Abstract
Background
The increasing prevalence of heart failure (HF) and high associated costs have spurred investigation of factors leading to adverse outcomes in HF patients. Studies to date report inconsistent evidence regarding the link between depression and outcomes with only limited data on emergency department (ED) and outpatient visits.
Methods and Results
Olmsted, Dodge, and Fillmore county, MN residents with HF were prospectively recruited between October 2007 and December 2010, and completed a one-time 9-item Patient Health Questionnaire (PHQ-9) for depression categorized as: none-minimal (PHQ-9 score 0–4), mild (5–9), or moderate-severe (≥10). Andersen-Gill models were used to determine if depression predicted hospitalizations and ED visits while negative binomial regression models explored the association of depression with outpatient visits. Cox proportional hazards regression characterized the relationship between depression and all-cause mortality. Among 402 HF patients (mean age 73±13, 58% male), 15% had moderate-severe depression, 26% mild, and 59% none-minimal. Over a mean follow-up of 1.6 years, 781 hospitalizations, 1000 ED visits, 15,515 outpatient visits, and 74 deaths occurred. After adjustment, moderate-severe depression was associated with nearly a 2-fold increased risk of hospitalization (HR 1.79, 95% CI 1.30–2.47) and ED visits (HR 1.83, 95% CI 1.34–2.50), a modest increase in outpatient visits (RR 1.20, 95% CI 1.00–1.45), and a 4-fold increase in all-cause mortality (HR 4.06, 95% CI 2.35–7.01).
Conclusions
In this prospective cohort study, depression independently predicted an increase in the use of healthcare resources and mortality. Greater recognition and management of depression in HF may optimize clinical outcomes and resource utilization.
Keywords: cardiovascular outcomes, depression, healthcare utilization, heart failure, psychosocial factors
Heart failure (HF) affects nearly 6 million Americans1 and remains the most common cause of hospitalization in the Medicare population,2 with readmission rates approaching 50% within 6 months after initial hospitalization.2–4 As such, HF is one of the most costly health care problems in the U.S., with estimated direct and indirect costs of $39.2 billion in 2010,1 an increase of 163% compared with 2000.2 These costs continue to rise with the aging population and improvements in survival after cardiovascular events.
Due to its high prevalence, associated costs, and relatively poor prognosis, factors contributing to adverse outcomes in HF are targets of investigation. Among such factors, depression has been given special attention, as it is often under-diagnosed and potentially modifiable.5–7 Although depression rates are consistently higher in HF than the general population, estimated at 5%–10%, the exact prevalence and severity of depression in HF varies considerably across studies, ranging from 11%–25% in outpatients to 35%–70% among inpatients.2, 8, 9 These discrepancies leave uncertainties about the importance of depression in HF, from both a clinical and public health standpoint.
Several studies have reported an increased risk of death and hospitalizations in patients with HF and depressive symptoms,2, 5, 10–17 while others have failed to identify significant associations with rehospitalizations17, 18 or mortality.19, 20 Still others have demonstrated mixed results, with significant associations only in the most severely depressed.8, 21, 22
As most studies have focused on mortality and rehospitalization, the impact of depression on other forms of healthcare utilization such as outpatient or emergency department (ED) visits is unknown. This study was designed to address, in a prospective community-based cohort study, the aforementioned knowledge gaps by examining the prevalence and severity of depression among HF patients, as well as its impact on hospitalizations, ED visits, outpatient visits and survival.
Methods
Study Setting
This was a prospective cohort study conducted in southeast Minnesota, which constitutes a unique environment because there are a small number of medical providers including Mayo Clinic, Olmsted Medical Center, and a few private practitioners. Each provider uses comprehensive medical records, which are indexed through the Rochester Epidemiology Project (REP).23 This record linkage system, enables virtually complete capture of outcomes and healthcare utilization in Olmsted County. This system captures outcomes and utilization for non-Olmsted County residents who are seen by an Olmsted County provider, but non-residents may also seek care in their own counties with providers that do not participate in the REP. Therefore, capture of utilization for these patients may be less comprehensive than that of Olmsted County residents. This study was approved by the Mayo Clinic and Olmsted Medical Center Institutional Review Boards.
Identification of the Study Cohort
Patients with either incident or prevalent HF during an inpatient or outpatient visit were identified using natural language processing of the electronic medical record and the diagnoses were manually validated by trained nurse abstractors using the Framingham criteria, as described previously.24 Participants meeting the following criteria were prospectively recruited between October 2007 and December 2010: 1) aged ≥18 years, 2) residents of Olmsted, Dodge, or Fillmore counties, MN, and 3) completed a 9-item Patient Health Questionnaire (PHQ-9) for depression upon study enrollment. Written informed consent was obtained from all participants prior to enrollment.
Clinical Data Collection
Patient characteristics including age, gender, education, marital status, current or former cigarette smoking status, and medications at index were obtained from patient records. Body mass index (BMI) was calculated from the outpatient weight and height recorded in the medical record closest to study enrollment. Hypertension was defined as systolic blood pressure ≥140 mm Hg, diastolic blood pressure ≥90 mm Hg, or a physician diagnosis of hypertension.25 Prevalent diabetes was defined by the American Diabetes Association criteria.26 A clinical diagnosis recorded in the medical record was used to identify hyperlipidemia and previous myocardial infarction (MI). Glomerular filtration rate (GFR) was estimated using the closest serum creatinine value within 1 year of HF diagnosis using the Modification of Diet in Renal Disease Study (MDRD) equation.27 Comorbidities abstracted from patient records were used to calculate an overall comorbidity score for each patient using the Charlson comorbidity index.28 Left ventricular ejection fraction (LVEF) (%) was obtained using the closest value from an echocardiogram within 6 months prior to 2 months after HF date.
Depression Measurement
Depression was assessed once using a 9-item Patient Health Questionnaire (PHQ-9) administered by a registered nurse during a face-to-face interview conducted during a return visit within 6 weeks of consent. This brief questionnaire has been validated and assesses each of the 9 criteria in the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV) for clinical depression on a scale from “0” being “not at all” to “3” being “nearly every day”.29 According to Kroenke and colleagues (2001), PHQ-9 scores of ≥10 were 88% sensitive and 88% specific for detecting major depression and scores of 5, 10, 15, and 20 corresponded well to mild, moderate, moderately severe, and severe depressive symptoms, respectively, as measured by diagnostic interview.29 Taking the results of this study into consideration, depressive symptoms were categorized as none-minimal (PHQ-9 score 0–4), mild (5–9), or moderate-severe (10 or greater).
Ascertainment of Healthcare Utilization and Death
Participants were followed from study enrollment through December 31, 2010 for death and healthcare utilization. Deaths were obtained from inpatient and outpatient medical records and death certificates received annually from Olmsted County and the state of Minnesota. Hospitalizations, ED visits, and outpatient office visits were ascertained through the Olmsted County Healthcare Expenditure and Utilization Database, which contains healthcare utilization information from 1987 to present. For patients enrolled during hospitalization, only subsequent hospitalizations were included in the analysis. In-hospital transfers or transfers between Olmsted Medical Center and Mayo Clinic were analyzed as a single hospitalization. ED visits that resulted in admission and hospitalization were counted as both an ED visit and a hospitalization. Outpatient visits for psychiatric care, tests, imaging, or outpatient procedures were not included.
Statistical Analysis
Baseline patient characteristics are reported as a frequency (%) for categorical variables and mean (standard deviation) for continuous variables. Mantel-Haenszel chi-square tests and generalized linear models were used to test differences in baseline characteristics between depression categories. Follow-up was calculated from HF date until death, last follow-up visit, or December 31, 2010, whichever came first.
Kaplan-Meier plots were constructed to illustrate the association of depression severity with all-cause mortality. Cox proportional hazards regression was used to describe associations between severity of depressive symptoms and mortality after adjustment for age, sex, Charlson comorbidity index, and incident vs. prevalent HF status. The proportional hazards assumption was tested using Schoenfeld residuals and found to be valid. Andersen-Gill modeling, which allows for modeling of multiple outcome events, was used to explore associations of depressive symptoms with hospitalizations and ED visits. Since outpatient visits during follow-up may cluster together (e.g. multiple outpatient visits on a given day or within in a span of several days as part of the diagnostic process or for yearly physical examinations), a time-to-event analysis such as the Andersen-Gill model, is not appropriate. Thus, the association between depression and outpatient office visits was evaluated by calculating the number of visits per person-year for each patient. A likelihood ratio test for overdispersion in the Poisson regression model examining the association between depression severity and rate of outpatient visits indicated that overdispersion existed; therefore, the negative binomial regression model was used.
A number of sensitivity analyses were also conducted. First, in an attempt to reduce the possible impact of residual confounding on the association of depression with healthcare utilization and mortality, we additionally adjusted for LVEF, eGFR, serum sodium, hypertension, use of antidepressants or heart failure medications, and hospitalizations within the last year in our fully adjusted models. Second, because responses to 2 of the questions of the PHQ-9 may be reflective of a patient’s symptoms due to their HF and not due to depression, we deleted the responses to questions 4 and 5, which asked participants how often they were bothered by ‘feeling tired or having little energy’ and ‘poor appetite or overeating.’ The totals were re-calculated after deleing these 2 questions, but the same cutpoints were used to define none-minimal, mild, and moderate-severe levels of depression. All analyses were then repeated to determine the robustness of our results. Analyses were conducted using SAS statistical software, version 9.2 (SAS Institute Inc., Cary, NC).
Results
Baseline Patient Characteristics
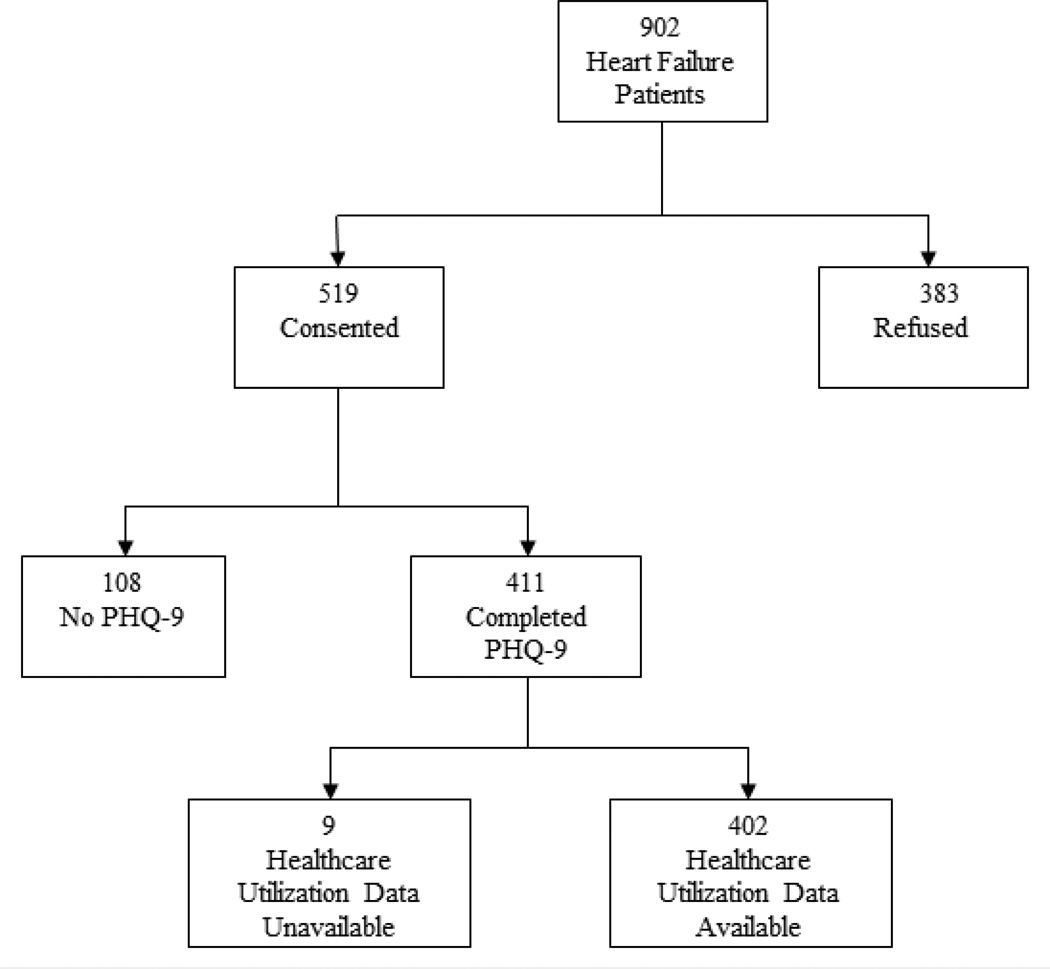
Between October 2007 and December 2010, we identified 902 HF patients, of which 402 patients (mean age 73±13 years, 58% male, 41% incident HF), were enrolled and completed all necessary components of this study (Figure 1). Of these 402 patients, 189 (47%) were identified during an inpatient visit, whereas 213 (53%) were identified during an outpatient visit. Furthermore, nearly 60% of the HF patients enrolled had prevalent HF, with a median duration of HF of 4.9 years. Greater than 50% of all patients, regardless of depression status, had a reduced EF (<50%). Sixty-two (15%) had moderate-severe depressive symptoms, 104 (26%) mild symptoms, and 236 (59%) none-minimal symptoms. Among the inpatients, 11%, 28%, and 61% had moderate-severe, mild, and none-minimal depression; the respective proportions were 19%, 24%, and 56% in the outpatients. No significant differences in baseline characteristics were observed between depression categories, with the exception of an increasing proportion of diabetes and current or former smoking status in those with more severe depression (Table 1). As expected, there was an increased use of antidepressants among patients with more severe depression. Interestingly, only 37.1% of patients with moderate-severe depression were on antidepressant medication.
Figure 1.
Heart Failure Participant Enrollment
Table 1.
Baseline Patient Characteristics by Severity of Depressive Symptoms
| Total (N=402) |
None-Minimal (N=236) |
Mild (N=104) |
Moderate-Severe (N=62) |
P-value | |
|---|---|---|---|---|---|
| Socio-demographic variable | |||||
| Age (years), mean (SD) | 73.3 (13.2) | 74.4 (12.6) | 71.8 (13.8) | 71.4 (14.2) | 0.054 |
| Male, % | 57.7 | 56.4 | 61.5 | 56.5 | 0.743 |
| Marital status, % | |||||
| Married | 59.1 | 59.1 | 61.5 | 54.8 | 0.044 |
| Widowed | 23.2 | 26.4 | 15.4 | 24.2 | |
| Divorced | 10.0 | 6.4 | 14.4 | 16.1 | |
| Single | 7.7 | 8.1 | 8.7 | 4.8 | |
| Education, % | 0.728 | ||||
| Non high school graduate | 14.2 | 15.2 | 12.7 | 13.1 | |
| High school graduate | 38.0 | 37.1 | 35.3 | 45.9 | |
| Some college / college degree | 37.5 | 37.5 | 38.2 | 36.1 | |
| Graduate school | 10.3 | 10.3 | 13.7 | 4.9 | |
| Cardiovascular risk factors | |||||
| Hypertension, % | 90.3 | 89.0 | 93.3 | 90.3 | 0.481 |
| Hyperlipidemia,% | 81.8 | 80.5 | 81.7 | 87.1 | 0.266 |
| Current or former smoking, % | 60.4 | 55.9 | 64.4 | 71.0 | 0.019 |
| Diabetes mellitus, % | 39.2 | 34.0 | 44.2 | 50.0 | 0.010 |
| Body mass index (kg/m2), % | 0.852 | ||||
| Normal (<25) | 22.3 | 21.7 | 24.0 | 21.3 | |
| Overweight (25 to <30) | 31.3 | 31.5 | 33.7 | 26.2 | |
| Obese (≥30) | 46.5 | 46.8 | 42.3 | 52.5 | |
| Comorbidities | |||||
| Myocardial infarction, % | 26.6 | 25.4 | 25.0 | 33.9 | 0.268 |
| Charlson index score, % | 0.457 | ||||
| 0 | 8.2 | 9.7 | 7.7 | 3.2 | |
| 1–2 | 22.6 | 20.8 | 25.0 | 25.8 | |
| ≥3 | 69.2 | 69.5 | 67.3 | 71.0 | |
| Estimated glomerular filtration rate, mL/min per 1.73 m2, mean (SD) | 57.2 (22.8) | 58.6 (22.8) | 54.7 (22.2) | 56.1 (23.4) | 0.267 |
| Serum sodium, mmol/L, mean (SD) | 138.2 (4.1) | 138.3 (3.9) | 138.0 (4.4) | 137.9 (4.1) | 0.009 |
| Heart failure characteristics | |||||
| Prevalent heart failure, % | 59.5 | 54.7 | 64.4 | 69.4 | 0.017 |
| Ejection fraction (<50%), % | 53.2 | 50.4 | 56.7 | 58.1 | 0.197 |
| Treatments | |||||
| Beta blockers, % | 84.8 | 83.9 | 88.5 | 82.3 | 0.911 |
| Angiotensin converting enzyme inhibitors/angiotensin II receptor blockers | 67.7 | 68.2 | 65.4 | 69.4 | 0.969 |
| Statins, % | 58.7 | 59.7 | 54.8 | 61.3 | 0.908 |
| Antidepressants, % | 24.4 | 18.2 | 30.8 | 37.1 | 0.001 |
Depression and Healthcare Utilization
Over a mean follow-up of 1.6 years, 781 hospitalizations, 1000 ED visits, and 15,515 outpatient office visits occurred. Hospitalizations after HF ranged from 0–18 (median 1) per person, ED visits ranged from 0–32 (median 2), and outpatient office visits ranged from 1–189 (median 30). Sixty-seven percent of hospitalizations were preceded by ED visits, while 53% of ED visits resulted in hospitalizations. There were more hospitalizations and ED visits with increasing severity of depressive symptoms, contrasting with a more modest effect on outpatient office visits (Table 2). Compared to patients with none-minimal depression, patients with mild depressive symptoms demonstrated a marginal increase in hospitalizations (hazard ratio (HR) 1.16, 95% CI 0.88–1.53), ED visits (HR 1.35, 95% CI 1.00–1.83), and outpatient visits (risk ratio (RR) 1.04, 95% CI 0.89–1.21) after adjustment for age, sex, comorbidity, and incident vs. prevalent HF status. Patients with moderate-severe depression demonstrated nearly a 2-fold increased risk of hospitalizations (HR 1.79, 95% CI 1.30–2.47) and ED visits (HR 1.83, 95% CI 1.34–2.50) compared to those with none-minimal depression (P for trend, 0.001 and <0.001 respectively). A modest increase in outpatient office visits was also apparent among moderate-severely depressed HF patients, keeping in mind that psychiatric care related visits were excluded (RR 1.20, 95% CI 1.00–1.45, P for trend =0.068).
Table 2.
Rates and Hazard Ratios* (95% CI) or Rate Ratios† (95% CI) for Healthcare Utilization by Severity of Depression
| Severity of Depressive Symptoms | ||||
|---|---|---|---|---|
| None-Minimal | Mild | Moderate-Severe | P for trend | |
| Hospitalizations | ||||
| Rate‡ | 1.05 | 1.23 | 2.04 | |
| Crude | 1.00 (ref) | 1.20 (0.91–1.59) | 1.90 (1.36–2.64) | <0.001 |
| Fully-Adjusted§ | 1.00 (ref) | 1.16 (0.88– 1.53) | 1.79 (1.30– 2.47) | 0.001 |
| Emergency Department Visits | ||||
| Rate‡ | 1.43 | 1.93 | 2.66 | |
| Crude | 1.00 (ref) | 1.36 (1.02–1.82) | 1.83 (1.36–2.46) | <0.001 |
| Fully-Adjusted§ | 1.00 (ref) | 1.35 (1.00– 1.83) | 1.83 (1.34–2.50) | <0.001 |
| Outpatient Visits | ||||
| Rate‡ | 23.46 | 25.66 | 28.37 | |
| Crude | 1.00 (ref) | 1.05 (0.90–1.23) | 1.24 (1.03– 1.50) | 0.029 |
| Fully-Adjusted§ | 1.00 (ref) | 1.04 (0.89–1.21) | 1.20 (1.00– 1.45) | 0.068 |
For hospitalizations and emergency department visits.
For outpatient visits.
Crude event rate per person-year.
Adjusted for: age, sex, Charlson comorbidity index, and incident vs. prevalent HF status.
Outpatient Visits exclude psychiatric care, tests, imaging, and outpatient procedures.
Depression and Mortality
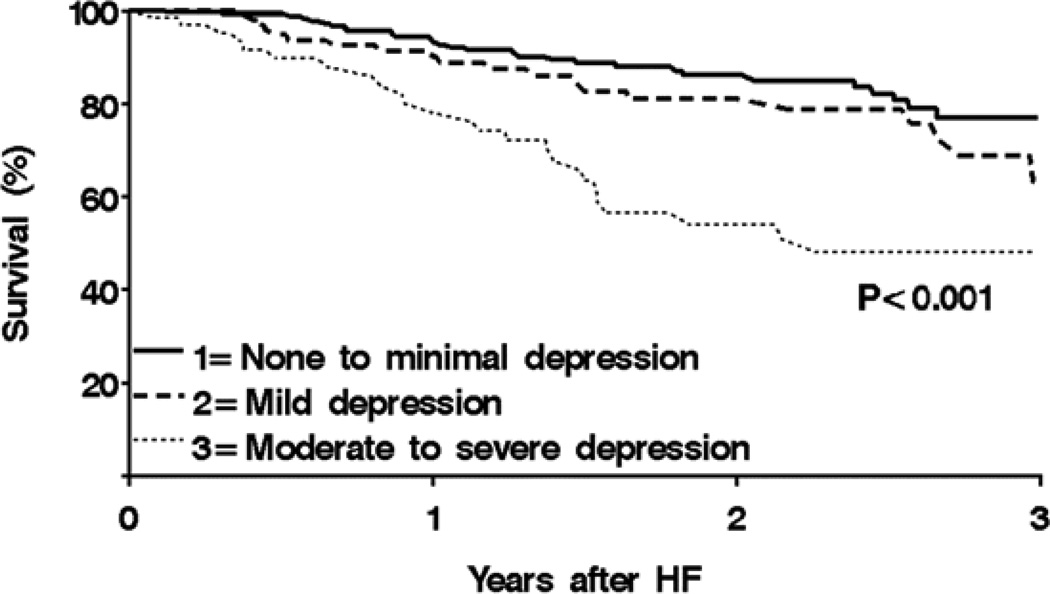
Within the 402 study participants, 74 deaths occurred. There was a strong positive and graded association between depressive symptom severity and mortality (P for trend <0.001, Figure 2). In fully-adjusted models, moderate-severe depression was associated with a 4-fold increased risk of all-cause mortality compared to none-minimal depression (HR 4.06, 95% CI 2.35–7.01). Mild depression was associated with a more modest increased risk of mortality (HR 1.59, 95% CI 0.89–2.83, Table 3).
Figure 2.
All-Cause Mortality in Heart Failure Patients by Severity of Depression
Table 3.
Rates and Hazard Ratios (95% CI) for All-Cause Mortality by Severity of Depression
| Severity of Depressive Symptoms | ||||
|---|---|---|---|---|
| None-Minimal | Mild | Moderate-Severe | P for trend | |
| All-Cause Mortality | ||||
| Rate* | 7.76 | 11.69 | 26.36 | |
| Crude | 1.00 (ref) | 1.50 (0.85–2.65) | 3.37 (1.97– 5.75) | <0.001 |
| Fully-Adjusted† | 1.00 (ref) | 1.59 (0.89–2.83) | 4.06 (2.35–7.01) | <0.001 |
Crude death rate per 100 person-years.
Adjusted for: age, sex, Charlson comorbidity index, and incident vs. prevalent HF status.
Sensitivity Analyses
Additional adjustment for LVEF, eGFR, serum sodium, hypertension, hospitalizations within the last year, and the use of antidepressants or heart failure related medications, including beta-blockers, angiotensin converting enzyme inhibitors, angiotensin receptor blockers, or statins, did not alter results for healthcare utilization or all-cause mortality. After the removal of 2 questions on the PHQ-9 that may be related to symptoms of HF, 306 people were classified as none-minimal depression, 69 had mild depression, and only 27 patients remained in the moderate-severe depression category. While the associations of depression with each measure of healthcare utilization remained the same, the hazard ratio for all-cause mortality became higher for those categorized as mildly depressed (HR 3.07, 95% CI 1.80–5.22 for mild and HR 3.72, 95% CI 1.92–7.23 for moderate-severe in the fully-adjusted model).
Discussion
Depression Prevalence in HF
In this community-based HF cohort, depression was frequent in HF patients, with 26% of patients reporting mild depressive symptoms and 15% reporting moderate-severe depressive symptoms, and its presence and severity was not related to HF characteristics. Although reported prevalence of depression in HF are variable,5 our findings are similar to the 15–20% rate of major depression cited in studies of coronary artery disease (CAD).30, 31 Importantly, the rate of depression in our HF patients was 2 to 3 times the estimated rate in the general population.2 Interestingly, despite the high prevalence of depression in HF patients, of those reporting mild and moderate-severe depressive symptoms at study enrollment, only approximately 1/3 were on antidepressant medications at that time. Although it is possible that some patients were receiving a non-pharmacologic therapy, this finding raises the possibility that depression might be under-recognized and undertreated in these patients.
Depression, Healthcare Utilization, and Mortality in HF
Within our cohort, patients with moderate-severe depression had nearly double the rate of hospitalizations and ED visits, in contrast with only a modest increase in outpatient visits compared to those with none-minimal depression. Depression is known to have a strong impact on patient behaviors, particularly among the more severely depressed. Psychosocial stressors contribute to increased smoking and alcohol abuse, poor diet, physical inactivity, and poor medication adherence, all behaviors that are risk factors for cardiovascular deterioration.32, 33 These behavioral changes could at least partially explain why these patients have increased healthcare utilization.
In addition, patients with moderate-severe depression had a four-fold increased risk of all-cause mortality compared to none-minimal depression. Just as depression is associated with negative behavioral changes, it can also cause deleterious physiologic and hormonal changes. Depressed states have been shown to induce sympathetic activation, hypercortisolemia and other metabolic abnormalities, increased heart rhythm disturbances, hypercoagulability, endothelial dysfunction, and a state of elevated proinflammatory cytokines including interleukin (IL)-6, tumor necrosis factor (TNF)-alpha, and IL-1β .2, 34, 35 The effects of neurohormonal dysregulation and a pro-inflammatory state over time have been hypothesized to adversely affect the failing heart,2, 36–38 which could be part of the mechanism underlying the increased cardiovascular mortality in depressed HF patients. However, other causes of mortality were also increased in these patients, suggesting that the physiologic changes occurring in depression negatively affect other organ systems as well. Finally, as the hypothetical pathways are complex, the elevation of cytokines that occurs in HF may play a role in the genesis of depression. In this scenario, depression itself may not have a strong impact on survival as depression may be a symptom of cytokine activation rather than a cause.
The finding of higher rates of hospitalizations and mortality among depressed HF patients are congruent with findings from several prior studies of HF as well as CAD patients.5, 8, 13, 19, 39, 40 However, only limited data exist for ED and outpatient office visits.41, 42 Although hospitalizations are considered to be one of the largest expenditures in HF patients,1 outpatient and ED visits are also important contributors to the excess cost associated with depression in HF and ED visits denote care seeking behaviors often leading to hospitalizations.
Clinical Implications
In this study, only about 1/3 of patients with mild and moderate-severe depression were on antidepressants. These data resonate with prior reports suggesting that depression is under-recognized and undertreated in practice.5, 43 We acknowledge that the most effective ways to assess and manage depression in HF remain to be fully defined as there are limited data investigating options to treat depression in HF and uncertainties about impact on outcomes.5 A trial of the antidepressant sertraline showed relative efficacy with 44.3% remission, as well as decreased hospitalizations and nonfatal cardiovascular events.44 However, non-pharmacologic treatments may also be helpful, as exercise programs have been shown to favorably impact cytokines, which are elevated with depression.45, 46 It is likely that clinical approaches will be most effective when tailored to individual patients’ profiles. Regardless of uncertainties surrounding the optimal treatment approach, the present data underscore that depression is a key driver of health care utilization in HF thereby delineating an opportunity for a greater emphasis on managing depression to reduce acute care use.
Limitations and Strengths
Several limitations should be acknowledged. Depressive symptoms were measured only at enrollment and therefore we cannot account for temporal changes in depressive symptoms. Likewise, medications were only available at baseline, and treatments for depression other than anti-depressant medications were unavailable. Some of the symptoms of depression overlap with common symptoms of HF including fatigue, low energy, psychomotor retardation, and difficulty sleeping or insomnia,2, 47 a limitation that is common to all studies of depression in HF. Additionally, participants willing to enroll in the study and complete questionnaires may differ from non-participants. While it is possible that some healthcare utilization may have occurred outside of Olmsted County, in our experience, such under-ascertainment is minimal and would not have impacted our results. Finally, the population of southeastern Minnesota is chiefly white and thus, our results should be examined in other racial groups.
Despite potential limitations, this study has a number of unique strengths including its defined cohort of HF patients, prospectively recruited from the community with validated HF diagnoses. In addition, through the record-linkage system of the REP, we captured most healthcare utilization among participants, allowing us to analyze ED and outpatient office visits, indicators of health resource use rarely evaluated in prior studies. This enabled the categorization of healthcare utilization patterns into chronic (outpatient visits) and acute (ED and hospitalization) care. In doing so, we identified that the striking impact of depression on acute care use contrasted with a more modest increase in chronic care. This adds support for recasting care models for depression in HF towards more proactive management in primary care, as had been done in some settings.48
Conclusions
Depression is frequent among HF patients in the community and is associated with a large increase in acute healthcare utilization and mortality. Further research is warranted to develop more effective clinical approaches for management of depressed HF patients.
Heart failure (HF) affects nearly 6 million Americans and is one of the most costly health care problems in the United States. Depression is a potentially modifiable risk factor that may increase the risk of healthcare utilization and death in patients with HF. However, results from previous studies are inconsistent and information on the association of depression with healthcare utilization measures other than hospitalizations, such as outpatient and emergency department visits, are lacking. Therefore, this study was designed to address the impact of depression on hospitalizations, emergency department visits, outpatient visits, and mortality in a prospective community-based cohort study of 402 HF patients from Olmsted County, MN from 2007–2010. Among the 402 HF patients, 62 had moderate-severe depressive symptoms, 104 had mild symptoms, and 236 had none-minimal symptoms. Over a mean follow-up of 1.6 years, 781 hospitalizations, 1000 ED visits, 15,515 outpatient office visits, and 74 deaths occurred. HF patients with moderate-severe depression exhibited a nearly a 2-fold increased risk of hospitalizations and emergency department visits, a modest 20% increase in outpatient visits, and a 4-fold increase in all-cause mortality compared to patients with none-minimal depression. Thus, greater recognition and management of depression in HF may optimize clinical outcomes and resource utilization in these patients.
Acknowledgements
We thank Annette L. McNallan, RN, Kay A. Traverse, RN and Ellen E. Koepsell, RN for assistance with participant enrollment and data collection, Ruoxiang Jiang and Jill M. Killian for assistance with statistical analysis, and Deborah S. Russell for secretarial assistance.
Sources of Funding
This study was supported by grants from the National Institutes of Health (R01 HL72435) and the National Institute on Aging (R01 AG034676). The funding sources played no role in the design, conduct, or reporting of this study.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosures
None.
References
- 1.Roger VL, Go AS, Lloyd-Jones DM, Adams RJ, Berry JD, Brown TM, Carnethon MR, Dai S, de Simone G, Ford ES, Fox CS, Fullerton HJ, Gillespie C, Greenlund KJ, Hailpern SM, Heit JA, Ho PM, Howard VJ, Kissela BM, Kittner SJ, Lackland DT, Lichtman JH, Lisabeth LD, Makuc DM, Marcus GM, Marelli A, Matchar DB, McDermott MM, Meigs JB, Moy CS, Mozaffarian D, Mussolino ME, Nichol G, Paynter NP, Rosamond WD, Sorlie PD, Stafford RS, Turan TN, Turner MB, Wong ND, Wylie-Rosett J. Heart Disease and Stroke Statistics--2011 update: A report from the American Heart Association. Circulation. 2011;123:e18–e209. doi: 10.1161/CIR.0b013e3182009701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Joynt KE, Whellan DJ, O'Connor CM. Why is depression bad for the failing heart? A review of the mechanistic relationship between depression and heart failure. J Card Fail. 2004;10:258–271. doi: 10.1016/j.cardfail.2003.09.008. [DOI] [PubMed] [Google Scholar]
- 3.Rich MW, Beckham V, Wittenberg C, Leven CL, Freedland KE, Carney RM. A multidisciplinary intervention to prevent the readmission of elderly patients with congestive heart failure. N Engl J Med. 1995;333:1190–1195. doi: 10.1056/NEJM199511023331806. [DOI] [PubMed] [Google Scholar]
- 4.Krumholz HM, Parent EM, Tu N, Vaccarino V, Wang Y, Radford MJ, Hennen J. Readmission after hospitalization for congestive heart failure among Medicare beneficiaries. Arch Intern Med. 1997;157:99–104. [PubMed] [Google Scholar]
- 5.Rutledge T, Reis VA, Linke SE, Greenberg BH, Mills PJ. Depression in heart failure a meta-analytic review of prevalence, intervention effects, and associations with clinical outcomes. J Am Coll Cardiol. 2006;48:1527–1537. doi: 10.1016/j.jacc.2006.06.055. [DOI] [PubMed] [Google Scholar]
- 6.Musselman DL, Evans DL, Nemeroff CB. The relationship of depression to cardiovascular disease: Epidemiology, biology, and treatment. Arch Gen Psychiatry. 1998;55:580–592. doi: 10.1001/archpsyc.55.7.580. [DOI] [PubMed] [Google Scholar]
- 7.Effects of treating depression and low perceived social support on clinical events after myocardial infarction: The Enhancing Recovery in Coronary Heart Disease Patients (ENRICHD) randomized trial. JAMA. 2003;289:3106–3116. doi: 10.1001/jama.289.23.3106. [DOI] [PubMed] [Google Scholar]
- 8.Jiang W, Alexander J, Christopher E, Kuchibhatla M, Gaulden LH, Cuffe MS, Blazing MA, Davenport C, Califf RM, Krishnan RR, O'Connor CM. Relationship of depression to increased risk of mortality and rehospitalization in patients with congestive heart failure. Arch Intern Med. 2001;161:1849–1856. doi: 10.1001/archinte.161.15.1849. [DOI] [PubMed] [Google Scholar]
- 9.Freedland KE, Rich MW, Skala JA, Carney RM, Davila-Roman VG, Jaffe AS. Prevalence of depression in hospitalized patients with congestive heart failure. Psychosom Med. 2003;65:119–128. doi: 10.1097/01.psy.0000038938.67401.85. [DOI] [PubMed] [Google Scholar]
- 10.Frasure-Smith N, Lesperance F, Habra M, Talajic M, Khairy P, Dorian P, Roy D. Elevated depression symptoms predict long-term cardiovascular mortality in patients with atrial fibrillation and heart failure. Circulation. 2009;120:134–140. doi: 10.1161/CIRCULATIONAHA.109.851675. [DOI] [PubMed] [Google Scholar]
- 11.Jiang W, Kuchibhatla M, Cuffe MS, Christopher EJ, Alexander JD, Clary GL, Blazing MA, Gaulden LH, Califf RM, Krishnan RR, O'Connor CM. Prognostic value of anxiety and depression in patients with chronic heart failure. Circulation. 2004;110:3452–3456. doi: 10.1161/01.CIR.0000148138.25157.F9. [DOI] [PubMed] [Google Scholar]
- 12.Rumsfeld JS, Havranek E, Masoudi FA, Peterson ED, Jones P, Tooley JF, Krumholz HM, Spertus JA. Depressive symptoms are the strongest predictors of short-term declines in health status in patients with heart failure. J Am Coll Cardiol. 2003;42:1811–1817. doi: 10.1016/j.jacc.2003.07.013. [DOI] [PubMed] [Google Scholar]
- 13.Murberg TA, Furze G. Depressive symptoms and mortality in patients with congestive heart failure: A six-year follow-up study. Med Sci Monit. 2004;10:CR643–CR648. [PubMed] [Google Scholar]
- 14.Song EK, Lennie TA, Moser DK. Depressive symptoms increase risk of rehospitalisation in heart failure patients with preserved systolic function. J Clin Nurs. 2009;18:1871–1877. doi: 10.1111/j.1365-2702.2008.02722.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sherwood A, Blumenthal JA, Trivedi R, Johnson KS, O'Connor CM, Adams KF, Jr, Dupree CS, Waugh RA, Bensimhon DR, Gaulden L, Christenson RH, Koch GG, Hinderliter AL. Relationship of depression to death or hospitalization in patients with heart failure. Arch Intern Med. 2007;167:367–373. doi: 10.1001/archinte.167.4.367. [DOI] [PubMed] [Google Scholar]
- 16.Friedmann E, Thomas SA, Liu F, Morton PG, Chapa D, Gottlieb SS. Relationship of depression, anxiety, and social isolation to chronic heart failure outpatient mortality. Am Heart J. 2006;152:940.e1–940.e8. doi: 10.1016/j.ahj.2006.05.009. [DOI] [PubMed] [Google Scholar]
- 17.Macchia A, Monte S, Pellegrini F, Romero M, D'Ettorre A, Tavazzi L, Tognoni G, Maggioni AP. Depression worsens outcomes in elderly patients with heart failure: An analysis of 48,117 patients in a community setting. Eur J Heart Fail. 2008;10:714–721. doi: 10.1016/j.ejheart.2008.05.011. [DOI] [PubMed] [Google Scholar]
- 18.Tsuchihashi-Makaya M, Kato N, Chishaki A, Takeshita A, Tsutsui H. Anxiety and poor social support are independently associated with adverse outcomes in patients with mild heart failure. Circ J. 2009;73:280–287. doi: 10.1253/circj.cj-08-0625. [DOI] [PubMed] [Google Scholar]
- 19.Vaccarino V, Kasl SV, Abramson J, Krumholz HM. Depressive symptoms and risk of functional decline and death in patients with heart failure. J Am Coll Cardiol. 2001;38:199–205. doi: 10.1016/s0735-1097(01)01334-1. [DOI] [PubMed] [Google Scholar]
- 20.Koenig HG. Depression in hospitalized older patients with congestive heart failure. Gen Hosp Psychiatry. 1998;20:29–43. doi: 10.1016/s0163-8343(98)80001-7. [DOI] [PubMed] [Google Scholar]
- 21.Pelle AJ, Gidron YY, Szabo BM, Denollet J. Psychological predictors of prognosis in chronic heart failure. J Card Fail. 2008;14:341–350. doi: 10.1016/j.cardfail.2008.01.004. [DOI] [PubMed] [Google Scholar]
- 22.Faller H, Stork S, Schowalter M, Steinbuchel T, Wollner V, Ertl G, Angermann CE. Depression and survival in chronic heart failure: Does gender play a role? Eur J Heart Fail. 2007;9:1018–1023. doi: 10.1016/j.ejheart.2007.06.011. [DOI] [PubMed] [Google Scholar]
- 23.St Sauver JL, Grossardt BR, Yawn BP, Melton LJ, 3rd, Rocca WA. Use of a medical records linkage system to enumerate a dynamic population over time: The Rochester Epidemiology Project. Am J Epidemiol. 2011;173:1059–1068. doi: 10.1093/aje/kwq482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bursi F, Weston SA, Redfield MM, Jacobsen SJ, Pakhomov S, Nkomo VT, Meverden RA, Roger VL. Systolic and diastolic heart failure in the community. JAMA. 2006;296:2209–2216. doi: 10.1001/jama.296.18.2209. [DOI] [PubMed] [Google Scholar]
- 25.Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, Jr, Jones DW, Materson BJ, Oparil S, Wright JT, Jr, Roccella EJ. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: The JNC 7 report. JAMA. 2003;289:2560–2572. doi: 10.1001/jama.289.19.2560. [DOI] [PubMed] [Google Scholar]
- 26.American Diabetes Association. Standards of medical care in diabetes--2006. Diabetes Care. 2006;29(Suppl 1):S4–S42. [PubMed] [Google Scholar]
- 27.Levey AS, Coresh J, Greene T, Stevens LA, Zhang YL, Hendriksen S, Kusek JW, Van Lente F. Using standardized serum creatinine values in the Modification of Diet in Renal Disease Study equation for estimating glomerular filtration rate. Ann Intern Med. 2006;145:247–254. doi: 10.7326/0003-4819-145-4-200608150-00004. [DOI] [PubMed] [Google Scholar]
- 28.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. J Chronic Dis. 1987;40:373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 29.Kroenke K, Spitzer RL, Williams JB. The PHQ-9: Validity of a brief depression severity measure. J Gen Intern Med. 2001;16:606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Schleifer SJ, Macari-Hinson MM, Coyle DA, Slater WR, Kahn M, Gorlin R, Zucker HD. The nature and course of depression following myocardial infarction. Arch Intern Med. 1989;149:1785–1789. [PubMed] [Google Scholar]
- 31.Rozanski A, Blumenthal JA, Kaplan J. Impact of psychological factors on the pathogenesis of cardiovascular disease and implications for therapy. Circulation. 1999;99:2192–2217. doi: 10.1161/01.cir.99.16.2192. [DOI] [PubMed] [Google Scholar]
- 32.Figueredo VM. The time has come for physicians to take notice: The impact of psychosocial stressors on the heart. Am J Med. 2009;122:704–712. doi: 10.1016/j.amjmed.2009.05.001. [DOI] [PubMed] [Google Scholar]
- 33.Rozanski A, Blumenthal JA, Davidson KW, Saab PG, Kubzansky L. The epidemiology, pathophysiology, and management of psychosocial risk factors in cardiac practice: The emerging field of behavioral cardiology. J Am Coll Cardiol. 2005;45:637–651. doi: 10.1016/j.jacc.2004.12.005. [DOI] [PubMed] [Google Scholar]
- 34.Irwin M. Psychoneuroimmunology of depression: Clinical implications. Brain Behav Immun. 2002;16:1–16. doi: 10.1006/brbi.2001.0654. [DOI] [PubMed] [Google Scholar]
- 35.Leonard BE. Stress, norepinephrine and depression. J Psychiatry Neurosci. 2001;26(Suppl):S11–S16. [PMC free article] [PubMed] [Google Scholar]
- 36.Oral H, Kapadia S, Nakano M, Torre-Amione G, Lee J, Lee-Jackson D, Young JB, Mann DL. Tumor necrosis factor-alpha and the failing human heart. Clin Cardiol. 1995;18:IV20–IV27. doi: 10.1002/clc.4960181605. [DOI] [PubMed] [Google Scholar]
- 37.Roberts AB, Roche NS, Winokur TS, Burmester JK, Sporn MB. Role of transforming growth factor-beta in maintenance of function of cultured neonatal cardiac myocytes. Autocrine action and reversal of damaging effects of interleukin-1. J Clin Invest. 1992;90:2056–2062. doi: 10.1172/JCI116087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Paulus WJ. Cytokines and heart failure. Heart Fail Monit. 2000;1:50–56. [PubMed] [Google Scholar]
- 39.Barth J, Schumacher M, Herrmann-Lingen C. Depression as a risk factor for mortality in patients with coronary heart disease: A meta-analysis. Psychosom Med. 2004;66:802–813. doi: 10.1097/01.psy.0000146332.53619.b2. [DOI] [PubMed] [Google Scholar]
- 40.van Melle JP, de Jonge P, Spijkerman TA, Tijssen JG, Ormel J, van Veldhuisen DJ, van den Brink RH, van den Berg MP. Prognostic association of depression following myocardial infarction with mortality and cardiovascular events: A meta-analysis. Psychosom Med. 2004;66:814–822. doi: 10.1097/01.psy.0000146294.82810.9c. [DOI] [PubMed] [Google Scholar]
- 41.Himelhoch S, Weller WE, Wu AW, Anderson GF, Cooper LA. Chronic medical illness, depression, and use of acute medical services among Medicare beneficiaries. Med Care. 2004;42:512–521. doi: 10.1097/01.mlr.0000127998.89246.ef. [DOI] [PubMed] [Google Scholar]
- 42.Fulop G, Strain JJ, Stettin G. Congestive heart failure and depression in older adults: Clinical course and health services use 6 months after hospitalization. Psychosomatics. 2003;44:367–373. doi: 10.1176/appi.psy.44.5.367. [DOI] [PubMed] [Google Scholar]
- 43.Hirschfeld RM, Keller MB, Panico S, Arons BS, Barlow D, Davidoff F, Endicott J, Froom J, Goldstein M, Gorman JM, Marek RG, Maurer TA, Meyer R, Phillips K, Ross J, Schwenk TL, Sharfstein SS, Thase ME, Wyatt RJ. The National Depressive and Manic-Depressive Association consensus statement on the undertreatment of depression. JAMA. 1997;277:333–340. [PubMed] [Google Scholar]
- 44.Jiang W, Krishnan R, Kuchibhatla M, Cuffe MS, Martsberger C, Arias RM, O'Connor CM. Characteristics of depression remission and its relation with cardiovascular outcome among patients with chronic heart failure (from the SADHART-CHF Study) Am J Cardiol. 2011;107:545–551. doi: 10.1016/j.amjcard.2010.10.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Adamopoulos S, Parissis J, Karatzas D, Kroupis C, Georgiadis M, Karavolias G, Paraskevaidis J, Koniavitou K, Coats AJ, Kremastinos DT. Physical training modulates proinflammatory cytokines and the soluble Fas/soluble Fas ligand system in patients with chronic heart failure. J Am Coll Cardiol. 2002;39:653–663. doi: 10.1016/s0735-1097(01)01795-8. [DOI] [PubMed] [Google Scholar]
- 46.LeMaitre JP, Harris S, Fox KA, Denvir M. Change in circulating cytokines after 2 forms of exercise training in chronic stable heart failure. Am Heart J. 2004;147:100–105. doi: 10.1016/j.ahj.2003.07.001. [DOI] [PubMed] [Google Scholar]
- 47.MacMahon KM, Lip GY. Psychological factors in heart failure: A review of the literature. Arch Intern Med. 2002;162:509–516. doi: 10.1001/archinte.162.5.509. [DOI] [PubMed] [Google Scholar]
- 48.Reiss-Brennan B, Briot P, Cannon W, James B. Mental health integration: Rethinking practitioner roles in the treatment of depression: The specialist, primary care physicians, and the practice nurse. Ethn Dis. 2006;16 S3-37-43. [PubMed] [Google Scholar]