Abstract
Objectives
To provide a measure of perceived stress that is psychometrically superior to existing instruments and novel in dimensionality.
Design
At 4-week intervals over 48 weeks, patients with multiple sclerosis (N = 138) completed 26 items from the Perceived Stress Scale (PSS) and the Perceived Stress Questionnaire (PSQ).
Results
Extant factor analytic models of the PSS fit poorly. A new measure using nine PSS and PSQ items, the Brief Inventory of Perceived Stress (BIPS), demonstrated good fit, construct validity, and stability with 3 factors: Lack of Control, Pushed, and Conflict and Imposition.
Conclusions
Items commonly used to measure perceived stress may have a more sophisticated underlying structure than previously thought. The BIPS's multidimensionality and longitudinal stability offer potential benefits in conceptualization and outcome prediction.
Keywords: perceived stress, factor analysis, psychometric properties, stress appraisal, factorial invariance, measurement
Early research on stress typically adopted models assuming that events themselves serve as the causal agent behind pathology, illness, maladaptive behavior, and other unhealthy outcomes. In contrast to environmental models, psychological models of stress have emphasized the perception of threat in response to specific environmental demands, coupled with a second-order appraisal of one's ability to cope with the demand (Benight & Bandura, 2004; Lazarus, 1999; Lazarus & Folkman, 1984). Despite agreement around this general conceptualization, from which the construct of “perceived stress” emerged (Cohen, Kessler, & Gordon, 1995), the critical constructs underlying perceived stress have been more challenging to identify.
Approaching this challenge, Cohen and colleagues (Cohen, Kamarck, & Mermelstein, 1983; Cohen & Williamson, 1988) developed the Perceived Stress Scale (PSS) to assess the extent to which individuals globally find their lives to be unpredictable, uncontrollable, and overloaded. Factor analyses tended to find two factors, one reflecting unpredictable-uncontrollable-overloaded appraisals, and another seeming to tap into confidence in executing an appropriate coping response (e.g., Golden-Kreutz, Browne, Frierson, & Andersen, 2004; Sharp, Kimmel, Kee, Saltoun, & Chang, 2007). Although their factor analyses indicated the presence of two factors, some of these researchers attributed the separation between these two factors to semantic (i.e., positively vs. negatively worded items), rather than conceptual differences (Cohen & Williamson, 1988; González Ramírez & Landero Hernández, 2007; Mimura & Griffiths, 2008; Siqueira Reis, Ferreira Hino, & Rodriguez-Añez, 2010). Thus, subsequent research using the Perceived Stress Scale (PSS) has overwhelming treated perceived stress as a monolithic construct.
An alternative approach to understanding the dimensionality of perceived stress was proposed by Levenstein and colleagues, who developed the Perceived Stress Questionnaire (PSQ; Levenstein et al., 1993) by selecting items tapping potential cognitive, emotional, and symptomatic sequelae of stressful events. Because they viewed affect and psychosomatic conditions—e.g., feeling rested, feeling discouraged, being lighthearted—as triggers of subsequent symptomatology and reflective of perceived stress, rather than as symptoms themselves, the dimensions of perceived stress underlying the PSQ differ from the PSS. Psychometric studies have found a variety of factors reflected in the PSQ, including worries, tension, joy, demands, and fatigue (Fliege et al., 2005; Levenstein et al., 1993).
The PSQ and the PSS both show strengths in predicting physiological (Cohen & Williamson, 1988; Fliege et al., 2005; Levenstein et al., 1993; Remor, Penedo, Shen, & Schneiderman, 2007) and psychological (Cohen et al., 1983; Crowe et al., 2011; Levenstein et al., 1993; Pedrelli, Feldman, Vorono, Fava, & Petersen, 2008) outcomes that one would expect to follow from stress. What remains unanswered, however, is why the stories they tell about the constructs underlying perceived stress appear to be so different. The lack of a clear answer to this question suggests that further investigation of the dimensionality of perceived stress is warranted. A better understanding of what is actually being measured can help elucidate the reasons why perceived stress is such a potent predictor of pathology, and whether this relationship is a consequence of global or specific aspects of stress appraisal.
The Current Study
We sought to better understand the factors underlying perceived stress. Items designed to measure this construct were administered every 4 weeks (13 times total) to participants diagnosed with multiple sclerosis (MS). These items included the entire PSS as well as 16 items drawn from the PSQ that were selected to avoid confounding with symptoms of chronic illness (e.g., fatigue) or psychopathology (e.g., anhedonia), as these constructs are common endpoints in stress research.
This approach permitted comparisons of the dimensions of perceived stress offered by several alternate models. A priori, we aimed to use confirmatory factor analysis (CFA) to replicate the one-dimensional and two-dimensional solutions to the PSS described above and determine their validity in our population. Next, exploratory factor analysis (EFA) of the 10-item PSS permitted us to see if the solutions reported in previous studies were the most appropriate ones for our population.
Finally, we aimed to construct a new measure of perceived stress with improved breadth and structural validity, by deriving a novel solution using the combined 26-item set of indicators. To examine the validity of these different solutions, we compared correlations between the factor-derived subscales and constructs relevant to concurrent validity (i.e., depressive and anxiety symptoms, health services utilization, stressful events) across the different models. We also examined stability of the competing models over time.
Methods
Participants
Participants were 138 individuals in a trial examining the effects of a stress management program on neuroimaging markers of disease activity in MS (Mohr et al., in press). Participants were recruited through neurology clinics and local chapters of the National Multiple Sclerosis Society. Eligible patients satisfied MacDonald criteria for MS (Polman et al., 2005) and experienced a verified relapse or Gd+ magnetic resonance imaging (MRI) brain lesion in the past 12 months. All participants were at least 18 years of age, were able to speak and read English, and had Expanded Disability Status Scale (EDSS; Kurtzke, 1983) scores of 0–6.5, indicating they did not require a wheelchair. Exclusion criteria included use of a corticosteroid in the past 28 days, use of natalizumab or a cytotoxic agent, diagnosis of another autoimmune or endocrine disorder, diagnosis of a serious mental health condition, and receipt or plans to receive psychotherapy. Patients completed self-reports assessing perceived stress and the validity constructs 13 times at 4-week intervals (Week 0-Week 48). Data from patients who dropped out were used when collected, but not imputed beyond the last point of collection.
Materials
Perceived stress measures
Patients rated items on the PSS-10 (described above1), and 16 items from the PSQ (also described above), on 5-point Likert scales based on frequency.
Validation measures
Several measures were included to compare the functioning of new perceived stress measures to that of the PSS, as well as to provide evidence of construct validity. Depressive and anxiety symptoms were included to establish convergent validity, given the substantial overlap between these variables and perceived stress noted in the literature (e.g., Cohen et al., 1983). Depressive symptom severity was measured using the Center for Epidemiologic Studies Depression Scale (CES-D; Radloff, 1977), while the seven-item Hospital Anxiety and Depression Scale (HADS; Zigmond & Snaith, 1983) was used to measure anxiety symptoms. For the same reasons, a measure of major, stressful life events (adapted from Cohen, Doyle, & Skoner, 1999) was expected to have a medium-to-small positive correlation with the perceived stress measures. Finally, a self-reported measure of health services utilization (HSU), developed from an instrument by Fox (1997), summed the number of visits to medical personnel, medical support personnel (e.g., physical therapists), and the emergency room during the past 3 months. This variable was included to confirm the small correlation observed by Cohen and colleagues in their initial report on the PSS (Cohen et al., 1983).
Statistical Procedures
Confirmatory factor analyses were conducted using Mplus, version 5.21 (Muthén & Muthén, 2007). Maximum likelihood (ML) estimation was used. For cross-sectional models, incremental fit statistics were calculated using the standard independence null model. In contrast, for longitudinal models, null models included assumptions of equal variances and means of the indicators across time points, which has been shown to be more appropriate as a null model (Widaman & Thompson, 2003). To establish the tenability of strong and weak metric invariance, chi-square difference tests of nested models were used to detect deterioration in fit.
EFA was conducted using CEFA, version 3.02 (Browne, Cudeck, Tateneni, & Mels, 2008). Maximum Wishart likelihood (MWL) estimation was used, with a direct quartimin (oblique) rotation. To detect the number of factors to be extracted, fit indices and interpretability of factors were principally used, with single-item-loading factors interpreted as evidence of overfactoring. Because factors were appropriately overdetermined (e.g., item-to-factor ratios of 10:1 and 10:2 were explicitly generated for the PSS EFA) and communalities were modestly large (between .45 and .70), the sample size at baseline was appropriately large for EFA according to past simulation studies (MacCallum, Widaman, Zhang, & Hong, 1999), despite not being as large as suggested by older, less empirically derived “rules of thumb.”
A variety of goodness-of-fit statistics were calculated to evaluate the models:
Chi-square (χ2), a statistic of a null hypothesis test. Although χ2 has several problems and tends to be over-conservative, it remains a mainstay in reporting model fit (Barrett, 2007).
Comparative fit index (CFI; Bentler, 1990), a measure of incremental fit above that of a null model. Good fit was indicated by a value above .95 (Hu & Bentler, 1999).
Non-normed fit index (NNFI; Bentler & Bonett, 1980), another incremental fit statistic. The value .95 is generally accepted as the lower limit of good fit (Hu & Bentler, 1999).
Steiger-Lind root mean square error of approximation (RMSEA; Steiger, 1990), a parsimony adjusted absolute fit index. RMSEA<.05 indicated close fit, .05<RMSEA<.08 indicated reasonable fit, .08<RMSEA<.10 indicated mediocre fit, and RMSEA>.10 was unacceptable (Browne & Cudeck, 1993; MacCallum, Browne, & Sugawara, 1996).
Standardized root mean square residual (SRMR), based on the difference between observed and predicted covariance residuals. SRMR<.08 indicated acceptable fit (Hu & Bentler, 1999).
Results
Participants
All enrolled participants were included in the analysis (N = 138). Participants were predominantly female (81.2%, n = 112, 1 missing) and Caucasian (80.4%, n = 111). The average age was 42.88 years (standard deviation [SD] = 9.78, range 24–69). All but one individual reported at least 12 years of education (mean [M] = 15.76, SD = 2.23). Participants varied on employment status: slightly over half were employed at baseline (53.6%, n = 74, 3 missing), with fewer reporting being on disability assistance (18.1%, n = 25) or being unemployed (15.9%, n = 22). Almost two-thirds were rated as having at least moderate disability from MS at baseline (EDSS≥3.0; 65.4%, n = 87, median [Mdn] = 3.5). Although participants, relative to nonclinical populations observed elsewhere, reported elevated depressive symptoms (CES-D: 14.1 v. 8.4; Magni, Caldieron, Rigatti-Luchini, & Merskey, 1990; Zhong et al., 2010), their perceived stress (PSS: 16.4 [6.3] v. 15.3 [7.8]; Cohen & Janicki-Deverts, in press [2006 data]) and anxiety symptoms (HADS: 6.2 [3.6] v. 6.1 [3.8]; Crawford, Henry, Crombie, & Taylor, 2001) were relatively consistent with the general population.
Most participants (76.8%, n = 106) were retained across the 13 measurement points (n's for Weeks 4–48: 130, 130, 129, 128, 121, 120, 114, 113, 112, 111, 107, 106). Likelihood of dropout was associated with being on disability assistance (r = .187, p<.05), but not with any other demographic measure nor with neurological disability from MS.
Model Building and Evaluation
PSS
Confirmatory factor analyses of the PSS, using the two-factor model proposed by Golden-Kreutz et al. (2004) and Roberti, Harrington, and Storch (2006), showed mediocre fit overall (Table 1). Although 6 of the 13 weeks generally evidenced fit in the acceptable or better range, the remaining 7 weeks showed mediocre to unacceptable fit on at least one absolute and one incremental fit statistic. Tests of invariance of factor loadings across time showed significant differences from the nested configural models for both the Stress and Counterstress factors, while tests of invariance of intercepts was marginally acceptable only for the Stress factor.
Table 1.
Goodness-of-Fit Statistics for the Perceived Stress Scale Two-Factor Solution
| PSS (2-factor) Week & model | χ 2 | df | p | CFI | NNFI | RMSEA | RMSEA 90% CI | SRMR | Δ χ 2 | Δ df | p | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| CFA | 54.259 | 34 | 0.0151 | 0.969 | 0.959 | 0.066 | (0.029, 0.097) | 0.044 | — | — | — | |
| 4 CFA | 68.706 | 34 | 0.0004 | 0.939 | 0.919 | 0.090 | (0.059, 0.121) | 0.046 | — | — | — | |
| 8 CFA | 88.861 | 34 | 0.0000 | 0.914 | 0.886 | 0.112 | (0.084, 0.141) | 0.054 | — | — | — | |
| 12 CFA | 63.187 | 34 | 0.0017 | 0.953 | 0.937 | 0.085 | (0.051, 0.117) | 0.042 | — | — | — | |
| 16 CFA | 49.822 | 34 | 0.0391 | 0.979 | 0.972 | 0.061 | (0.014, 0.096) | 0.036 | — | — | — | |
| 20 CFA | 61.602 | 34 | 0.0026 | 0.954 | 0.939 | 0.083 | (0.049, 0.116) | 0.043 | — | — | — | |
| 24 CFA | 55.068 | 34 | 0.0126 | 0.966 | 0.955 | 0.073 | (0.034, 0.108) | 0.046 | — | — | — | |
| 28 CFA | 41.414 | 34 | 0.1787 | 0.985 | 0.980 | 0.045 | (0.000, 0.086) | 0.043 | — | — | — | |
| 32 CFA | 59.856 | 34 | 0.0040 | 0.947 | 0.929 | 0.083 | (0.047, 0.117) | 0.049 | — | — | — | |
| 36 CFA | 49.106 | 34 | 0.0452 | 0.974 | 0.966 | 0.064 | (0.010, 0.102) | 0.038 | — | — | — | |
| 40 CFA | 58.673 | 34 | 0.0054 | 0.955 | 0.941 | 0.083 | (0.045, 0.118) | 0.048 | — | — | — | |
| 44 CFA | 45.046 | 34 | 0.0975 | 0.977 | 0.969 | 0.057 | (0.000, 0.097) | 0.042 | — | — | — | |
| 48 CFA | 73.277 | 34 | 0.0001 | 0.922 | 0.897 | 0.104 | (0.071, 0.137) | 0.066 | — | — | — | |
| Stress | 0–48 CFA | 4116.669 | 2379 | 0.0000 | 0.763 | 0.686 | 0.073 | (0.069, 0.076) | 0.085 | — | — | — |
| 0–48 WMI | 4205.863 | 2439 | 0.0000 | 0.759 | 0.689 | 0.072 | (0.069, 0.076) | 0.084 | 89.194 | 60 | 0.0085 | |
| 0–48 SMI | 4293.419 | 2499 | 0.0000 | 0.755 | 0.692 | 0.072 | (0.068, 0.076) | 0.085 | 87.556 | 60 | 0.0116 | |
| Counterstress | 0–48 CFA | 1378.463 | 884 | 0.0000 | 0.895 | 0.832 | 0.064 | (0.057, 0.070) | 0.059 | — | — | — |
| 0–48 WMI | 1446.025 | 920 | 0.0000 | 0.889 | 0.828 | 0.064 | (0.058, 0.071) | 0.071 | 67.562 | 36 | 0.0011 | |
| 0–48 SMI | 1511.391 | 956 | 0.0000 | 0.883 | 0.825 | 0.065 | (0.059, 0.071) | 0.074 | 65.366 | 36 | 0.0019 | |
Note. df = degree of freedom; CFI = comparative fit index; NNFI = non-normed fit index; RMSEA = root-mean square error of approximation; CI = confidence interval; SRMR = standardized root mean square residual; CFA = confirmatory factor analysis (configural model); WMI = weak metric invariant model; SMI = strong metric invariant model.
Dashes indicate that the statistic was not estimated.
The one-factor solution of the PSS was even more poorly supported by CFA. For these models, few weeks (28, 36, and perhaps Week 44) showed good fit among the various indices. In contrast, data from the remaining 10 weeks clearly did not fit the one-factor solution well (i.e., in all 10 weeks, NNFI < .95 and RMSEA > .08, in 9 weeks CFI < .95).
EFA of Week 0 (baseline; see Table 2) data provided a new solution with factors conceptually similar to those from the previously identified two-factor model: Stress (items 1, 2, 3, 8, 9, 11, and 14) and Counterstress (items 2, 6, 7, and 10). This differed from the aforementioned model by item 9 switching factors, as well as permitting cross-loading for item 2. Clear evidence of overfactoring emerged for 3-factor and 4-factor solutions, while the two-factor solution evidenced very good fit at baseline (χ2 = 31.077, CFI = .992, NNFI = .986, RMSEA = .038). The two factors of this solution were significantly correlated, r = −.712.
Table 2.
Rotated Factor Loadings for the Perceived Stress Scale, Two-Factor Exploratory Factor Analysis Solution
| Stress |
Counterstress |
|||
|---|---|---|---|---|
| PSS item | Loading | SE | Loading | SE |
| 1 | 0.667a | (0.115) | −0.001 | (0.123) |
| 2 | 0.330a | (0.133) | −0.399a | (0.132) |
| 3 | 0.836a | (0.067) | 0.116b | (0.058) |
| 6 | 0.030 | (0.075) | 0.844a | (0.082) |
| 7 | 0.005 | (0.088) | 0.835a | (0.090) |
| 8 | 0.436a | (0.132) | −0.268b | (0.137) |
| 9 | −0.490a | (0.126) | 0.286b | (0.133) |
| 10 | −0.191 | (0.125) | 0.600a | (0.117) |
| 11 | 0.697a | (0.111) | −0.006 | (0.120) |
| 14 | 0.643a | (0.116) | −0.217 | (0.127) |
Note. SE = standard error.
Loading is significant (p<.05), and factor loading is included in subsequent modeling.
Loading is significant (p<.05), but factor loading is not included in subsequent modeling due to its small magnitude (<.30).
Upon CFA for this new two-factor model of the PSS, the model showed unacceptable fit (i.e., NNFI < .95 and RMSEA > .08) for 8 of the 12 time points following Week 0. Although WMI may have been tenable for the Counterstress factor, all other tests showed dubious invariance of loading and intercept parameters over time.
PSS + PSQ items
The item pool was expanded to include 16 questions from the PSQ. EFAs of all possible factor solutions (up to the point of obvious overfactoring) for the Week 0 data were then iteratively conducted on sets of 26, 25, 24, and 23 items, each time removing the item with the most extreme (and consistent across solutions) problem of low communality. This did not yield useful solutions—although several models seemed to fit adequately, interpreting the factors was difficult and substantial numbers of factor loadings were of low magnitude (<.35).
However, several patterns in these analyses did emerge that informed subsequent work. In nearly every EFA performed, items 4, 16, and 30 and items 6, 23, and 24 from the PSQ loaded onto the same factors, which can be referred to respectively as Pushed, and Conflict and Imposition. More subtly, across these EFAs, item 18 from the PSQ frequently loaded with PSS item 14, which, in turn, tended to load with PSS item 10. Consequently, these three items were proposed to tap into a similar construct, Lack of Control. The resulting instrument is hereafter referred to as the Brief Inventory of Perceived Stress (BIPS; Table 3).
Table 3.
Items Included in the Brief Inventory of Perceived Stress (BIPS)
| Pushed subscale | |
|---|---|
| PSQ, item 4. | In the last month, how often have you had too many things to do? |
| PSQ, item 16. | In the last month, how often have you felt you were in a hurry? |
| PSQ, item 30. | In the last month, how often have you felt under pressure from deadlines? |
| Conflict AND imposition subscale | |
|---|---|
| PSQ, item 6. | In the last month, how often have you found yourself in situations of conflict? |
| PSQ, item 23. | In the last month, how often have you felt you were doing things because you had to not because you wanted to? |
| PSQ, item 24. | In the last month, how often have you felt criticized or judged? |
| Lack of control subscale | |
|---|---|
| PSS, item 14. | In the last month, how often have you felt difficulties were piling up so high that you could not overcome them? |
| PSS, item 10a. | In the last month, how often have you felt that you were on top of things? |
| PSQ, item 18b. | In the last month, how often have you had too many worries? |
Note. PSS = Perceived Stress Scale; PSQ = Perceived Stress Questionnaire.
Reverse-scored.
The original PSQ did not include the word “too.”
This proposed 9-item, 3-factor amalgamation was then tested with CFA for the entire range of time points (Table 4), with standardized parameter estimates, including factor loadings, for Week 0 (Figure 1). Good fit was indicated by nearly all indices2; minor misfit was suggested solely by the NNFI at Weeks 8 and 12, with mediocre fit more clearly evident at Week 32. Tests of invariance confirmed that weak metric invariance was tenable for Lack of Control and Conflict and Imposition, and possibly tenable for Pushed. Strong metric invariance was evident for Conflict and Imposition and Pushed, but was unsupported for Lack of Control.
Table 4.
Goodness-of-Fit Statistics for the Brief Inventory of Perceived Stress Three-Factor Solution
| BIPS week and model | χ 2 | df | p | CFI | NNFI | RMSEA | RMSEA 90% CI | SRMR | Δ χ 2 | Δ df | p | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 0 CFA | 25.613 | 23 | 0.3195 | 0.995 | 0.992 | 0.029 | (0.000, 0.078) | 0.032 | — | — | — | |
| 4 CFA | 36.084 | 23 | 0.0404 | 0.968 | 0.950 | 0.067 | (0.014, 0.108) | 0.053 | — | — | — | |
| 8 CFA | 41.719 | 23 | 0.0098 | 0.958 | 0.934 | 0.079 | (0.039, 0.117) | 0.034 | — | — | — | |
| 12 CFA | 38.691 | 23 | 0.0214 | 0.965 | 0.945 | 0.075 | (0.029, 0.116) | 0.047 | — | — | — | |
| 16 CFA | 28.686 | 23 | 0.1910 | 0.989 | 0.983 | 0.044 | (0.000, 0.090) | 0.032 | — | — | — | |
| 20 CFA | 18.894 | 23 | 0.7074 | 1.000 | 1.014 | 0.000 | (0.000, 0.059) | 0.032 | — | — | — | |
| 24 CFA | 25.692 | 23 | 0.3156 | 0.995 | 0.992 | 0.032 | (0.000, 0.086) | 0.041 | — | — | — | |
| 28 CFA | 29.931 | 23 | 0.1514 | 0.984 | 0.975 | 0.052 | (0.000, 0.100) | 0.046 | — | — | — | |
| 32 CFA | 42.750 | 23 | 0.0074 | 0.947 | 0.918 | 0.088 | (0.045, 0.129) | 0.050 | — | — | — | |
| 36 CFA | 36.766 | 23 | 0.0344 | 0.971 | 0.954 | 0.074 | (0.021, 0.118) | 0.055 | — | — | — | |
| 40 CFA | 35.002 | 23 | 0.0520 | 0.976 | 0.962 | 0.070 | (0.000, 0.115) | 0.054 | — | — | — | |
| 44 CFA | 27.783 | 23 | 0.2241 | 0.986 | 0.978 | 0.045 | (0.000, 0.098) | 0.054 | — | — | — | |
| 48 CFA | 30.566 | 23 | 0.1338 | 0.980 | 0.969 | 0.056 | (0.000, 0.103) | 0.043 | — | — | — | |
| Lack of control | 0–48 CFA | 518.690 | 390 | 0.0000 | 0.963 | 0.922 | 0.049 | (0.037, 0.060) | 0.061 | — | — | — |
| 0–48 WMI | 545.032 | 414 | 0.0000 | 0.962 | 0.925 | 0.048 | (0.036, 0.059) | 0.063 | 26.342 | 24 | 0.3360 | |
| 0–48 SMI | 590.838 | 438 | 0.0000 | 0.956 | 0.917 | 0.050 | (0.039, 0.060) | 0.064 | 45.806 | 24 | 0.0046 | |
| Pushed | 0–48 CFA | 483.875 | 390 | 0.0008 | 0.977 | 0.953 | 0.042 | (0.028, 0.053) | 0.055 | — | — | — |
| 0–48 WMI | 527.153 | 414 | 0.0001 | 0.973 | 0.946 | 0.045 | (0.032, 0.056) | 0.065 | 43.278 | 24 | 0.0092 | |
| 0–48 SMI | 563.671 | 438 | 0.0000 | 0.970 | 0.944 | 0.046 | (0.034, 0.056) | 0.067 | 36.518 | 24 | 0.0488 | |
| Conflict and imposition | 0–48 CFA | 519.792 | 377 | 0.0000 | 0.950 | 0.892 | 0.052 | (0.041, 0.063) | 0.076 | — | — | — |
| 0–48 WMI | 554.810 | 401 | 0.0000 | 0.946 | 0.891 | 0.053 | (0.042, 0.063) | 0.058 | 35.018 | 24 | 0.0681 | |
| 0–48 SMI | 577.528 | 425 | 0.0000 | 0.947 | 0.898 | 0.051 | (0.040, 0.061) | 0.059 | 22.718 | 24 | 0.5364 |
Note. df = degree of freedom; H1 = hypothesized model; CFI = comparative fit index; NNFI = non-normed fit index; RMSEA = root-mean square error of approximation; CI = confidence interval; SRMR = standardized root mean square residual; CFA = confirmatory factor analysis (configural model); WMI = weak metric invariant model; SMI = strong metric invariant model.
Dashes indicate that the statistic was not estimated.
Figure 1.
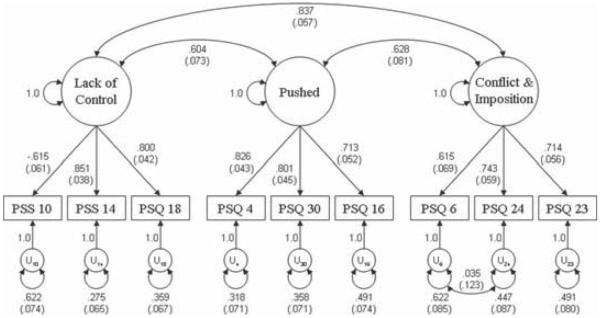
Confirmatory factor analytic model of the BIPS, with the standardized solution for the Week 0 data. Standardized errors for the estimates are provided in parentheses. All parameter estimates are significant at the .01 level, except for the correlated residual (p>.77).
Relationships Among Measures of Perceived Stress and Validity Measures
Scale and subscale scores for the PSS and the BIPS were generated by summing the items loading onto their respective factors (reverse-scoring when needed). The BIPS demonstrated good internal reliability and adequate internal reliability for each of its subscales (Table 5). Its 1-month and 1-year test-retest reliabilities were comparable to those of the PSS.
Table 5.
Correlations Among Measures of Perceived Stress (and Their Subscales) and Construct Validity Measures
| CES-D | PSS | Stress | Counterstress | HSU | HADS Anxiety | Lack of Control | Pushed | Conflict & Imposition | BIPS | Life Events | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| CES-D | range | 1 | .65–.76a | |||||||||
| PSS | range | .746 (.680, .811) | 1 | .22b | .32b | |||||||
| Stress | range | .690 (.605, .763) | .960 (.952, .969) | 1 | ||||||||
| Counter-stress | range | −.721 (−.786, −.686) | −.917 (−.942, −.906) | −.771 (−.819, −.744) | 1 | |||||||
| HSU | range | [7] .170 (.007, .267) | [9] .223 (.039, .320) | [9] .237 (.039, .360) | [6] −.185 (−.341, −.005) | 1 | ||||||
| HADS Anxiety | range | .773 (.629, .841) | .749 (.595, .860) | .735 (.583, .859) | −.677 (−.748, −.521) | [1] .148 (−.158, .442) | 1 | |||||
| Lack of Control | range | .696 (.592, .781) | .908 (.880, .920) | .869 (.841, .886) | −.838 (−.881, −.795) | [9] .218 (.053, .342) | .771 (.585, .864) | 1 | ||||
| Pushed | range | [11] .242 (.089, .393) | .442 (.332, .520) | .480 (.368, .564) | −.329 (−.415, −.234) | [1] .101 (−.033, .235) | [11] .429 (.236, .653) | .485 (.368, .555) | 1 | |||
| Conflict & Imposition | range | .551 (.506, .595) | .671 (.601, .718) | .670 (.592, .717) | −.583 (−.646, −.534) | [5] .157 (.002, .243) | .597 (.436, .724) | .623 (.555, .703) | .492 (.397, .593) | 1 | ||
| BIPS | range | .582 (.515, .670) | .804 (.755, .832) | .803 (.754, .835) | .694 (.656, .734) | [6] .177 (.016, .282) | .667 (.559, .798)) | .842 (.813, .871) | .815 (.776, .852) | .827 (.791, .870) | 1 | |
| Life Events | range | [12] .214 (.048, .325) | .277 (.169, .404) | [12] .290 (.149, .409) | [10] .−227 (−.326, −.053) | [6] .190 (−.044, .352) | [4] .234 (−.066, .397) | [10] .251 (.120, .438) | [5] .146 (−.028, .274) | [10] .225 (.084, .315) | [11] .236 (.104, .398) | 1 |
| M (SD), baseline | 14.11 (10.31) | 16.37 (6.27) | 10.89 (3.91) | 5.48 (2.78) | 3.25 (4.00) | 6.16 (3.64) | 5.38 (2.41) | 7.20 (2.55) | 5.41 (2.25) | 17.99 (6.02) | 2.60 (2.08) | |
| Cronbach's α, baseline | .913 | .904 | .847 | .847 | — | .796 | .796 | .819 | .733 | .869 | — | |
| 1-month Stability | .640 | .657 | .606 | .619 | .271 | .753 | .566 | .626 | .664 | .676 | .332 | |
| 12-month Stability | .638 | .670 | .604 | .658 | .049, ns | .542 | .519 | .584 | .568 | .626 | .088, ns |
Note>. CES-D= Center for Epidemiologic Studies Depression Scale; PSS = Perceived Stress Scale; Stress = the original Stress subscale of the Perceived Stress Scale; Counterstress = the original Counterstress subscale of the Perceived Distress Scale; HSU = Health Services Utilization; HADS = Hospital Anxiety and Depression Scale; Lack of Control = Lack of Control subscale of the Brief Inventory of Perceived Stress; Pushed = Pushed subscale of the Brief Inventory of Perceived Stress; Conflict & Imposition = Conflict & Imposition subscale of the Brief Inventory of Perceived Stress; BIPS = Brief Inventory of Perceived Stress; m = mean; SD = standard deviation.
For each time point, all 13 Pearson correlations within a cell were significant, p < .05, unless the number of significant correlations is otherwise noted in brackets in front of the correlation coefficient. All stabilities were significant, p < .01, unless otherwise indicated, r = average Pearson correlation among the 13 time points measured (calculated from the coefficient of determination); range = range of Pearson correlations among the 13 time points measured.
As hypothesized, the PSS showed large correlations with anxiety and depression, a small correlation with health service utilization, and a small-approaching-medium correlation with number of stressful life events. Nearly identical associations were found using the original Stress and Counterstress variables, which were also highly correlated to each other. The same pattern of correlations was observed for the BIPS, although, with the exception of its relationship with stressful life events, the associations were somewhat attenuated. However, this appeared to reflect differences among the BIPS subscales, described as follows, rather than reduced validity.
The BIPS Lack of Control subscale performed equivalently to the PSS in terms of concurrent validity, while relationships with the validity variables were attenuated for the Conflict and Imposition subscale. The Pushed subscale diverged notably from these associations, with a tendency to have reduced correlations with all convergent validity scales, to the point of only one week's measurements being correlated with health services utilization, fewer than half the weeks being correlated with stressful life events, and small correlations with depressive symptoms. Nevertheless, the Pushed subscale still showed medium-magnitude correlations to other measures of perceived stress, including the other BIPS subscales.
Discussion
The purpose of this study was to examine and compare factor structures underlying perceived stress in a sample of participants with MS, using results to develop the BIPS, a new measure of perceived stress with improved structural validity. To this end, we compared models drawn from the literature and empirically from the data, using both the 10 original PSS items and an amalgamation of items hypothesized to indicate perceived stress more broadly.
The previously proposed two-factor solution for the PSS (Golden-Kreutz et al., 2004; Roberti et al., 2006) evidenced better fit than the one-factor alternative, consistent with past analyses (Golden-Kreutz et al., 2004). As noted previously (Golden-Kreutz et al., 2004), a three-factor solution was inappropriate. However, the two-factor solution did not provide models of consistently good fit over time, or a stable solution. Several factors may explain these findings.
First, the population from which we drew our sample may have yielded worse fit, as the two-factor model was originally designed around samples of women with breast cancer (Golden-Kreutz et al., 2004) and undergraduates (Roberti et al., 2006). In varying populations, stress may be conceptualized differently. However, this explanation is somewhat suspect, as this original two-factor model failed to fit the data well despite the scales showing better internal consistencies (e.g., PSS: alpha = .90 v .78; Cohen et al., 1983) than reported for the samples with which the models were developed.
Second, this is the first study evaluating the PSS factor models with such a focus on longitudinal stability. One previous study used longitudinal data (Golden-Kreutz et al., 2004), but centered around identifying consistent loading patterns (i.e., the same items loading “high” and “low” on the same factors over time). This contrasts with our more conservative, formal tests of stability using statistical tests of invariance of item loadings and intercepts (Horn & McArdle, 1992).
Third, the fit indices reported by Roberti and colleagues (2006) would actually have been classified as mediocre or poor under the thresholds in this study. Finally, use of more recent developments in methodology of factor analysis may also have contributed to our finding a distinct (but still inadequate) EFA solution.
Findings from these one-factor and two-factor solutions offer several caveats on current usage of the PSS. Most notably, despite the consistent lack of evidence for a one-factor conceptualization of perceived stress, the use of single scale measures has been ubiquitous. Use of a single composite measure of perceived stress may diminish the capacity of an instrument to predict stress sequelae, because of conflation of the underlying factors. The apparent unreliability of factors derived from the PSS may also result in diminished power to predict health outcomes. Finally, findings from these models suggest that expanding an item set beyond the PSS's 10 items may be needed to identify any additional factors underlying perceived stress.
The BIPS may offer a solution to several of these concerns. Its underlying factors—Lack of Control, Pushed, and Conflict and Imposition—fit our data well and seem to reflect the same constructs longitudinally, with consistent factor loadings and item intercepts across time points (see Model Building and Evaluation, however, for some questions about the Lack of Control item intercepts). Also advantageous is that the BIPS requires only nine items for quick administration, demonstrates good internal reliability, and evidences no decrement relative to the PSS in terms of test-retest reliability.
The BIPS shows promise in uncovering new ways of understanding perceived stress. The BIPS subscales yielded intercorrelations that were smaller than those found between PSS-only subscale correlations, but still statistically significant. This suggests the BIPS factors represent related but distinct constructs. Moreover, the BIPS enjoys convergent validity with the PSS, as the total BIPS and the Lack of Control subscale overlapped substantially with the composite PSS. Conflict and Imposition and Pushed also correlated with the PSS significantly, but more modestly. These findings again suggest the factors underlying the BIPS are conceptually separable and offer distinctions among numerous manifestations of perceived stress. Further, the associations between validity measures and BIPS subscales suggest that the Lack of Control factor captured much of the same information as the PSS composite, with seven fewer items. The total BIPS was also similar to the PSS in terms of construct validity, although the pattern of associations was somewhat smaller because of the novel behavior of the other two BIPS subscales.
For example, in our study, the PSS significantly correlated with CES-D scores at each time point, with an average correlation of .746 that was comparable to previous studies (r = .50–.74; Christian, Franco, Glaser, & Iams, 2009; McCallum, Sorocco, & Fritsch, 2006; Riggs, Vosvick, & Stallings, 2007). Lack of Control evidenced similar associations with depression, r=.696. The correlation between depression and Conflict and Imposition was smaller but remarkable, r = .551, and similar to the correlation between the total PSQ and the CES-D (r = .56; Levenstein et al., 1993). In contrast, Pushed had much smaller correlations with depression, r = .242, and was nonsignificant at 2 of 13 time points. This offers a compelling area of exploration: Despite clear associations with other perceived-stress-related constructs, which themselves reflect vulnerability to depression, Pushed does not consistently share this characteristic. Stated differently, despite a wealth of evidence cited above showing that perceived stress reflects a vulnerability to depression, the “pushed” aspect of perceived stress seems to operate largely externally to this. Thus, perceived stress could have substantially different implications depending on the particular stress appraisals being made—a distinction that may be captured more easily by the BIPS than by other measures of perceived stress.
One limitation of this study is that the data were drawn from a population of individuals with MS. The inflammation involved in MS can increase activity of the hypothalamic-pituitary-adrenal (HPA) axis, which might lead to altered stress responses (Mohr & Pelletier, 2006); thus, findings might not generalize to other medical populations. Although there was a range of psychiatric morbidity in this sample, this was not an inclusion criterion, and to be enrolled, participants had to report no current or planned participation in psychotherapy. Thus, results may not generalize to psychiatric samples. It will be crucial to test the generalizability of these findings in other patient populations as well as nonclinical populations—as multiple perceived stress measures are relatively rarely used in studies as large as this one, we were unable to confirm our findings with an independent sample. Second, as noted above, the sample size was smaller than is often used for factor analysis; despite evidence that it likely was sufficiently large for yielding stable estimates (MacCallum, Widaman, Preacher, & Hong, 2001), this point reinforces the need for confirmation of our model in a separate sample. Finally, the items used to design the BIPS were derived from preexisting measures. Although this strategy was not problematic in itself, a similar study, for which entirely new items are generated, may expand our understanding of perceived stress's dimensionality even beyond the present findings.
In summary, this study offers new insights into conceptualization of perceived stress. Researchers may benefit by examining a variety of aspects of perceived stress relevant to their specific research questions. We have thus proposed a new measure of perceived stress, the BIPS. The BIPS enjoys beneficial psychometric properties, including good model fit and discrimination among underlying factors. The BIPS also demonstrated reliable factor loadings across a long time period, and its subscales capture nuances of the relationships between perceived stress and related constructs that may not be detectable using composite measures of perceived stress. Future research on the BIPS is encouraged to confirm these properties in other populations and examine the utility of the BIPS in predicting psychosocial and health-related outcomes.
Acknowledgments
This work was funded by NIH grant R01-HD043323 to David C. Mohr.
Footnotes
PSS item numberings are based on the 14-item version.
Correlated residuals were permitted between PSQ items 23 and 24, due to semantic attributes not shared with PSQ item 6.
References
- Barrett P. Structural equation modelling: Adjudging model fit. Personality and Individual Differences. 2007;42(5):815–824. [Google Scholar]
- Benight CC, Bandura A. Social cognitive theory of posttraumatic recovery: The role of perceived self-efficacy. Behaviour Research and Therapy. 2004;42(10):1129–1148. doi: 10.1016/j.brat.2003.08.008. [DOI] [PubMed] [Google Scholar]
- Bentler PM. Comparative fit indexes in structural models. Psychological Bulletin. 1990;107(2):238–246. doi: 10.1037/0033-2909.107.2.238. [DOI] [PubMed] [Google Scholar]
- Bentler PM, Bonett DG. Significance tests and goodness of fit in the analysis of covariance structures. Psychological Bulletin. 1980;88(3):588–606. [Google Scholar]
- Browne MW, Cudeck R. Alternative ways of assessing model fit. Sociological Methods & Research. 1993;21(2):230–258. [Google Scholar]
- Browne MW, Cudeck R, Tateneni K, Mels G. CEFA: Comprehensive Exploratory Factor Analysis. Version 3.02. 2008. Computer software and manual. [Google Scholar]
- Christian LM, Franco A, Glaser R, Iams JD. Depressive symptoms are associated with elevated serum proinflammatory cytokines among pregnant women. Brain, Behavior, and Immunity. 2009;23(6):750–754. doi: 10.1016/j.bbi.2009.02.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen S, Doyle WJ, Skoner DP. Psychological stress, cytokine production, and severity of upper respiratory illness. Psychosomatic Medicine. 1999;61:175–180. doi: 10.1097/00006842-199903000-00009. [DOI] [PubMed] [Google Scholar]
- Cohen S, Janicki-Deverts D. Who's stressed? Distributions of Psychological Stress in the United States in Probability Samples from 1983, 2006 and 2009. in press. Retrieved from http://www.psy.cmu.edu/~scohen/Cohen_Janicki_PSS_JASP_2010.doc, archived at http://www.webcitation.org/62gF4Wrhi.
- Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. Journal of Health and Social Behavior. 1983;24(4):385–396. [PubMed] [Google Scholar]
- Cohen S, Kessler RC, Gordon LU. Measuring stress: A guide for health and social scientists. Oxford University Press; New York, NY: 1995. [Google Scholar]
- Cohen S, Williamson GM. Perceived stress in a probability sample of the United States. In: Spacapan S, Oskamp S, editors. The social psychology of health. Sage; Newbury Park, CA: 1988. pp. 31–67. [Google Scholar]
- Crawford JR, Henry JD, Crombie C, Taylor EP. Brief report Normative data for the HADS from a large non-clinical sample. British Journal of Clinical Psychology. 2001;40(4):429. doi: 10.1348/014466501163904. [DOI] [PubMed] [Google Scholar]
- Crowe SF, Barot J, Caldow S, D'Aspromonte J, Dell'Orso J, Di Clemente A, Sapega S. The effect of caffeine and stress on auditory hallucinations in a non-clinical sample. Personality and Individual Differences. 2011;50(5):626–630. [Google Scholar]
- Fliege H, Rose M, Arck P, Kocalevent R-D, Klapp BF, Weber C, Klapp BF. The Perceived Stress Questionnaire (PSQ) reconsidered: Validation and reference values from different clinical and healthy adult samples. Psychosomatic Medicine. 2005;67(1):78–88. doi: 10.1097/01.psy.0000151491.80178.78. [DOI] [PubMed] [Google Scholar]
- Fox PJ. Service use and cost outcomes for persons with Alzheimer disease. Alzheimer Disease and Associated Disorders. 1997;11:125–134. [PubMed] [Google Scholar]
- Golden-Kreutz DM, Browne MW, Frierson GM, Andersen BL. Assessing stress in cancer patients: A second-order factor analysis model for the Perceived Stress Scale. Assessment. 2004;11(3):216–223. doi: 10.1177/1073191104267398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- González Ramírez MT, Landero Hernández R. Factor structure of the Perceived Stress Scale (PSS) in a sample from Mexico. The Spanish Journal of Psychology. 2007;10(1):199–206. doi: 10.1017/s1138741600006466. [DOI] [PubMed] [Google Scholar]
- Horn JL, McArdle JJ. A practical and theoretical guide to measurement invariance in aging research. Experimental Aging Research. 1992;18(3–4):117–144. doi: 10.1080/03610739208253916. [DOI] [PubMed] [Google Scholar]
- Hu L.-t., Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling. 1999;6(1):1–55. [Google Scholar]
- Kurtzke JF. Rating neurologic impairment in multiple sclerosis: An expanded disability status scale (EDSS) Neurology. 1983;33(11):1444–1452. doi: 10.1212/wnl.33.11.1444. [DOI] [PubMed] [Google Scholar]
- Lazarus RS. Stress and emotion: A new synthesis. Free Association Books; London, UK: 1999. [Google Scholar]
- Lazarus RS, Folkman S. Stress, appraisal, and coping. Springer Publishing Inc.; New York, NY: 1984. [Google Scholar]
- Levenstein S, Prantera C, Varvo V, Scribano ML, Berto E, Luzi C, Andreoli A. Development of the Perceived Stress Questionnaire: A new tool for psychosomatic research. Journal of Psychosomatic Research. 1993;37(1):19–32. doi: 10.1016/0022-3999(93)90120-5. [DOI] [PubMed] [Google Scholar]
- MacCallum RC, Browne MW, Sugawara HM. Power analysis and determination of sample size for covariance structure modeling. Psychological Methods. 1996;1:130–149. [Google Scholar]
- MacCallum RC, Widaman KF, Preacher KJ, Hong S. Sample size in factor analysis: The role of model error. Multivariate Behavioral Research. 2001;36(4):611–637. doi: 10.1207/S15327906MBR3604_06. [DOI] [PubMed] [Google Scholar]
- MacCallum RC, Widaman KF, Zhang S, Hong S. Sample size in factor analysis. Psychological Methods. 1999;4(1):84–99. [Google Scholar]
- Magni G, Caldieron C, Rigatti-Luchini S, Merskey H. Chronic musculoskeletal pain and depressive symptoms in the general population. An analysis of the 1st National Health and Nutrituion Examination Survey data. Pain. 1990;43:299–307. doi: 10.1016/0304-3959(90)90027-B. [DOI] [PubMed] [Google Scholar]
- McCallum TJ, Sorocco KH, Fritsch T. Mental health and diurnal salivary cortisol patterns among African American and european american female dementia family caregivers. American Journal of Geriatric Psychiatry. 2006;14(8):684–693. doi: 10.1097/01.JGP.0000225109.85406.89. [DOI] [PubMed] [Google Scholar]
- Mimura C, Griffiths P. A Japanese version of the Perceived Stress Scale: Cross-cultural translation and equivalence assessment. BMC Psychiatry. 2008;8:85. doi: 10.1186/1471-244X-8-85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mohr DC, Lovera J, Brown T, Cohen B, Neylan T, Henry R, Pelletier D. A randomized trial of stress management for the prevention of new brain lesions in MS. Neurology. doi: 10.1212/WNL.0b013e3182616ff9. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mohr DC, Pelletier D. A temporal framework for understanding the effects of stressful life events on inflammation in patients with multiple sclerosis. Brain Behavior and Immunity. 2006;20(1):27–36. doi: 10.1016/j.bbi.2005.03.011. [DOI] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO. Mplus user's guide. 5th ed. Muthén & Muthén; Los Angeles, CA: 2007. [Google Scholar]
- Pedrelli P, Feldman GC, Vorono S, Fava M, Petersen T. Dysfunctional attitudes and perceived stress predict depressive symptoms severity following antidepressant treatment in patients with chronic depression. Psychiatry Research. 2008;161(3):302–308. doi: 10.1016/j.psychres.2007.08.004. [DOI] [PubMed] [Google Scholar]
- Polman CH, Reingold SC, Edan G, Filippi M, Hartung HP, Kappos L, et al. Diagnostic criteria for multiple sclerosis: 2005 revisions to the “McDonald Criteria.”. Annals of Neurology. 2005;58(6):840–846. doi: 10.1002/ana.20703. [DOI] [PubMed] [Google Scholar]
- Radloff LS. The CES-D Scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1(3):385–401. [Google Scholar]
- Remor E, Penedo FJ, Shen BJ, Schneiderman N. Perceived stress is associated with CD4+cell decline in men and women living with HIV/AIDS in Spain. Aids Care-Psychological and Socio-Medical Aspects of Aids/Hiv. 2007;19(2):215–219. doi: 10.1080/09540120600645570. [DOI] [PubMed] [Google Scholar]
- Riggs SA, Vosvick M, Stallings S. Attachment style, stigma and psychological distress among HIV+ adults. Journal of Health Psychology. 2007;12(6):922–936. doi: 10.1177/1359105307082457. [DOI] [PubMed] [Google Scholar]
- Roberti JW, Harrington LN, Storch EA. Further psychometric support for the 10-Item version of the Perceived Stress Scale. Journal of College Counseling. 2006;9(2):135–147. [Google Scholar]
- Sharp LK, Kimmel LG, Kee R, Saltoun C, Chang C-H. Assessing the Perceived Stress Scale for African American adults with asthma and low literacy. Journal of Asthma. 2007;44(4):311–316. doi: 10.1080/02770900701344165. [DOI] [PubMed] [Google Scholar]
- Siqueira Reis R, Ferreira Hino AA, Rodriguez-Añez CR. Perceived Stress Scale: Reliability and validity study in Brazil. Journal of Health Psychology. 2010;15(1):107–114. doi: 10.1177/1359105309346343. [DOI] [PubMed] [Google Scholar]
- Steiger JH. Structural model evaluation and modification: An interval estimation approach. Multivariate Behavioral Research. 1990;25(2):173–180. doi: 10.1207/s15327906mbr2502_4. [DOI] [PubMed] [Google Scholar]
- Widaman KF, Thompson JS. On specifying the null model for incremental fit indices in structural equation modeling. Psychological Methods. 2003;8(1):16–37. doi: 10.1037/1082-989x.8.1.16. [DOI] [PubMed] [Google Scholar]
- Zhong WJ, Cruickshanks KJ, Schubert CR, Nieto FJ, Huang GH, Klein BEK, et al. Obesity and Depression Symptoms in the Beaver Dam Offspring Study Population. Depression and Anxiety. 2010;27(9):846–851. doi: 10.1002/da.20666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zigmond AS, Snaith RP. The Hospital Anxiety and Depression Scale. Acta Psychiatrica Scandinavica. 1983;67:361–370. doi: 10.1111/j.1600-0447.1983.tb09716.x. [DOI] [PubMed] [Google Scholar]


