Abstract
Background
A rapid scaling-up of HIV interventions in India is anticipated, but systematic information on how costs of HIV interventions change over time and programme scale is not available for informed planning.
Methods
We studied the changes in unit costs of two major interventions, voluntary counseling and testing (VCT) and sex worker programmes in the south Indian state of Andhra Pradesh between 2002-2003 and 2005-2006 fiscal years. Economic costs (from the provider perspective) and output data from 17 publicly funded VCT centers and 14 sex worker programmes were collected using standardized methods. We calculated unit costs for each programme in each period and explored possible reasons for the changes seen.
Results
In 2005-2006, the VCT centers served 66,445 clients and the sex worker programmes served 32,550. The unit cost of providing VCTC services dropped over 3 years by half to Indian Rupees (INR) 147.5 (US$ 3.33) mainly because the number of clients doubled. There was no decrease in the average time spent counseling each client. The unit cost of providing HIV prevention services to sex workers increased 2.41 times over 3 years to INR 1,401 (US$31.6) as a result of increases in male condom distribution, staff salaries and training expense, and treatment for sexually transmitted infections, all suggestive of improved services.
Conclusions
The unit cost of these two interventions changed dramatically over a 3-year period, but in opposite directions. The current unit cost for VCT in Andhra Pradesh is much lower than the estimated global average for low-income settings. These local longitudinal cost data are useful to inform the currently planned scaling up of HIV interventions in India.
Keywords: cost analysis, HIV, India, prevention, sex worker, voluntary counseling and testing
Introduction
It is now widely recognized that, for global control of the HIV epidemic, insufficient attention has been focused on the costs of scaling up HIV prevention interventions, despite a sixfold increase in HIV financing in low and middle-income countries between 2001 and 2006 [1].
Prevention activities are expected to increase substantially in the new 2007 – 2012 phase of India’s National AIDS Control Programme [2], but data on the changes in unit costs of HIV prevention interventions with scaling up are not readily available to inform planning, including how the efficiency of services could be improved. Recent estimates of HIV prevention costs and their impact at the global and regional levels [3,4] are very valuable for macroplanning, but are based on a range of estimates that often vary considerably even within the same region of the world. Local data are therefore necessary for decisions on resource allocation and budget planning for interventions at country and subcountry levels. Ideally, these data should include unit costs of HIV interventions, determinants of these costs, relation of unit costs with quality, change in unit costs with increasing scale, and cost-effectiveness/cost-benefit of interventions. We have previously reported data on the first of these three issues for some major HIV prevention interventions in the south Indian state of Andhra Pradesh [5 - 7]. Although other data from India on the economic aspects of prevention interventions are scarce, two recent studies have provided useful information specifically about the cost-effectiveness of sex worker interventions in India [8,9]. In this paper we analyse the change in unit costs of providing HIV prevention services to sex workers and voluntary counseling and testing (VCT) in Andhra Pradesh between the 2002 – 2003 and 2005 – 2006 fiscal years and explore possible reasons for the changes seen.
Methods
We quantified economic costs of providing VCT and sex worker interventions in Andhra Pradesh state, which has a population of 80 million and is estimated to have the highest burden of HIV among Indian states [10]. Costs were total programme costs from the provider perspective. Seventeen publicly funded VCT centers at public hospitals were randomly selected from the 26 operating in this state in 2003, all located at large public hospitals [5]. Sex worker intervention costs were collected from all of the 15 publicly funded sex worker programmes run by non-governmental organizations in the state in 2003 [6].
Data collection
Economic cost and output data were initially collected for the 2002 – 2003 fiscal year for each programme as part of the multicountry Prevent AIDS Network for Cost-Effectiveness Analysis (PANCEA) study [5,6,11,12]. Data were collected through interviews with programme staff and a review of written records after obtaining formal consent for the study from senior programme managers. Standard data collection instruments prepared for the multicountry PANCEA study were used after review and refinement for the Andhra Pradesh context through pre-pilot and pilot studies. Using the same methods, data were later collected for the 2005 – 2006 fiscal year at the same VCT centers and sex worker programmes.
Cost data
Costs were grouped into five categories: personnel; recurrent goods; recurrent services; capital goods; and building rentals [5,6]. Personnel cost was computed using economic payroll costs (salary and fringe benefits) for the relevant time that each staff member committed to the programme. The value of cash or in-kind stipend payments to peer educators in the sex worker programme was also included.
Recurrent goods used at the VCT centers included HIV test kits, male condoms, information, 6 education and communication (IEC) materials, medical supplies and stationery. Goods were valued at market prices. Prices were obtained when possible from the financial records of each programme or else by taking the average of three quotations requested for the relevant financial year. Several recurrent goods were not directly purchased by the VCT center. For example, the HIV test kits, male condoms, and IEC materials were donated to the centers by the Andhra Pradesh State AIDS Control Society. Test kits, bulk purchased, were valued at the manufacturer’s bulk purchase price for the fiscal year. Condom prices were adjusted to exclude the existing 70% government subsidy. Costs for the IEC materials were obtained from the Andhra Pradesh State AIDS Control Society. Similar recurrent goods were costed at each sex worker programme, including medication for the treatment of sexually transmitted infections.
Recurrent services included staff training (including repeat training), local travel, special events, cleaning, building maintenance and utilities. The cost for staff training was calculated including all inputs such as travel, per diem, trainer fees, training materials and training facility. The cost of building maintenance was calculated on the basis of the space occupied by the VCT center. Electricity and water costs were based on market rates applied to the estimated usage. Telephone and other recurrent services costs were based on actual usage.
Capital goods at VCT centers included furniture and both medical and administrative equipment. Items were valued at the price from the financial records of the programme or, when unavailable, obtained from retail sellers. The life of the capital goods was assumed to be 5 years, and one-fifth of the cost was allocated to each fiscal year if the good was used for the full year, or calculated proportionately if used only a part of the year. For the joint use of capital items with other programmes, cost was determined on proportional use estimated by programme staff. We calculated the cost of building space at rent paid (for sex work programmes) or, when no rent was paid (VCT programmes housed in public hospitals), by obtaining area-specific rental rates for the relevant fiscal year for the amount of space occupied by the VCT center.
The percentage change in cost between the 2002 – 2003 and 2005 – 2006 fiscal years was calculated for Indian Rupee (INR) costs only, as the exchange rate with the US dollar changed from INR 48.40 to INR 44.27 during this period [13]. The 4 – 5% annual inflation rate in India during the 3-year study period would have increased costs by 14% from 2002 – 2003 to 2005 – 2006 [14]. Accordingly, the 2002 – 2003 costs were adjusted upwards by 14% for comparison with the 2005 – 2006 costs to assess the real change in costs.
Outputs data
The VCT written records provided monthly data on the number, format and duration of pre and post-test counseling sessions, the number of HIV tests conducted and the number of HIV-positive tests [5]. We also recorded client characteristics, referral sources, types of HIV tests administered, fees and time taken to give test results.
The Andhra Pradesh State AIDS Control Society categorizes sex worker intervention services into four components: behaviour change communication; sexually transmitted infections care; condom promotion; and creation of an enabling environment. Monthly data were obtained from sex worker programme records detailing the provision of each of these services per month [6].
Data analysis
We used economic cost per client receiving post-HIV test counseling as the unit cost for VCT programmes and as the unit cost for sex worker programmes, cost per sex worker reached with HIV prevention services (all sex worker programmes studied provide all four components mentioned above) [5,6]. We assessed the change in unit costs between 2002 – 2003 and 2005 – 2006 and analysed the correlates/reasons for the change, including the scale of services and the cost breakdown over various components. The HIV-positive rate at VCT centers was used as an indicator of clients’ risk profile. Changes in indicators of quality were also assessed to understand 8 their relationship to the change in unit cost of services. For VCT, quality indicators included the number of full-time equivalent counselors and the average time that they spent with each client. For sex worker programmes, quality indicators included the quantity of male condoms distributed, the number of sexually transmitted infections treated, and annual expenditure on staff training and development.
We calculated the difference in unit cost between 2002 – 2003 and 2005 – 2006 and related this to the base 2002 – 2003 cost (independent variable). We assessed the relation between the unit cost and scale of the programme (independent variable) in 2005 – 2006. These relations were assessed using the bivariate regression types available in Microsoft Excel (exponential, linear, logar ithmic, polynomial and power) and the relations with the highest R2 value are presented. SPSS and Microsoft Excel were used for statistical analysis.
Results
Change in unit cost at voluntary counseling and testing centers
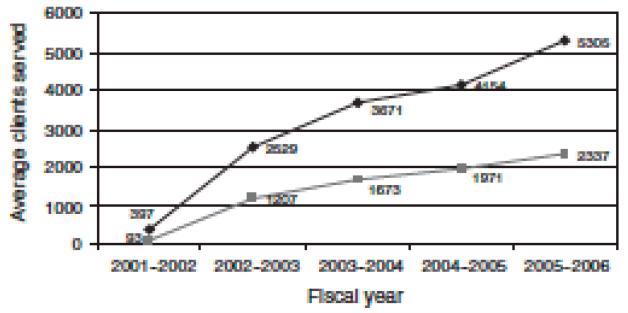
The cost breakdown in each period and changes over time by cost item are shown in Table 1. The average unit cost of providing VCT to each client in 2005 – 2006 was INR 147.5 (US$3.33), 51% less than the average unit cost in 2002 – 2003 adjusted for inflation. Nearly 18% of the total unit cost drop observed over 3 years can be explained by lower HIV test kit costs, which decreased on average by 38.7% after adjusting for inflation. The only other substantial change in the cost categories was for personnel, which, after adjusting for inflation, dropped by 12.2% because some unusually highly paid employees in 2002 – 2003 were no longer on the staff 3 years later. This accounted for another 6.3% of the total decrease in unit cost. Unit cost decline was largely driven by the increase in the number of clients served across the 17 VCT centers (Fig. 1). In 2005 – 2006, 66 445 clients completed post-HIV test counseling at these VCT centers, an increase of 105% from the 32 413 clients served in 2002 – 2003. The average number of clients increased for the nine 9 VCT centers in medical college hospitals (the largest public sector hospitals) by 110% (their number of clients in 2005 – 2006 ranging from 2898 to 7453), and in the eight centers in district headquarters hospitals (the next level of public sector hospitals) by 94% (range of clients in 2005 – 2006: 1706 – 4933).
Table 1.
Changes in unit cost of providing voluntary counseling and testing services from 2002 – 2003 to 2005 – 2006 at 17 voluntary counseling and testing centers in Andhra Pradesh.
| Cost item | Unit cost in 2002 – 2003 in INR [US$]a (range in US$) |
% Total unit cost |
Unit cost in 2005 – 2006 in INR [US$]b (range in US$) |
% Total unit cost |
% Change in unit costc (range) |
|---|---|---|---|---|---|
| Personnel | 141.9 [2.93] (1.21 – 11.87) | 53.7 | 69.3 [1.57] (0.78 – 3.10) | 47.0 | −57 (−89 to +83) |
| Recurrent goods | 79.2 [1.64] (1.03 – 2.46) | 30.0 | 54.0 [1.22] (0.83 – 1.96) | 36.6 | −40 (−71 to −18) |
| Recurrent services | 10.2 [0.21] (0.09 – 0.99) | 3.9 | 6.6 [0.15] (0.06 – 0.82) | 4.5 | −44 (−89 to +18) |
| Capital goods | 4.5 [0.09] (0.05 – 0.27) | 1.7 | 2.0 [0.05] (0.02 – 0.14) | 1.4 | −60 (−89 to −27) |
| Building rental | 28.3 [0.58] (0.18 – 1.75) | 10.7 | 15.5 [0.35] (0.17 – 1.01) | 10.5 | −52 (−89 to +73) |
| Total unit cost | 264.1 [5.46] (2.92 – 17.14) | 100 | 147.5 [3.33] (1.86 – 5.15) | 100 | −51 (−83 to +14) |
US$1 ¼ INR 48.40 in 2002 – 2003.
US$1 ¼ INR 44.27 in 2005 – 2006.
Percentage change calculated for change in INR cost after inflating 2002 – 2003 cost by 14%, which was the inflation between 2002 – 2003 and 2005 – 2006, to assess real change.
Fig. 1. Change in average scale over time at voluntary counseling and testing centers located in medical college hospitals and district headquaters hospitals.
 Medical college hospital;
Medical college hospital;  district headquarters hospitals.
district headquarters hospitals.
The HIV rate among the centers’ clients was 20.5% and 26.2% in the 2002 – 2003 and 2005 – 2006 fiscal years, respectively, indicating that the risk profile of clients did not decrease during this period. Average full-time equivalent counselors per VCT center did not change substantially over 3 years, with 1.35 in 2002 – 2003 and 1.47 in 2005 – 2006 at the larger hospital VCT centers, and 0.92 and 0.97 at the district hospitals-based programmes. The average time spent in one-to-one counseling was reported by VCT staff as unchanged over 3 years: 15 min for pre-HIV test; 12 min for post-test HIV-negative clients, and 32 min for post-test HIV-positive clients.
Change in unit cost at sex worker programmes
One sex worker programme closed during the study period. Results are therefore presented across the remaining 14 programmes. Table 2 shows the cost breakdown in each period and changes over time by cost item. The average unit cost of providing services to each sex worker in 2005 – 2006 was INR 1401 (US$31.65), 2.41 times higher than the average unit cost in 2002 – 2003 adjusted for inflation. In 2005 – 2006, these programmes provided services to 32 550 sex workers (average 2325, range 1109 – 5721), similar to the total of 33 138 3 years earlier.
Table 2.
Changes in unit cost of providing HIV prevention services from 2002 – 2003 to 2005 – 2006 at 14 sex worker programmes in Andhra Pradesh.
| Cost item | Unit cost in 2002 – 2003 in INR [US$]a (range in US$) |
% Total unit cost |
Unit cost in 2005 – 2006 in INR [US$]b (range in US$) |
% Total Unit cost |
% Change in unit costc (range) |
|---|---|---|---|---|---|
| Personnel | 174.8 [3.61] (2.15 – 7.81) | 34.3 | 485.0 [10.96] (5.61 – 21.86) | 34.6 | +143 (+17 to +509) |
| Recurrent goods | 199.1 [4.11] (0.90 – 12.60) | 39.0 | 609.8 [13.78] (7.59 – 23.58) | 43.5 | +169 (0 to +749) |
| Recurrent services | 106.8 [2.21] (1.11 – 6.40) | 20.9 | 243.8 [5.51] (2.80 – 13.27) | 17.4 | +100 (−11 to +408) |
| Capitol goods | 8.6 [0.18] (0.07 – 0.41) | 1.7 | 14.9 [0.34] (0.16 – 0.68) | 1.1 | +52 (−35 to +268) |
| Building rental | 20.7 [0.43] (0.18 – 1.07) | 4.1 | 47.5 [1.07] (0.44 – 2.68) | 3.4 | +101 (+1 to +370) |
| Total unit cost | 510 [10.54] (4.58 – 28.29) | 100 | 1401 [31.65] (21.50 – 57.19) | 100 | +141 (+5 to +500) |
US$1 ¼ INR 48.40 in 2002 – 2003.
US$1 ¼ INR 44.27 in 2005 – 2006.
Percentage change calculated for change in INR cost after inflating 2002 – 2003 cost by 14%, which was the inflation between 2002 – 2003 and 2005 – 2006, to assess real change.
The number of condoms distributed by the 14 programmes increased 2.69 times from 4.77 million to 12.83 million over the 3 years, increasing the unit cost of serving each sex worker by 59.1%. Although the number of sex workers served by the programmes remained similar over 3 years, the annual number of sexually transmitted infections treated among sex workers and their partners increased by 32.5%, from 9800 to 12 989. This increased the total cost of treating sexually transmitted infections over 3 years by 37.3%, which increased the unit cost of providing HIV 10 prevention services to each sex worker by 10.6%.
Personnel costs increased by 69% over 3 years for the 14 programmes after adjusting for inflation, which increased the unit cost per sex worker by 26.5%, mostly as a result of increased payments to peer educators (14.5%) and outreach workers (7%). Over 3 years, adjusting for inflation, the average annual payment to each peer educator for part-time work increased fivefold to INR 9747 (US$220), and the average annual salary for each outreach worker increased by 145% to INR 47 393 (US$1071). The total full-time staff of the 14 programmes changed only slightly from 137 in 2002 – 2003 to 145 in 2005 – 2006, but the number of part-time peer educators decreased from 586 to 408 over this period.
The cost of recurrent services nearly doubled over 3 years for the 14 programmes after adjusting for inflation, increasing the unit cost by 19.2%. Approximately half of this increase was the result of more expenditures on staff training and development.
Original unit cost versus change in unit cost
The range of unit cost of VCT for each client in 2005 – 2006 at the 17 VCT centers was 2.7-fold, INR 82.3 (US$1.86) to INR 227.9 (US$5.15). This was less than half the 5.9-fold range for the unit cost at these centers in 2002 – 2003 [5]. The range in unit cost to serve each sex worker at the 14 programmes also decreased, from 6.2-fold in 2002 – 2003 [6] to 2.6-fold in 2005 – 2006, INR 952 (US$21.50) to INR 2532 (US$57.19).
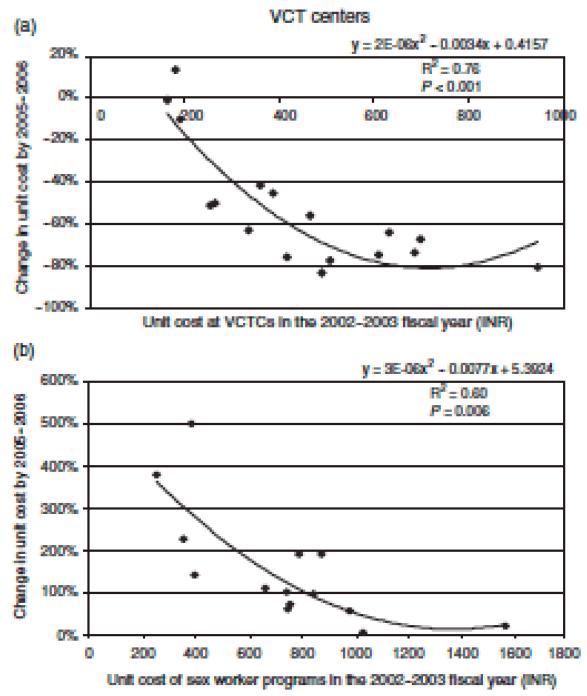
There was a direct relation between the unit cost at a VCT center in 2002 – 2003 and the magnitude of the decrease in unit cost by 2005 – 2006 for most of the distribution (Fig. 2), indicating that the centers with a higher original unit cost generally had a larger drop. There was an inverse relation between the unit cost at a sex worker programme in 2002 – 20103 and 1 the magnitude of increase in unit cost by 2005-2006 for most of the distribution (Fig. 2), indicating that programmes with a lower original unit cost generally had a higher increase.
Fig. 2. Relation between original unit cost and magnitude of change in unit cost from 2002 – 2003 to 2005 – 2006.
Unit cost versus scale in 2005 – 2006
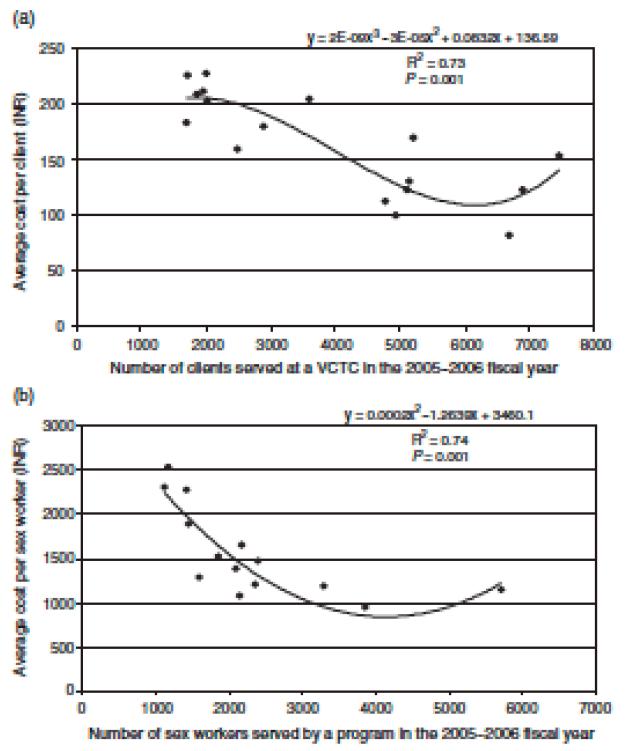
For the 2005 – 2006 fiscal year, there was mostly an inverse relation between average unit cost and scale of VCT, which suggested an upward inflection at the highest end of the scale, with the best fit obtained using a cubic function (Fig. 3). The minimum unit cost was observed at a scale above 4000 clients served per year and there was a suggestion of an increase in unit cost above a scale of 7000. There was also mostly an inverse relation between average unit cost and the scale of the sex worker programme for 2005 – 2006, which also showed an upward inflection at the highest end of the scale, with the best fit obtained using a quadratic function for 2005 – 2006 (Fig. 3). The minimum unit cost was observed at a scale of 3000 – 4000 sex workers served per year, with a suggestion of an increase in unit cost above a scale of 5000 – 6000. The upward inflections for the VCT and sex workers are only suggestive, as they were caused by only one or two data points in the two graphs.
Fig. 3. Relation of average unit cost with scale in 2005–2006.
Discussion
Scaling up of HIV prevention is currently considered the most important priority for control of the HIV epidemic by the Global HIV Prevention Working Group [1]. For scale up to be optimally effective, informed planning requires locally relevant data on how the cost of providing HIV prevention services and other aspects of these services change over a period of time, and the relation of these changes to increasing scale. This paper reports such longitudinal data for VCT and sex worker interventions in the south Indian state of Andhra Pradesh. The unit cost of providing VCT to each client halved and that for providing HIV prevention services to each sex worker more than doubled over a period of 3 years in publicly funded programmes in Andhra Pradesh.
The major reason for the drop in the unit cost of VCTwas an increase in the number of clients. This increase has continued since the VCT centers started in 2001/2002 (Fig. 1). The personnel at these centers did not change substantially over the 3-year period, nor did the time spent counseling each client, indicating that the increase in scale was unlikely to be accompanied by a decrease in quality. The HIV rate also did not drop at the centers over this period, indicating that the proportion of patients needing more intense post-test counseling did not decrease. These findings together indicate that the initial underutilization of VCT staff in the 2002 – 2003 fiscal year improved dramatically by 2005 – 2006. The low volume of services in the baseline data of 2002 – 2003 was reported by the VCT staff as being caused by inadequate demand [5], which is not surprising as the VCT services were relatively new at that time having started only in 2001/2002. The average annual load at the large VCT centers was 5305, with a counselor full-time equivalent of 1.45 in 2005 – 2006. With 250 working days a year, this translates into each counselor providing pre and post-test counseling to 15 clients daily, suggesting that this scale is reaching the limit for the available counselors. In this context, the recent plans to increase VCT services in Andhra Pradesh seem appropriate. The declining cost of HIV test kits, commonly believed to have resulted from an increase in competition among manufacturers, also contributed to lowering the unit cost of VCT.
The increase in unit cost for sex worker programmes should not necessarily be interpreted negatively, as there are suggestions of improved quality of service delivery. These included increases in the numbers of male condoms distributed, sexually transmitted infections treated, pay ments to staff (particularly peer educators and outreach workers who were previously underpaid), and spending on staff training and development, all of which plausibly could mean better services for HIV prevention. The publicly funded sex worker HIV prevention programmes started in Andhra Pradesh in 1999/2000 and their coverage has stabilized in recent years. Additional sex worker programmes have been initiated recently in Andhra Pradesh with support from the Bill and Melinda Gates Foundation. Continued focus on improved quality would be important for more effective HIV prevention programmes for sex workers in this Indian state.
Interestingly, the sixfold variation in unit costs among both VCT and sex worker programmes observed in 2002 – 2003 [5,6] decreased to less than a threefold variation in 2005 – 2006. The higher percentage decrease in unit cost at VCT centers that originally had a higher unit cost (unit cost had a strong inverse correlation with scale in 2002 – 2003) [5] indicates that inefficiencies decreased more over time when they were higher earlier. The higher percentage increase in unit cost at sex worker programmes that originally had a lower unit cost, combined with the likelihood that the increase in unit cost was related to improved quality, suggests that programmes with a lower initial unit cost had more room for improvement.
For both VCT and sex worker programmes, the suggestion of an upward inflection of unit cost at the highest end of the scale observed in 2005 – 2006 was not present in 2002 – 2003. This difference should, however, be interpreted with caution as the suggestive upward inflection was caused only by one or two data points and was not conclusive. Further assessment of this pattern is needed as the interventions progress. A rise in unit cost at the higher end of the scale was also suggested in a previous study of sex worker programmes in southern India [8]. Our data suggest the minimum unit cost for VCT above an annual scale of 4000 clients and an increase in unit cost above a scale of 7000. The minimum unit cost for sex workers suggested by our data was at an annual scale of 3000 – 4000 and an increase in unit cost above a scale of 5000 – 6000. These findings are useful for further programme planning.
The average cost of US$3.33 for providing VCT to a client in Andhra Pradesh during the 2005 – 2006 fiscal year is substantially lower than the US$11 – 22 recently used in global scale-up cost estimations for HIV interventions [3]. The 2005 – 2006 average cost of US$31.6 for providing HIV prevention services to a sex worker in Andhra Pradesh, although within the range of US$16 – 50 used recently for global scale-up estimates for different regions, is lower than the US$50 median unit cost estimated for south and southeast Asia [3]. These differences, along with the dramatic change in opposite directions we observed for the unit cost for VCT and sex workers, highlight the need for generating and using local longitudinal data to inform planning and budgeting of HIV prevention interventions. This is particularly important in the context of scaling up HIV interventions anticipated with a large increase in funding for the next phase of India’s National AIDS Control Programme [2].
Acknowledgements
The authors would like to thank the VCT centers and sex worker programmes for participating in this study, Pratap Sisodia for assistance in conducting this study, and the Andhra Pradesh State AIDS Control Society and its Technical Resource Unit for facilitating the data collection for this study.
Sponsorship: The initial portion of this study covering the baseline data was supported by the US National Institutes of Health through task order #7 contract 282-98-0026 and grant R01 DA15612.
The views expressed in this paper are those of the authors and do not necessarily reflect the views of the organizations that facilitated this study, the funding agency, or the institutions with which the authors are affiliated.
Footnotes
Conflict of interest: None
References
- 1.Global HIV Prevention Working Group . Bringing HIV prevention to scale: an urgent global priority. [Accessed: January 2008]. 2007. Available at: http://www.globalhivprevention.org/pdfs/PWG-HIV_prevention_report_FINAL.pdf. [Google Scholar]
- 2.National AIDS Control Organization, Ministry of Health and Family Welfare, Government of India . Funds and Expenditures. [Accessed: January 2008]. Available at: http://www.nacoonline.org/About_NACO/Funds_and_Expenditures/ [Google Scholar]
- 3.Stover J, Bertozzi S, Gutierrez JP, Walker N, Stanecki KA, Greener R, et al. The global impact of scaling up HIV/AIDS prevention programs in low- and middle-income countries. Science. 2006;311:1474–1476. doi: 10.1126/science.1121176. [DOI] [PubMed] [Google Scholar]
- 4.Joint United Nations Programme on HIV/AIDS (UNAIDS) Resource needs for an expanded response to AIDS in low- and middle-income countries. UNAIDS; Geneva: 2006. [Google Scholar]
- 5.Dandona L, Sisodia P, Ramesh YK, Kumar SGP, Kumar AA, Rao MC, et al. Cost and efficiency of HIV voluntary counselling and testing centres in Andhra Pradesh, India. Natl Med J India. 2005;18:26–31. [PubMed] [Google Scholar]
- 6.Dandona L, Sisodia P, Kumar SGP, Ramesh YK, Kumar AA, Rao MC, et al. HIV prevention programmes for female sex workers in Andhra Pradesh, India: outputs, cost and efficiency. BMC Public Health. 2005;5:98. doi: 10.1186/1471-2458-5-98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dandona L, Sisodia P, Prasad TLN, Marseille E, Rao MC, Kumar AA, et al. Cost and efficiency of public sector sexually transmitted infection clinics in Andhra Pradesh, India. BMC Health Serv Res. 2005;5:69. doi: 10.1186/1472-6963-5-69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Guinness L, Kumaranayake L, Rajaraman B, Sankaranarayanan G, Vannela G, Raghupathi P, et al. Does scale matter? The costs of HIV-prevention interventions for commercial sex workers in India. Bull WHO. 2005;83:747–755. [PMC free article] [PubMed] [Google Scholar]
- 9.Fung IC, Guinness L, Vickerman P, Watts C, Vannela G, Vadhvana J, et al. Modelling the impact and cost-effectiveness of the HIV intervention programme amongst commercial sex workers in Ahmedabad, Gujarat, India. BMC Public Health. 2007;7:195. doi: 10.1186/1471-2458-7-195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.National AIDS Control Organization, Ministry of Health and Family Welfare, Government of India . HIV sentinel surveillance and HIV estimation, 2006. [Accessed: January 2008]. 2007. Available at: http://www.nacoonline.org/upload/Publication/M&E%20Surveillance,%20Research/HIV%20Sentinel%20Surveillance%20and%20HIV%20Estimation,%202006.pdf. [Google Scholar]
- 11.Marseille E, Dandona L, Saba J, McConnel C, Rollins B, Gaist P, et al. Assessing the efficiency of HIV prevention around the world: methods of the PANCEA project. Health Serv Res. 2004;39:1993–2012. doi: 10.1111/j.1475-6773.2004.00329.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Marseille E, Dandona L, Marshall N, Gaist P, Bautista-Arredon-do S, Rollins B, et al. HIV prevention costs and program scale: data from the PANCEA project in five low and middle-income countries. BMC Health Serv Res. 2007;7:108. doi: 10.1186/1472-6963-7-108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Reserve Bank of India . Exchange rate of the Indian rupee: Table 154. [Accessed: August 2007]. Available at: http://rbidocs.rbi.org.in/rdocs/Publications/PDFs/72784.pdf. [Google Scholar]
- 14.India inflation rate [Accessed: August 2007]; Available at: http://indexmundi.com/india/inflation_rate_(consumer_prices).html.