Abstract
Background:
Charcot neuropathic osteoarthropathy associated foot deformity can result in joint instability, ulceration, and even amputation. The purpose of the present study was to follow patients with and without active Charcot osteoarthropathy for as long as two years to examine the magnitude and timing of foot alignment changes.
Methods:
We studied fifteen subjects with Charcot osteoarthropathy and nineteen subjects with diabetes mellitus and peripheral neuropathy without Charcot osteoarthropathy for one year; eight of the subjects with osteoarthropathy and five of the subjects with diabetes and peripheral neuropathy were followed for two years. Bilateral weight-bearing radiographs of the foot were made at baseline for all subjects, with repeat radiographs being made at six months for the osteoarthropathy group and at one and two years for both groups. Radiographic measurements included the Meary angle, cuboid height, calcaneal pitch, and hindfoot-forefoot angle.
Results:
The Meary angle, cuboid height, and calcaneal pitch worsened in feet with Charcot osteoarthropathy over one year as compared with the contralateral, uninvolved feet and feet in patients with diabetes and peripheral neuropathy. Cuboid height continued to worsen over the two-year follow-up in the feet with Charcot osteoarthropathy. These feet also had a greater change in the hindfoot-forefoot angle at one year as compared with the feet in patients with diabetes and peripheral neuropathy and at two years as compared with the contralateral, uninvolved feet.
Conclusions:
In patients with Charcot neuropathic osteoarthropathy, radiographic alignment measurements demonstrate the presence of foot deformity at the time of the initial clinical presentation and evidence of progressive changes over the first and second years. The six-month data suggest worsening of medial column alignment prior to lateral column worsening. This radiographic evidence of worsening foot alignment over time supports the need for aggressive intervention (conservative bracing or surgical fixation) to attempt to prevent limb-threatening complications.
Level of Evidence:
Prognostic Level II. See Instructions for Authors for a complete description of levels of evidence.
Charcot neuropathic osteoarthropathy is characterized by bone and joint destruction associated with peripheral neuropathy. Peripheral neuropathy can be the result of diabetes mellitus, chronic alcohol abuse, and heavy metal exposure, or it can be idiopathic1,2. The onset of Charcot arthropathy is commonly preceded by an undetected injury that initiates an uncontrolled inflammatory process. This unchecked peripheral hypervascular response is thought to contribute to reduced bone mineral density in the foot3-5. Continued weight-bearing on the injured and fragile foot can result in fracture. Charcot arthropathy is associated with a high frequency of fracture nonunion6, joint dislocation, foot deformity7-9, and skin ulceration10 and with an increased relative risk of amputation by a factor as high as twelvefold2.
The Eichenholtz classification system is used to stage Charcot arthropathy11-13. Stage 0, an addition by Shibata et al.14, is the clinical phase in which the foot is warm, swollen, and red with limited or no radiographic evidence of fracture. Stage I is the fragmentation or dislocation phase in which clinical signs continue but fractures, joint dislocations, and deformity become visible on radiographs. Stage II is the coalescence phase with resorption or fusion of bone fragments. Stage III is the consolidation phase, during which the foot becomes stable11-13,15. The Schon anatomical location classification system is used to identify deformity location7. There are four types: Type I (Lisfranc pattern), Type II (naviculocuneiform pattern), Type III (perinavicular pattern), and Type IV (transverse tarsal pattern). The location, the magnitude of deformity, and the time course are patient-specific, although it has been suggested that it can take up to twenty-four months for the foot to become stable16.
Treatment for Charcot arthropathy includes foot immobilization and offloading until Eichenholtz stage III occurs. Bracing or shoewear modifications are then required to accommodate deformity, to prevent ulceration and deformity progression, and to provide lower extremity stability for weight-bearing activities1,2,17-20. While deformity progression is a concern during stage II, the deformity is generally considered stable at stage III and further alignment change is thought to occur only with a recurrent episode of Charcot arthropathy. However, the natural history of the magnitude and duration of deformity progression has not previously been reported for this disease. The purpose of the present study was to follow patients with active Charcot arthropathy for as long as two years to examine the magnitude and timing of foot alignment changes in the sagittal and transverse planes.
Materials and Methods
Study Design Overview
Three groups of subjects were recruited for this study. The first group (designated as the CN group) included subjects who had active Charcot arthropathy of any etiology. The second group (designated as the DMPN group) included subjects with diabetes mellitus and peripheral neuropathy but without a history of Charcot arthropathy; this group provided information about alignment stability in patients at risk for the development of Charcot arthropathy. The third group (designated as the unimpaired comparison group) included subjects without diabetes mellitus, peripheral neuropathy, and Charcot arthropathy who had no known impairment. This group provided normative data for baseline alignment measurements. Foot alignment measurements were made on weight-bearing foot and ankle radiographs at baseline, six months, one year, and two years for the CN group; at baseline, one year, and two years for the DMPN group; and at baseline only for the unimpaired comparison group. The two-year follow-up duration was chosen to permit measurement of alignment changes in both the acute and chronic phases of Charcot arthropathy16,21. All subjects provided written informed consent, in compliance with the human studies protocol approved by the Human Research Protection Office at Washington University School of Medicine. All subjects were enrolled from June 2007 to August 2010 and received monetary compensation for their time.
Inclusion/Exclusion Criteria
Subjects were considered for inclusion in the CN group if they met the following criteria: (1) peripheral neuropathy (the inability to feel a 5.07 Semmes-Weinstein monofilament on at least one location on the plantar aspect of the foot or the inability to feel <25 V with use of the biothesiometer), (2) clinical signs of active Charcot arthropathy (redness, swelling, and elevated skin temperatures), and (3) radiographic evidence of active Charcot arthropathy. Patients were excluded from the CN group if they had foot amputation proximal to the phalanges or a history of osteomyelitis.
Subjects were included in the DMPN group if they met the following criteria: (1) Type-1 or 2 diabetes mellitus, (2) peripheral neuropathy as defined above, and (3) no medical history or radiographic evidence of active Charcot arthropathy. Individuals were excluded if they had a history or current clinical signs of foot disease, including plantar ulcerations, foot fractures, and/or fixed midfoot or hindfoot deformities. In addition, individuals were excluded if they were taking immunosuppressive medications or had a medical condition that might impact foot bone health (e.g., foot or leg trauma, metabolic bone disease, or a medical diagnosis of osteoporosis).
Subjects were included in the unimpaired comparison group if they met the following criteria: (1) an age of less than forty-five years, (2) no known medical condition at the time of enrollment, and, especially, (3) no medical condition that might impact foot bone health.
Subject Characteristics
CN Group
Twenty subjects with active Charcot arthropathy met the study criteria and agreed to participate, and fifteen of these subjects had complete data both at the time of the first clinical presentation (baseline) and at one year (Fig. 1 and Appendix). The majority (ten) of the subjects in the CN group with one-year data had peripheral neuropathy as a result of type-2 diabetes mellitus, whereas two patients had type-1 diabetes mellitus. The remaining three patients had idiopathic peripheral neuropathy with hemoglobin A1c (HbA1c) values in the prediabetic range (5.7% to 5.9%). Eight subjects in the CN group were able to complete baseline, six-month, one-year, and two-year testing prior to the study end date.
Fig. 1.
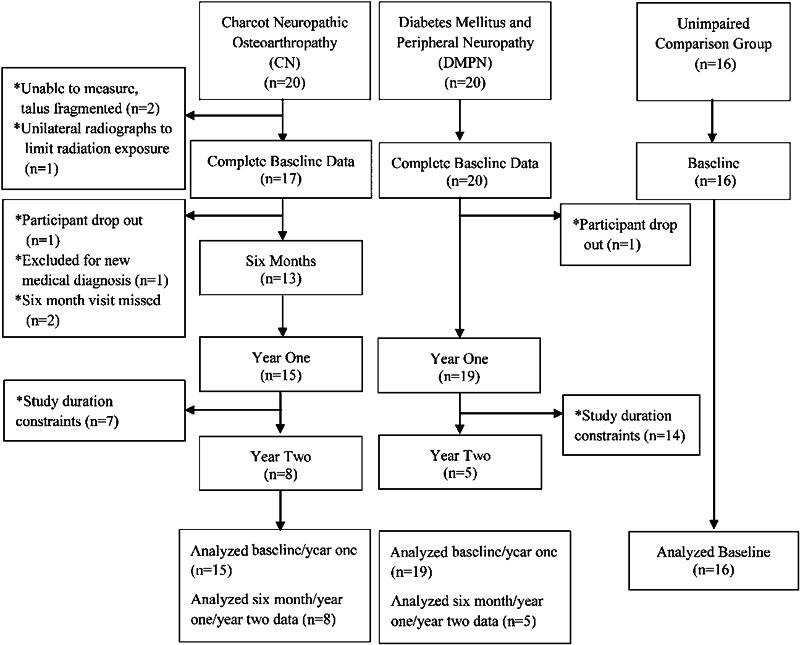
Enrollment and follow-up of the study sample.
DMPN Group
Twenty subjects met the criteria for inclusion in the DMPN group, and nineteen had complete data at baseline and at one year. Five subjects in the DMPN group had complete data at baseline, six months, one year, and two years prior to the study end date.
Unimpaired Comparison Group
Sixteen subjects in the unimpaired comparison group completed baseline testing. The involved foot was determined by means of a coin flip.
Radiographic Examination
Lateral, dorsoplantar, and oblique weight-bearing radiographs were made for all subjects. A standardized protocol was followed with the feet prealigned by the research coordinator and a radiopaque ruler included in each radiograph to adjust for magnification error. Radiographs were made at baseline for all subjects and were repeated at an average of six months (mean [and standard deviation], 0.6 ± 0.2 years), one year (mean, 1.0 ± 0.3 years), and two years (mean, 2.1 ± 0.2 years) for the CN group and at one year (mean, 1.1 ± 0.3 years) and two years (mean, 2.0 ± 0.2 years) for the DMPN group. All radiographic measurements were made by one rater (J.E.J.) as previously described20. Radiographic measurements were made with use of the iSite PACS software (Philips Healthcare Informatics, Foster City, California), which provides length measurements to the nearest 0.1 mm and angle measurements to the nearest 1°. Three measurements from the lateral radiograph provided an indication of sagittal alignment. The Meary angle (measured in degrees) is the angle between the line drawn from the center of the body of the talus bisecting the talar neck and head and the line drawn through the longitudinal axis of the first metatarsal. A negative angle represents arch lowering (Fig. 2). Cuboid height (measured in millimeters) is the distance from the most plantar aspect of the cuboid to a horizontal line drawn from the plantar calcaneal tuberosity to the fifth metatarsal head. A smaller number represents arch lowering (Fig. 2). Calcaneal pitch (measured in degrees) is the angle created by a line drawn from the calcaneal tuberosity to the plantar aspect of the distal part of the calcaneus and a horizontal line drawn from the plantar calcaneal tuberosity to the fifth metatarsal head. A smaller angle indicates arch lowering (Fig. 2). Transverse plane alignment was measured on the dorsoplantar radiograph with use of the hindfoot-forefoot angle, which is the angle between the talocalcaneal bisector and the second metatarsal shaft. A positive number represents adduction of the forefoot on the hindfoot, and a negative number represents abduction of the forefoot on the hindfoot (Fig. 2).
Fig. 2.
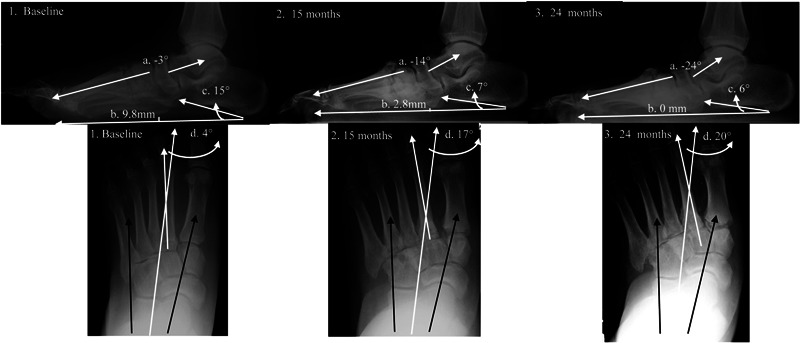
Radiographs showing the Meary angle (a), cuboid height (b), calcaneal pitch (c), and transverse plane measurements (d) at baseline (1), fifteen months (2), and twenty-four months (3) for a representative patient with Charcot arthropathy. Note the progressive decline in the Meary angle, cuboid height, and calcaneal pitch and the increase in forefoot abduction relative to the hindfoot over two years.
In our previous study, intra-rater precision was 3° for the Meary angle, 0.9 mm for cuboid height, and 2° for both calcaneal pitch and the hindfoot-forefoot angle20. The least significant change, the smallest change considered to be clinically real and not the result of chance for intra-rater measures22, was 9° for the Meary angle, 2.4 mm for cuboid height, 4° for calcaneal pitch, and 6° for the hindfoot-forefoot angle20.
Treatment of Charcot Neuropathic Osteoarthropathy
Medical treatment, including the choice of immobilization device and the duration of immobilization, was determined by each individual’s care provider. Immobilization consisted of total contact casting with transition to a removable cast walker-boot for nine subjects23 and a removable cast walker-boot only for six subjects24 (see Appendix). Nine patients received treatment from one of the authors (D.R.S.), and the remaining six subjects received treatment from providers not associated with the study (e.g., primary care physicians, community orthopaedists).
Statistical Methods
A group-by-side-by-time repeated-measures analysis of variance was performed for the sagittal radiographic measures. A group-by-side analysis of variance was performed for each baseline radiographic measure. Worsening of alignment for the hindfoot-forefoot angle could be a change into greater abduction or adduction, and therefore an absolute deviation score was calculated over Years 1 and 2, and the results were compared with repeated-measures contrasts. The baseline and one-year comparisons for each sagittal measurement resulted in seventeen comparisons and a significant Bonferroni-corrected p value of ≤0.0029, which maintained the familywise error rate at an alpha of <0.05. For the two-year comparisons, each sagittal radiographic measurement resulted in thirty comparisons and a significant Bonferroni-corrected p value of ≤0.0017. The hindfoot-forefoot comparison for Year 1 resulted in four comparisons and a significant Bonferroni-corrected p value of ≤0.0125. For the two-year comparisons of hindfoot-forefoot measurements, there were twenty-four comparisons and a significant Bonferroni-corrected p value of ≤0.0021. Results reported as p < 0.05 reflect these Bonferroni adjustments.
Source of Funding
This study was made possible by Grant Numbers R21 DK079457 and R01 DK059224 from the National Institute of Diabetes and Digestive and Kidney Diseases, K12 HD055931 from the Eunice Kennedy Shriver National Institute of Child Health and Human Development, and KL2 TR000450 from the Institute of Clinical and Translational Sciences Multidisciplinary Clinical Research Career Development Program, all of which are components of the National Institutes of Health (NIH). Its contents are solely the responsibility of the authors and do not necessarily represent the official view of NIH.
Results
CN Group Characteristics
In the CN group, thirteen subjects were classified as Eichenholtz stage I and two subjects were classified as stage II (see Appendix). According to the Schon anatomical location classification system7, seven subjects had Lisfranc joint involvement (Type I), four had transverse tarsal joint involvement (Type IV), two had naviculocuneiform joint involvement (Type II), one had perinavicular joint involvement (Type III), and one had multiple joint involvement.
Alignment: Baseline and One Year
Change Over Time
Feet with Charcot arthropathy (the involved feet in the CN group) had worsening alignment from baseline to one year in all sagittal plane deformity measurements; the changes in cuboid height and calcaneal pitch were significant (p < 0.05) (Fig. 3). The mean change in the hindfoot-forefoot angle over one year was greater in the involved feet in the CN group than in the feet in the DMPN group (p < 0.05). There was no change in any radiographic alignment measurement over one year in the uninvolved feet in the CN group or in the feet in the DMPN group.
Fig. 3.
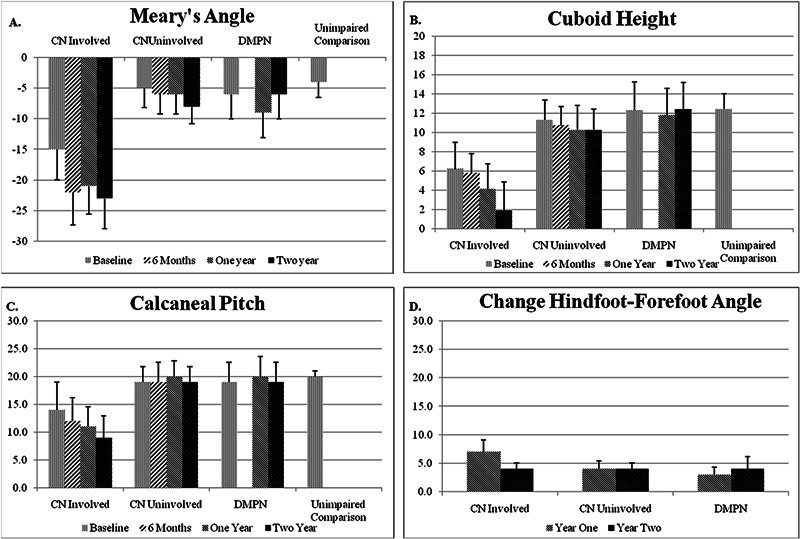
Figs. 3-A, 3-B, and 3-C Bar graphs showing the mean value (and standard error) at baseline, six months, one year, and two years for the Meary angle (Fig. 3-A), cuboid height (Fig. 3-B), and calcaneal pitch (Fig. 3-C). Fig. 3-D Bar graph showing the mean change in the hindfoot-forefoot angle over Years 1 and 2.
Group and Foot Comparisons at Baseline and One Year
The involved feet in the CN group had worse mean sagittal plane alignment than (1) the feet in the unimpaired comparison group in terms of the Meary angle and cuboid height at baseline (p < 0.05) and (2) the uninvolved feet in the CN group and the feet in the DMPN group in terms of the Meary angle, cuboid height, and calcaneal pitch at one year (p < 0.05).
Alignment: Baseline, Six Months, One Year, and Two Years
Change Over Time
The involved feet in the CN group worsened in terms of cuboid height between baseline and two years (p < 0.05). In addition, the change in the hindfoot-forefoot angle from baseline to two years was greater in the involved feet in the CN group than in the uninvolved feet in the CN group (p < 0.05). There were three nonsignificant trends in the involved feet of the CN group: (1) worsening of Meary angle occurred primarily during the first six months, (2) worsening of cuboid height occurred between six months and two years, and (3) progressive decrease in calcaneal pitch occurred over the two-year follow-up period (Fig. 3).
Changes Greater Than the Least Significant Change
The least significant change (the smallest change considered to be clinically real and not the result of chance) was calculated from previous reliability work20. In the involved feet in the CN group, alignment changes that exceeded the least significant change were observed at one year in the Meary angle (six of fifteen feet), cuboid height (seven of fifteen feet), calcaneal pitch (seven of fifteen feet), and the hindfoot-forefoot angle (five of fifteen feet). In this group, such changes were observed at two years in the Meary angle (five of eight feet), cuboid height (six of eight feet), calcaneal pitch (three of eight feet), and the hindfoot-forefoot angle (seven of eight feet). Four or fewer uninvolved feet in the CN group and three or fewer uninvolved comparison feet in the DMPN group feet had alignment changes greater than the least significant change at one and two years (Table I).
TABLE I.
One and Two-Year Outcomes: Measurements That Changed Greater Than Least Significant Change
| Measurement Change Greater Than Least Significant Change (no. of subjects) |
||||
| Meary Angle | Cuboid Height | Calcaneal Pitch | Hindfoot-Forefoot Angle | |
| CN group | ||||
| Involved | ||||
| One year (n = 15) | 6 | 7 | 7 | 5 |
| Two years (n = 8) | 5 | 6 | 3 | 7 |
| Uninvolved | ||||
| One year (n = 15) | 1 | 2 | 0 | 4 |
| Two years (n = 8) | 1 | 1 | 1 | 2 |
| DMPN group | ||||
| Matched involved | ||||
| One year (n = 15) | 0 | 0 | 0 | 2 |
| Two years (n = 8) | 0 | 0 | 0 | 2 |
| Matched uninvolved | ||||
| One year (n = 15) | 1 | 1 | 0 | 3 |
| Two years (n = 8) | 0 | 0 | 0 | 1 |
Only the involved feet in the CN group had alignment changes in three or more measurements in Year 1. One of these individuals had alignment changes in three measurements in the uninvolved foot during the two-year follow-up period and was diagnosed with active Charcot arthropathy just prior to the second-year follow-up visit. Most subjects in the DMPN group had no change in any measurement greater than the least significant change at both one year (seventeen of nineteen feet) and two years (three of five feet) (Fig. 4).
Fig. 4.
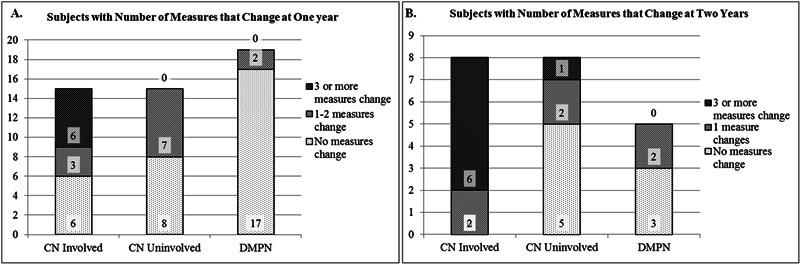
Bar graphs showing the number of subjects (indicated within the bar) with no measurements that changed (light pattern), one to two measures that changed (medium pattern), and three or more measurements that changed (dark pattern) at one year (Fig. 4-A) and two years (Fig. 4-B). Note that no individual in the control group had three or more measurements that changed over the two-year period.
Fracture Outcomes
Four subjects developed a fracture during the study period: two subjects in the CN group had a new fracture in the involved foot, one subject in the CN group developed stage-I Charcot arthropathy in the uninvolved foot, and one subject in the DMPN group developed a new foot fracture. All fractures were associated with abnormalities in the Meary angle. Two fractures occurred in subjects who had a poor Meary angle at baseline (−22° and −26°), and two fractures occurred in subjects who had a decrease of 11° in the Meary angle during the study period. Although cuboid height was ≤10 mm at baseline in three of the four subjects who had a new fracture, no other baseline alignment measurements or changes in measurements over time were consistently abnormal in the subjects with a new fracture.
Discussion
To our knowledge, the present study is the first to provide longitudinal radiographic alignment measures over one and two years for individuals with active Charcot arthropathy. Subjects with Charcot arthropathy had poor alignment at baseline, with large alignment changes occurring during the first year, despite cast and brace treatment, and evidence of smaller but continued worsening of alignment during the second year. Baseline to six-month data indicated large alignment changes along the medial column of the foot (Meary angle), with changes in alignment along the lateral column of the foot (cuboid height) occurring during the second six months and the second year.
At the time of the initial clinical presentation, the involved feet in the CN group had alignment measurements that were worse than those of the uninvolved feet in the CN group, the feet in the DMPN group, and the feet in the unimpaired comparison group. Baseline measurements in the feet with Charcot arthropathy were within the range reported by Schon et al.7 but were worse than those recently reported by Hastings et al.20. Bevan and Tomlinson10 reported a Meary angle that was similar to our baseline measurement but a cuboid height that was worse and a calcaneal pitch that was better. Differences in measured alignment between studies could be the result of a number of factors. The data in the present study were collected prospectively with use of standardized weight-bearing radiographic methods. Previous studies7,20 have been retrospective and have included non-weight-bearing radiographic measures, which likely underestimate deformity severity. In addition, deformity severity at the time of the initial clinical presentation may be related, in part, to the time between the onset of Charcot arthropathy and study enrollment, the aggressiveness of and compliance with immobilization treatment, and whether the event being tracked during the study period was a first event or a chronic recurrent event. The subjects in the CN group had long, but typical, durations between event onset and study enrollment. More than half of the subjects had removable immobilization devices that allow noncompliance, and four of the fifteen subjects had chronic recurrent Charcot arthropathy with a history of diabetes-related foot complications.
The alignment of the involved feet in the CN group worsened over one and two years, whereas the alignment remained fairly stable in the uninvolved feet in the CN group and the comparison feet in the DMPN group. The Meary angle in the involved feet in the CN group changed most during the first six months and remained stable through Year 2. A Meary angle of lower than −27° has previously been associated with the presence of an ulcer10. In the present study, three subjects had progressive worsening of the Meary angle below −27° during the first year, with one developing an ulcer. In contrast, cuboid height changed little during the first six months, with rapid changes occurring during the second six months and the second year. Calcaneal pitch showed a gradual and steady decline across all measurement periods. Lateral column involvement in all patterns of foot deformity has been documented previously7 and is clinically associated with a poor prognosis. The longitudinal data in the present study suggest a progressive pattern of lateral column involvement and highlight the need for early and aggressive treatment in an effort to prevent progressive deformity over time across the foot.
The magnitude and timing of alignment change is variable and is not readily predictable; however, our limited data provide preliminary evidence that change in alignment greater than measurement error is inevitable if sufficient follow-up occurs. By the end of two years, all eight patients with Charcot arthropathy had at least one alignment measure that exceeded the least significant change. Future research must examine factors that predict the magnitude and timing of alignment change as well as treatment options to prevent what currently results in inevitable deformity.
The present study had limitations that should be considered when interpreting the results. Most importantly, because of the small sample size, particularly for the two-year follow-up, caution should be used when applying the results to the patient population at large. Charcot arthropathy is variable in its presentation and progression. The inclusion of multiple etiologies of peripheral neuropathy as well as the lack of control of intervention may have had an unpredictable impact on deformity progression in the present study. Although all patients with Charcot arthropathy received an offloading treatment, the type and duration was not controlled, and we do not know the influence of the treatment variability on the course of the condition. Studies with larger sample sizes are needed to more fully assess the impact of group and patient-specific factors (e.g., Charcot arthropathy location, severity, and treatment type; etiology of peripheral neuropathy; comorbidities; and the temporal relationship to the onset of the Charcot arthropathy) on outcome. Another important limitation is that the two-year follow-up is insufficient to fully assess the ultimate outcome of Charcot arthropathy. Our study provides benchmark data to guide larger, multicenter studies that can provide external validity for our preliminary findings.
In conclusion, in patients with Charcot neuropathic osteoarthropathy, radiographic alignment measurements demonstrated the presence of foot deformity at the time of the initial clinical presentation. Longitudinal measures provided evidence of progression of foot deformity over the first and second years. Additionally, six-month interval data suggested that worsening medial column alignment precedes worsening lateral column alignment. The radiographic evidence of worsening foot alignment in a subset of patients with Charcot arthropathy indicates the possible need for more aggressive orthopaedic intervention to prevent limb-threatening complications resulting from severe deformity.
Appendix
A table showing baseline subject characteristics is available with the online version of this article as a data supplement at jbjs.org.
Supplementary Material
Disclosure of Potential Conflicts of Interest
A table showing baseline subject characteristics
Acknowledgments
Note: We would like to acknowledge Mary Wolfsberger and Joan Moulton for their assistance in calibrating and loading radiographic images to iSite software.
Footnotes
Disclosure: One or more of the authors received payments or services, either directly or indirectly (i.e., via his or her institution), from a third party in support of an aspect of this work. In addition, one or more of the authors, or his or her institution, has had a financial relationship, in the thirty-six months prior to submission of this work, with an entity in the biomedical arena that could be perceived to influence or have the potential to influence what is written in this work. No author has had any other relationships, or has engaged in any other activities, that could be perceived to influence or have the potential to influence what is written in this work. The complete Disclosures of Potential Conflicts of Interest submitted by authors are always provided with the online version of the article.
References
- 1.Johnson JE. Surgical treatment of neuropathic arthropathy of the foot and ankle. Instr Course Lect. 1999;48:269-77 [PubMed] [Google Scholar]
- 2.Rogers LC, Frykberg RG, Armstrong DG, Boulton AJ, Edmonds M, Van GH, Hartemann A, Game F, Jeffcoate W, Jirkovska A, Jude E, Morbach S, Morrison WB, Pinzur M, Pitocco D, Sanders L, Wukich DK, Uccioli L. The Charcot foot in diabetes. Diabetes Care. 2011 Sep;34(9):2123-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Young MJ, Marshall A, Adams JE, Selby PL, Boulton AJ. Osteopenia, neurological dysfunction, and the development of Charcot neuroarthropathy. Diabetes Care. 1995 Jan;18(1):34-8 [DOI] [PubMed] [Google Scholar]
- 4.Hastings MK, Sinacore DR, Fielder FA, Johnson JE. Bone mineral density during total contact cast immobilization for a patient with neuropathic (Charcot) arthropathy. Phys Ther. 2005 Mar;85(3):249-56 [PMC free article] [PubMed] [Google Scholar]
- 5.Piaggesi A, Rizzo L, Golia F, Costi D, Baccetti F, Ciaccio S, De Gregorio S, Vignali E, Trippi D, Zampa V, Marcocci C, Del Prato S. Biochemical and ultrasound tests for early diagnosis of active neuro-osteoarthropathy (NOA) of the diabetic foot. Diabetes Res Clin Pract. 2002 Oct;58(1):1-9 [DOI] [PubMed] [Google Scholar]
- 6.Sinacore DR, Withrington NC. Recognition and management of acute neuropathic (Charcot) arthropathies of the foot and ankle. J Orthop Sports Phys Ther. 1999 Dec;29(12):736-46 [DOI] [PubMed] [Google Scholar]
- 7.Schon LC, Weinfeld SB, Horton GA, Resch S. Radiographic and clinical classification of acquired midtarsus deformities. Foot Ankle Int. 1998 Jun;19(6):394-404 [DOI] [PubMed] [Google Scholar]
- 8.Sohn MW, Stuck RM, Pinzur M, Lee TA, Budiman-Mak E. Lower-extremity amputation risk after charcot arthropathy and diabetic foot ulcer. Diabetes Care. 2010 Jan;33(1):98-100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pecoraro RE, Reiber GE, Burgess EM. Pathways to diabetic limb amputation. Basis for prevention. Diabetes Care. 1990 May;13(5):513-21 [DOI] [PubMed] [Google Scholar]
- 10.Bevan WP, Tomlinson MP. Radiographic measures as a predictor of ulcer formation in diabetic charcot midfoot. Foot Ankle Int. 2008 Jun;29(6):568-73 [DOI] [PubMed] [Google Scholar]
- 11.Sommer TC, Lee TH. Charcot foot: the diagnostic dilemma. Am Fam Physician. 2001 Nov 1;64(9):1591-8 [PubMed] [Google Scholar]
- 12.Eichenholtz S. Charcot joints. Springfield: Thomas; 1966 [Google Scholar]
- 13.Sella EJ, Barrette C. Staging of Charcot neuroarthropathy along the medial column of the foot in the diabetic patient. J Foot Ankle Surg. 1999 Jan-Feb;38(1):34-40 [DOI] [PubMed] [Google Scholar]
- 14.Shibata T, Tada K, Hashizume C. The results of arthrodesis of the ankle for leprotic neuroarthropathy. J Bone Joint Surg Am. 1990 Jun;72(5):749-56 [PubMed] [Google Scholar]
- 15.Yu GV, Hudson JR. Evaluation and treatment of stage 0 Charcot’s neuroarthropathy of the foot and ankle. J Am Podiatr Med Assoc. 2002 Apr;92(4):210-20 [DOI] [PubMed] [Google Scholar]
- 16.de Souza LJ. Charcot arthropathy and immobilization in a weight-bearing total contact cast. J Bone Joint Surg Am. 2008 Apr;90(4):754-9 [DOI] [PubMed] [Google Scholar]
- 17.Brodsky JW. The diabetic foot. In: Coughlin M, Mann R, Saltzman C, editors. The diabetic foot. 8th edition Philadelphia: Mosby Elsevier; 2007. p 1333-68 [Google Scholar]
- 18.Johnson JE, Thomson AB. Charcot neuropathy of the foot: surgical aspects. In: Bowker JH, Pfeifer MA, editors. 7th edition Levin and O’Neal’s the diabetic foot. Philadelphia: Mosby Elsevier; 2007 [Google Scholar]
- 19.Sanders L, Frykberg R. The charcot foot. In: Bowker J, Pfeifer M, editors. Levin and O’Neal’s the diabetic foot. Philadephia: Mosby Elsevier; 2007 [Google Scholar]
- 20.Hastings MK, Sinacore DR, Mercer-Bolton N, McCormick JJ, Hildebolt CF, Prior FW, Johnson JE. Precision of foot alignment measures in Charcot arthropathy. Foot Ankle Int. 2011 Sep;32(9):867-72 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Armstrong DG, Todd WF, Lavery LA, Harkless LB, Bushman TR. The natural history of acute Charcot’s arthropathy in a diabetic foot specialty clinic. J Am Podiatr Med Assoc. 1997 Jun;87(6):272-8 [DOI] [PubMed] [Google Scholar]
- 22.Bonnick SL. Bone densitometry in clinical practice: application and interpretation. Totowa: Humana Press; 2003. p. 274-6 [Google Scholar]
- 23.Mueller MJ, Diamond JE, Sinacore DR, Delitto A, Blair VP, 3rd, Drury DA, Rose SJ. Total contact casting in treatment of diabetic plantar ulcers. Controlled clinical trial. Diabetes Care. 1989 Jun;12(6):384-8 [DOI] [PubMed] [Google Scholar]
- 24.Gutekunst DJ, Hastings MK, Bohnert KL, Strube MJ, Sinacore DR. Removable cast walker boots yield greater forefoot off-loading than total contact casts. Clin Biomech (Bristol, Avon). 2011 Jul;26(6):649-54 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Disclosure of Potential Conflicts of Interest
A table showing baseline subject characteristics


