variants, ABO, and Rhesus blood group distribution among students in the Niger Delta of Nigeria. Pathol Lab Med Int. 2010;2:41–6. [Google Scholar]
- 9.Jeremiah ZA. Abnormal haemoglobin variants, ABO and Rh blood groups among student of African descent in Port Harcourt, Nigeria. Afr Health Sci. 2006;6:177–81. doi: 10.5555/afhs.2006.6.3.177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Akhigbe RE, Ige SF, Afolabi AO, Azeez OM, Adegunlola GJ, Bamidele JO. Prevalence of haemoglobin variants, ABO and rhesus blood groups in ladoke akintola University of Technology, Ogbomoso, Nigeria. Trends Med Res. 2009;4:24–9. [Google Scholar]
- 11.Egesie UG, Egesie OJ, Usar I, Johnbull TO. Distribution of ABO, Rhesus blood groups and haemoglobin electrophoresis among the undergraduate students of Niger Delta University Nigeria. Niger J Physiol Sci. 2008;23:5–8. doi: 10.4314/njps.v23i1-2.54900. [DOI] [PubMed] [Google Scholar]
- 12.Patel J, Patel A, Patel J, Kaur A, Patel V. Prevalence Of Haemoglobinopathies in Gujarat, India: A Cross-Sectional Study. Int J Hematol. 2009;5:1. [Google Scholar]
- 13.Swarup-Mitra S. Medical Genetics in India. In: Verma IC, editor. Vol. 2. Pondicherry: Auroma Enterprises; 1978. pp. 199–213. [Google Scholar]
- 14.Balgir RS. Spectrum of Hemoglobinopathies in the state of Orissa, India: A Ten years cohort study. J Assoc Physicians India. 2005;53:1021–6. [PubMed] [Google Scholar]


