In order to promote a successful recovery after a hospitalization, health care professionals often focus their efforts on issues related to the acute illness that precipitated the hospitalization. Their disproportionate attention on the reason for the hospitalization, however, may be misdirected. Patients who were recently hospitalized are not only recovering from their acute illness, but they also experience a transient period of generalized risk for a wide range of adverse health events. Thus, their condition may be better characterized as a post-hospital syndrome, an acquired condition of vulnerability. This theory of illness would suggest that the risks in the critical 30-day period after discharge might derive as much, or more, from the allostatic stress that patients experience in the hospital as they do from the lingering effects of the acute illness that precipitated the hospitalization. At the time of discharge, the physiological systems are impaired, physiological reserves are depleted, and the body cannot effectively avoid or mitigate health threats.
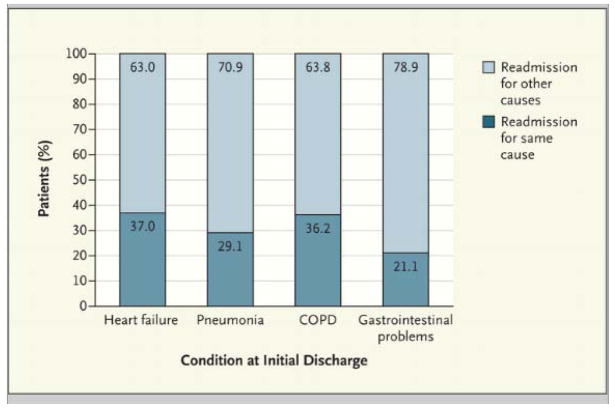
Nearly one fifth of Medicare patients discharged from a hospital — approximately 2.6 million seniors — develop an acute medical problem within the subsequent 30 days that necessitates another hospitalization. These recently discharged patients have heightened risk for a myriad of conditions, many of which appear to have little in common with the initial diagnosis. For example, among patients admitted for treatment of heart failure, pneumonia, or chronic obstructive pulmonary disease (COPD), the cause of readmission is the same as that of the index admission for only 37%, 29%, and 36%, respectively.1 The causes of readmission, regardless of the original admitting diagnosis, commonly include heart failure, pneumonia, COPD, infection, gastrointestinal conditions, mental illness, metabolic derangements, and trauma. Further evidence of the distinctiveness of this syndrome is that information about the severity of the acute illness that led to the hospitalization predicts poorly who will experience an adverse medical event soon after discharge.
How might the post-hospital syndrome emerge? Hospitalized patients are not only enduring an acute illness, which can markedly perturb physiological systems, but are experiencing substantial stress. During hospitalization, patients are commonly deprived of sleep, experience disruption of normal circadian rhythms, are nourished poorly, have pain and other discomfort, confront a baffling array of mentally challenging situations, receive medications that can alter cognition and physical function, and become deconditioned by bed rest or inactivity. Each of these perturbations can adversely affect health and contribute to substantial impairments during the early recovery period, an inability to fend off disease, and susceptibility to mental error.
Scientific studies have already documented the prevalence and risk of these stressors. For example, hospitalized patients often experience disturbance of sleep. Studies have documented polysomnographic abnormalities in hospitalized patients, including reductions in sleep time and stages R (rapid eye movement [REM]) and N3 (slow wave) and an increase in stage N1 (non-REM). This disruption can have debilitating behavioral and physiological effects. In particular, sleep deprivation adversely affects metabolism, cognitive performance, physical functioning and coordination, immune function, coagulation cascade, and cardiac risk. In addition, sleep-wake–cycle disruptions may cause perturbations in circadian rhythms, and may have adverse effects even independently of the sleep deprivation and abnormalities. These sleep-wake–cycle disturbances in hospitalized patients may confer jet-lag–type disabilities. Studies of people with jet lag have revealed increased incidence of dysphoric mood, diminished physical performance, cognitive impairment, and gastrointestinal disturbances.
Nutritional issues during hospitalizations may cause problems, yet often receive limited attention. In one study, one fifth of hospitalized patients 65 years and older had an average nutrient intake of less than 50% of their calculated maintenance energy requirements. Patients are commonly ordered to have nothing by mouth for specified periods, during which they are not fed by alternate means. Cancellations and rescheduling of procedures or tests can extend these periods. For patients receiving mechanical ventilation or who cannot take food by mouth, there are often delays in addressing nutritional needs. These deficits, rarely addressed at discharge, can lead to protein-energy malnutrition. Friedmann et al. have shown loss of weight and decreased albumin blood levels after discharge to be strong predictors of readmission within 30 days.3 Meanwhile, malnutrition can affect every system in the body, resulting in impairment of wound healing, increased risk of infections and pressure ulcers, decreased respiratory and cardiac function, poorer outcomes of chronic lung diseases, cardiovascular and gastrointestinal disorders, and poorer physical function.
On the cognitive front, hospitalized patients often meet a variety of health care professionals but have little time to learn their names or understand their roles. Schedules are often unpredictable, and in patients who are already under stress, information overload may provoke confusion. Moreover, the stress of the hospitalization can cause delirium, which occurs commonly among patients hospitalized for acute medical conditions. Delirium may affect subsequent cognitive function, which may lead to decline in activities of daily living and reduced motor function.
Pain and other discomforts, common among these patients, are often inadequately addressed. They can lead to sleep disorders, mood disturbances, and impaired cognitive functioning, and are also known to influence immune and metabolic function. Moreover, medications to treat symptoms can negatively affect the early recovery period. Sedatives, especially benzodiazepines, are commonly prescribed and may become part of the discharge regimen. Under-sedation can cause hypercatabolism, immunosupression, hypercoagulability, and increased sympathetic activity. Over-sedation can dull the senses and impair cognitive function and judgment, and may also lead to post-traumatic stress disorder.
Finally, hospitalized patients commonly become deconditioned. Thus, recently discharged patients often have impaired stamina, coordination, and strength, which place them at greater risk for accidents and falls. In addition, these limitations may diminish their ability to comply with post-discharge instructions such as daily use of a scale to weigh themselves. The capacity to resume basic activities or be able to attend a follow-up appointment can be affected.
Recognition of the post-hospital syndrome can provide the impetus to develop novel interventions to promote successful recovery. Although we need to continue to improve transitional care and ensure that the condition for which a patient was initially admitted is successfully treated, we also need to focus on the factors during the hospitalization and the early recovery period that are contributing to the transient period of vulnerability.
What can be done now? At a minimum, we should inventory the patient’s condition at discharge by soliciting details far beyond that related to the condition that led to hospitalization. As we assess readiness for transition from the inpatient setting, we need to be aware of functional disabilities, with attention to cognitive and physical function, and align care appropriately. The transition plan should incorporate this information into efforts to promote a safe, successful recovery. We should also employ risk mitigation strategies that stretch beyond the initial cause for the hospitalization and include infections, metabolic disorders, falls, trauma and the gamut of events that commonly occur in this period of generalized risk.
Comprehensive strategies for mitigating post-hospital syndrome and its accompanying risks might begin with efforts to target the stressors that may contribute to this period of vulnerability in patients soon after discharge. We should more assertively apply interventions aimed at reducing disruptions in sleep, minimizing pain and stress, promoting good nutrition and addressing nutritional deficiencies, optimizing the use of sedatives, promoting practices that reduce the risk of delirium and confusion, emphasizing physical activity and strength maintenance or improvement, and enhancing cognitive and physical function. The hospitalization should not only address the urgencies of the acute illness, but also seek to promote health actively by strengthening patients and contributing to their physiological reserve. Attention to sleep, nutrition, activity, strength, and judicious symptom management can pay great dividends. Many interventions may be akin to those developed to reduce delirium. Shorter lengths of stay put an even greater premium on preparing patients for a successful convalescence period from the first day. At the least, we should test this theory.
If this construct is valid, we will need to reorient our efforts to reduce readmissions during this high-risk period, exploring new approaches to making hospitalization less toxic and promoting safe passage from acute care settings.
Figure 1.
Footnotes
Disclosure forms provided by the author are available with the full text of this article at NEJM.org.
References
- 1.Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. N Engl J Med. 2009;360:1418–28. doi: 10.1056/NEJMsa0803563. [DOI] [PubMed] [Google Scholar]
- 2.Kansagara D, Englander H, Salanitro A, et al. Risk prediction models for hospital readmission: a systematic review. JAMA. 2011;306:1688–98. doi: 10.1001/jama.2011.1515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Friedmann JM, Jensen GL, Smiciklas-Wright H, McCamish MA. Predicting early nonelective hospital readmission in nutritionally compromised older adults. Am J Clin Nutr. 1997;65:1714–20. doi: 10.1093/ajcn/65.6.1714. [DOI] [PubMed] [Google Scholar]