Abstract
Background
Job strain is associated with an increased coronary heart disease risk, but few large-scale studies have examined the relationship of this psychosocial characteristic with the biological risk factors that potentially mediate the job strain – heart disease association.
Methodology and Principal Findings
We pooled cross-sectional, individual-level data from eight studies comprising 47,045 participants to investigate the association between job strain and the following cardiovascular disease risk factors: diabetes, blood pressure, pulse pressure, lipid fractions, smoking, alcohol consumption, physical inactivity, obesity, and overall cardiovascular disease risk as indexed by the Framingham Risk Score. In age-, sex-, and socioeconomic status-adjusted analyses, compared to those without job strain, people with job strain were more likely to have diabetes (odds ratio 1.29; 95% CI: 1.11–1.51), to smoke (1.14; 1.08–1.20), to be physically inactive (1.34; 1.26–1.41), and to be obese (1.12; 1.04–1.20). The association between job strain and elevated Framingham risk score (1.13; 1.03–1.25) was attributable to the higher prevalence of diabetes, smoking and physical inactivity among those reporting job strain.
Conclusions
In this meta-analysis of work-related stress and cardiovascular disease risk factors, job strain was linked to adverse lifestyle and diabetes. No association was observed between job strain, clinic blood pressure or blood lipids.
Introduction
Psychological stress at work, or job strain, has been shown to be moderately associated with an increased risk of coronary heart disease [1]–[4]. However, despite a series of studies, the association of this psychological characteristic with many cardiovascular risk factors remains unclear. While there is evidence that stress is linked to unfavourable levels of lifestyle factors, such as physical activity, smoking habits, alcohol consumption and weight control [5]–[8], its influence, if any, on biological risk factors, especially clinic blood pressure, blood lipids and blood glucose, remains controversial [9]–[18]. Many studies of stress biology are characterised by small sample sizes, single risk factor outcomes, and the use of heterogeneous measures of stress. If we are to understand risk management in people with job strain, larger studies which capture a wide range of risk factors are needed._ENREF_17 Accordingly, we conducted the largest study on this issue to date by pooling individual-level data from eight European studies comprising a total of 47,045 men and women.
Materials and Methods
Study population
We used data from eight independent studies, in which clinical examinations had been conducted between 1984 and 2003, in Belgium (Belstress [19]), Germany (HNR [20], KORA S1-S3 [21]), Sweden (WOLF-N [13], WOLF-S [22]) and the UK (Whitehall II [23]). All studies are part of the "Individual-Participant-Data Meta-analysis of Working Populations" (IPD-Work) Consortium established in 2008 [4]. Ethical approval for each constituent study in the IPD-Work consortium was obtained from the relevant local or national ethics committees and all participants gave informed consent to take part. Details of the design, recruitment, and ethical approval for the participating studies are described elsewhere and presented in Text S1.
Our analyses were based on 47,045 participants who were in employment at the time of the assessment and underwent a clinical examination. We excluded 4394 (8.5%) participants with missing information on sex, age, or job strain, or with a history of myocardial infarction (data on prevalent myocardial infarction was not available from KORA).
Assessment of job strain
Job strain was measured in all studies using questions from the Job Content Questionnaire and Demand-Control Questionnaire [24]. Briefly, enquiries were made about the psychosocial aspects of study members’ job. For each participant, mean response scores were calculated for job demands items and job control items. High job demands were defined as a score in this domain that was higher than the study-specific median score; low job control was defined as a score in this domain that was lower than the study-specific median score. Job strain was then denoted by high demands and low control and, for the purposes of analyses, compared to all other combinations (no strain). We have previously published a detailed description of this job strain measure, including its validation and harmonization, as part of this collaboration [25].
Assessment of demographic characteristics
Socioeconomic status (SES) was based on occupational position obtained from employers' or other registers, or participant-completed questionnaires. SES was categorized into low, intermediate or high. Participants who were self-employed or who had missing data on job title were included in the analyses in the "other" SES category. We also identified respondents who worked in shifts.
Assessment of cardiovascular disease risk factors
Participants underwent a clinical examination where their height, weight, and blood pressure were measured; a blood sample was also taken. Body mass index (BMI) was calculated as weight in kilograms divided by height in meters squared and, based on World Health Organization (WHO) guidance, obesity was defined as a BMI of ≥ 30 kg/m2 [26]. Hypertension was denoted by as systolic (diastolic) blood pressure of at least 140 (90) mmHg, or use of antihypertensive medication. Total and HDL-cholesterol levels were measured in all studies, but triglyceride values were only available in four (HNR, WOLF N, WOLF S and Whitehall II). Blood cholesterol ratio was defined as the total divided by HDL cholesterol. Diabetes and the use of antihypertensive or lipid-lowering medication were based on self-report. In the Whitehall II study, diabetes was additionally measured by 2-h oral glucose tolerance test [27]. In addition to these standard risk factors, we assessed pulse pressure, computed as systolic minus the diastolic blood pressure, because high pulse pressure is an independent correlate of atherosclerosis [28].
We extracted data on smoking, alcohol use, and physical inactivity from standard questionnaires completed by participants in all studies. While there were inevitably some differences in the questions used to ascertain levels of smoking, alcohol intake and physical activity across studies, we were able to harmonise these data [5]–[7]. In general, the enquiries used are standard and have shown sufficiently high agreement with objective measures of these behaviours to justify their use in large, population-based surveys [29]–[32]. Smoking status was dichotomized (current smoker or non-smoker) [6]. Alcohol use was requested by questions on the total number of alcoholic drinks, by type of drink, which the participants consumed in a week. One drink was defined as approximately equivalent to one unit or one glass of alcoholic drink or 10 g of ethanol. Alcohol use was categorized as none, moderate use (1–15 and 1–22 units of alcohol per week in women and men, respectively) or greater [7]. The questions used to assess leisure-time physical activity differed between studies. Some studies had only questions on sports activities and exercise, while for other studies information was also available for other types of leisure-time physical activities, such as walking and cycling. Participants were denoted as being physically inactive if they reported none or very little moderate or vigorous leisure-time physical activity or exercise [5]. As expected, smoking and physical inactivity were associated with incident coronary heart disease in IPD-Work [33].
To assess overall cardiovascular disease risk, we constructed the Framingham cardiovascular disease risk score on the basis of age, total cholesterol, HDL cholesterol, systolic blood pressure, hypertensive medication use, smoking and diabetes status. Following clinical guidelines, “high” overall risk was defined as a Framingham score of 20% or higher [34].
Data analysis
Individual-level data from the studies were pooled into one dataset. The associations between job strain and CVD risk factors were analyzed using mixed effects linear and logistic regression models with the study as the random effect. In these analyses, triglyceride values were logarithmically transformed due to their skewed distribution. Measures of association were adjusted for sex and age, and additionally for SES. In the main analysis, we excluded participants who reported use of antihypertensive medication when the outcome was diastolic or systolic blood pressure or pulse pressure, and participants who reported the use of lipid-lowering medication when the outcome was any measure of cholesterol or triglycerides although a sensitivity analysis was conducted including these participants. In further analyses of statistically significant job strain-risk factor associations, multiple multivariable adjustments were undertaken to examine the robustness of each association. Because shift or night time work has been found to be a strong predictor of the metabolic syndrome [35], the job strain-diabetes association was repeated excluding participants who had shift or night time work. SAS statistical software, version 9.2, was used for all statistical analyses.
Results
The basic characteristics of the participants according to each study are presented in Table 1 . Mean age was 45.1 years and 29.2% of the study members were women. Table 2 shows age- and sex-adjusted associations between job strain and various risk factors. Compared to participants without job strain, those reporting job strain were 35% more likely to have diabetes (odds ratio 1.35, 95% confidence interval 1.15, 1.57). These associations were little changed after additional adjustment for SES. Job strain was associated with several lifestyle variables, such as physical inactivity (1.43, 95% CI 1.36, 1.51), current smoking (1.23, 95% CI 1.16, 1.30), alcohol abstinence (1.21, 95% CI 1.13, 1.30) and obesity (1.19, 95% CI 1.11, 1.28).
Table 1. Participant Characteristics According to Study, the IPD-Work Consortium, 1984–2003.
| Study | Baseline | N | Age (SD), y | Women (%) | Job strain (%) |
| Belstress [19] | 1994–1998 | 20,692 | 45.4 (5.9) | 4909 (23.7) | 3900 (18.9) |
| Heinz-Nixdorf Recall [20] | 2000–2003 | 1776 | 53.3 (4.8) | 736 (41.4) | 217 (12.2) |
| KORA Survey 1 [21] | 1984–1985 | 2460 | 42.3 (10.2) | 864 (35.1) | 483 (19.6) |
| KORA Survey 2 [21] | 1989–1990 | 2370 | 42.3 (10.6) | 896 (37.8) | 417 (17.6) |
| KORA Survey 3 [21] | 1994–1995 | 2345 | 42.6 (10.4) | 953 (40.6) | 372 (15.9) |
| WOLF Norrland [13] | 1996–1998 | 4678 | 44.0 (10.3) | 780 (16.7) | 599 (12.8) |
| WOLF Stockholm [22] | 1992–1995 | 5654 | 41.5 (11.0) | 2447 (43.3) | 917 (16.2) |
| Whitehall II [23] | 1991–1993 | 7070 | 48.8 (5.7) | 2168 (30.7) | 959 (13.6) |
| Pooled data | 1984–2003 | 47,045 | 45.1 (8.4) | 13,753 (29.2) | 7864 (16.7) |
Table 2. Association Between Job Strain and Biological and Lifestyle Risk Factors, the IPD-Work Consortium, 1984–2003.
| Mean (SE) § | |||||
| Total N | No strain | Job strain | Mean difference (95% CI)§ | Mean difference (95% CI)# | |
| Biological risk factors | |||||
| Systolic blood pressure, mmHg* | 44,106 | 126.8 (1.6) | 126.8 (1.6) | 0.01 (–0.35, 0.38) | –0.01 (–0.38, 0.36) |
| Diastolic blood pressure, mmHg* | 44,104 | 79.5 (1.1) | 79.5 (1.1) | –0.04 (–0.28, 0.21) | 0.01 (–0.24, 0.26) |
| Pulse pressure, mmHg * | 44,104 | 47.3 (1.2) | 47.3 (1.2) | 0.05 (–0.21, 0.31) | –0.02 (–0.28, 0.24) |
| Total cholesterol, mmol/l † | 45,776 | 5.87 (0.1) | 5.89 (0.1) | 0.01 (–0.01, 0.04) | 0.01 (–0.02, 0.04) |
| HDL, mmol/l † | 45,728 | 1.42 (0.01) | 1.41 (0.01) | –0.01 (–0.02, –0.00) | –0.001 (–0.01, 0.01) |
| Cholesterol ratio † | 45,723 | 4.5 (0.1) | 4.6 (0.1) | 0.04 (0.00, 0.09) | 0.01 (–0.03, 0.06) |
| Triglycerides, mmol/l † | 18,858 | 1.4 (0.1) | 1.4 (0.1) | 0.01 (–0.01, 0.04) | –0.001 (–0.02, 0.02) |
| Prevalence (%) § | Odds ratio (95% CI) § | Odds ratio (95% CI)# | |||
| Hypertension | 47,045 | 30.4 | 30.1 | 0.99 (0.94, 1.05) | 0.99 (0.93, 1.04) |
| Diabetes | 46,510 | 2.2 | 2.8 | 1.35 (1.15, 1.57) | 1.29 (1.11, 1.51) |
| Lifestyle risk factors | |||||
| Smoking | 46,553 | 26.6 | 30.7 | 1.23 (1.16, 1.30) | 1.14 (1.08, 1.20) |
| Non-drinking | 46,482 | 16.5 | 19.3 | 1.21 (1.13, 1.30) ‡ | 1.11 (1.04, 1.19) |
| High alcohol use | 46,482 | 21.6 | 21.6 | 1.06 (0.99, 1.13) ‡ | 1.06 (0.99, 1.14) |
| Physical inactivity | 46,395 | 31.7 | 38.7 | 1.43 (1.36, 1.51) | 1.34 (1.26, 1.41) |
| Obesity | 46,891 | 13.7 | 15.7 | 1.19 (1.11, 1.28) | 1.12 (1.04, 1.20) |
| Overall cardiovascular risk | |||||
| Framingham risk ≥20 | 45,428 | 9.6 | 9.9 | 1.19 (1.08, 1.31) | 1.13 (1.03, 1.25) |
Participants not using antihypertensive medication.
Participants not using lipid-lowering medication.
Compared to moderate drinkers only.
Age- and sex-adjusted.
#Age-, sex-, and SES-adjusted.
Table 2 also shows that in the age-, sex-, and SES-adjusted analyses, there were no differences between people with and without job strain for systolic or diastolic blood pressure, pulse pressure, cholesterol or triglyceride values. These findings were unchanged in sensitivity analyses: No associations of job strain with blood pressure and blood cholesterol were observed after including participants treated with antihypertensive and lipid-lowering drugs in the analysis: age-, sex- and SES-adjusted mean difference in systolic blood pressure and total cholesterol 0.08 (95% confidence interval –0.29, 0.45) mmHg and 0.01 (95% confidence interval –0.01, 0.04) mmol/L between those with and without job strain, respectively. This was also the case after adding a constant of 10 mmHg to systolic blood pressure values among participants on antihypertensive treatment (adjusted difference 0.12, 95% confidence interval –0.26, 0.50 mmHg) and a constant of 2 mmol/L to total cholesterol values among participants on lipid-lowering treatment (adjusted difference 0.01, 95% confidence interval –0.01, 0.04 mmol/L) (N = 46,991 and 46,659 in these analyses) [36].
Job strain was associated with a slightly higher overall cardiovascular disease risk (1.19, 95% CI 1.08, 1.31), as indicated by a Framingham risk ≥20%; this association was due to the higher prevalence of physical inactivity, smoking and diabetes among participants with job strain (odds ratio after adjusting for these factors: 1.03, 95% CI 0.92, 1.16).
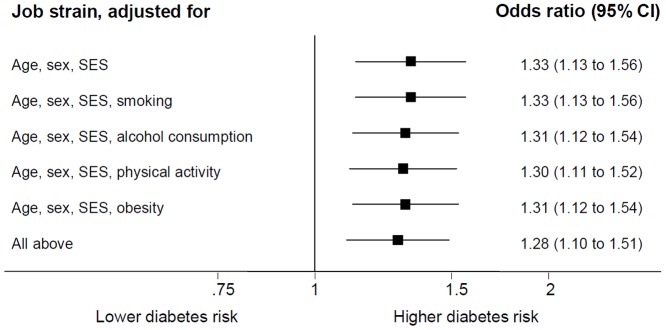
In figure 1 we present results from the multivariable adjusted analyses for the job strain-diabetes association. The age-, sex- and SES-adjusted association was little attenuated after additional adjustment for smoking, alcohol consumption, physical inactivity and obesity, suggesting that the association is not explained by lifestyle factors.Sex-specific analyses showed little difference in the associations of job strain with diabetes (age- and SES-adjusted odds ratio 1.21, 95% CI 1.00, 1.46 in men and 1.48, 95% CI 1.12, 1.97 in women). No significant interaction effect between sex and job strain was found for diabetes (P = 0.18) either. The exclusion of the shift and night workers only slightly attenuated the age-, sex and SES-adjusted odds ratio (1.20, 95% CI 0.99, 1.45).
Figure 1. Adjusted Odds Ratios (95% CI) for the Association Between Job Strain and Diabetes (N = 44,818 in All Models), the IPD-Work Consortium, 1984–2003.
Discussion
Meta-analysis of individual participant data from over 47,000 participants showed that persons with job strain had higher prevalence of diabetes. This association was robust to adjustment for smoking, alcohol consumption, physical inactivity and obesity, suggesting that it is not explained by poorer lifestyle among persons reporting job strain. Contrary to popular opinion, we found no clinically relevant differences in lipid levels, clinic blood or pulse pressure or prevalence of hypertension between participants with or without job strain.
We used a pre-defined measure of job strain which was harmonised before the inclusion and analysis of risk factors, excluding bias arising from post hoc exposure definition [25]. Furthermore, the job strain measure has been shown to be associated with subsequent coronary heart disease in this dataset [4], suggesting that imprecise measurement, present when capturing any self-reported variable, is an unlikely explanation for the absence of associations with some of the biological factors. The associations with lifestyle factors in this analysis of 8 studies with biological data corresponded to our findings reported for the entire IPD-Consortium of >140,000 men and women [5]–[8]. A limitation of our study is that it is not based on a systematic review of all available data in the field. Also, we cannot draw causal inference due to the non-randomised nature of the utilised data. These points notwithstanding, a causal association is unlikely if no cross-sectional association is observed.
The key mediators of the association between job strain and cardiovascular diseases have long been debated. Our findings are in agreement with the view that job strain affects disease risk via poor health behaviors, and by increasing risk of diabetes. A previous report using longitudinal data from the IPD-Work consortium has shown that job strain predicts physical inactivity more strongly than physical inactivity predicts job strain [5]. This is consistent with the expected causal direction of the association. The evidence on the temporal nature of the association between job strain, obesity, smoking and drinking patterns is less clear. It is possible that the associations are bidirectional and partially explained by common causes [6]–[8].
An alternative hypothesis is that job strain affects the development of cardiovascular diseases by directly altering standard biological risk factors. Our analyses provide limited support for this view as we found no evidence of a consistent association between job strain and most of the cardiovascular disease risk factors. Our findings of the absence of a relation between resting blood pressure and hypertension are concordant with several previous studies in this field [13], [16], [37], although this is not a universal finding and does not apply to findings on ambulatory blood pressure [9], [10], [38], [39]. Similarly, the present results are in agreement with earlier studies which have concluded that job strain is not associated with cholesterol [13], [37], [38], [40], although, again, the literature is discordant [11], [41].
Our results show job strain to be related to increased risk of diabetes. This association was present in age- and sex-adjusted models, and after adjustment for SES and measures of health behavior. Furthermore, the association between job strain and diabetes was somewhat stronger in women than men, in accordance with other evidence [18], [42], [43]. Our findings support the possibility that job strain contributes to disturbances in glucose metabolism leading to a raised risk of diabetes. However, given the cross-sectional nature of these data, we cannot exclude the possibility that a chronic condition, such as diabetes, affected perceptions of job strain.
In principle, stress could simultaneously affect multiple risk factors, rather than a particular risk factor, and thus increase the risk of cardiovascular diseases. To test this possibility, we assessed the overall risk using a validated multifactorial risk algorithm, the Framingham score, comprising age, total cholesterol, HDL-cholesterol, systolic blood pressure, hypertensive medication use, smoking, and diabetes status [34], [44]. We found job strain to be associated with elevated Framingham risk, although this association was attributable to the combination of poor lifestyle and increased diabetes prevalence among those with job strain.
These results suggest that job strain links to cardiovascular disease risk mostly via lifestyle factors and hyperglycemia. Our findings provide strong evidence against the common belief that job strain increases resting blood pressure. Similarly, we found no evidence to suggest that job strain is associated with pulse pressure. However, there is a range of other potential biological stress mediators to be assessed in future studies: chronic inflammation (e.g., interleukin 6) [45], blood coagulation factors, and increased risk of stress response that act as a trigger of cardiac events among individuals with undiagnosed advanced atherosclerosis. It has also been suggested that non-dipping blood pressure is more prevalent among individuals with job strain [46], [47].
Our findings are based on a large number of participants, providing sufficient power to detect relatively small effects and also to confirm the absence of an association. The study covers a wide range of risk factors and a measure of overall cardiovascular risk; and it is the first to use an individual participant meta-analysis methodology to examine the association between job strain and risk factors. These data suggest that risk management among people with job strain should focus on glucose levels and lifestyle factors. The main emphasis of future mechanistic investigations of job strain and cardiovascular disease risk should be placed on examining diabetes and lifestyle factors rather than standard cardiovascular risk factors.
Supporting Information
Studies and participants.
(DOC)
PRISMA Checklist.
(DOC)
Funding Statement
This work is supported by the European Union New OSH ERA research programme (funded by the Finnish Work Environment Fund, Finland, the Swedish Council for Working Life and Social Research, Sweden, the German Social Accident Insurance, Germany, the Danish National Research Centre for the Working Environment, Denmark), the Academy of Finland (grant number 132944), the BUPA Foundation (grant number 22094477), and the British Heart Foundation (BHF), UK. The HNR was funded by the Heinz Nixdorf Foundation, Germany, German Ministry of Education and Science and the German Research Foundation. The German National Accident Insurance supports analyses in the frame of the OSH ERA project. MK is supported by the Medical Research Council, UK (K013351), and the US National Institutes of Health (R01HL036310, R01AG034454) and a professorial fellowship from the Economic and Social Research Council, UK. GDB was a Wellcome Trust Fellow during the preparation of this manuscript. AS is a BHF professor. Funding bodies for participating cohort studies are listed on their websites. The study was conducted independently of funding agencies. None of the funding agencies played an active role in the preparation, review, or editing of this manuscript.
References
- 1. Belkic KL, Landsbergis PA, Schnall PL, Baker D (2004) Is job strain a major source of cardiovascular disease risk? Scand J Work Environ Health 30: 85–128. [DOI] [PubMed] [Google Scholar]
- 2. Kivimäki M, Virtanen M, Elovainio M, Kouvonen A, Väänänen A, et al. (2006) Work stress in the etiology of coronary heart disease—a meta-analysis. Scand J Work Environ Health 32: 431–442. [DOI] [PubMed] [Google Scholar]
- 3. Steptoe A, Kivimaki M (2012) Stress and cardiovascular disease. Nature reviews Cardiology 9: 360–370. [DOI] [PubMed] [Google Scholar]
- 4. Kivimäki M, Nyberg ST, Batty GD, Fransson EI, Heikkilä K, et al. (2012) Job strain as a risk factor for coronary heart disease: a collaborative meta-analysis of individual participant data. Lancet 380: 1491–1497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Fransson EI, Heikkila K, Nyberg ST, Zins M, Westerlund H, et al. (2012) Job Strain as a Risk Factor for Leisure-Time Physical Inactivity: An Individual-Participant Meta-Analysis of Up to 170,000 Men and Women: The IPD-Work Consortium. Am J Epidemiol 176: 1078–1089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Heikkilä K, Nyberg ST, Fransson EI, Alfredsson L, De Bacquer D, et al. (2012) Job Strain and Tobacco Smoking: An Individual-Participant Data Meta-Analysis of 166 130 Adults in 15 European Studies. PLoS One 7: e35463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Heikkilä K, Nyberg ST, Fransson EI, Alfredsson L, De Bacquer D, et al. (2012) Job Strain and Alcohol Intake: A Collaborative Meta-Analysis of Individual-Participant Data from 140 000 Men and Women. PLoS One 7: e40101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Nyberg ST, Heikkilä K, Fransson EI, Alfredsson L, De Bacquer D, et al. (2012) Job strain in relation to body mass index: pooled analysis of 160 000 adults from 13 cohort studies. J Intern Med 272: 65–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Landsbergis PA, Schnall PL, Warren K, Pickering TG, Schwartz JE (1994) Association between ambulatory blood pressure and alternative formulations of job strain. Scand J Work Environ Health 20: 349–363. [DOI] [PubMed] [Google Scholar]
- 10. Schnall PL, Schwartz JE, Landsbergis PA, Warren K, Pickering TG (1998) A longitudinal study of job strain and ambulatory blood pressure: results from a three-year follow-up. Psychosom Med 60: 697–706. [DOI] [PubMed] [Google Scholar]
- 11. Kivimäki M, Leino-Arjas P, Luukkonen R, Riihimäki H, Vahtera J, et al. (2002) Work stress and risk of cardiovascular mortality: prospective cohort study of industrial employees. BMJ 325: 857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Rosenthal T, Alter A (2012) Occupational stress and hypertension. J Am Soc Hypertens 6: 2–22. [DOI] [PubMed] [Google Scholar]
- 13. Alfredsson L, Hammar N, Fransson E, de Faire U, Hallqvist J, et al. (2002) Job strain and major risk factors for coronary heart disease among employed males and females in a Swedish study on work, lipids and fibrinogen. Scand J Work Environ Health 28: 238–248. [DOI] [PubMed] [Google Scholar]
- 14. Mezuk B, Kershaw KN, Hudson D, Lim KA, Ratliff S (2011) Job Strain, Workplace Discrimination, and Hypertension among Older Workers: The Health and Retirement Study. Race Soc Probl 3: 38–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Laflamme N, Brisson C, Moisan J, Milot A, Masse B, et al. (1998) Job strain and ambulatory blood pressure among female white-collar workers. Scand J Work Environ Health 24: 334–343. [DOI] [PubMed] [Google Scholar]
- 16. Kang MG, Koh SB, Cha BS, Park JK, Baik SK, et al. (2005) Job stress and cardiovascular risk factors in male workers. Prev Med 40: 583–588. [DOI] [PubMed] [Google Scholar]
- 17. Cosgrove MP, Sargeant LA, Caleyachetty R, Griffin SJ (2012) Work-related stress and Type 2 diabetes: systematic review and meta-analysis. Occup Med 62: 167–173. [DOI] [PubMed] [Google Scholar]
- 18. Heraclides AM, Chandola T, Witte DR, Brunner EJ (2012) Work stress, obesity and the risk of type 2 diabetes: gender-specific bidirectional effect in the Whitehall II study. Obesity 20: 428–433. [DOI] [PubMed] [Google Scholar]
- 19. De Bacquer D, Pelfrene E, Clays E, Mak R, Moreau M, et al. (2005) Perceived job stress and incidence of coronary events: 3-year follow-up of the Belgian Job Stress Project cohort. Am J Epidemiol 161: 434–441. [DOI] [PubMed] [Google Scholar]
- 20. Stang A, Moebus S, Dragano N, Beck EM, Mohlenkamp S, et al. (2005) Baseline recruitment and analyses of nonresponse of the Heinz Nixdorf Recall Study: identifiability of phone numbers as the major determinant of response. Eur J Epidemiol 20: 489–496. [DOI] [PubMed] [Google Scholar]
- 21. Holle R, Happich M, Lowel H, Wichmann HE (2005) KORA—a research platform for population based health research. Gesundheitswesen 67 Suppl 1S19–25. [DOI] [PubMed] [Google Scholar]
- 22. Peter R, Alfredsson L, Hammar N, Siegrist J, Theorell T, et al. (1998) High effort, low reward, and cardiovascular risk factors in employed Swedish men and women: baseline results from the WOLF Study. J Epidemiol Community Health 52: 540–547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Marmot MG, Smith GD, Stansfeld S, Patel C, North F, et al. (1991) Health inequalities among British civil servants: the Whitehall II study. Lancet 337: 1387–1393. [DOI] [PubMed] [Google Scholar]
- 24.Karasek R, Theorell T (1990) Healthy work : stress, productivity, and the reconstruction of working life. New York: Basic Books. [Google Scholar]
- 25. Fransson EI, Nyberg ST, Heikkila K, Alfredsson L, De Bacquer D, et al. (2012) Comparison of alternative versions of the job demand-control scales in 17 European cohort studies: the IPD-Work consortium. BMC Public Health 12: 62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.World Health Organization (2000) Obesity: preventing and managing the global epidemic. Report of a WHO consultation. World Health Organ Tech Rep Ser 894:: i-xii, 1–253. [PubMed] [Google Scholar]
- 27. Alberti KG, Zimmet PZ (1998) Definition, diagnosis and classification of diabetes mellitus and its complications. Part 1: diagnosis and classification of diabetes mellitus provisional report of a WHO consultation. Diabet Med 15: 539–553. [DOI] [PubMed] [Google Scholar]
- 28. Matthews KA, Owens JF, Kuller LH, Sutton-Tyrrell K, Lassila HC, et al. (1998) Stress-induced pulse pressure change predicts women's carotid atherosclerosis. Stroke 29: 1525–1530. [DOI] [PubMed] [Google Scholar]
- 29. Shaper AG, Pocock SJ, Ashby D, Walker M, Whitehead TP (1985) Biochemical and haematological response to alcohol intake. Annals of Clinical Biochemistry 22 (Pt 1): 50–61. [DOI] [PubMed] [Google Scholar]
- 30. Assaf AR, Parker D, Lapane KL, McKenney JL, Carleton RA (2002) Are there gender differences in self-reported smoking practices? Correlation with thiocyanate and cotinine levels in smokers and nonsmokers from the Pawtucket Heart Health Program. J Womens Health 11: 899–906. [DOI] [PubMed] [Google Scholar]
- 31. Pereira MA, FitzerGerald SJ, Gregg EW, Joswiak ML, Ryan WJ, et al. (1997) A collection of Physical Activity Questionnaires for health-related research. Med Sci Sport Exer 29: S1–205. [PubMed] [Google Scholar]
- 32. Hamer M, Kivimaki M, Steptoe A (2012) Longitudinal patterns in physical activity and sedentary behaviour from mid-life to early old age: a substudy of the Whitehall II cohort. J Epidemiol Community Health 66: 1110–1115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kivimaki M, Nyberg ST, Fransson EI, Heikkila K, Alfredsson L, et al.. (2013) Associations of job strain and lifestyle risk factors with risk of coronary artery disease: a meta-analysis of individual participant data. CMAJ [Epub ahead of print]. [Google Scholar]
- 34. D'Agostino RB Sr, Vasan RS, Pencina MJ, Wolf PA, Cobain M, et al. (2008) General cardiovascular risk profile for use in primary care: the Framingham Heart Study. Circulation 117: 743–753. [DOI] [PubMed] [Google Scholar]
- 35. De Bacquer D, Van Risseghem M, Clays E, Kittel F, De Backer G, et al. (2009) Rotating shift work and the metabolic syndrome: a prospective study. Int J Epidemiol 38: 848–854. [DOI] [PubMed] [Google Scholar]
- 36. Kivimaki M, Shipley MJ, Ferrie JE, Singh-Manoux A, Batty GD, et al. (2008) Best-practice interventions to reduce socioeconomic inequalities of coronary heart disease mortality in UK: a prospective occupational cohort study. Lancet 372: 1648–1654. [DOI] [PubMed] [Google Scholar]
- 37. Netterstrom B, Kristensen TS, Damsgaard MT, Olsen O, Sjol A (1991) Job strain and cardiovascular risk-factors - a cross-sectional study of employed Danish men and women. Brit J Ind Med 48: 684–689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Soderberg M, Rosengren A, Hillstrom J, Lissner L, Toren K (2012) A cross-sectional study of the relationship between job demand-control, effort-reward imbalance and cardiovascular heart disease risk factors. BMC Public Health 12: 1102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Landsbergis PA, Dobson M, Koutsouras G, Schnall P (2013) Job strain and ambulatory blood pressure: a meta-analysis and systematic review. Am J Public Health 103: e61–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Tsutsumi A, Kayaba K, Ishikawa S, Gotoh T, Nago N, et al. (2003) Job characteristics and serum lipid profile in Japanese rural workers: the Jichi Medical School Cohort Study. J Epidemiol 13: 63–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Eaker ED, Sullivan LM, Kelly-Hayes M, D'Agostino RB Sr, Benjamin EJ (2004) Does job strain increase the risk for coronary heart disease or death in men and women? The Framingham Offspring Study. Am J Epidemiol 159: 950–958. [DOI] [PubMed] [Google Scholar]
- 42. Heraclides A, Chandola T, Witte DR, Brunner EJ (2009) Psychosocial stress at work doubles the risk of type 2 diabetes in middle-aged women: evidence from the Whitehall II study. Diabetes care 32: 2230–2235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Leynen F, Moreau M, Pelfrene E, Clays E, De Backer G, et al. (2003) Job stress and prevalence of diabetes: results from the Belstress study. Archives of Public Health 61: 75–90. [Google Scholar]
- 44. Mosca L, Appel LJ, Benjamin EJ, Berra K, Chandra-Strobos N, et al. (2004) Evidence-based guidelines for cardiovascular disease prevention in women. Circulation 109: 672–693. [DOI] [PubMed] [Google Scholar]
- 45. Interleukin-6 Receptor Mendelian Randomisation Analysis (IL6R MR) Consortium (2012) The interleukin-6 receptor as a target for prevention of coronary heart disease: a mendelian randomisation analysis. Lancet 379: 1214–1224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Clays E, Van Herck K, De Buyzere M, Kornitzer M, Kittel F, et al. (2011) Behavioural and psychosocial correlates of nondipping blood pressure pattern among middle-aged men and women at work. J Hum Hypertens 26: 381–7. [DOI] [PubMed] [Google Scholar]
- 47. Fan L, Blumenthal JA, Hinderliter AL, Sherwood A (2013) The effect of job strain on nighttime blood pressure dipping among men and women with high blood pressure. Scand J Work Environ Health 39: 112–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Studies and participants.
(DOC)
PRISMA Checklist.
(DOC)


