Abstract
Introduction
Vein wall fibrotic injury following deep venous thrombosis (VT) is associated with elevated matrix metalloproteinases (MMPs). Whether and by what mechanism MMP2 contributes to vein wall remodeling after VT is unknown.
Methods
Stasis VT was produced by ligation of the inferior vena cava (IVC) and tissue was harvested at 2, 8, and 21 days in MMP2 −/− and genetic wild type (WT) mice. Tissue analysis by immunohistochemistry, ELISA, real time PCR, and zymography was performed.
Results
Thrombus resolution was impaired at 8d in MMP2 −/− as compared with WT, evidenced by a 51% increase in VT size (p < .01), and 3 fold fewer vWF positive channels (p<.05). In MMP2 −/− mice, the main phenotypic fibrotic differences occurred at 8d post VT, with significantly less vein wall collagen content (p=.013), 4 fold lower procollagen III gene expression (p < .01) but no difference in procollagen I as compared to WT. Decreased inflammation in MMP2−/− vein walls was suggested by ~ 3 fold reduced TNFα and IL1β at 2d and 8d post VT (p < .05). A 4 fold increase in vein wall monocytes (p = .03) with 3 fold decreased apoptosis (p < .05), but no difference in cellular proliferation at 8d was found in MMP2−/− as compared with WT. As increased compensatory MMP9 activity was observed in the MMP2 −/− mice, MMP2/9 double null mice had thrombus induced with VT harvest at 8d. Consistently, 2 fold larger VT, a 3 fold decrease in vein wall collagen, and a 3 fold increase in monocytes was found (all p < .05). Similar findings were observed in MMP9 −/− mice administered an exogenous MMP2 inhibitor.
Conclusion
In stasis VT, deletion of MMP2 was associated with less midterm vein wall fibrosis and inflammation, despite an increase in monocytes. Consideration that VT resolution was impaired with MMP2 (and MMP2/9) deletion suggests direct inhibition will likely also require anticoagulant therapy.
Keywords: Venous thrombosis, inflammation, matrix metalloproteinases, monocytes
Introduction
Deep venous thrombosis (DVT) is a significant health care problem in this country, with over 250,000 patients affected yearly, although these figures may be conservative.1 An additional 200,000 patients are affected by the late sequelae of post thrombotic syndrome (PTS), characterized by leg pain, sensations of heaviness, limb edema, discoloration and occasionally ulceration.2 The end result after DVT is the conversion of a compliant, thin walled vein with functional valves to a thick walled vessel, often with nonfunctioning valves.3 The physiological result of damaged veins is pooling of blood in the dependent extremities, producing venous hypertension, fluid transudation, edema, and potentially ulceration.
Despite effective anticoagulant therapy treatments for DVT, there are no therapies that specifically target the PTS remodeling processes.4 While surgical and interventional therapy may be beneficial for selected patients, treatment for PTS is mainly supportive, consisting of compression and wound care. While largely effective, compression does not correct the fundamental changes that occur in the venous system and compliance with such ongoing regimens is often difficult.
Rodent studies have suggested that the mechanism and duration of thrombosis affects the magnitude of post-thrombotic vein wall damage seen. For example, a stasis thrombus is more damaging than a non-static thrombus, and negatively affects collagen structure and venous compliance.5, 6 In addition to the intense inflammatory reaction seen following DVT, there is a phenotypic alteration in the extracellular matrix, associated with activation of matrix metalloproteinases (MMPs), including MMP2 and 9.6–9 Of these, MMP2 is most significantly elevated in the vein wall after stasis VT at the mid and later time points,6 and is when PTS occurs in humans. While broad MMP inhibition may decrease some measures of injury,10, 11 their specific role has not been defined in the vein wall after VT. The additive effects of MMP2/9 genetic deletions have been highlighted with experimental lung injury.12 Moreover, recent studies suggest certain biomarkers may be predictive of PTS well as associated with DVT resolution in humans, including MMPs.4, 13
We hypothesized that abrogation of matrix remodeling via genetic deletion of MMP2 and combined MMP2/9 would lessen the damage seen in the vein wall following stasis venous thrombosis (VT).
Methods
Animal Model
Male mice 6 – 8 weeks old, MMP2 −/− (kindly donated by Dr. Eric Choi) and C57BL/6 their WT were used for the experiments. With all surgical procedures, the mice were anesthetized using inhalational Isoflurane and O2, and continuously monitored. Animal studies were approved by the University of Michigan Committee on Use and Care of Animals.
Experimental VT was created in the mouse using infrarenal inferior vena cava (IVC) ligation as previously described.6, 14–16 Briefly, mice were anesthetized, and underwent midline laparotomy. The IVC was ligated with a 7 - 0 prolene suture immediately below the renal veins. Back (lumbar) branches were ablated with cautery, and all visible side branches were interrupted with 7 - 0 prolene suture. Mice were sacrificed on days 2, 8, and 21d post ligation. At sacrifice, the thrombosed IVC segment was carefully dissected and removed for formalin fixation and paraffin embedding (for histology/immunohistochemistry) or immediately snap frozen (−70° C) to preserve for tissue processing.
At days 2 and 8, the thrombus was separated from the vein wall for processing; however, at 21d, the thrombus and vein wall form a segment of scar tissue, which cannot be separated without tissue disruption, and those segments were processed together. In other experiments, a specific MMP2 inhibitor17, 18 (OA-Hy, EMD Biosciences, Gibbstown, NJ) 6.25 mcg per mouse in 1 mg/ml diluted DMSO or the vehicle, was administered intra-peritoneal to MMP9 −/− mice immediately after IVC ligation and at 4d post VT, with harvest at 8 days. Separate C57BL/6 MMP9 −/− were crossed with C57BL/6 MMP-2 −/− mice to generate MMP2 −/− double null mice.
SDS-PAGE Gelatin Zymography
Activity of the gelatinases (MMP2 and MMP9, active and latent forms) was determined by gelatin zymography on 10% SDS-polyacrylamide gels, as previously described.5, 15, 18 Activity was visualized as light staining bands on a dark background, and normalized to the total amount of protein present in each sample as previously described.
Histology/Immunohistochemical/Apoptosis/Collagen Staining
Tissue samples were formalin fixed, paraffin embedded, and cut into 5 μm sections as described.14, 15 Nonspecific sites were blocked with normal serum, and sections were incubated with primary antibodies to Mac2 (1:200, Cedarlane Laboratories, Burlington, NC), von Willebrand’s Factor (vWF; 1:500, Abcam, Cambridge, MA), and Ki-67 (1:100, Abcam, Cambridge, MA). A species-specific ABC peroxidase kit for either rabbit or rat (Vector Laboratories Inc., Burlingame, California) was used according to the manufacturer’s instructions for the corresponding secondary antibody and subsequent steps. The slides were counterstained with hematoxylin. In a blinded fashion, positive cells in 5 high power fields (1000x) radially around the IVC were counted and totaled.
The presence of apoptotic cell death was assessed in the vein wall by using a commercially available kit to determine the presence of characteristic DNA breaks by the TUNEL method (Trevigen Inc., Gaithersburg, MD).
Picrosirius red staining to quantify collagen content was performed as described.19, 20 These sections were then analyzed in crossed-plane polarized light from a monochromatic source to assess cross linked collagen. Two images for each were obtained using a Zeiss Axio M1 scope and Zeiss AxioVision software (Carl Zeiss Microimaging GmbH, Göttingen, Germany) at 0 and 90 degrees to the plane of polarization, in order to capture the birefringence of fibers extinguished in one direction. The images were analyzed blindly utilizing NIH Image J software. The area corresponding to the vein wall was selected as a region of interest, and then the image underwent threshold segmentation to differentiate collagen from other (mainly cellular and empty space) components of the vein wall. A vein wall collagen score was assigned by the formula [(% birefringent area) × (measured vein wall area)]/(total specimen area).21
To account for non-collagen vein wall changes, intimal thickness scoring was assessed from H and E sections as described.22 A consistent mid-section thrombosed IVC segment was used for all histological analysis.16, 18, 23
Antigen Analysis by ELISA
Vein wall tissue was homogenized, subjected to ultrasonic sonication, followed by centrifugation samples centrifuged at 10,000×g for 5 minutes, and the supernatant was collected for analysis. Quantification of the analyzed antigens was normalized to the total protein present in the sample, using a modified Bradford assay (Pierce Inc., Rockford, IL). ELISA for mouse tumor necrosis factor-alpha (TNF-α), interleukin-1 beta (IL-1β), and monocyte chemotactic protein-1 (MCP-1) was performed according to manufacturer’s instructions (all from R and D, Minneapolis, MN).5, 14
Quantitative (real-time) RT-Polymerase Chain Reaction (PCR)
The levels of expression for genes of interest were determined by isolating total RNA (RNA) via Trizol extraction as previously described.15, 16 Then, the RNA underwent reverse transcription. The cDNA was then subjected to a real-time reverse transcriptase reaction using Taq polymerase (Promega, Madison, WI) in a SmartCycler quantitative PCR system (Cepheid, Sunnyvale, CA). SYBR green intercalating dye (Roche, Indianapolis, IN) was used to monitor levels of cDNA amplification for each gene. β-actin was used as an internal control for reference in each sample. The sequence numbers were: Col1a2 - RefSeq# NM_007743.3; Col3a1- RefSeq# NM_009930.2; tropoelastin - RefSeq # NM_ 0036834.3; beta Actin- RefSeq# NM_007393.3.
Statistical Analysis
All data are presented as mean +/− SE. Comparisons were made using an unpaired Student’s t-test or ANOVA with Dunnett’s or Bonferroni’s multiple comparison tests as appropriate, using GraphPad Prism version 4.0 for Windows (Graphpad Software, San Diego, CA).
Results
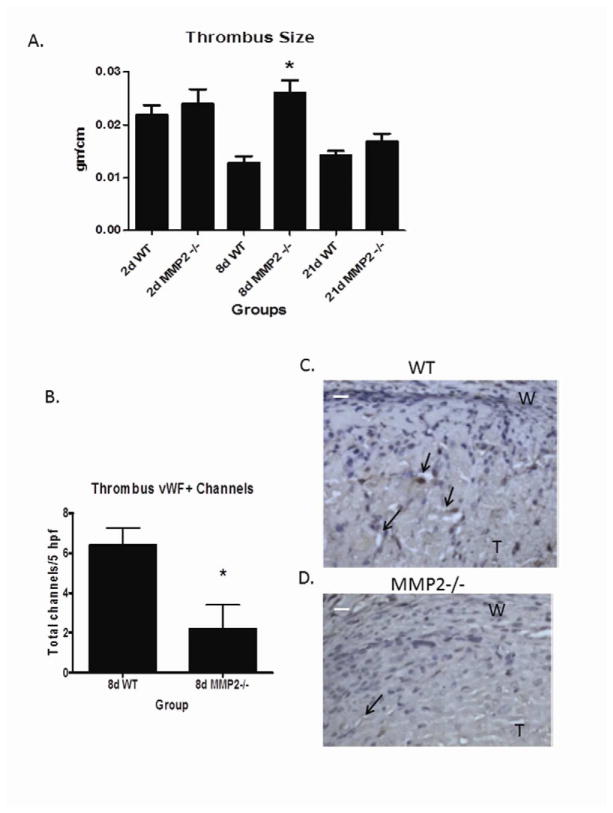
MMP2 deletion impairs midpoint VT resolution
The weight:length ratio of a resolving thrombus provides a simple but reliable measure of thrombus resolution.6, 14–16 Given that the inflammatory response is crucial for resolving VT, interventions which affect inflammation might impair thrombus resolution. At 8 days, MMP2 −/− mice had a 51% increase in VT size compared with WT (N = 15 – 20, P < .001) (Figure 1a). These data are consistent with prior investigation of MMP2 activity in VT resolution between 4 and 8d and this timepoint was not repeated.15, 18 No differences were observed in VT size at 2d (N = 12 – 14; P = .6) or 21d (14 ± 1 vs. 17 ± 2 mg/cm, N= 20–22, P = .16) in MMP2 −/− mice as compared to WT controls.
Figure 1.
Thrombus size as measured by weight/length ratio showed larger VT at d8 in MMP2 −/− mice (A). Thrombus channels were fewer in MMP2 −/− mice as compared to WT (B). Photomicrographs in WT (C) show numerous channels in periphery of the thrombus. Fewer vWF(+) channels noted in MMP2 −/− VT (D). @400x, arrows mark channels. W = wall; T = thrombus. White bar = 10 μm.
Resolution of a VT is conferred in part by development of vWF+ vascular channels in the thrombus.14, 16 Correlating with impaired thrombus resolution in MMP2 −/− mice at 8d were 3 fold less vWF + channels (N = 5; P = .025) (Figure 1b,c,d).
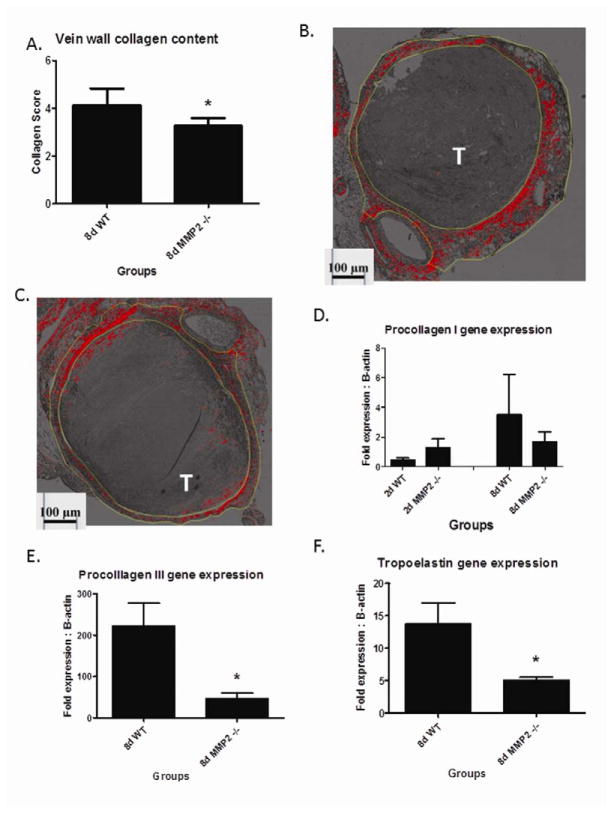
Post-Thrombotic Vein Wall Collagen Metabolism is altered in MMP2 −/− mice
The 8 and 21d time points were chosen to evaluate the loss of MMP2 as these mimic the post-thrombotic syndrome time frame, with a significantly thicker and collagen dense vein wall, as well as when MMP2 activity is present.5, 6 Vein wall collagen as assessed by Picosirius red increases over time following thrombosis (Supplemental Figure S1). The collagen content was ~35% less in the MMP2 −/− mice as compared with the WT (N = 4 – 5; P = .013) (Figure 2a – c), with no differences in intimal thickness at 8d (Supplemental Figure S2). No difference in collagen was found at 21d in MMP2 −/− compared to WT (6.5 +/− 1.3 vs. 6.0 +/− 1.4% vein wall section; N = 4 – 5, P = .9).
Figure 2.
A) Vein wall collagen content was less in MMP2 −/− compared with WT. Sirius Red stained vein wall section of WT (B), contrasting with the thinner and less dense collagen (red) in the MMP2 −/− vein walls(C). Histological images @100X. Procollagen I was not altered in the MMP2 −/− vein wall as compared to WT (D), while Procollagen III was reduced at 8d (E). Tropoelastin gene expression was reduced at 8d in the MMP2−/− as compared with WT (F). T = thrombus. * P < .05.
Experimental VT is associated with an upregulation of procollagen mRNA in the vein wall,13 specifically procollagen I and procollagen III. This was analyzed at 2 and 8d. In the MMP2 −/− mice, procollagen I gene expression was not significantly different at 2 or 8d (2d comparison P = .26; 8d comparison P = .55; N = 4–5 each group) (Figure 2d). Pro-collagen III gene expression was decreased ~4 fold in the MMP2 −/− mice as compared with the WT at 8d (N = 5; P < .01), with no differences at 2d (not shown) (Figure 2e). As a precursor to elastin, tropoelastin gene expression was not altered at 2d, but was decreased ~ 2.5 fold at 8d in MMP2 −/− as compared to WT mice (Figure 2f).
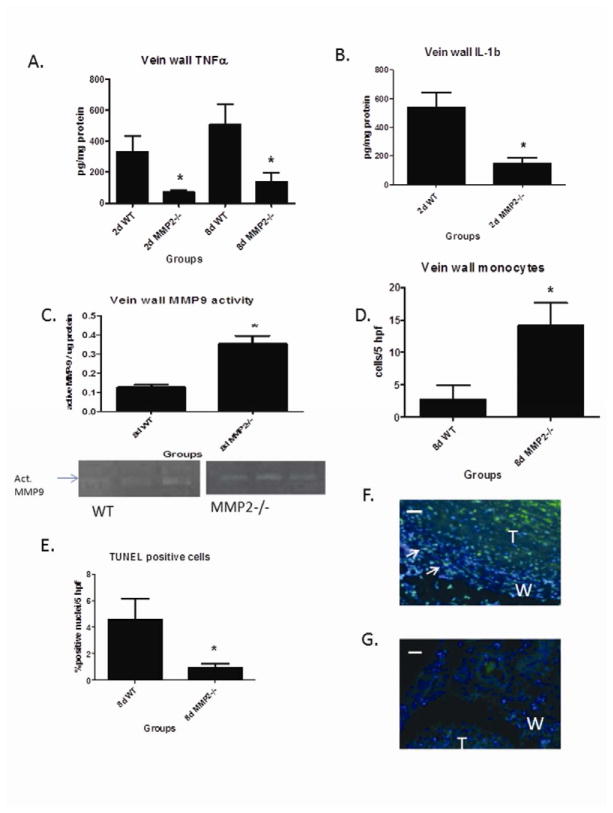
Vein wall inflammation and apoptosis is decreased in MMP2 −/− mice at 8d
Inflammatory mediators are present in the thrombus and vein wall after VT, including TNFα, IL1β, and MCP-1.5, 14, 15 In the MMP2 −/− mice, TGFβ protein levels were not significantly different at 8d (3.9 +/− 0.9 vs. 2.5 +/− 0.08 ng/mg protein; N = 5, P = NS), as compared with WT. TNFα was reduced 3 – 4 fold at 2 and 8d in the MMP2 −/− mice as compared with WT (N = 4 – 5; P = .03) (Figure 3a). IL-1β was reduced 2.5 fold in the MMP2 −/− mice as compared with WT at 2d (N = 4 – 5; P = .01) (Figure 3b), but not at 8d (517 ± 300 vs. 361 ± 71 pg/mg protein; N = 5, P > .05). No significant differences were found in MCP-1 levels at 2 or 8d (not shown). The MMP2 −/− mice had ~3 fold reciprocally increased MMP9 activity by zymography (N = 5; P = < .01) at day 8 only (Figure 3c).
Figure 3.
Vein wall TNFα in MMP2−/− was less at 2 and 8d (A), while IL1β was reduced at 2d (B). C) Vein wall active MMP9 activity was increased in MMP2 −/− mice at 8d by zymography. D) Vein wall monocytes were increased at 8d in MMP2 −/− mice as compared to WT. E, F, G) Apoptosis as marked by TUNEL + green colocalized with DAPI blue staining nuclei showed less medial (+) cells at 8d in the MMP2 −/− vein wall compared with WT. @400X. W = wall; T = thrombus; arrows mark (+) cells; * p < .05. White measurement bar = 10 μm.
Since MMP2 is both produced by leukocytes in the early inflammatory response, and in part mediates their migration across collagen-rich matrices such as the basement membrane,24 we investigated whether the loss of MMP2 would have an effect on the number of inflammatory cells present in the vein wall. In the MMP2 −/− vein wall, monocytes were increased ~4 fold in MMP2 −/− mice as compared to WT (N = 4 – 5; P = .03) (Figure 3d and Supplemental Figure S3).
Medial cellular proliferation and apoptosis contributes to post vascular injury fibrosis.25, 26 To evaluate for the contribution of cellular proliferation, Ki67 antigen staining was evaluated in the medial vein layer.5 Ki67 positive cells staining showed no significant difference in MMP2 −/− as compared with WT sections (7 +/− 1 vs. 5 +/− 1, cells/5hpf N = 6 – 7, P = .3). However, fewer apoptotic nuclei by TUNEL + staining was present in the MMP2 −/− mice, with ~4 fold less apoptosis at 8d as compared to WT (N = 6; P = .045) (Figure 3e – g).
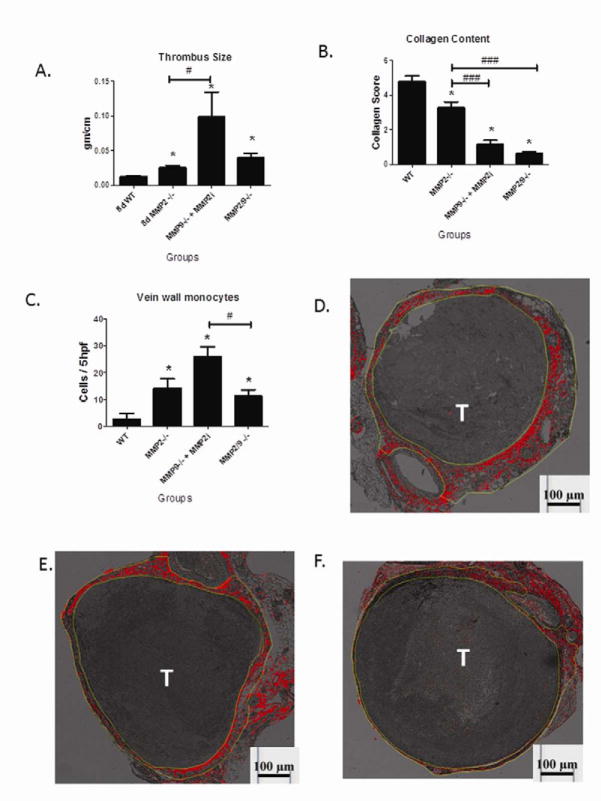
Combined MMP2 and MMP9 Deletion on Vein Wall Response
For the previous experiments with the single MMP2 deleted mice, we found reciprocally elevated MMP9 activity at 8d. This was also the point where the collagen metabolism was affected most significantly by the MMP2 deletion. Thus, we evaluated MMP2 −/− MMP9 −/− double null mice as well as MMP9 −/− mice given a specific MMP2 inhibitor.18 Stasis VT was induced with harvest at 8 d. We found that thrombus resolution was impaired in the MMP9 −/− + MMP2 inhibitor with 2.5 fold increase (N = 14; P < .05), and 1.6 fold increase in VT size in the MMP2/9 double null mice as compared to WT (N = 5; P < .05) (Figure 4a). Evaluating the vein wall collagen by Sirius red analysis, we found that MMP9 −/− + MMP2 inhibitor and MMP2/9 double null mice had 3–6 fold reduced collagen content in the vein wall (N = 4 – 5; P < .05) (Figure 4b, d–f). Consistent with the single MMP9 −/− or MMP2 −/− phenotypes, we found a ~5 fold increase in vein wall monocytes with MMP9 −/− + MMP2 inhibitor and a 4 fold increase in monocytes in the MMP2/9 double null mice as compared with WT (N = 4, P < .05) (Figure 4c).
Figure 4.
A) Thrombus size was increased at 8d in MMP9 −/− (+) MMP2 inhibitor as well as MMP2/9 −/− double null mice. B) Collagen content was reduced in the MMP9 −/− (+) MMP2 inhibitor and the MMP2/9 −/− double null as compared to WT. C) Monocytes were elevated in MMP9 −/− + MMP2 inhibition and MMP2/9 double null −/− mice. D, E, F) Representative photomicrographs of WT, MMP9 −/− (+) MMP2 inhibition and MMP2/9 −/− mice. Histological images @100X. T = thrombus; * = p < .05 by ANOVA with Dunnett’s multiple comparison test. # = P < .05, ### = P < .001 by ANOVA with Bonferonni’s correction.
We performed a second analysis using only MMP2−/− as the control for the MMP9−/− + MMP2 inhibitor and MMP2/9−/− (Figure 4). We found that comparison using ANOVA with Bonferroni’s correction that the VT size was only significantly larger in the MMP9−/− + MMP2 inhibitor group (P <.05) as compared with the MMP2−/− group. Vein wall collagen content was significantly less in both MMP9−/− + MMP2 inhibitor and MMP2/9−/− as compared with MMP2−/− (P < .001). Finally, vein wall monocytes were significantly greater in the MMP9−/− + MMP2−/− inhibitor group (P = .03), but not greater in the MMP2/9−/− group.
Discussion
While anticoagulation is effective treatment for DVT, no specific therapies are available to target the vascular inflammatory and fibrotic processes that result in PTS.2, 4 Remodeling of the ECM in vessels is mediated in part by the MMPs,25 and activity has been visualized in vivo in arterial injury27 and veins after VT.9Resolving VT and the vein wall response are associated with MMP2 and MMP9 time dependent activity changes, but their direct role had not been assessed.6, 7 The MMP2 seems most likely involved with vein wall metabolism given its kinetics and activities6, 25 and thus we focused on this. In this study, we demonstrate VT resolution was impaired in MMP2 −/− mice, and that the post thrombotic vein is characterized by temporal changes in collagen content, dependent on both MMP2 with associated genetic, cellular, and inflammatory changes. These findings also suggest a complex interplay of factors that is likely not simply related to collagen or matrix turnover.24, 25
Although not the primary focus of these experiments, VT resolution was impaired at the mid time point (8d) in MMP2 −/− mice. Our data suggest VT resolution is in part dependent on MMP2 activity, as VT were significantly larger in MMP2 −/− mice at 8d. We have also observed a correlation between concentration of MMP activity and thrombus resolution in real time imaging.9 Prior work in our lab has also shown that deletion or inhibition of MMP2 is associated with impaired thrombus resolution at 4d,15, 18 independent of plasminogen activation. Thrombi resolve in part by neovascularization.8 MMP2 is critical for neovascularization28 and consistent with impaired VT resolution, significantly fewer vWF + channels in MMP2 −/− thrombi were found. The lack of MMP2 activity did not affect early thrombus formation or resolution, probably because the stasis model mechanism predominates, as well as cellular mediated resolution may be more important at mid to later time points.15, 29 Other cellular mechanisms independent from MMP2 exist as the VT sizes were similar at 21d, suggesting compensatory accelerated resolution in the MMP2 −/− mice. This observation also underscores the temporal importance of MMP2 in VT resolution.
Numerous studies have highlighted the role of MMPs in the response to vascular injury, including VT resolution.6, 25 Matrix metalloproteinases are zinc containing endoproteinases with multiple targets, including matrix and non-matrix substrates.24 In multiple models of tissue injury, early activation of both MMP2 and MMP9 occurs prior to the end stage-fibrotic process,25 including our own model.6 In this study, we demonstrate that loss of MMP2 is associated with less vein wall collagen at midterm after the stasis thrombosis injury. Moreover, the addition of MMP9 deletion was additive, as the MMP2/9 −/− double null mice or MMP9 −/− with an exogenous MMP2 inhibitor had markedly less post-thrombotic vein wall collagen than the single MMP2 deletion (Figure 4). Consistent with our findings is that both MMP2 and/or MMP9 gene deletions are associated with less constrictive fibrosis in direct and flow mediated arterial injury models.26, 30–32 Although we did not specifically investigate the MMP2 −/− venous vascular smooth muscle cell (vSMC) migration potential, these reports suggest significant migration impairment in vitro. These studies provide an explanation for our observed phenotype; namely, less collagen production after injury occurs, possibly because of less VSMC migration and activation. We acknowledge that we did not specifically co-localize collagen production to VSMC and other medial cells may be important. Lastly, the protection from late vein wall fibrosis in MMP2−/− mice was not observed at 21d post thrombosis. We have observed this in other experiments with different genetic deletions and genetic backgrounds.21 This suggests that other processes that are not monocyte and MMP dependent mechanisms of injury predominate at this late time point.
In general, the MMPs regulate vessel collagen by degradation as well as cellular influx and function.24, 25 Deletion of MMP2 was associated with decreased gene expression of procollagen III and tropoelastin in response to vein wall injury, suggesting less vein wall metabolic turnover. Specifically, the decrease in vein wall collagen in the MMP2 −/− mice may be directly related to decreased collagen gene expression and protein translation. Moreover, increased TNFα is associated with fibrosis,33, 34 and was significantly decreased in the MMP2 −/− mice. We did not directly address if any of the cytokines were mechanistically involved with vein wall responses, however. It is unlikely that VSMC were directly affected, as medial cell proliferation was not affected by loss of MMP2, consistent with some, but not all reports.25, 31 However, medial vein wall cellular apoptosis was significantly decreased in MMP2 −/− as compared to WT. This may be related to the relative increase in MMP9 activity in the MMP2 −/− mice, and greater clearance of apoptotic cells, as suggested in other models.12 Other MMPs that we did not assess may also play a role in response to injury, such as MMP3 and MMP12.32 Besides the proinflammatory cytokine induction of MMP activation, vessel wall strain may contribute as has been highlighted by arterial experimental data.35 Certainly, stasis thrombosis distends the vein wall and likely directly promotes MMP activation, possibly accounting for the upregulation of MMP9 activity in the MMP2−/− mice.
Although TIMPs may play a major role in certain disease process such as atherosclerosis36 and hepatic fibrosis,37 it did not appear these were altered significantly in our prior report after stasis VT.6 Preliminary experiments with TIMP1 −/− mice, which have significantly increased MMP2 and 9 activities at 8 and 21d, did not show a significant increase in vein wall collagen (Henke, PK, unpublished data). This suggests that increased MMP2 and 9 activity itself does not worsen parameters of vein wall healing in the stasis VT model, contrasting with solid organ injury models.37
Most of the phenotype differences were observed at 8d post VT, which is when monocytes predominate in the vein wall.5, 14, 15 While part of the normal inflammatory response, monocytes may or may not promote fibrotic tissue repair.38 Consistent with the current report is that P-selectin inhibition after stasis VT is associated with increased vein wall monocytes, but less vein wall fibrosis.22, 39 Recent investigations suggest that monocyte subtypes confer differing inflammatory or anti-inflammatory responses (e.g. M2) depending on the environment and time frame.38 Interestingly, both MMP2 −/−, the MMP9−/− + MMP2 inhibitor, and the double null mice had increased vein wall monocyte influx, suggesting these proteinases are not essential for monocyte influx following injury, but may be important for cellular egress. Indeed, in a pulmonary inflammatory model with MMP2/9 double deletion, a significant increase in inflammatory cells was observed after injury due to inhibited trafficking.12 Another mechanism accounting for increased monocytes may involve MMP chemokine processing.24 However, since MCP-1 was not significantly altered with MMP2 deletion, other chemokines such as MCP 2–5 may be responsible for the increase in vein wall monocytes observed. Interestingly, the MMP9−/− + MMP2 inhibitor had a more exaggerated response with larger thrombi and more vein wall monocytes than the MMP2/9−/− as compared with MMP2−/− alone. This may be due to the fact that the MMP2 inhibitor, while specific,17 may have other effects on the vein wall injury as it is a long chain fatty acid with fibronectin binding sites, and may mimic the basement membrane of the vessel wall with alteration in monocyte influx and thrombus resolution.40
Targeting of MMPs has been evaluated in various models of cardiovascular injury and VT.11, 25, 41 While the deletion of MMP2 in these experiments correlates with diminished collagen at 8d, the significance of this effect is lost by 21 days. Thus, the role of MMP2 in the fibrotic response is temporally related to the duration of thrombus contact. Translationally, the timing and duration of MMP2 or MMP9 inhibition needs to guide future studies in treatment of PTS, and a practical means to reduce up-regulation of MMPs may be by limiting the thrombus-vein wall contact time via anticoagulation and pharmacomechanical therapies.4 More importantly, the cost of decreased fibrosis may be a larger thrombus (at least if MMP2 is inhibited).
Acknowledgments
Supported by: HL083918 and HL092129 (PKH), and T32HL092129 (TW)
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Lloyd-Jones D, Adams RJ, Brown TM, Carnethon M, Dai S, De Simone G, Ferguson TB, Ford E, Furie K, Gillespie C, Go A, Greenlund K, Haase N, Hailpern S, Ho PM, Howard V, Kissela B, Kittner S, Lackland D, Lisabeth L, Marelli A, McDermott MM, Meigs J, Mozaffarian D, Mussolino M, Nichol G, Roger V, Rosamond W, Sacco R, Sorlie P, Stafford R, Thom T, Wasserthiel-Smoller S, Wong ND, Wylie-Rosett J. Heart disease and stroke statistics--2010 update. A report from the american heart association. Circulation. 2009 doi: 10.1161/CIRCULATIONAHA.109.192667. [DOI] [PubMed] [Google Scholar]
- 2.Bergan JJ, Schmid-Schonbein GW, Smith PD, Nicolaides AN, Boisseau MR, Eklof B. Chronic venous disease. N Engl J Med. 2006;355:488–498. doi: 10.1056/NEJMra055289. [DOI] [PubMed] [Google Scholar]
- 3.Johnson BF, Manzo RA, Bergelin RO, Strandness DE., Jr Relationship between changes in the deep venous system and the development of the postthrombotic syndrome after an acute episode of lower limb deep vein thrombosis: A one- to six-year follow-up. J Vasc Surg. 1995;21:307–312. doi: 10.1016/s0741-5214(95)70271-7. discussion 313. [DOI] [PubMed] [Google Scholar]
- 4.Henke PK, Comerota AJ. An update on etiology, prevention, and therapy of postthrombotic syndrome. J Vasc Surg. 2011;53:500–509. doi: 10.1016/j.jvs.2010.08.050. [DOI] [PubMed] [Google Scholar]
- 5.Henke PK, Varma MR, Moaveni DK, Dewyer NA, Moore AJ, Lynch EM, Longo C, Deatrick CB, Kunkel SL, Upchurch GR, Jr, Wakefield TW. Fibrotic injury after experimental deep vein thrombosis is determined by the mechanism of thrombogenesis. Thromb Haemost. 2007;98:1045–1055. [PubMed] [Google Scholar]
- 6.Deatrick KB, Eliason JL, Lynch EM, Moore AJ, Dewyer NA, Varma MR, Pearce CG, Upchurch GR, Wakefield TW, Henke PK. Vein wall remodeling after deep vein thrombosis involves matrix metalloproteinases and late fibrosis in a mouse model. J Vasc Surg. 2005;42:140–148. doi: 10.1016/j.jvs.2005.04.014. [DOI] [PubMed] [Google Scholar]
- 7.Dahi S, Lee JG, Lovett DH, Sarkar R. Differential transcriptional activation of matrix metalloproteinase-2 and membrane type-1 matrix metalloproteinase by experimental deep venous thrombosis and thrombin. J Vasc Surg. 2005;42:539–545. doi: 10.1016/j.jvs.2005.04.051. [DOI] [PubMed] [Google Scholar]
- 8.Henke PK, Varma MR, Deatrick KB, Drewyer NA, Lynch EM, Moore AJ, Dubay DA, Sukheepod P, Pearce CG, Upchurch GR, Jr, Kunkel SL, Franz MG, Wakefield TW. Neutrophils modulate post-thrombotic vein wall remodeling but not thrombus neovascularization. Thromb Haemost. 2006;95:272–281. doi: 10.1160/TH05-02-0099. [DOI] [PubMed] [Google Scholar]
- 9.Ripplinger CM, Kessinger CW, Li C, Kim JW, McCarthy JR, Weissleder R, Henke PK, Lin CP, Jaffer FA. Inflammation modulates murine venous thrombosis resolution in vivo: Assessment by multimodal fluorescence molecular imaging. Arterioscler Thromb Vasc Biol. 2012;32:2616–2624. doi: 10.1161/ATVBAHA.112.251983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dewyer NA, Sood V, Lynch EM, Luke CE, Upchurch GR, Jr, Wakefield TW, Kunkel S, Henke PK. Plasmin inhibition increases mmp-9 activity and decreases vein wall stiffness during venous thrombosis resolution. J Surg Res. 2007;142:357–363. doi: 10.1016/j.jss.2007.03.064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sood V, Luke C, Miller E, Mitsuya M, Upchurch GR, Jr, Wakefield TW, Myers DD, Henke PK. Vein wall remodeling after deep vein thrombosis: Differential effects of low molecular weight heparin and doxycycline. Ann Vasc Surg. 2010;24:233–241. doi: 10.1016/j.avsg.2009.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Corry DB, Kiss A, Song LZ, Song L, Xu J, Lee SH, Werb Z, Kheradmand F. Overlapping and independent contributions of mmp2 and mmp9 to lung allergic inflammatory cell egression through decreased cc chemokines. FASEB J. 2004;18:995–997. doi: 10.1096/fj.03-1412fje. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Deatrick KB, Elfline M, Baker N, Luke CE, Blackburn S, Stabler C, Wakefield TW, Henke PK. Postthrombotic vein wall remodeling: Preliminary observations. J Vasc Surg. 2011;53:139–146. doi: 10.1016/j.jvs.2010.07.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Henke PK, Varga A, De S, Deatrick CB, Eliason J, Arenberg DA, Sukheepod P, Thanaporn P, Kunkel SL, Upchurch GR, Jr, Wakefield TW. Deep vein thrombosis resolution is modulated by monocyte cxcr2-mediated activity in a mouse model. Arterioscler Thromb Vasc Biol. 2004;24:1130–1137. doi: 10.1161/01.ATV.0000129537.72553.73. [DOI] [PubMed] [Google Scholar]
- 15.Henke PK, Pearce CG, Moaveni DM, Moore AJ, Lynch EM, Longo C, Varma M, Dewyer NA, Deatrick KB, Upchurch GR, Jr, Wakefield TW, Hogaboam C, Kunkel SL. Targeted deletion of ccr2 impairs deep vein thombosis resolution in a mouse model. J Immunol. 2006;177:3388–3397. doi: 10.4049/jimmunol.177.5.3388. [DOI] [PubMed] [Google Scholar]
- 16.Henke PK, Mitsuya M, Luke CE, Elfline MA, Baldwin JF, Deatrick KB, Diaz JA, Sood V, Upchurch GR, Wakefield TW, Hogaboam C, Kunkel SL. Toll-like receptor 9 signaling is critical for early experimental deep vein thrombosis resolution. Arterioscler Thromb Vasc Biol. 2011;31:43–49. doi: 10.1161/ATVBAHA.110.216317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Siu MK, Cheng CY. Interactions of proteases, protease inhibitors, and the beta1 integrin/laminin gamma3 protein complex in the regulation of ectoplasmic specialization dynamics in the rat testis. Biol Reprod. 2004;70:945–964. doi: 10.1095/biolreprod.103.023606. [DOI] [PubMed] [Google Scholar]
- 18.Sood V, Luke CE, Deatrick KB, Baldwin J, Miller EM, Elfline M, Upchurch GR, Jr, Wakefield TW, Henke PK. Urokinase plasminogen activator independent early experimental thrombus resolution: Mmp2 as an alternative mechanism. Thromb Haemost. 2010;104:1174–1183. doi: 10.1160/TH10-03-0184. [DOI] [PubMed] [Google Scholar]
- 19.Junqueira LC, Bignolas G, Brentani RR. Picrosirius staining plus polarization microscopy, a specific method for collagen detection in tissue sections. Histochem J. 1979;11:447–455. doi: 10.1007/BF01002772. [DOI] [PubMed] [Google Scholar]
- 20.Cuttle L, Nataatmadja M, Fraser JF, Kempf M, Kimble RM, Hayes MT. Collagen in the scarless fetal skin wound: Detection with picrosirius-polarization. Wound Repair Regen. 2005;13:198–204. doi: 10.1111/j.1067-1927.2005.130211.x. [DOI] [PubMed] [Google Scholar]
- 21.Baldwin JF, Sood V, Elfline MA, Luke CE, Dewyer NA, Diaz JA, Myers DD, Wakefield T, Henke PK. The role of urokinase plasminogen activator and plasmin activator inhibitor-1 on vein wall remodeling in experimental deep vein thrombosis. J Vasc Surg. 2012;56:1089–1097. doi: 10.1016/j.jvs.2012.02.054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Myers DD, Jr, Henke PK, Bedard PW, Wrobleski SK, Kaila N, Shaw G, Meier TR, Hawley AE, Schaub RG, Wakefield TW. Treatment with an oral small molecule inhibitor of p selectin (psi-697) decreases vein wall injury in a rat stenosis model of venous thrombosis. J Vasc Surg. 2006;44:625–632. doi: 10.1016/j.jvs.2006.05.021. [DOI] [PubMed] [Google Scholar]
- 23.Moaveni DK, Lynch EM, Luke C, Sood V, Upchurch GR, Wakefield TW, Henke PK. Vein wall re-endothelialization after deep vein thrombosis is improved with low-molecular-weight heparin. J Vasc Surg. 2008;47:616–624. doi: 10.1016/j.jvs.2007.11.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Parks WC, Wilson CL, Lopez-Boado YS. Matrix metalloproteinases as modulators of inflammation and innate immunity. Nat Rev Immunol. 2004;4:617–629. doi: 10.1038/nri1418. [DOI] [PubMed] [Google Scholar]
- 25.Galis ZS, Khatri JJ. Matrix metalloproteinases in vascular remodeling and atherogenesis: The good, the bad, and the ugly. Circ Res. 2002;90:251–262. [PubMed] [Google Scholar]
- 26.Cho A, Reidy MA. Matrix metalloproteinase-9 is necessary for the regulation of smooth muscle cell replication and migration after arterial injury. Circ Res. 2002;91:845–851. doi: 10.1161/01.res.0000040420.17366.2e. [DOI] [PubMed] [Google Scholar]
- 27.Zhang J, Nie L, Razavian M, Ahmed M, Dobrucki LW, Asadi A, Edwards DS, Azure M, Sinusas AJ, Sadeghi MM. Molecular imaging of activated matrix metalloproteinases in vascular remodeling. Circulation. 2008;118:1953–1960. doi: 10.1161/CIRCULATIONAHA.108.789743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Pepper MS. Role of the matrix metalloproteinase and plasminogen activator-plasmin systems in angiogenesis. Arterioscler Thromb Vasc Biol. 2001;21:1104–1117. doi: 10.1161/hq0701.093685. [DOI] [PubMed] [Google Scholar]
- 29.Singh I, Burnand KG, Collins M, Luttun A, Collen D, Boelhouwer B, Smith A. Failure of thrombus to resolve in urokinase-type plasminogen activator gene-knockout mice: Rescue by normal bone marrow-derived cells. Circulation. 2003;107:869–875. doi: 10.1161/01.cir.0000050149.22928.39. [DOI] [PubMed] [Google Scholar]
- 30.Johnson C, Galis ZS. Matrix metalloproteinase-2 and -9 differentially regulate smooth muscle cell migration and cell-mediated collagen organization. Arterioscler Thromb Vasc Biol. 2004;24:54–60. doi: 10.1161/01.ATV.0000100402.69997.C3. [DOI] [PubMed] [Google Scholar]
- 31.Kuzuya M, Kanda S, Sasaki T, Tamaya-Mori N, Cheng XW, Itoh T, Itohara S, Iguchi A. Deficiency of gelatinase a suppresses smooth muscle cell invasion and development of experimental intimal hyperplasia. Circulation. 2003;108:1375–1381. doi: 10.1161/01.CIR.0000086463.15540.3C. [DOI] [PubMed] [Google Scholar]
- 32.Johnson JL, Dwivedi A, Somerville M, George SJ, Newby AC. Matrix metalloproteinase (mmp)-3 activates mmp-9 mediated vascular smooth muscle cell migration and neointima formation in mice. Arterioscler Thromb Vasc Biol. 2011;31:e35–44. doi: 10.1161/ATVBAHA.111.225623. [DOI] [PubMed] [Google Scholar]
- 33.Castagnoli C, Stella M, Berthod C, Magliacani G, Richiardi PM. Tnf production and hypertrophic scarring. Cell Immunol. 1993;147:51–63. doi: 10.1006/cimm.1993.1047. [DOI] [PubMed] [Google Scholar]
- 34.Bienkowski RS, Gotkin MG. Control of collagen deposition in mammalian lung. Proc Soc Exp Biol Med. 1995;209:118–140. doi: 10.3181/00379727-209-43886a. [DOI] [PubMed] [Google Scholar]
- 35.Cummins PM, von Offenberg Sweeney N, Killeen MT, Birney YA, Redmond EM, Cahill PA. Cyclic strain-mediated matrix metalloproteinase regulation within the vascular endothelium: A force to be reckoned with. Am J Physiol Heart Circ Physiol. 2007;292:H28–42. doi: 10.1152/ajpheart.00304.2006. [DOI] [PubMed] [Google Scholar]
- 36.Ikonomidis JS, Gibson WC, Butler JE, McClister DM, Sweterlitsch SE, Thompson RP, Mukherjee R, Spinale FG. Effects of deletion of the tissue inhibitor of matrix metalloproteinases-1 gene on the progression of murine thoracic aortic aneurysms. Circulation. 2004;110:II-268–II-273. doi: 10.1161/01.CIR.0000138384.68947.20. [DOI] [PubMed] [Google Scholar]
- 37.Vaillant B, Chiaramonte MG, Cheever AW, Soloway PD, Wynn TA. Regulation of hepatic fibrosis and extracellular matrix genes by the th response: New insight into the role of tissue inhibitors of matrix metalloproteinases. J Immunol. 2001;167:7017–7026. doi: 10.4049/jimmunol.167.12.7017. [DOI] [PubMed] [Google Scholar]
- 38.Wynn TA, Barron L. Macrophages: Master regulators of inflammation and fibrosis. Semin Liver Dis. 2010;30:245–257. doi: 10.1055/s-0030-1255354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Myers DD, Jr, Wrobleski SK, Longo C, Bedard PW, Kaila N, Shaw GD, Londy FJ, Rohrer SE, Fex BA, Zajkowski PJ, Meier TR, Hawley AE, Farris DM, Ballard NE, Henke PK, Schaub RG, Wakefield TW. Resolution of venous thrombosis using a novel oral small-molecule inhibitor of p-selectin (psi-697) without anticoagulation. Thromb Haemost. 2007;97:400–407. [PubMed] [Google Scholar]
- 40.Berton A, Rigot V, Huet E, Decarme M, Eeckhout Y, Patthy L, Godeau G, Hornebeck W, Bellon G, Emonard H. Involvement of fibronectin type ii repeats in the efficient inhibition of gelatinases a and b by long-chain unsaturated fatty acids. J Biol Chem. 2001;276:20458–20465. doi: 10.1074/jbc.M011664200. [DOI] [PubMed] [Google Scholar]
- 41.Visse R, Nagase H. Matrix metalloproteinases and tissue inhibitors of metalloproteinases: Structure, function, and biochemistry. Circ Res. 2003;92:827–839. doi: 10.1161/01.RES.0000070112.80711.3D. [DOI] [PubMed] [Google Scholar]