Abstract
Context
Thirty day readmission rates have become a publicly reported quality performance measure for congestive heart failure (CHF), acute myocardial infarction (AMI), and percutaneous coronary intervention (PCI). However, little is known regarding the factors associated with 30-day readmission after PCI.
Objective
To assess the demographic, clinical, and procedural factors associated with 30-day readmission rates after PCI.
Design, Setting, and Patients
We identified 15,498 PCI hospitalizations (elective or for acute coronary syndromes) from January 1998 through June 2008 at Saint Marys Hospital, Rochester, MN. All were included in this analysis. Multivariable logistic regression models were employed to estimate the adjusted association between demographic, clinical, and procedural variables and 30-day readmission. The association between 30-day readmission and 1-year mortality was estimated using Cox proportional hazards models with readmission as a time dependent covariate and by using landmark analysis.
Main Outcome Measure(s)
All-cause 30-day readmission to any hospital following PCI and 1-year mortality.
Results
Overall, 9.4% of PCIs (n=1,459) were readmitted and 0.68% (n=106) of PCIs resulted in death within 30-days after discharge. After multivariable analysis, female sex, Medicare insurance, less than a high school education, unstable angina, cerebrovascular accident/transient ischemic attack (CVA/TIA), moderate/severe renal disease, chronic obstructive pulmonary disease (COPD), peptic ulcer disease, metastatic cancer, and a length of stay >3 days were associated with an increased risk of 30-day readmission after PCI. Thirty-day readmission after PCI was associated with a higher risk of 1-year mortality (adjusted HR=1.38; 95% CI: 1.08–1.75; p=0.009).
Conclusions
Nearly 1 in 10 patients undergoing PCI were readmitted within 30-days. Thirty-day readmission after PCI was associated with a higher risk of 1-year mortality.
Introduction
Thirty-day readmission rates have become a quality performance measure and the Center for Medicare and Medicaid Services (CMS) publicly reports hospital-level 30-day risk-standardized readmission rates for patients hospitalized with congestive heart failure (CHF), acute myocardial infarction (AMI), and for patients undergoing percutaneous coronary intervention (PCI).1–3 The Patient Protection and Affordable Care Act of 2010 will link quality outcomes, such as 30-day readmission rates, to hospital reimbursement with the expected implementation of value-based purchasing.4–6 Hence, there is great interest from hospitals and clinicians to understand and improve modifiable factors associated with 30-day readmission rates.
PCIs are among the most common procedures performed in the United States and a recent analysis of Medicare beneficiaries who underwent PCI in 2005 demonstrated that 30-day readmission and mortality rates were 14.6% and 1.0%, respectively, and that readmitted patients had a higher risk of 30-day mortality.7 However, we have limited knowledge regarding demographic, clinical, and procedural factors associated with 30-day readmission after PCI for a general population as Medicare beneficiaries account for only 49% of all PCIs.8 Moreover, the association between 30-day readmission after PCI and 1-year mortality is not known. The Mayo Clinic PCI registry prospectively collects demographic, clinical, and procedural variables, as well as follow-up outcomes including readmission and mortality for all patients undergoing PCI. Accordingly, we sought to identify factors associated with 30-day readmission rates, the reason for the readmission, and the association of 30-day readmission with 1-year mortality for patients after PCI.
Methods
All patients undergoing PCI at Saint Marys Hospital in Rochester, Minnesota are followed in a prospective registry. Data elements include demographic, clinical, angiographic, procedural, and follow-up variables. Post procedural and in-hospital events are recorded and each patient is contacted by telephone using a standardized questionnaire at six months, one year, and then annually by trained personnel to document long-term outcomes. During the six month follow-up contact, details of any readmission during that time period are collected including the date, name of hospital, and if the reason for readmission was cardiovascular or non-cardiovascular. All adverse events are confirmed by reviewing the medical records for patients followed at our institution and by contacting the patients’ physicians and requesting hospital records for patients treated elsewhere.
All patients undergoing PCI (including elective or for an acute coronary syndrome) from January 1998 to June 2008 were included in this analysis. Patients (n=375) were excluded if they declined authorization allowing the use of their medical records for research, as required by State of Minnesota statute and if their health care was paid for by the Federal Bureau of Prisons or by non-US governments (n=499). Additionally, patients who died prior to discharge (n=289) and those without 30-day follow-up (n=425) were excluded. We identified 15,498 PCI hospitalizations (of 12,813 unique patients) which met the inclusion criteria. The study was approved by the Mayo Clinic Institutional Review Board.
Demographic variables including age and sex were collected from the Mayo Clinic PCI registry. Other demographic variables were collected from Mayo Clinic administrative databases and merged with the PCI registry. These variables included: marital status (single, married, divorced, separated, or widowed), education level (8th grade or less, some high school, high school graduate or equivalent, some college, college graduate, post-graduate studies, or unknown), miles traveled to Mayo Clinic, and insurance type (Medicare, Medicaid, uninsured, or privately insured).
Clinical variables included MI type (ST-elevation myocardial infarction (STEMI) or non-ST-elevation myocardial infarction (NSTEMI)), unstable angina, time since most recent MI, multivessel disease, body mass index (BMI) (kg/m2), CHF status, diabetes mellitus, hypertension, hyperlipidemia, moderate/severe renal dysfunction (defined as a creatinine of >3.0 mg/dl or a history of dialysis or renal transplant), history of cerebrovascular accident or transient ischemic attack (CVA/TIA), peripheral vascular disease (PVD), chronic obstructive pulmonary disease (COPD), peptic ulcer disease, tumor/lymphoma/leukemia, metastatic cancer, pre-procedure shock, and left ventricular ejection fraction (LVEF). Procedural characteristics included the urgency of PCI, drug-eluting stent use, intra-aortic balloon pump (IABP) use, procedural success (defined as less than a 20% residual stenosis without in-hospital death, MI, or stroke), in-hospital MI, in-hospital MI/CABG/TVR (target vessel revascularization), and length of stay. All patients who receive PCI at Mayo Clinic receive a baseline troponin level and electrocardiogram prior to PCI and have 3 follow-up troponin levels with an electrocardiogram to detect in-hospital MI. Procedural complications included major bleeding, blood transfusions, and post-PCI renal failure.
The study outcomes were all-cause readmission to any hospital within 30 days of discharge and 1-year mortality following PCI. During the study period, all patients undergoing PCI were hospitalized and no same-day discharges occurred after PCI. Continuous data are summarized as mean ± standard deviation, unless otherwise stated. Categorical data are summarized as frequency and group percentage. Differences between patients who were versus were not readmitted within 30 days were tested with generalized estimating equations to account for the correlation between multiple hospitalizations on the same patients. Logistic regression models were built for 30-day readmission by selecting from the 40 covariates associated with the endpoint at the 0.15 significance level and then choosing the best subset of covariates according to an overall model score test. The covariates in the model included: age (forced covariate), procedure date (per year), female sex, insurance status (Medicare, Medicaid, privately insured, and uninsured), education level (8th grade or less, some high school, high school graduate or equivalent, some college, college graduate, post-graduate studies, or unknown), distance traveled to Mayo Clinic per 100 miles, time since most recent MI (<24 hours, 1–7 days, >7 days, never (reference group)), unstable angina, CHF on presentation, hyperlipidemia, PVD, CVA/TIA, moderate/severe renal disease, COPD, peptic ulcer disease, metastatic cancer, elective PCI, drug eluting stent use, procedural success, extreme blood loss, and length of stay > 3 days. To assess model performance, we calculated the max-rescaled R-squared statistic9, the receiver operating characteristic area under the curve (AUC), and the observed readmission rates in the lowest and highest risk deciles. We also performed a sensitivity analysis at the patient-level that included only the first PCI for each patient (n=12,813), and all subsequent PCIs for the same patient were excluded. The results from the sensitivity analysis are similar to the analysis at the PCI hospitalization level and are not reported separately.
The association between 30-day readmission and 1-year mortality was estimated using hazard ratios from Cox proportional hazards models. Thirty-day readmission was coded as a time-dependent covariate and was considered “absent” until readmission within 30 days after discharge. Additionally, the partial hazard ratio was also estimated in a Cox hazard ratio using a 3 degree of freedom spline function of the linear predictor for 30-day readmission from the previous logistic regression model for risk adjustment. For the Cox regression analysis for mortality, time zero started at the time of discharge and only the first PCI per patient was included. We also performed a landmark analysis for mortality by 30-day readmission status calculated with Kaplan-Meier methods which included only patients after first PCI who survived to 30 days after hospital discharge. Time zero for the Kaplan Meier landmark analysis plot was 30-days after hospital discharge to discriminate between those who were and were not readmitted within 30 days.
Results
This study included 15,498 PCI procedures, which met the inclusion criteria, at Saint Marys Hospital, Rochester, Minnesota between January 1998 and June 2008. Overall, 1,459 (9.4%) PCI procedures were readmitted within 30 days. There were 106 (0.68%) deaths within 30 days including 33 deaths that occurred during or after a readmission and 73 deaths that were not associated with a readmission.
Factors Associated with 30-day Readmission
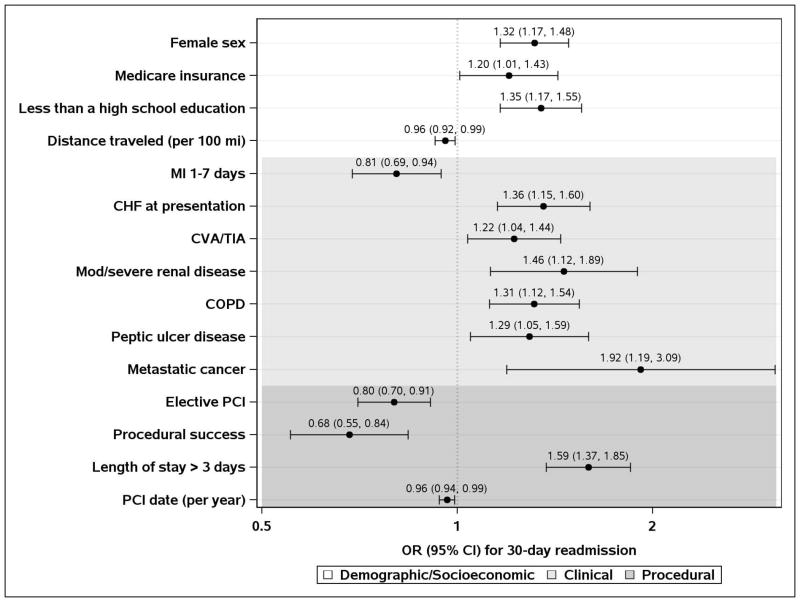
Demographic characteristics are shown in Table 1 and clinical and procedural characteristics are shown in Table 2. After multivariable analysis (Figure 1), demographic factors associated with an increased risk of 30-day readmission after PCI included: Female sex (OR=1.32; 95% CI: 1.17–1.48), Medicare insurance (OR=1.20; 95% CI: 1.01–1.43; reference group was all other insurance types), and less than a high school education (OR=1.35; 95% CI: 1.17–1.55; reference group was high school graduate or higher education levels). The clinical and procedural factors associated with an increased risk of readmission included: CHF at presentation (OR 1.36; 95% CI: 1.15–1.60), CVA/TIA (OR=1.22; 95% CI: 1.04–1.44), moderate/severe renal disease (OR=1.46; 95% CI: 1.12–1.89), COPD (OR=1.31; 95% CI: 1.12–1.54), peptic ulcer disease (OR=1.29; 95% CI: 1.05–1.59), metastatic cancer (OR=1.92; 95% CI: 1.19–3.09), and a length of stay >3 days (OR=1.59; 95% CI: 1.37–1.84). The general R-squared statistic for the model for 30-day readmission was 0.052, the AUC was 0.65 (Figure 2), and the observed readmission rates ranged from 3.2% in the lowest predicted decile to 19.7% in the highest decile.
Table 1.
Demographic Characteristics
| Variable | No 30-Day Readmission (N=14039) | 30-Day Readmission (N=1459) | P-value |
|---|---|---|---|
| Age, years | 66.8 ± 12.0 | 68.9 ± 12.1 | <0.001 |
| Female Sex, No. (%) | 4070 (29%) | 540 (37%) | <0.001 |
| Marital Status, No. (%) | <0.001 | ||
| Single | 848 (6%) | 70 (5%) | |
| Married | 10737 (78%) | 1066 (74%) | |
| Divorced | 847 (6%) | 103 (7%) | |
| Separated | 27 (0%) | 0 (0%) | |
| Widowed | 1381 (10%) | 204 (14%) | |
| Education Level, No. (%) | <0.001 | ||
| 8th Grade or Less | 1094 (8%) | 175 (12%) | |
| Some High School | 1023 (7%) | 143 (10%) | |
| High School Graduate or GED | 4768 (34%) | 467 (32%) | |
| Some College | 2438 (17%) | 261 (18%) | |
| College Graduate | 1088 (8%) | 83 (6%) | |
| Post-Graduate Studies | 1396 (10%) | 116 (8%) | |
| Unknown | 2232 (16%) | 214 (15%) | |
| Insurance Category, No. (%) | <0.001 | ||
| Medicaid | 436 (3%) | 51 (3%) | |
| Medicare | 7947 (57%) | 967 (66%) | |
| Privately Insured | 5497 (39%) | 424 (29%) | |
| Uninsured | 159 (1%) | 17 (1%) | |
| Miles Traveled to Mayo Clinic, Median (Q1, Q3) | 51.8 (30.8, 109.9) | 40.8 (16.4, 86.4) | 0.003 |
Table 2.
Clinical and Procedural Characteristics
| Variable | No 30-Day Readmission (N=14039) | 30-Day Readmission (N=1459) | P-value |
|---|---|---|---|
| Clinical Characteristics | |||
| Unstable Angina, No. (%) | 8014 (57%) | 864 (59%) | 0.19 |
| MI Type (STEMI/NSTEMI), No. (%) | 0.003 | ||
| No MI | 9465 (67%) | 918 (63%) | |
| STEMI | 2399 (17%) | 276 (19%) | |
| NSTEMI | 2175 (15%) | 265 (18%) | |
| Most recent MI, No. (%) | <0.001 | ||
| <24 hours | 2498 (18%) | 330 (23%) | |
| 1–7 days | 2076 (15%) | 211 (15%) | |
| >7 days | 3322 (24%) | 344 (24%) | |
| Never | 5918 (43%) | 556 (39%) | |
| Multivessel Disease, No. (%) | 8966 (68%) | 970 (70%) | 0.082 |
| Body Mass Index (BMI) (kg/m2) | 29.7 ± 5.7 | 29.4 ± 6.1 | 0.033 |
| CHF at presentation, No. (%) | 1427 (11%) | 254 (18%) | <0.001 |
| Diabetes, No. (%) | 3555 (25%) | 390 (27%) | 0.23 |
| Hyperlipidemia, No. (%) | 10404 (81%) | 1042 (78%) | 0.012 |
| Hypertension, No. (%) | 9864 (73%) | 1084 (77%) | 0.004 |
| Moderate/Severe Renal Disease, No. (%) | 447 (3%) | 88 (6%) | <0.001 |
| CVA/TIA, No. (%) | 1573 (11%) | 237 (17%) | <0.001 |
| Peripheral Vascular Disease, No. (%) | 1451 (11%) | 210 (15%) | <0.001 |
| COPD, No. (%) | 1489 (11%) | 237 (17%) | <0.001 |
| Peptic Ulcer Disease, No. (%) | 814 (6%) | 129 (9%) | <0.001 |
| Tumor/Lymphoma/Leukemia, No. (%) | 1687 (12%) | 220 (15%) | <0.001 |
| Metastatic Cancer, No. (%) | 107 (1%) | 27 (2%) | <0.001 |
| Pre-procedural shock, No. (%) | 379 (3%) | 77 (5%) | <0.001 |
| LVEF measure, No. (%) | <0.001 | ||
| >40% | 6511 (46%) | 586 (40%) | |
| NA | 6131 (44%) | 684 (47%) | |
| <=40% | 1397 (10%) | 189 (13%) | |
| Procedural Characteristics | |||
| Urgency of PCI, No. (%) | <0.001 | ||
| Elective | 4887 (35%) | 390 (27%) | |
| Urgent | 6581 (47%) | 714 (49%) | |
| Emergency | 2567 (18%) | 355 (24%) | |
| Drug-Eluting Stents, No. (%) | 5104 (36%) | 426 (29%) | <0.001 |
| IABP Use, No. (%) | 218 (2%) | 41 (3%) | <0.001 |
| Procedural success, No. (%) | 13285 (95%) | 1327 (91%) | <0.001 |
| In-Hospital MI, No. (%) | 562 (4%) | 86 (6%) | <0.001 |
| In-Hospital MI/CABG/TVR, No. (%) | 694 (5%) | 113 (8%) | <0.001 |
| Blood Transfusion, No. (%) | 597 (4%) | 126 (9%) | <0.001 |
| GI Bleed, No. (%) | 108 (1%) | 24 (2%) | <0.001 |
| Renal Failure Post-PCI, No. (%) | 98 (1%) | 26 (2%) | <0.001 |
| Length of Stay (Days), Median (Q1, Q3) | 1.0 (1.0, 3.0) | 2.0 (1.0, 4.0) | 0.004 |
MI – Myocardial Infarction, STEMI-ST Elevation Myocardial Infarction, NSTEMI- Non-ST Elevation Myocardial Infarction, CHF – Congestive Heart Failure, CVA/TIA – Cerebrovascular Accident / Transient Ischemic Attack, COPD – Chronic Obstructive Pulmonary Disease, LVEF – Left Ventricular Ejection Fraction, PCI – Percutaneous Coronary Intervention, IABP – Intra-Aortic Balloon Pump, CABG – Coronary Artery Bypass Graft, TVR – Target Vessel Revascularization
Figure 1.
Factors Associated with 30-Day Readmission after Multivariable Analysis
Figure 2.
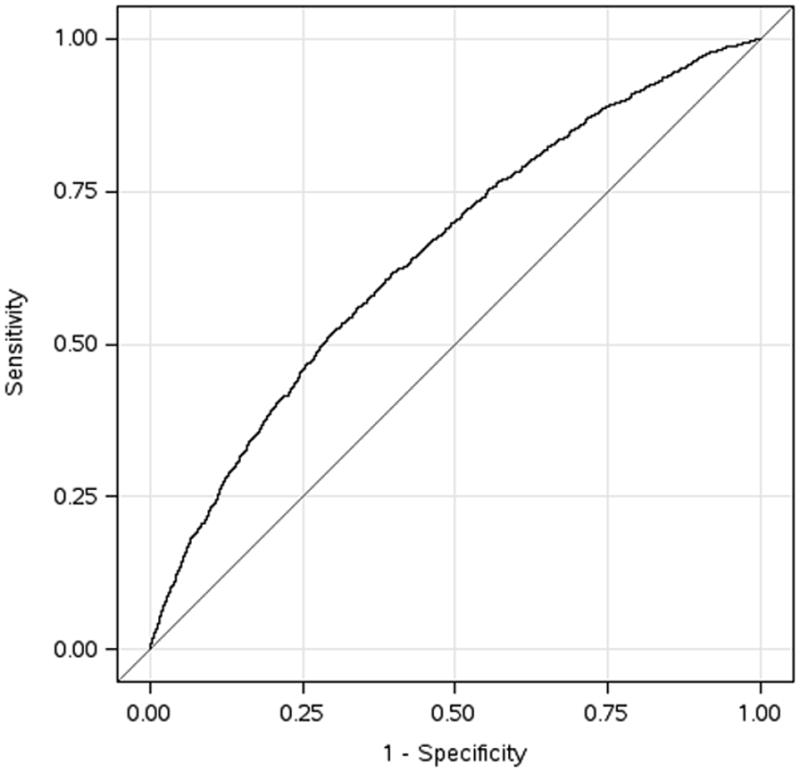
Receiver Operating Characteristic Curve for Model Discrimination
Readmission Diagnoses
Of the 1,459 PCIs readmitted within 30 days, 1,003 (69%) were readmitted for cardiac-related reasons. Only 4.2% (n=61) had repeat PCI within 30-days of discharge and 8.9% (n=130) had PCI or CABG within 30 days of discharge.
Readmission and Subsequent Mortality
In unadjusted analysis, 30-day readmission after PCI was associated with a higher risk of 1-year mortality (HR=1.99; 95% CI: 1.57–2.52; p<0.001). After adjustment using the Cox proportional hazards model for factors associated with 30-day readmission, 30-day readmission remained associated with a higher risk of 1-year mortality (HR=1.38; 95% CI: 1.08–1.75; p=0.009).
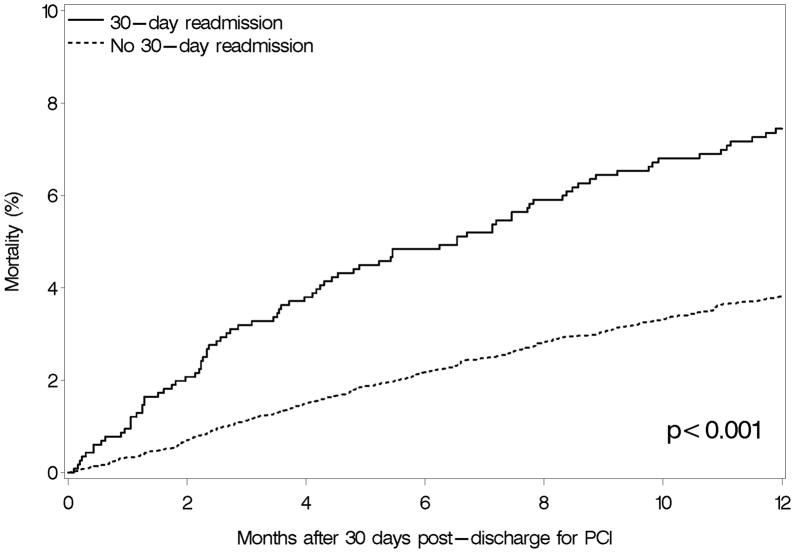
Figure 3 shows the Kaplan-Meier landmark analysis plot for mortality rates by 30-day readmission status. This landmark analysis included only patients who survived to 30 days after discharge. Patients who were readmitted within 30 days had higher mortality at one year compared with patients who were not readmitted (p<0.001).
Figure 3.
Kaplan-Meier Landmark Analysis of Mortality after Readmission
Comment
Preventable readmissions have become a focus of national quality improvement efforts. The current focus is on readmissions for patients hospitalized with AMI and HF, although it has been recently extended to PCI.3 Among 15,498 PCI hospitalizations from 1998–2008 including Medicare and other payer types, we found that almost 1 in 10 patients are readmitted within 30-days after PCI and the majority (69%) of readmissions were related to a cardiac reason. Further, 30-day readmission was associated with an increased risk of 1-year mortality.
Thirty-day risk-standardized readmission rates after PCI have become a publicly reported performance measure and there is high interest from hospitals and clinicians to understand and improve modifiable factors associated with 30-day readmission rates. We identified several factors associated with a higher risk for 30-day readmission after PCI using a prospective, clinical database that included patients with Medicare and non-Medicare insurance; however, most of the variables are not readily modifiable, such as female sex, Medicare insurance, less than a high school education, CHF at presentation, and moderate renal disease. Even though these variables are not modifiable, interventions to improve access and follow-up care should be studied to assess impact on readmission rates.
Our model had modest ability to discriminate the risk for 30-day readmission with a general R-squared statistic of 0.052, an AUC of 0.65, and the observed readmission rates ranged from 3.2% in the lowest predicted decile to 19.7% in the highest decile. The discriminatory ability (both R-squared and AUC) of our model is comparable to previously published models for the risk of readmissions for patients with AMI and CHF.10,11 The discriminatory ability of our model would likely be improved by additional variables that were not available such as patient literacy, frailty, access to care, and socioeconomic status. Further, since all patients in this study received PCI at a single healthcare system, we did not have the capability to compare system-level factors associated with 30-day readmissions.
Prior to this study, knowledge of readmission rates after PCI was limited to administrative data from Medicare patients.7 Our study extended these findings as we found that thirty-day readmission rates after PCI were high across all insurance types and ranged from 7.2% in the privately insured group to 10.8% in the Medicare group. Among insurance categories, Medicare patients experienced the highest readmission rate. Gaps in transitions in care from the inpatient to the outpatient context may account for many of the observed readmissions, especially amongst non-privately insured patients (Medicare, Medicaid, and uninsured patients) who may experience difficulty in accessing outpatient care.12,13
Lack of early follow-up has been associated with increased risk of readmission among patients with heart failure14 and may also be playing a role in PCI patients. Early follow-up allows patients and clinicians to ensure understanding, compliance, and gauge the effectiveness of therapies. The educational component of follow-up cannot be underestimated because in one study, less than half of patients were able to list their diagnoses and the names, purpose, and side effects of their medications at the time of discharge.15 Education at the time of discharge and early follow-up also needs to be tailored to patient education level, which has previously been shown to be associated with the risk of readmission among Medicare beneficiaries.16 In our study, patients with less than a high school education were more likely to be readmitted after PCI than those with high school or higher education.
There are several limitations to this study. This is a prospective registry that collected demographic, clinical, procedural, and outcomes variables and merged with socioeconomic variables from an administrative database and hence, cannot demonstrate if any of the observed associations are causal in nature. Although multivariable modeling was performed, residual unmeasured confounders may exist. We have no data regarding outpatient clinic follow-up, medication compliance, health literacy, frailty, or other barriers to health care access.
In summary, about 1 in 10 PCI procedures resulted in a readmission within 30 days and the majority of readmissions were due to a cardiovascular cause. Patients who were readmitted within 30 days of discharge were at an increased risk of 1-year mortality compared with those who were not readmitted.
Acknowledgments
Funding:
This study was funded by the Division of Cardiovascular Diseases, Mayo Clinic, Rochester, Minnesota.
Footnotes
Authors List of Contributions:
Khawaja, Shah, Lennon, Slusser, Alkatib, Rihal, Gersh, Montori, Holmes, Bell, Curtis, Krumholz, Ting – 1, 2, 3 for All Authors
Data Access and Responsibility:
Khawaja, Lennon, Slusser, and Ting had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Conflicts of Interest:
Khawaja, Shah, Lennon, Slusser, Alkatib, Rihal, Gersh, Montori, Holmes, Bell, Curtis, Krumholz, Ting–none
References
- 1.Krumholz HM, Normand SL, Spertus JA, Shahian DM, Bradley EH. Measuring performance for treating heart attacks and heart failure: the case for outcomes measurement. Health Aff (Millwood) 2007;26(1):75–85. doi: 10.1377/hlthaff.26.1.75. [DOI] [PubMed] [Google Scholar]
- 2.Krumholz HM, Normand SL. Public reporting of 30-day mortality for patients hospitalized with acute myocardial infarction and heart failure. Circulation. 2008;118(13):1394–1397. doi: 10.1161/CIRCULATIONAHA.108.804880. [DOI] [PubMed] [Google Scholar]
- 3.Kereiakes DJ. Return to sender hospital readmission after percutaneous coronary intervention. J Am Coll Cardiol. 2009;54(10):908–910. doi: 10.1016/j.jacc.2009.05.037. [DOI] [PubMed] [Google Scholar]
- 4.Patient Protection and Affordable Care Act of 2010. Pub L. No. 111–148; 124 STAT. 119 (2010).
- 5.Epstein AM. Paying for performance in the United States and abroad. N Engl J Med. 2006;355(4):406–408. doi: 10.1056/NEJMe068131. [DOI] [PubMed] [Google Scholar]
- 6.Straube B, Blum JD. The policy on paying for treating hospital-acquired conditions: CMS officials respond. Health Aff (Millwood) 2009;28(5):1494–1497. doi: 10.1377/hlthaff.28.5.1494. [DOI] [PubMed] [Google Scholar]
- 7.Curtis JP, Schreiner G, Wang Y, et al. All-cause readmission and repeat revascularization after percutaneous coronary intervention in a cohort of medicare patients. J Am Coll Cardiol. 2009;54(10):903–907. doi: 10.1016/j.jacc.2009.04.076. [DOI] [PubMed] [Google Scholar]
- 8.Epstein AJ, Rathore SS, Krumholz HM, Volpp KG. Volume-based referral for cardiovascular procedures in the United States: a cross-sectional regression analysis. BMC health services research. 2005;5:42. doi: 10.1186/1472-6963-5-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nagelkerke NJD. A Note on a General Definition of the Coefficient of Determination. Biometrika. 1991;78:691–692. [Google Scholar]
- 10.Krumholz HM, Lin Z, Drye EE, et al. An administrative claims measure suitable for profiling hospital performance based on 30-day all-cause readmission rates among patients with acute myocardial infarction. Circ Cardiovasc Qual Outcomes. 2011;4:243–252. doi: 10.1161/CIRCOUTCOMES.110.957498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Keenan PS, Normand SLT, Lin Z, et al. An administrative claims measure suitable for profiling hospital performance on the basis of 30-day all-cause readmission rates among patients with heart failure. Circ Cardiovasc Qual Outcomes. 2008;1:29–37. doi: 10.1161/CIRCOUTCOMES.108.802686. [DOI] [PubMed] [Google Scholar]
- 12.Chou WC, Cooney LM, Jr, Van Ness PH, Allore HG, Gill TM. Access to primary care for Medicare beneficiaries. J Am Geriatr Soc. 2007;55(5):763–768. doi: 10.1111/j.1532-5415.2007.01154.x. [DOI] [PubMed] [Google Scholar]
- 13.Asplin BR, Rhodes KV, Levy H, et al. Insurance status and access to urgent ambulatory care follow-up appointments. JAMA. 2005;294(10):1248–1254. doi: 10.1001/jama.294.10.1248. [DOI] [PubMed] [Google Scholar]
- 14.Hernandez AF, Greiner MA, Fonarow GC, et al. Relationship between early physician follow-up and 30-day readmission among Medicare beneficiaries hospitalized for heart failure. JAMA. 2010;303(17):1716–1722. doi: 10.1001/jama.2010.533. [DOI] [PubMed] [Google Scholar]
- 15.Makaryus AN, Friedman EA. Patients’ understanding of their treatment plans and diagnosis at discharge. Mayo Clin Proc. 2005;80(8):991–994. doi: 10.4065/80.8.991. [DOI] [PubMed] [Google Scholar]
- 16.Arbaje AI, Wolff JL, Yu Q, Powe NR, Anderson GF, Boult C. Postdischarge environmental and socioeconomic factors and the likelihood of early hospital readmission among community-dwelling Medicare beneficiaries. Gerontologist. 2008;48(4):495–504. doi: 10.1093/geront/48.4.495. [DOI] [PubMed] [Google Scholar]