Abstract
mHealth (mobile technologies for health) represents a growing array of tools being applied in diverse health care settings. mHealth interventions for improving HIV/AIDS care is a promising strategy, but its evidence-base is limited. We conducted a formative research evaluation to inform the development of novel, mHealth HIV/AIDS care interventions to be used by community health workers (CHWs) in Kampala, Uganda. A mixed methods formative research approach was utilized. Qualitative methods included 20 in-depth interviews and 6 focus groups with CHWs, clinic staff, and patients. Thematic analysis was performed and selected quotations used to illustrate themes. Quantitative methods consisted of a survey administered to CHWs and clinic staff using categorical and Likert scale questions regarding current mobile phone and internet access and perceptions on the potential use of smartphones by CHWs. Qualitative results included themes on significant current care challenges, multiple perceived mHealth benefits, and general intervention acceptability. Key mHealth features desired included tools to verify CHW task completions, clinical decision support tools, and simple access to voice calling. Inhibiting factors identified included concerns about CHW job security and unrealistic expectations of mHealth capabilities. Quantitative results from 27 staff participants found that 26 (96%) did not have internet access at home; yet, only 2 (7.4%) did not own a mobile phone. Likert scale survey responses (1–5, 1=Strongly Disagree, 5=Strongly Agree) indicated general agreement that smartphones would improve efficiency (Mean=4.35) and patient care (4.31) but might be harmful to patient confidentiality (3.88) and training was needed (4.63). Qualitative and quantitative results were generally consistent, and, overall, there was enthusiasm for mHealth technology. However, a number of potential inhibiting factors were also discovered. Findings from this study may help guide future design and implementation of mHealth interventions in this setting, optimizing their chances for success.
Keywords: mHealth, community health workers, Uganda, antiretroviral treatment, mixed methods
Introduction
mHealth (mobile technologies for health) is a growing set of tools being applied in diverse health settings (Kahn et al., 2010). mHealth interventions for improving HIV/AIDS care in low and middle-income countries is a promising strategy, but its evidence-base is still limited (Curioso et al., 2007; Kahn et al., 2010; Kaplan, 2006; Lester et al., 2010; Pop-Eleches et al., 2011). The application of technology for improving health care has not always resulted in unconditional success (Black et al., 2011), suggesting a need for thoughtful implementation guided by formative evaluations.
Formative research to systematically collect and analyze contextual information has been advocated as an important initial step in the design of HIV-related interventions (Gordon et al., 2004). On its own, such research may provide valuable baseline knowledge on participants and the community (Fisher et al., 2004). Therefore, obtaining health worker and community input is an important step in designing effective HIV/AIDS interventions and better ensuring their successful implementation.
This formative research study was designed to guide the development and implementation of task-shifting mHealth HIV/AIDS care interventions at a community-based HIV/AIDS clinic in Kampala, Uganda (World Health Organization, 2007). The mHealth interventions were conceptualized as empowering existing community health workers (CHWs) with smartphone-based tools (Figure 1). This proposed model represented a major paradigm shift in CHW tasks. We therefore conducted a formative evaluation using mixed methods to accomplish study objectives of exploring intervention acceptability, feasibility, and design considerations (Creswell et al., 2007).
Figure 1.
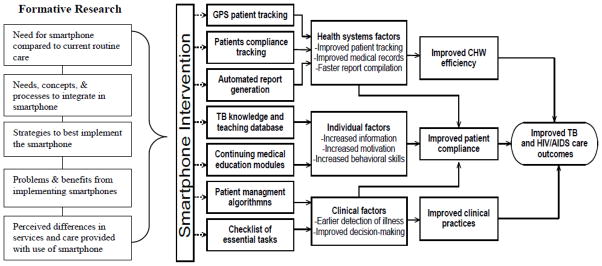
Preliminary conceptual model for a smartphone-based, mHealth HIV care intervention used by community health workers.
Methods
Study Setting
Reach Out is a community-based HIV care organization in Kampala, Uganda (Chang et al., 2009). Reach Out employs about 48 CHWs, most of whom are HIV-infected themselves, who provide supportive home visits every 1–4 weeks to about 60–150 patients each (Alamo et al., 2011).
mHealth Intervention Concept
Based upon recent experiences using mHealth in Uganda (Chang et al., 2010; Tumwebaze et al., 2012), an intervention to improve HIV/AIDS care was preliminarily conceptualized based upon a situated Information, Motivation, and Behavioral Skills model (Amico, 2011). Broadly, the mHealth intervention would involve CHWs using a smartphone application to improve communication, streamline data collection, improve clinical decisions, and receive alerts. eMOCHA (electronic Mobile Open-source Comprehensive Health Application, Baltimore, MD), previously implemented locally, was the proposed software platform (Bollinger et al., 2011).
Qualitative Methods
We conducted in-depth interviews (IDI) with 20 participants (6 CHWs, 4 clinic staff, 10 patients), and 6 focus groups (FG) (3 CHWs/clinic staff, 7–8 participants per group, mixed gender; 3 patient, 7–8 participants per group, one male, one female, and one mixed gender). Stratified purposeful sampling was used; we further sought perspective diversity in terms of age, gender, and experience (Patton, 2001). Study investigators reviewed and edited semi-structured interview guides. Guides were translated into Luganda and Luo and back-translated. A capacity-building workshop was held to train Reach Out staff members to conduct IDIs and FGs (Njie-Carr et al., 2012). Study interviews were conducted by these staff members and three of the authors over a one month period May/June 2010.
Interview questions were open-ended and explored perceived needs for smartphones, features and processes to integrate in smartphones, implementation strategies, problems and benefits, and perceived differences in care with smartphone use. Participants were shown a prototype phone with a demonstration version of software with clinical decision support and data collection tools. Clinical decision support tools are tools, often electronic but not necessarily, which health care providers interact with by linking health observations (e.g. age) with health knowledge (e.g. test all adults for HIV). CHWs were familiar with this concept as they have previously used algorithm-based paper forms.
All IDIs and FGs were conducted in the participant’s preferred language, digitally recorded, translated, and transcribed. Two authors (LWC and VNC) first read all transcripts independently, then jointly developed a codebook. Disagreements were resolved by discussion. The final list of codes was applied to all transcripts using NVivo 8 (QSR International, Victoria, Australia). Coded output was then read, merged into major themes, and summary memos and illustrative quotations were developed.
Quantitative Methods
A survey was administered to 27 CHWs and clinic staff regarding current mobile phone and internet access, as well as impressions on smartphones. Responses were analyzed descriptively using SAS 9.2 (SAS Institute Inc., Cary, NC).
Ethical Review
This study was approved by institutional review boards at the Makerere University School of Public Health, the Uganda National Council for Science and Technology, and the Johns Hopkins University School of Medicine. Written informed consent was obtained from all participants.
Results
Qualitative Evaluation Results
We identified eight major themes:
Existing Care Challenges
A number of existing challenges to providing high quality care were noted. These included structural issues such as communication difficulties among CHWs and clinic staff due to poor access to phones and inadequate patient transport and financial resources, as well the need for CHW training and skill development. As one staff member noted: “They [CHWs] get complications which really overwhelm the level of training and the level of expertise that the CHW has and they can’t deal with those complaints.” (FG) Another key issue were significant challenges related to CHW supervision and quality assurance. In particular, it was difficult for CHW supervisors to validate CHW patient reports. As one clinic staff member noted: “Yet by the report they only write, there is no proof.” (Interview)
Potential Benefits of mHealth
Almost all participants recognized areas in which mHealth interventions could be beneficial in improving quality of care. The main benefit noted was that phones would improve communication between decentralized CHWs and clinic-based staff. Often, this benefit could be realized simply through easing the ability to make voice calls. As one CHW indicated: “CHWs coming from the center to tell the clinician that the patient is in this condition, on the phone it would speed up the work as you would just call them and explain the situation and they would tell you to do this and this rather than the person coming physically.” (FG)
Another benefit was the ability to better track patients and their records and reduce paper burden. One CHW indicated, “They [CHWs] are going for home visits, they carry many files, the boxes and whatever. But when they are using this one [smartphone], I think it will reduce the burden and they will not carry a lot of things.” (FG) The potential of clinical decision support tools was also apparent: “So when we have been given the reference to identify and know the steps to follow to check a patient coughing and by using the phone to know that he/she is coughing blood, sweating at night, you will therefore be able to ask the client all those at that time, and the referral system will be made easy.” (CHW, FG)
While there were a few participants concerned about intervention costs, most appeared to feel that the intervention could bring cost savings: “Instead of the CHW to run from the community to reaching here and then go back, [he/she] will just communicate to you and then gets information. I think it will be reducing the costs.” (CHW, FG)
Desired mHealth Features
When participants were asked what features they would want in a mHealth intervention, tools to more rapidly and accurately assess adherence were repeatedly mentioned, along with the ability to better document and triage non-adherent patients to additional services. Also important was the suggestion to use photos for documenting physical findings: “I think the smartphone, what can be helpful like you can get the person is sick like maybe some parts of the body is swollen…you just snap then you bring it to the clinicians.” (CHW, Interview). Participants also cited the need for locally-appropriate clinical decision support tools and using GPS to improve patient tracking. Additionally, information on side effects of drugs, contact information for Reach Out and local hospitals, appointment reminders, and counseling information were requested. Participants also expressed interest in multimedia features for both patient and CHW validation. A CHW noted, “I go to a client who has not a blanket, they say it is not true but you just picked someone you are interested in, yet you have done your assessment that he needs it. But when I record this information and also take a photo of the resident, my bosses will confirm that this patient has no beddings.” (FG)
Quality Assurance and Improvement
Several participants, CHWs, patient, and staff, felt the intervention would be positive in terms of assuring CHW work quality and would lead to quality improvements. One CHW was quite honest in stating: “Yeah, like doing stuff and report later, I won’t report exactly what I did.” (FG). Another CHW interestingly offered: “In my view, this phone will help to bring about better understanding between the bosses and workers because it will be like a spy to establish that this employee is working. I think it will improve the working relationship between employer and the employee.” (FG) This ability to quality assure was echoed by a clinic staff member who felt “the GPS will show that so and so visited this homestead on such a date and time.” (Interview) Patients in particular felt this would improve the fidelity of CHW activities: “It will benefit us a lot to verify the information given by the CHW.” (Patient, FG)
CHW Job Security Concerns
A persistent theme surrounded CHW job security. Participants recognized how introduction of mHealth tools could lead to improved efficiencies: “First of all it’s going to reduce on time spent by the health worker or between the health worker and the client.” (Patient, FG). Some CHWs were quite forthright that the mHealth intervention represented a threat to their livelihoods, for example, revealing that CHWs often had other income-generating activities supplementing the stipend they received. Several recognized that this new technology could result in needing fewer CHWs: “Take for example in the banks before introduction of computers, it used to take many people to count money…but now it’s the machine that counts the money…. Now it is the phone that is going to do that job. So it means a job that has been done by 4 or 5 people, one person can do it.” (CHW, FG)
Confidentiality
Some participants expressed concerns about confidentiality and the security of patient data with smartphones. For example, the multimedia capabilities were perceived as having the potential for abuse if used improperly or stolen. One CHW noted: “They [Patients] will think that by taking their photos we are going to report or publicize in newspapers.” (FG). In contrast, other participants felt information would be more secure because of the mHealth intervention: “I think this smartphone will be beneficial because I think there is no one who can access the information you have talked with the client or what you have written.” (CHW, FG) Additionally, the discrete size of smartphones was cited as having confidentially benefits: “I think some of the clients who are stigmatized by other people will feel okay because the phone will be in our pockets…and nobody can identify you.” (CHW, FG)
Potential Problems and Unintended Consequences
A variety of concerns were raised about the negative consequences of the mHealth intervention improving the quality of CHW reporting. One patient described the current informal relationships between CHWs and patients which relied to a certain extent on misinformation: “Previously, he or she [CHW] might have covered up for you saying that my client is sick in that he or she might not be able to turn up and he or she comes over and signs for your drugs and she brings it to you. However with the phones she may no longer be able to do this because they will be able to see that you have not failed to come but instead you are in your own business.” (FG)
Security issues were also frequently mentioned as a potential problem, not only in terms of potential theft, but also that phones might make CHWs a target: “You will feel insecure moving with a smartphone, like a patient calls you, they are in problems, but you fear to walk with this thing at night.” (CHW, FG)
Also raised was the danger of having the CHWs tasks exceed certain limits. One clinic staff member said: “A CHW calls me on a smartphone and asks me ‘what can I give this person who is having diarrhea?’ That question seems very simple but it is very difficult because there are so many causes, so it is not healthy to prescribe what you have not seen and when you have not taken full history.” (Interview) Some also expressed concern that technology would be detrimental to the human side of their interactions: “It’s ok, but also it should not make us relax and we don’t come, because there physical sharing is very important you see?” (CHW, Interview)
Concerns were also raised about consequences if phones were diverted for non-work uses or not used properly: “I think first of all if the person who is using the phone is not well versed with using the phone, I think the information will be distorted and much of the information will be left out.” (Patient, Interview). One CHW was quite forthright in the need for security procedures or else “I may decide to sell it off and report that it has been stolen. So there must be some restrictions.” (FG)
Participants also had a number of ideas on what needed to be done at a community level to prepare for the introduction of a mHealth intervention to minimize undesirable outcomes. One patient commented: “If not sensitized then some people will not take it.” (FG). Regarding CHW preparation, one CHW said “the person who is going to handle this phone is handling…people’s lives in this smartphone, so this person must be sensitized very well.” (FG)
Unrealistic Expectations of mHealth Capabilities
Some participants demonstrated unrealistic expectations about what a mHealth intervention could accomplish. Some thought the phones might be able to diagnose all illnesses: “You find somebody sick and you can’t explain, you just take a snap and they will know exactly what’s wrong.” (CHW, FG) A few participants also seemed to believe the phone could have almost omniscient ability to detect antiretroviral adherence and other problems: “There are no ways the client can lie to you…since it’s shown on the screen.” (Interview)
Quantitative Evaluation Results
Twenty-seven staff members completed the survey. 63% (n=17) were female with a mean age of 35.2 years (range 21–56 years). Twenty-six (96%) indicated they did not have internet access at home; only 2 (7.4%) did not own a mobile phone. The median travel time to access the internet was 50 minutes (SD 66, range 3–210). About half (n=12, 44%), did not have electricity at home. Likert scale responses are shown in Table 1.
Table 1.
Likert Scale survey responses of Reach Out CHWs and staff.*
| Statement | N | Mean (SD) [Range] |
|---|---|---|
| I have a good understanding of what a smartphone is. | 27 | 4.00 (.73) [3–5] |
| Smartphones are easy to use. | 27 | 3.37 (1.1) [1–5] |
| I am comfortable using a mobile phone. | 25 | 4.52 (.59) [3–5] |
| Smartphones will be an effective tool for helping the community health workers to provide patient care. | 27 | 4.31 (.68) [2–5] |
| Smartphones will improve patient triage. | 27 | 3.81 (1.1) [1–5] |
| Smartphones will improve community health worker oversight. | 27 | 4.07 (.78) [2–5] |
| Smartphones will be harmful to patient confidentiality. | 26 | 3.88 (1.2) [1–5] |
| Smartphones will reduce the time spent on routine patient care tasks. | 26 | 4.35 (.75) [2–5] |
| I will need more training to be able to use the smartphones effectively. | 27 | 4.59 (.57) [3–5] |
| I need more training to learn how well smartphones will work. | 27 | 4.63 (.69) [2–5] |
Likert scale response options were as follows: 1=Strongly Disagree, 2=Disagree, 3=Neutral, 4=Agree, 5=Strongly Agree.
Discussion
Qualitative results found several important themes including significant current care challenges, multiple perceived benefits and desired features, and general intervention acceptability. A number of potential inhibiting factors were also identified. Quantitative results were generally consistent and supportive of qualitative findings. Overall, results indicated that our preliminary conceptual model was suitable for further intervention development and implementation.
Interestingly, qualitative results indicate that one of the most significant potential barriers was not related technology complexities but rather job security concerns. CHWs were typically living on subsistence wages, and protecting their livelihood was a paramount concern (World Health Organization, 2010). While Reach Out is a model organization (Chang et al., 2009), this evaluation identified several areas where mHealth could be beneficially applied, with assuring CHW work quality a priority issue.
This tension highlighted by this research between the benefits of technologic “industrialization” and the status of workers is well described in other fields such as manufacturing (Brynjolfsson et al., 2011). However, this phenomena has not received significant attention in the HIV/AIDS and mHealth literature, and may be a significant challenge to creating efficiencies in HIV/AIDS programming (Cohn et al., 2011). While task shifting from higher trained to lower trained cadres of workers is supported by PEPFAR and the World Health Organization (World Health Organization, 2007), as global funding for HIV/AIDS declines, improving efficiency may come at the cost of provider jobs. Implementers will need to plan for and address these critical issues to maximize the chances for success of health delivery interventions. Nonetheless, our study demonstrates the desire and need for implementation and evaluation of mHealth interventions in low and middle-income countries, and the potential of these interventions to improve HIV/AIDS services.
This study had important limitations including challenges with generalisability as this evaluation was performed at a single, urban institution with a relatively small sample size. Although researchers attempted to use a variety of data collection methods to reduce response bias and informed consent emphasized participant protections, participants responses may have been influenced by social biases. Most interviews were conducted by staff members, which may have shaped responses. We also conducted a thematic analysis after data collection was completed rather than a true iterative analysis. However, we did have repeated mention of the same issues and felt saturation of themes was largely achieved. Finally, parts of this evaluation were carried out over a short period of time and may not have fully captured evolving viewpoints in a dynamic technologic and service delivery environment.
Overall, this study found enthusiasm for using mHealth at a community-based HIV/AIDS care program in Uganda. However, a number of important potential inhibiting factors were also discovered. This formative research may help guide future design and implementation of mHealth interventions in this setting, thereby optimizing their chances for success. Evaluations such as this one allow improved integration of local contextual issues and community concerns which will assist in having a more informed and user-centric approach. Ideally, next steps will be to develop a mHealth intervention based upon these study findings and then assess its impact on CHWs and patients. As one CHW aptly noted, “It is said that an organization has to develop. Even when you give birth to a child, it sits crawls, walks and eventually grows. Therefore, it is high time we also acquired this new technology.” (FG)
Acknowledgments
This study was supported by the National Institute of Mental Health of the National Institutes of Health (1K23MH086338-01A2). We thank the community health workers, clinic staff, and patients of Reach Out for their participation in this study, and Caitlin Kennedy for her editorial contributions.
References
- Alamo S, Wabwire-Mangen F, Kenneth E, Sundary P, Laga M, Colebunders RL. Task-Shifting to Community Health Workers: Evaluation of the Performance of a Peer-Led Model in an Antiretroviral Program in Uganda. AIDS Patient Care STDS. 2011;25 doi: 10.1089/apc.2011.0279. [DOI] [PubMed] [Google Scholar]
- Amico KR. A situated-Information Motivation Behavioral Skills Model of Care Initiation and Maintenance (sIMB-CIM): an IMB model based approach to understanding and intervening in engagement in care for chronic medical conditions. J Health Psychol. 2011;16(7):1071–1081. doi: 10.1177/1359105311398727. [DOI] [PubMed] [Google Scholar]
- Black AD, Car J, Pagliari C, Anandan C, Cresswell K, Bokun T, McKinstry B, Procter R, Majeed A, Sheikh A. The impact of eHealth on the quality and safety of health care: a systematic overview. PLoS Med. 2011;8(1):e1000387. doi: 10.1371/journal.pmed.1000387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bollinger RC, McKenzie-White J, Gupta A. Building a global health education network for clinical care and research. The benefits and challenges of distance learning tools. Lessons learned from the Hopkins Center for Clinical Global Health Education. Infect Dis Clin North Am. 2011;25(2):385–398. doi: 10.1016/j.idc.2011.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brynjolfsson E, McAfee A. Race Against The Machine: How the Digital Revolution is Accelerating Innovation, Driving Productivity, and Irreversibly Transforming Employment and the Economy. Digital Frontier Press; 2011. [Google Scholar]
- Chang LW, Alamo S, Guma S, Christopher J, Suntoke T, Omasete R, Montis JP, Quinn TC, Juncker M, Reynolds SJ. Two-year virologic outcomes of an alternative AIDS care model: evaluation of a peer health worker and nurse-staffed community-based program in Uganda. J Acquir Immune Defic Syndr. 2009;50(3):276–282. doi: 10.1097/QAI.0b013e3181988375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chang LW, Kagaayi J, Nakigozi G, Ssempijja V, Packer AH, Serwadda D, Quinn TC, Gray RH, Bollinger RC, Reynolds SJ. Effect of peer health workers on AIDS care in Rakai, Uganda: a cluster-randomized trial. PLoS One. 2010;5(6):e10923. doi: 10.1371/journal.pone.0010923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohn J, Holtzman D, Baker B. Efficiencies in AIDS programming: the rhetoric and the realities. J Acquir Immune Defic Syndr. 2011;58(3):229–232. doi: 10.1097/QAI.0b013e3182303428. [DOI] [PubMed] [Google Scholar]
- Creswell JW, Plano Clark VL. Designing and conducting mixed methods research. Sage Publications, Inc; 2007. [Google Scholar]
- Curioso WH, Kurth AE. Access, use and perceptions regarding Internet, cell phones and PDAs as a means for health promotion for people living with HIV in Peru. BMC Med Inform Decis Mak. 2007;7:24. doi: 10.1186/1472-6947-7-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fisher JD, Cornman DH, Osborn CY, Amico KR, Fisher WA, Friedland GA. Clinician-initiated HIV risk reduction intervention for HIV-positive persons: Formative Research, Acceptability, and Fidelity of the Options Project. J Acquir Immune Defic Syndr. 2004;37(Suppl 2):S78–87. doi: 10.1097/01.qai.0000140605.51640.5c. [DOI] [PubMed] [Google Scholar]
- Gordon CM, Stall R, Cheever LW. Prevention interventions with persons living with HIV/AIDS: challenges, progress, and research priorities. J Acquir Immune Defic Syndr. 2004;37(Suppl 2):S53–57. doi: 10.1097/01.qai.0000142321.27136.8b. [DOI] [PubMed] [Google Scholar]
- Kahn JG, Yang JS, Kahn JS. ‘Mobile’ health needs and opportunities in developing countries. Health Aff (Millwood) 2010;29(2):252–258. doi: 10.1377/hlthaff.2009.0965. [DOI] [PubMed] [Google Scholar]
- Kaplan WA. Can the ubiquitous power of mobile phones be used to improve health outcomes in developing countries? Global Health. 2006;2:9. doi: 10.1186/1744-8603-2-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lester RT, Ritvo P, Mills EJ, Kariri A, Karanja S, Chung MH, Jack W, Habyarimana J, Sadatsafavi M, Najafzadeh M, Marra CA, Estambale B, Ngugi E, Ball TB, Thabane L, Gelmon LJ, Kimani J, Ackers M, Plummer FA. Effects of a mobile phone short message service on antiretroviral treatment adherence in Kenya (WelTel Kenya1): a randomised trial. Lancet. 2010;376(9755):1838–1845. doi: 10.1016/S0140-6736(10)61997-6. [DOI] [PubMed] [Google Scholar]
- Njie-Carr V, Kalenge S, Kelley J, Wilson A, Muliira JK, Nabirye RC, Glass N, Bollinger R, Alamo-Talisuna S, Chang LW. Research Capacity-Building Program for Clinicians and Staff at a Community-Based HIV Clinic in Uganda: A Pre/Post Evaluation. J Assoc Nurses AIDS Care. 2012;23(5):431–441. doi: 10.1016/j.jana.2011.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patton MQ. Qualitative research and evaluation methods. 3. Thousand Oaks, CA: Sage Publications Inc; 2001. [Google Scholar]
- Pop-Eleches C, Thirumurthy H, Habyarimana JP, Zivin JG, Goldstein MP, de Walque D, Mackeen L, Haberer J, Kimaiyo S, Sidle J, Ngare D, Bangsberg DR. Mobile phone technologies improve adherence to antiretroviral treatment in a resource-limited setting: a randomized controlled trial of text message reminders. AIDS. 2011 doi: 10.1097/QAD.0b013e32834380c1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tumwebaze H, Tumwesigye E, Baeten JM, Kurth AE, Revall J, Murnane PM, Chang LW, Celum C. Household-Based HIV Counseling and Testing as a Platform for Referral to HIV Care and Medical Male Circumcision in Uganda: A Pilot Evaluation. PLoS One. 2012;7(12):e51620. doi: 10.1371/journal.pone.0051620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization. Global recommendations and guidelines on task shifting. Geneva: World Health Organization; 2007. [Google Scholar]
- World Health Organization. Increasing access to health workers in remote and rural areas through improved retention: global policy recommendations. Geneva: WHO; 2010. [PubMed] [Google Scholar]


