Abstract
Background:
Slipped upper femoral epiphysis (SUFE) is the gradually acquired malalignment of the upper femoral epiphysis (capital) and the proximal femoral metaphysis. SUFE is uncommon in India, and there are no previous studies on outcome and clinical characteristics of patients with SUFE from India. This study evaluates the presentation, disease associations and outcome of SUFE from a tertiary care centre in India.
Materials and Methods:
Twenty six consecutive children with SUFE seen over a period of 4 years were reviewed. The clinical presentations, severity of the slip, surgical interventions (n=30) were assessed. Twenty one boys and five girls with a mean age 13.1 years (range 10-16 years) were included in the study. Four children had bilateral involvement. There were 4 rural and 22 urban children from the eastern and southern states of the country. The presentation was acute in 7, acute on chronic in 5, and chronic in 14, with a mean duration of symptoms of 51 days (range 3-120 days). Slips were stable in 16 and unstable in 10 children. Two children had adiposogenital syndrome. Body mass index was high in 12 out of 23 children. Vitamin D levels were low in 20 out of 21 children, with a mean vitamin D level of 12.61 ± 5 ng/ml. Eighteen children underwent in situ pinning. Eight children underwent capital realignment.
Results:
Clinical outcome as assessed by Merle d’ Aubigne score was excellent in 6, good in 10, fair in 6 and poor in 1. Half of the in situ fixation patients underwent osteoplasty procedure for femoroacetabular impingement and 5 more were symptomatic. The head neck offset and α angle after in situ pinning were −1.12 ± 3 mm and 66.05 ± 9.7°, respectively and this improved to 8.7 mm and 49°, respectively, after osteoplasty. One child in the pinning group had chondrolysis. Eight patients with severe slip underwent capital realignment. Mean followup was 20.15 months. The anterior head neck offset and α angle were corrected to 6.8 ± 1.72 mm and 44.6 ± 7.0° mm, respectively. Two children with unstable slip in the capital realignment group had avascular necrosis which was diagnosed at presentation by bone scan.
Conclusion:
High BMI, vitamin D deficiency and endocrine disorders are associated with SUFE in India and should be evaluated as some of these are amenable to prevention and treatment. Most patients treated with in situ pinning developed femoroacetabular impingement. The early results after capital realignment procedure are encouraging and help to avoid a second procedure which is needed in a majority of patients who underwent in situ pinning.
Keywords: Capital realignment, femoroacetabular impingement, modified dunn procedure, slipped upper femoral epiphysis
INTRODUCTION
Slipped upper femoral epiphysis (SUFE) is the gradually acquired malalignment of the upper femoral epiphysis (capital) and the proximal femoral metaphysis. Traditionally the SUFE is described as having slipped inferior and posterior; however recently, the slip is described as displacement of the femoral neck in relation to the upper femoral epiphysis (capital).1 While frequently the upper femoral epiphysis displaces inferior and posterior, occasionally the slip may be anterior2,3 or lateral.4,5 SUFE typically occurs during adolescence and has a male preponderance.6 Mechanical and endocrine abnormalities have been implicated in its causation.7
SUFE is regarded as stable when the child is able to ambulate with or without crutches and is considered unstable when this is not possible.8 The risk of avascular necrosis (AVN) is zero when SUFE is stable, whereas it may be as high as 58% after unstable SUFE.9,10,11 The most accepted treatment for stable slips entails fluoroscopic-guided in situ pinning with a single screw placed centrally in the epiphysis, avoiding any attempt at reduction of the slip.12 In situ pinning prevents further slippage, but has the long term consequence of head deformity.13,14,15,16,17,18 There is considerable debate about the method of treatment of unstable SUFE.19 The roles of reduction, methods of fixation and decompression are still controversial.13 Moderate and severe slips have been treated with reduction using surgical hip dislocation approach.20,21,22 Reconstruction options, typically reserved for the child with functional abnormality, include proximal femur osteotomy23,24,25,26 and surgical dislocation of the hip with excision of metaphyseal prominent bone [to remove the source of femoroacetabular impingement (FAI)] with or without flexion intertrochanteric osteotomy.27
SUFE is uncommon in India, and there are no previous studies on outcome and clinical characteristics of patients with SUFE from India. We reviewed the associated factors and outcomes of treatment of SUFE with in situ pinning and capital realignment through surgical dislocation by Ganz approach.28
MATERIALS AND METHODS
After obtaining approval from the institutional review board, we retrospectively reviewed the clinical records and radiographs of a consecutive series of 26 patients (21 boys and 5 girls) who had undergone treatment for SUFE at our institution over a period of 4 years [Figure 1a]. Hospital records were reviewed for patient demography, duration of symptoms, serum calcium and phosphate levels, serum alkaline phosphatase, serum creatinine, serum thyroid stimulating hormone (TSH), and 25-hydroxyvitamin D [25(OH) D] level. When the duration of the symptoms was less than 3 weeks, it was classified as acute; when it was for 3 weeks or more, it was classified as chronic; and if the prodromal symptoms were present prior to slip, it was considered as acute on chronic.
Figure 1.
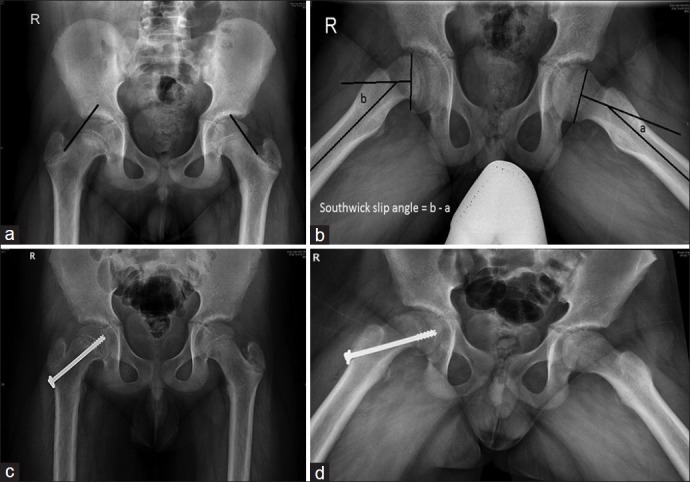
X-ray pelvis with both hip joints (a) Anteroposterior view of a 15-year-old boy showing a mild slip. The blurring of physis (Blanch sign) and capital epiphysis dipping below the Klein's line are observed. (b) Frog leg lateral view of the same child showing slip angle (Southwick) measuring 20° on the right side. (c and d) AP and frog leg lateral views showing a centrally placed cannulated screw crossing the physis
Body mass index (BMI) was calculated as weight in kilograms divided by the square of height in meters (kg/m2). Children were categorized according to BMI as underweight (<18.5 kg/m2), normal (18.5–24.99 kg/m2), overweight (25–29.99 kg/m2), and obese (>30 kg/m2).29
The slips were described as stable or unstable based on the clinical history at the time of presentation as suggested by Loder et al.8 The details of primary surgical procedure and any additional procedure for FAI were noted. Radiographs were retrieved from picture archiving and communication system and reviewed for the presence or absence of a crossover sign according to the definitions of Reynolds et al.30 Preoperative head shaft angle on frog leg lateral or cross leg lateral view was measured. The severity of each patient's slip was determined through interpretation of the frog leg lateral radiographs taken at the time of presentation [Figure 1b]. Slip severity was graded as mild, moderate, or severe according to the head shaft angle of the affected hip subtracted from the unaffected side on frog leg lateral.1,26 The slip angle for the bilateral slips was calculated by subtracting 10° from the measured slip angle.26 Radiologically, the α angle of Notzli was measured on the frog leg lateral view. The α angle is the angle between the axis of the neck and a line drawn to the center of the head from a point where the head loses its sphericity. Values above 50.5° are abnormal and indicate radiological impingement.31 The head shaft angle and α angle were measured using picture archival and communication system (PACS) (centricity enterprise web, GE Medical Systems 3, 2006; GE healthcare, New York, USA).
Bone scans were done in four children with a high suspicion of AVN in late presentation of unstable severe slips in some and increased density of the head or wide displacement at the slip.
Among 18 patients, 16 underwent in situ pinning for stable slips and 2 children underwent the same for unstable slips. The surgical aim was to insert a single cannulated screw in the center of the epiphysis with at least three threads across the physis [Figure 1c and d]. Eight patients underwent safe surgical dislocation and realignment procedure for unstable slips [Figure 2]. Intraoperative head vascularity assessment ensured that there was no tension on the vascular pedicle.32 Nine patients with in situ pinning underwent osteoplasty for FAI as a secondary procedure after the fusion of the growth plate at a mean of 13.3 months (range 11-16 months) after in situ pinning [Figure 3]. Two of these in addition required simultaneous subtrochanteric osteotomy to correct varus and external rotation deformity [Figure 4]. Five more were symptomatic. All these children had external rotation deformity and functional limitation of range of motion resulting in difficulty in squatting. Impingement was present on flexion and adduction.
Figure 2.
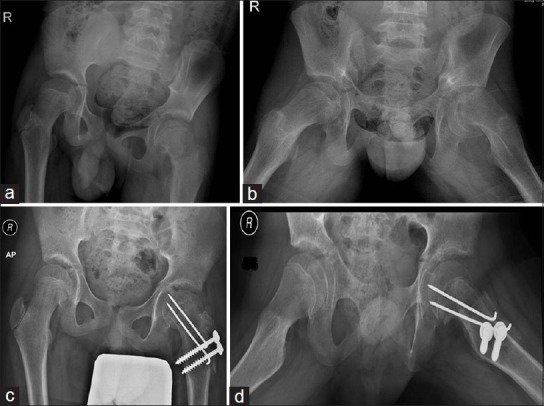
X-ray pelvis with both hip joints (a and b) A 12-year-old showing severe slip (Southwick 75°) on the left side. (c and d) AP and frog leg lateral radiographs 2 months after capital realignment through Ganz safe surgical dislocation approach for the hip
Figure 3.
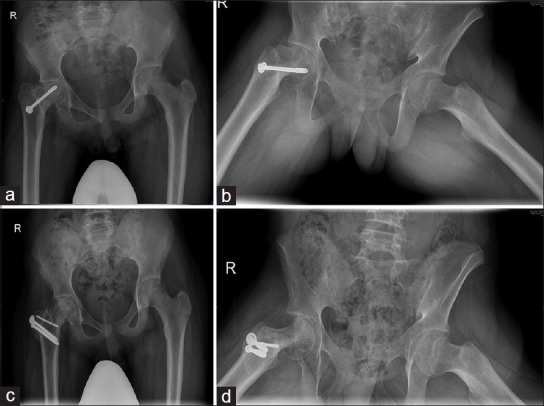
X-ray pelvis with both hip joints (a and b) A 13-year-old boy presented with chronic (duration 120 days), stable and severe slip 80° on the right side. (c) Two-year post operative in situ pinning with clinical impingement showing femoroacetabular impingement. (d) Postoperative radiographs of in situ pinning and osteoplasty
Figure 4.

X-ray pelvis showing both hips (a) and left hip frog leg view (b) in a 14-year-old boy presented with acute, unstable, and severe slip measuring 72° (Southwick angle) and initially treated with a single cannulated screw. The patient was symptomatic for impingement, southwick° angle was 75° and head neck offset was negative, i.e. neck with larger radius than head. (c and d) Six weeks after osteoplasty through Ganz approach combined with subtrochanteric osteotomy to correct varus, rotation, and extension deformity
Clinical outcome assessment was done by Merle d’ Aubigne-Postel score.33 Head shaft angle and α angle were also assessed similar to the preoperative workup. Radiological evidence of AVN was recorded if there was collapse or sclerosis of the femoral head. Chondrolysis was diagnosed if there was loss of 50% of the joint space or the joint space was less than 3 mm in patients with bilateral SUFE.1,34
The statistical analysis was performed using statistical package for social services (SPSS) software version 16. Student's t-test was used to test the significance of difference of means.
RESULTS
The mean age at the time of presentation for boys was 13.33 ± 1.44 years (range 11-16 years) and for girls was 11 ± 0.83 years (range 10-13 years). Four children had bilateral SUFE, totaling 30 hips. The left side was involved in 13 and the right side in 17. Seven children had acute, 5 had acute on chronic, and 14 had chronic slips when classified according to the traditional method of classification; the mean duration of slip was 50.96 ± 34.48 days (range 3-120 days). There were 16 children with stable and 10 with unstable slips. One child had mild (Southwick slip angle < 30°), 8 (30.77%) children had moderate (slip angle 31° − 60°), and 17 (65.38%) children had severe slips (slip angle > 60°).
Radiological evaluation showed bilateral acetabular retroversion in nine and unilateral in two children. Since this incidence was less than that reported in normal children, acetabular retroversion was not included as a risk factor during assessment of the associated risk factors.35
In two children, diagnosis of adiposogenital syndrome was made by endocrinologist based on the presence of hypogonadism and high BMI. One child was underweight (<18.5 kg/m2), 11 were normal (18.5-24.99 kg/m2), 10 were overweight (25-29.99 kg/m2), and 2 had class I obesity (30-34.99 kg/m2). The BMI could not be calculated for three children as the height and weight data at the time of surgery were not available. Other biochemical parameters checked included TSH, serum creatinine, serum calcium, phosphate, and alkaline phosphatase, and were found to be within normal limits. Vitamin D [25(OH) D] levels were available for 21 out of 26 patients and the mean vitamin D level was 12.61 ± 5.4 ng/ml (range 3.76-25.6 ng/ml). Twenty out of twenty one patients were severely vitamin D deficient. There were no rachitic changes on radiographs. Affected children were treated with vitamin D and calcium supplements. Mean duration of followup was 20.15 ± 14.13 months (range 4-48 months). Of a total of 26 children, 1 had no associated metabolic or endocrine disorder. Twenty five patients had at least one associated condition. Of these 25 children, 8 children had at least two and 1 had three associated risk factors.
Eighteen patients underwent in situ pinning; four of these were bilateral. Five of these patients also underwent prophylactic pinning of the opposite hip. The indications for prophylactic pinning were young age, obesity, or endocrine disease. All these patients had decreased internal rotation with a mean of 13.2° (range = −30° to 40°) internal rotation. All three lines should be deleted as updated clinical outcome given after 3-4 lines [Table 1]. Nine patients underwent a secondary osteoplasty procedure for FAI and two of these had an additional subtrochanteric realignment osteotomy. Five more children are clinically symptomatic with radiological impingement and are awaiting surgery. Out of the 18 patients in the in situ group, 10 had severe slip (mean slip angle 72.3°), 7 had moderate slip, and 1 had mild slip. Based on Merle d’ Aubigne-Postel score, one patient had excellent, eight had good, six had fair, and three had poor outcome [Table 1]. The head neck offset and α angle on followup after in situ pinning were 1.1. ± 3.0 mm and 66 ± 9.7°, respectively. One child, who had undergone pinning, developed chondrolysis with a uniform reduction in the joint space [Figure 5]. This complication was attributable to articular penetration by the screw.
Table 1.
Characteristics and outcomes of patients treated with different strategies for SUFE
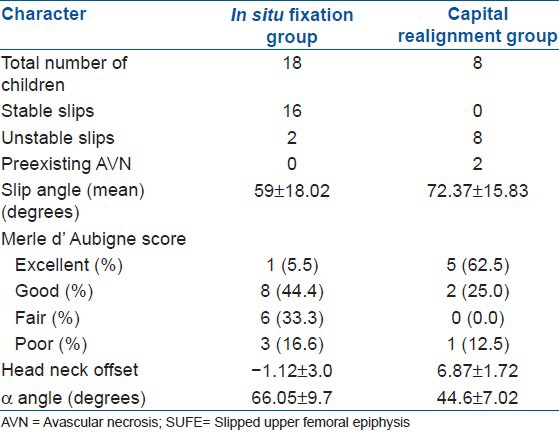
Figure 5.
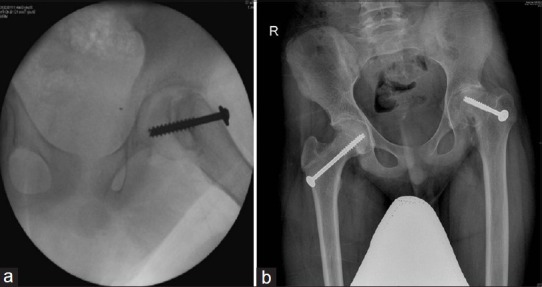
(a) Fluoroscopic anteroposterior view in a 14-year-old boy managed for chronic, severe slip on the left side with in situ pinning intraoperative image showing six threads crossing physis. (b) postoperative anteroposterior radiograph at nine months showing reduction in the joint space
Eight patients underwent safe surgical dislocation and realignment. All but one had severe slips with a mean slip angle of 72.33 ± 15.83° (range 45°-95°). The slip angle at final followup was 4.83 ± 2.01°. Average internal rotation was 44° (range 20°-50°). Based on Merle d’ Aubigne-Postel score, four patients had excellent, three had good, and one had poor outcome. The anterior head neck offset and α angle were 6.8 ± 1.7 mm and 44.6 ± 7.0°, respectively. Two children had AVN, one with a poor and another with a good outcome. In both these children who had severe unstable late slips, AVN was recorded preoperatively on the bone scan [Figure 6] [Table 1].
Figure 6.
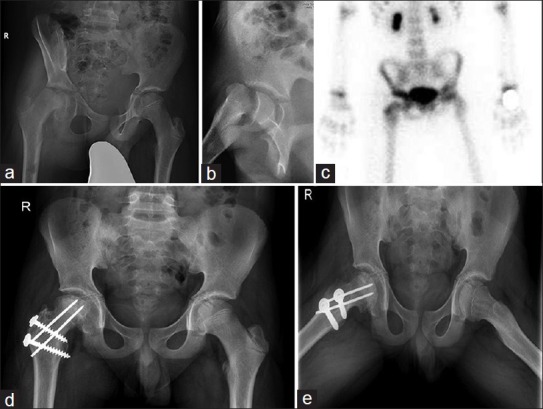
X-ray pelvis showing both hips anteroposterior view (a) and right hip frog leg lateral view (b) in a 14-year-old boy showing unstable, severe slip of 2 months duration. There is an increased density of the capital femoral epiphysis and Southwick slip angle of 80° (c) Bone scan at presentation before surgery showing decreased uptake in the femoral head. (d and e) Radiographs taken at 1 year post capital realignment through Ganz approach showing fused physis, increased density of the femoral head due to avascular necrosis
DISCUSSION
SUFE is not common, although a few case reports of SUFE have been published in the English literature.36,37,38,39 The known etiologies for SUFE include endocrinopathies, renal osteodystrophy and radiation.1,7 Our study found that a majority of SUFE were associated with endocrine or metabolic disorder [Figure 7].
Figure 7.
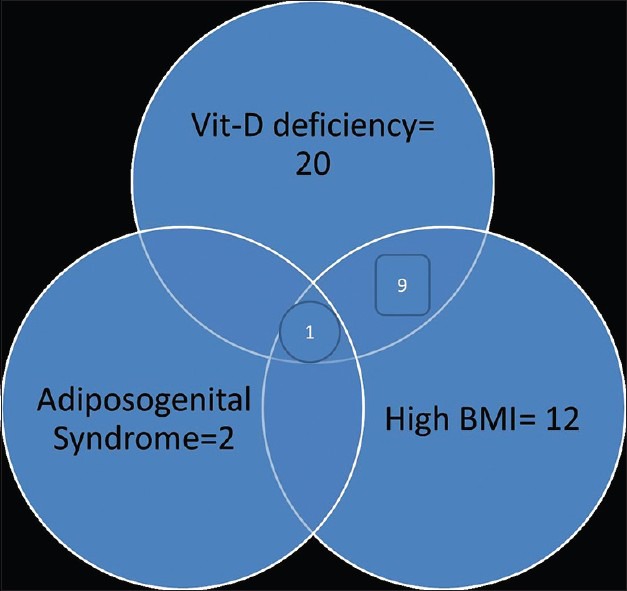
Associated risk factors in SUFE
The associated conditions looked for in this study were endocrine (hypothyroidism, hyperthyroidism, hyperparathyroidism, adiposogenital syndrome) and metabolic factors (low BMI and hypovitaminosis D). Other mechanical factors implicated such as retroversion of the acetabulum were also screened as an association is reported with SUFE in some series.40
In our study, overweight and class I obesity was seen in more than 50% of the affected children. Morrey and Wilson have shown a definite link to obesity and increasing incidence of SUFE in Scotland.41 The prominent metabolic disease associated with SUFE is renal osteodystrophy.42 There is one study which shows an association of SUFE with transient deficiency of parathyroid hormone and 1,25-dihydroxy vitamin D [1,25-(OH)2D], a transient active form of vitamin D, in Japanese children.43 There are no series describing vitamin D deficiency as an associated factor, although there is a single case report of vitamin D deficiency diagnosed 9 months after a failed pinning of the slip.44 In our study, there was deficiency of vitamin D levels in all but one of the children where it was measured. Obesity, usually associated with vitamin D deficiency, is a known risk factor.45,46 The possible reasons for the vitamin D deficiency being associated with SUFE may be the sedentary lifestyle of an obese child with decreased sunlight exposure. Obesity also has a known association with SUFE.6,13,41 A low vitamin D could affect the stability and vigour of the growth plate due to defective mineralization.
Other factors such as endocrinopathies (adiposogenital syndrome) were found in only a small proportion of children with SUFE. Mechanical factors such as acetabular retroversion were not found to be significantly more in the affected children with SUFE as compared to the reported prevalence in normal children.35
Age in this study was higher than that being reported from other countries currently, but is similar to that from older studies, and we postulate that we would see an increase in incidence and lowering of age as the lifestyle changes come to our population.6,9 Boys had a higher incidence than girls, which is similar to the trend reported in the literature probably because the boys are more active and are at risk for a longer period.1,6
In grades 1 and 2, in situ fixation using a single screw is considered to be the optimal management.47 In situ fixation without delay and without reduction has been the mainstay of primary treatment for most cases of clinically stable SUFE for decades.48 Several recent studies have recommended in situ fixation with a single cannulated screw rather than any gentle repositioning with two screws.10,19 In our study, the mild and moderate slips were in a minority, with only about 35% falling in these grades. Larsen et al. in their study of long term outcomes of in situ pinning found that one third of the patients treated for SUFE had residual pain and 10% of patients at 10 years underwent reconstructive surgery. Five percent of their patients were likely to develop arthritis severe enough to warrant total hip arthroplasty 20 years after surgery. In their series, a relatively high percentage of patients who developed severe arthritis had mild or moderate slips.49 In our series, 77% of children with in situ pinning required a second surgery for either an FAI or deformity within 4 years. In Larsen's series of over 40 years, the majority of the slips, 107 out of 176, were mild. In our series of in situ pinning, only one slip was mild. Difference in the severity between the two series explains why we have more symptomatic patients even in the short term as most had residual deformity at the end of pinning itself. Their reason for surgery was intractable pain and persistent disability and included nine osteotomies, three total hip replacements, and two safe surgical dislocations. Our reason for surgery was limitation of motion and pain during function. With a better current understanding of FAI, it is understood that the treatment for FAI needs to be applied early to avoid osteoarthritis rather than to do salvage after the onset of osteooarthitis. Our observations suggest that in severe slips, pinning is not a definitive procedure and the family needs to be warned regarding the need for a second surgery even though traditionally the results of uncomplicated SUFE after pinning have been considered to be good.
Based on our data, about 90% of this moderate to severely affected group required or would require surgical dislocation for either capital realignment or definitive surgery. Does this mean that there is a case for all children including stable slips to be treated with Ganz approach? In our opinion, when recommending this treatment, the real issue is that of safeguarding vascularity. It is more difficult to peel the thin periosteum in older children with stable slips, hence we suggest that older children with stable slips be stabilized by pinning and undergo osteoplasty and/or osteotomy after the physeal closure.20 The experience of the Boston/Swiss groups suggests that the capital realignment is most appropriate for moderate to severe unstable slips, but can be performed even in those stable slips where the physis tends to be mobile.21
Castaneda et al. found that after an average of 22.3 years followup, all their patients had radiographic evidence of osteoarthritis. 79% of their patients had FAI, 80% had pistol grip deformity and had significantly lower Harris hip scores.50 The FAI in children with in situ pinning may be due to asphericity caused by the neck bump, retroversion of the femur and acetabulum, and shortening of the femoral neck.14,18 These issues can be addressed by osteoplasty for the neck bump and realignment osteotomies such as subcapital Dunn osteotomy24, basal neck osteotomy,25 and flexion intertrochanteric osteotomy.26 However, all of these carry a significant risk of complications. Milder impingement due to neck bump to some extent can be addressed by an arthroscopic osteoplasty.51 Our findings are in concordance with the study by Castaneda50 as we found that most of our children who had undergone pinning had clinical and radiological features of impingement. In our study, out of 18 children who had undergone pinning for their slips, all had an abnormal α angle. The minimum α angle was 56° and the highest was 80°. Head neck offset was also reduced and ranged from - 6 to + 4 mm, indicating that radiologically all of them had impingement though correction is planned only for the symptomatic children. We emphasize that impingement following in situ pinning is a common occurrence and should not be underestimated in SUFE.
AVN of the capital epiphysis is a dreaded complication in SUFE. It could be attributed to either the slip itself due to kinking and damage to the retinacular vessels51 or increased intracapsular pressure developing during the slip.52 This can be made worse by the delay in the stabilization of the slip.53 The incidence is higher in young patients with a more acute onset of symptoms.54 The reported rates of incidence vary from 0% in stable slips to as high as 58% in unstable slips.9,10,11 The AVN rate in this series was 7.6%. The AVN in the two cases was suspected and documented by a preoperative bone scan and was attributable to preoperative severe unstable slip compounded by a significant delay of several months in the management. The intraoperative head vascularity monitoring showed no pressure wave on exposing the hip and no improvement in blood flow after reduction of the slip, confirming the permanent loss of vascularity which was the reason for the poor outcome in these two hips. The other known contributory factors for AVN in SUFE are a forceful reduction maneuver, certain kind of osteotomies such as subcapital osteotomy of Dunn, and neck osteotomies for correction of deformity.24,55,56,57 The Ganz safe surgical dislocation approach has been popularized by him and others to provide a safe access both for acute procedures such as capital realignment and for reconstructive procedures such as osteoplasty. In this study, this approach was used for acute realignment in eight cases and for osteoplasty in nine cases with no adverse outcomes or AVN attributable to the surgical procedure. Some children undergoing osteoplasty also required osteotomy which was carried out at the subtrochanteric level at the same sitting.
The other major complication in SUFE is chondrolysis. The incidence of chondrolysis varies from 1.5% to 50%.1 Chondrolysis or cartilage necrosis can occur in untreated slips, but is often associated with spica cast immobilization or penetration of the internal fixation screws into the joint space. In our study, the rate of chondrolysis was less than 4%. The one case of chondrolysis was due to inadvertent screw penetration into the joint space. The symptoms and range of movement improved after screw removal. Further improvement in the range of movement could be achieved by osteoplasty after surgical dislocation and this was the treatment followed by us. Chondrolysis can be avoided by careful pin placement during in situ pinning. The central position of the threaded screw in the center of the epiphysis, crossing the physis by no more than three threads, continuous screening in both planes to observe the pin regressing from the head outline and injection of a radiopaque dye using a cannula through the screw to look for the articular cartilage breach are some of the steps to enhance the safety of the pinning technique.
The limitations of this study are its short followup and the retrospective nature with small sample size. The smaller numbers are because of the relative rarity of this condition in our population.6 Number of patients treated with capital realignment and osteoplasty in this series is quite high with a low incidence of FAI as a consequence, making it noteworthy.
In conclusion, vitamin D deficiency and increased body weight are the major associated factors with SUFE in our study. In situ pinning is a safe alternative to the surgical dislocation technique in centers lacking technical expertise for surgical dislocation. FAI is a common occurrence following in situ pinning requiring secondary procedures. Safe surgical dislocation and capital realignment with meticulous technique to safeguard and monitor vascularity in unstable moderate to severe slips does not result in FAI and obviates the need for secondary procedures.
Footnotes
Source of Support: Nil
Conflict of Interest: None
REFERENCES
- 1.Herring JA, Tachdjian MO. 4th ed. Philadelphia: Saunders Elsevier; 2008. Tachdjian's pediatric orthopaedics; pp. 716–20. [Google Scholar]
- 2.Sasaki M, Nagoya S, Kaya M, Yamashita T. Anterior slip of the capital femoral epiphysis. A case report. J Bone Joint Surg Am. 2007;89:855–8. doi: 10.2106/JBJS.F.00322. [DOI] [PubMed] [Google Scholar]
- 3.Duncan JW, Lovell WW. Anterior slip of the capital femoral epiphysis. Report of a case and discussion. Clin Orthop Relat Res. 1975;110:171–3. doi: 10.1097/00003086-197507000-00022. [DOI] [PubMed] [Google Scholar]
- 4.García-Mata S, Hidalgo-Ovejero A. Valgus slipped capital femoral epiphysis. Iowa Orthop J. 2010;30:191–4. [PMC free article] [PubMed] [Google Scholar]
- 5.Loder RT, O’Donnell PW, Didelot WP, Kayes KJ. Valgus slipped capital femoral epiphysis. J Pediatr Orthop. 2006;26:594–600. doi: 10.1097/01.bpo.0000230331.96157.14. [DOI] [PubMed] [Google Scholar]
- 6.Loder RT. The demographics of slipped capital femoral epiphysis. An international multicenter study. Clin Orthop Relat Res. 1996;322:8–27. [PubMed] [Google Scholar]
- 7.Morrissy, Raymond T, Weinstein M, Stuart L. 6th ed. Philadelphia: Lippincott Williams and Wilkins; 2006. Lovell and Winter's Pediatric Orthopaedics; pp. 1086–8. [Google Scholar]
- 8.Loder RT, Richards BS, Shapiro PS, Reznick LR, Aronson DD. Acute slipped capital femoral epiphysis: The importance of physeal stability. J Bone Joint Surg Am. 1993;75:1134–40. doi: 10.2106/00004623-199308000-00002. [DOI] [PubMed] [Google Scholar]
- 9.Mulgrew E, Wells-Cole S, Ali F, Joshy S, Siddique I, Zenios M. Single screw fixation in stable and unstable slipped upper femoral epiphysis. J Pediatr Orthop B. 2011;20:147–51. doi: 10.1097/BPB.0b013e328344e76d. [DOI] [PubMed] [Google Scholar]
- 10.Tokmakova KP, Stanton RP, Mason DE. Factors influencing the development of osteonecrosis in patients treated for slipped capital femoral epiphysis. J Bone Joint Surg Am. 2003;85-A:798–801. doi: 10.2106/00004623-200305000-00004. [DOI] [PubMed] [Google Scholar]
- 11.Loder RT. Unstable slipped capital femoral epiphysis. J Pediatr Orthop. 2001;21:694–9. [PubMed] [Google Scholar]
- 12.Morrissy RT. Slipped capital femoral epiphysis technique of percutaneous in situ fixation. J Pediatr Orthop. 1990;10:347–50. doi: 10.1097/01241398-199005000-00010. [DOI] [PubMed] [Google Scholar]
- 13.Loder RT, Aronsson DD, Weinstein SL, Breur GJ, Ganz R, Leunig M. Slipped capital femoral epiphysis. Instr Course Lect. 2008;57:473–98. [PubMed] [Google Scholar]
- 14.Fraitzl CR, Käfer W, Nelitz M, Reichel H. Radiological evidence of femoroacetabular impingement in mild slipped capital femoral epiphysis: A mean followup of 14.4 years after pinning in situ. J Bone Joint Surg Br. 2007;89:1592–6. doi: 10.1302/0301-620X.89B12.19637. [DOI] [PubMed] [Google Scholar]
- 15.Mamisch TC, Kim YJ, Richolt JA, Millis MB, Kordelle J. Femoral morphology due to impingement influences the range of motion in slipped capital femoral epiphysis. Clin Orthop Relat Res. 2009;467:692–8. doi: 10.1007/s11999-008-0477-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Miese FR, Zilkens C, Holstein A, Bittersohl B, Kröpil P, Jäger M, et al. MRI morphometry, cartilage damage and impaired function in the followup after slipped capital femoral epiphysis. Skeletal Radiol. 2010;39:533–41. doi: 10.1007/s00256-010-0903-7. [DOI] [PubMed] [Google Scholar]
- 17.Dodds MK, McCormack D, Mulhall KJ. Femoroacetabular impingement after slipped capital femoral epiphysis: Does slip severity predict clinical symptoms? J Pediatr Orthop. 2009;29:535–9. doi: 10.1097/BPO.0b013e3181b2b3a3. [DOI] [PubMed] [Google Scholar]
- 18.Millis MB, Novais EN. In situ fixation for slipped capital femoral epiphysis: Perspectives in 2011. J Bone Joint Surg Am. 2011;93(Suppl 2):46–51. doi: 10.2106/JBJS.K.00040. [DOI] [PubMed] [Google Scholar]
- 19.Mooney JF, 3rd, Sanders JO, Browne RH, Anderson DJ, Jofe M, Feldman D, et al. Management of unstable/acute slipped capital femoral epiphysis: Results of a survey of the POSNA membership. J Pediatr Orthop. 2005;25:162–6. doi: 10.1097/01.bpo.0000151058.47109.fe. [DOI] [PubMed] [Google Scholar]
- 20.Ziebarth K, Zilkens C, Spencer S, Leunig M, Ganz R, Kim YJ. Capital realignment for moderate and severe SCFE using a modified Dunn procedure. Clin Orthop Relat Res. 2009;467:704–16. doi: 10.1007/s11999-008-0687-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Slongo T, Kakaty D, Krause F, Ziebarth K. Treatment of slipped capital femoral epiphysis with a modified Dunn procedure. J Bone Joint Surg Am. 2010;92:2898–908. doi: 10.2106/JBJS.I.01385. [DOI] [PubMed] [Google Scholar]
- 22.Sink EL, Zaltz I, Heare T, Dayton M. Acetabular cartilage and labral damage observed during surgical hip dislocation for stable slipped capital femoral epiphysis. J Pediatr Orthop. 2010;30:26–30. doi: 10.1097/BPO.0b013e3181c6b37a. [DOI] [PubMed] [Google Scholar]
- 23.Abraham E, Garst J, Barmada R. Treatment of moderate to severe slipped capital femoral epiphysis with extracapsular base-of-neck osteotomy. J Pediatr Orthop. 1993;13:294–302. doi: 10.1097/01241398-199305000-00004. [DOI] [PubMed] [Google Scholar]
- 24.Dunn DM. The treatment of adolescent slipping of the upper femoral epiphysis. J Bone Joint Surg Br. 1964;46:621–9. [PubMed] [Google Scholar]
- 25.Kramer WG, Craig WA, Noel S. Compensating osteotomy at the base of the femoral neck for slipped capital femoral epiphysis. J Bone Joint Surg Am. 1976;58:796–800. [PubMed] [Google Scholar]
- 26.Southwick WO. Osteotomy through the lesser trochanter for slipped capital femoral epiphysis. J Bone Joint Surg Am. 1967;49:807–35. [PubMed] [Google Scholar]
- 27.Kuzyk PR, Kim YJ, Millis MB. Surgical management of healed slipped capital femoral epiphysis. J Am Acad Orthop Surg. 2011;19:667–77. doi: 10.5435/00124635-201111000-00003. [DOI] [PubMed] [Google Scholar]
- 28.Ganz R, Gill TJ, Gautier E, Ganz K, Krügel N, Berlemann U. Surgical dislocation of the adult hip a technique with full access to the femoral head and acetabulum without the risk of avascular necrosis. J Bone Joint Surg Br. 2001;83:1119–24. doi: 10.1302/0301-620x.83b8.11964. [DOI] [PubMed] [Google Scholar]
- 29.WHO Expert Consultation. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet. 2004;363:157–63. doi: 10.1016/S0140-6736(03)15268-3. [DOI] [PubMed] [Google Scholar]
- 30.Reynolds D, Lucas J, Klaue K. Retroversion of the acetabulum. A cause of hip pain. J Bone Joint Surg Br. 1999;81:281–8. doi: 10.1302/0301-620x.81b2.8291. [DOI] [PubMed] [Google Scholar]
- 31.Nötzli HP, Wyss TF, Stoecklin CH, Schmid MR, Treiber K, Hodler J. The contour of the femoral head-neck junction as a predictor for the risk of anterior impingement. J Bone Joint Surg Br. 2002;84:556–60. doi: 10.1302/0301-620x.84b4.12014. [DOI] [PubMed] [Google Scholar]
- 32.Madhuri V, Dutt V, Samuel K, Gahukamble AD. Intraoperative femoral head vascularity assessment: An innovative and simple technique. Indian J Orthop. 2011;45:231–5. doi: 10.4103/0019-5413.80041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.D’aubigne RM, Postel M. Functional results of hip arthroplasty with acrylic prosthesis. J Bone Joint Surg Am. 1954;36-A:451–75. [PubMed] [Google Scholar]
- 34.Waldenström H. On necrosis of the joint cartilage by epiphyseolysis capitis femoris.1930. Clin Orthop Relat Res. 1996;322:3–7. [PubMed] [Google Scholar]
- 35.Stanitski CL, Woo R, Stanitski DF. Acetabular version in slipped capital femoral epiphysis: a prospective study. J Pediatr Orthop B. 1996;5:77–9. doi: 10.1097/01202412-199605020-00004. [DOI] [PubMed] [Google Scholar]
- 36.Oommen AT, Madhuri V, Paul TV. Slipped upper femoral epiphysis in Hashimoto's thyroiditis in a 29-year-old man. J Bone Joint Surg Br. 2009;91:666–9. doi: 10.1302/0301-620X.91B5.22160. [DOI] [PubMed] [Google Scholar]
- 37.Venkatadass K, Shetty AP, Rajasekaran S. Valgus slipped capital femoral epiphysis: Report of two cases and a comprehensive review of literature. J Pediatr Orthop B. 2011;20:291–4. doi: 10.1097/BPB.0b013e328346d2ec. [DOI] [PubMed] [Google Scholar]
- 38.Shah H, Singh G, Vijayan S, Girisha KM. Second report of slipped capital femoral epiphysis in Rubinstein-Taybi syndrome. Clin Dysmorphol. 2011;20:55–7. doi: 10.1097/MCD.0b013e32833f000b. [DOI] [PubMed] [Google Scholar]
- 39.Jacob J, Paul T. A boy with a limp. Slipped capital femoral epiphysis. N Z Med J. 2007;120:U2447. [PubMed] [Google Scholar]
- 40.Sankar WN, Brighton BK, Kim YJ, Millis MB. Acetabular morphology in slipped capital femoral epiphysis. J Pediatr Orthop. 2011;31:254–8. doi: 10.1097/BPO.0b013e31820fcc81. [DOI] [PubMed] [Google Scholar]
- 41.Murray AW, Wilson NI. Changing incidence of slipped capital femoral epiphysis: A relationship with obesity? J Bone Joint Surg Br. 2008;90:92–4. doi: 10.1302/0301-620X.90B1.19502. [DOI] [PubMed] [Google Scholar]
- 42.Oppenheim WL, Bowen RE, McDonough PW, Funahashi TT, Salusky IB. Outcome of slipped capital femoral epiphysis in renal osteodystrophy. J Pediatr Orthop. 2003;23:169–74. [PubMed] [Google Scholar]
- 43.Jingushi S, Hara T, Sugioka Y. Deficiency of a parathyroid hormone fragment containing the midportion and 1,25-dihydroxyvitamin D in serum of patients with slipped capital femoral epiphysis. J Pediatr Orthop. 1997;17:216–9. doi: 10.1097/00004694-199703000-00015. [DOI] [PubMed] [Google Scholar]
- 44.Skelley NW, Papp DF, Lee RJ, Sargent MC. Slipped capital femoral epiphysis with severe vitamin D deficiency. Orthopedics. 2010;33:921. doi: 10.3928/01477447-20101021-27. [DOI] [PubMed] [Google Scholar]
- 45.Olson ML, Maalouf NM, Oden JD, White PC, Hutchison MR. Vitamin D deficiency in obese children and its relationship to glucose homeostasis. J Clin Endocrinol Metab. 2012;97:279–85. doi: 10.1210/jc.2011-1507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Grethen E, McClintock R, Gupta CE, Jones R, Cacucci BM, Diaz D, et al. Vitamin D and hyperparathyroidism in obesity. J Clin Endocrinol Metab. 2011;96:1320–6. doi: 10.1210/jc.2010-2202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.O’Brien ET, Fahey JJ. Remodeling of the femoral neck after in situ pinning for slipped capital femoral epiphysis. J Bone Joint Surg Am. 1977;59:62–8. [PubMed] [Google Scholar]
- 48.Aronson DD, Carlson WE. Slipped capital femoral epiphysis. A prospective study of fixation with a single screw. J Bone Joint Surg Am. 1992;74:810–9. [PubMed] [Google Scholar]
- 49.Larson AN, Sierra RJ, Yu EM, Trousdale RT, Stans AA. Outcomes of slipped capital femoral epiphysis treated with in situ pinning. J Pediatr Orthop. 2012;32:125–30. doi: 10.1097/BPO.0b013e318246efcb. [DOI] [PubMed] [Google Scholar]
- 50.Castaneda P. The natural history of osteoarthritis after a slipped capital femoral epiphysis/The pistol grip deformity. Proceedings of POSNA One Day Course 2012: Adolescent and Young Adult Hip Disorders May 16, 2:00.2:10. [Last accessed date 2012 December 18]. Available from: http://www.mosbrookdesign.com/POSNA/ODC/Contents/files/18_Castaneda.pdf .
- 51.Leunig M, Horowitz K, Manner H, Ganz R. In situ pinning with arthroscopic osteoplasty for mild SCFE: A preliminary technical report. Clin Orthop Relat Res. 2010;468:3160–7. doi: 10.1007/s11999-010-1408-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Herrera-Soto JA, Duffy MF, Birnbaum MA, Vander Have KL. Increased intracapsular pressures after unstable slipped capital femoral epiphysis. J Pediatr Orthop. 2008;28:723–8. doi: 10.1097/BPO.0b013e318186bda3. [DOI] [PubMed] [Google Scholar]
- 53.Rached E, Akkari M, Braga SR, Minutti MF, Santili C. Slipped capital femoral epiphysis: Reduction as a risk factor for avascular necrosis. J Pediatr Orthop B. 2012;21:331–4. doi: 10.1097/BPB.0b013e32835368a7. [DOI] [PubMed] [Google Scholar]
- 54.Sankar WN, McPartland TG, Millis MB, Kim YJ. The unstable slipped capital femoral epiphysis: Risk factors for osteonecrosis. J Pediatr Orthop. 2010;30:544–8. doi: 10.1097/BPO.0b013e3181e4f372. [DOI] [PubMed] [Google Scholar]
- 55.Gage JR, Sundberg AB, Nolan DR, Sletten RG, Winter RB. Complications after cuneiform osteotomy for moderately or severely slipped capital femoral epiphysis. J Bone Joint Surg Am. 1978;60:157–65. [PubMed] [Google Scholar]
- 56.DeRosa GP, Mullins RC, Kling TF., Jr Cuneiform osteotomy of the femoral neck in severe slipped capital femoral epiphysis. Clin Orthop Relat Res. 1996;322:48–60. [PubMed] [Google Scholar]
- 57.Maeda S, Kita A, Funayama K, Kokubun S. Vascular supply to slipped capital femoral epiphysis. J Pediatr Orthop. 2001;21:664–7. [PubMed] [Google Scholar]


