Abstract
The aim of this pilot study was to investigate if an individualized and experiential training can promote family caregiver’s confidence (self-efficacy) in home care and symptom management. The study was conducted in a hematology/oncology unit in a southeastern regional medical center. Twenty informal cancer caregivers participated in the study. The individualized and experiential training was conducted at the bedside prior to patient’s hospital discharge. Self- efficacy in home care and cancer symptom management was measured using the Cancer Caregiver Self-Efficacy Measure (CCSE) before and after training, and at 1 week after hospital discharge of cancer patients. Results of the study showed mean CCSE increased by 41.1 points immediately after the training (Z=4.49, p <.001), and was 31.7 points higher at one week follow-up (Z=3.22, p <.01). The findings of this study suggest that individualized and experiential training may be another avenue for nurses, including home care nurses, to support family home caregiving. By helping family members in home care, favorable patient outcomes may be achieved, enabling older patients with cancer to stay longer in the comfort of their homes.
Introduction and Background
Approximately 1.5 million people in the U.S. received a diagnosis of cancer in 2007, and the majority of these were 55 and older (American Cancer Society, 2007). Most cancer care is delivered in outpatient settings, with only the sickest patients admitted to hospitals, and then discharged as quickly as possible, transferring the responsibility for the care of cancer patients onto their families or informal caregivers (Schumacher et al. 2002; Sutton, Demark-Wahnefried, Clipp, 2003). This responsibility is especially heightened because of limited discharge planning and the fact that many patients return home while still convalescing from the effects of treatments (Laizner, Yost, Barg, & McCorkle 1993; Weitzner, Jacobsen, Wagner, Friedland, & Cox, 1999). With minimal or no preparation, training, or support, informal caregivers are now expected to assume health management roles in the home and carry out medical tasks traditionally performed by professional health care providers especially by nurses (Donelan et al. 2002) and many are not confident that they can actually do so (Glajchean, 2004; Hwang et al., 2003; Osse, Vernooij-Dassen, Schade, 2006).
In their feasibility study, the authors of this paper found that an individualized experiential caregiver training in home care and cancer symptom management at the patient’s bedside prior to discharge was feasible and was well-received by family caregivers (Hendrix & Ray, 2006). More importantly, all participating family caregivers said that the format of the training facilitated an improvement in their confidence that they can care for their loved ones at home. The training required caregivers to interact, participate in problem-solving a symptom or care issue, and perform tasks under the tutelage of an expert. An individualized approach to training also makes it possible to tailor the training to the specific needs of family caregivers (Cameron, Shin, Williams, & Stewart, 2004).
This paper reports the findings of the authors’ second pilot study where the primary aim was to formally investigate if indeed an individualized and experiential training can promote family caregiver’s confidence (or self-efficacy) in home care and symptom management. The overall goal of this study was to provide preliminary findings as to the value of conducting future studies on the role of such training for family caregiver support and education.
Conceptual Framework
According to Bandura (1997), self-efficacy is the confidence or belief in one’s capabilities to organize and execute the course of action required to produce a given outcome. In the context of caregiving of a cancer patient, it is the caregiver’s confidence that she/he can provide the care that her/his loved one needs at home as well as help alleviate their loved ones’ symptoms at home. Self-efficacy is an important concept in caregiving because it is a prerequisite to the actual performance of tasks and strategies by an individual (Bandura 1986, Bandura 1997).
The individualized and experiential approach to caregiver training used in this study included various sources of self-efficacy or confidence: live modeling, performance exposure, positive appraisal, and mastery experience (Bandura 1986, Bandura 1997) (see Table 1). The knowledge and skills, as well as the contextually and personally relevant information provided by individualized and experiential training were expected to increase self-efficacy or confidence among family caregivers.
Table 1.
Sources of Self-Efficacy and Individualized, Experiential Caregiver Training
| Sources of Self-Efficacy or Confidence | Individualized, Experiential Caregiver Training |
|---|---|
| Live modeling | A caregiver observes a person who has mastered skills (expert) perform an intervention |
| Performance Exposure | Caregivers have an opportunity to do interventions requiring skills under the guidance of an expert Interactive discussions between the expert and caregiver about interventions on potential symptoms and care issues based on patient’s diagnosis and treatment, comorbidities, and functional status |
| Positive Appraisal | Training conducted at bedside provides an atmosphere that is non-threatening. Constructive feedback is given throughout the training. |
| Mastery Experience | For interventions requiring skills, caregivers are allotted enough time and guidance until interventions are successfully demonstrated. |
Methods
Setting and Sample
This pilot study was conducted in a hematology/oncology unit in a southeastern regional medical center. This unit cares primarily for patients with hematological malignancies who are admitted for chemotherapy and/or treatment of acute conditions that are cancer-related. The unit contains 31 private rooms, each with its own sink and bathroom. In addition, every room has a lounge chair that can be converted to a bed and used by a family member staying with the patient.
The study recruited family caregivers of older cancer patients aged 50 and above who had been admitted and were likely to be discharged to home. Patients who were projected to be actively dying were excluded from the study. A family caregiver was defined as an individual who lived in the same household as the cancer patient and provided the most “hands-on” care. Inclusion criteria for caregivers were: age 18 years or older; ability to talk, read, and write in English; and ability to spend time at the bedside of their cancer patients to participate in the training.
Approval for the study was obtained from the Institutional Review Board (IRB), and the targeted sample of 20 family caregivers subjects were recruited over a 6-month period. After conferring with the rounding oncologist, the principal investigator (PI) or study staff met with each patient and caregiver to explain the study and to invite participation if interested. If the caregiver was not present during the time of visit, the PI would either ask the patient for his/her caregiver’s telephone number or see the patient again during a time when the caregiver was expected to visit. Once the dyad had agreed to participate in the study, each was required to sign a consent form. Each caregiver training was scheduled as close to the discharge date as feasible. Flexibility was observed in scheduling: nights and weekends, in addition to days and weekdays, were given as options. Mileage reimbursement was provided to participating caregivers.
Caregiver Training
The individualized and experiential training was conducted by the PI, an experienced nurse, at the patient’s bedside in order to encourage patient participation. The training is a structured intervention based upon key areas relevant to home caregiving of patients with hematological malignancies (see Table 2). The intervention specially incorporated discussion topics about each key area, using a pictoral caregiving manual that the caregiver could take home (Hendrix, 2004). The intervention was also patient-centered and tailored to the needs of the specific patients so that it was most relevant and memorable.
Table 2.
Cancer Symptom Areas in Caregiver Training
| Symptoms | Topics Discussed |
|---|---|
| Prevention of Infection |
|
| Pain Control |
|
| Maintenance of Adequate Nutrition |
|
| Prevention and Management of Constipation or Diarrhea |
|
| Medication Regimen related to Cancer Symptoms |
|
For each care need or symptom, the discussion focused on nonpharmacologic interventions that could be implemented in home settings to assist the patient. The PI was flexible in the approach, accommodating specific queries by the caregiver or patient as they came. The PI also ensured that the training was interactive, encouraging dyad participation in problem-solving a specific symptom or care need. For example, for decreased appetite, the respondent (caregiver or patient) was asked for a list of foods that the patient loved to eat and taught how to make the food more palatable to the patient. If the cancer patient was a vegetarian, the discussion focused on maintaining or increasing caloric intake from plants and plant products. For prevention of infection, the dyad was asked to describe the home situation (queries included: “Do you have pets, live plants indoors?”, “Are you in frequent physical contact with your grandchildren?”, “Describe a typical day/week for the patient at home including outdoor activities”, etc.) and taught how to minimize exposure of the patient to potential pathogens.
The training combined didactic teaching and actual performance of the skills necessary to carry out home care procedures, if applicable. For intervention that required skills, the PI modeled the performance of the intervention. Afterwards, the caregiver was requested to give a return demonstration while the PI observed and offered guidance and positive feedback as necessary. For example, in the case of a patient requiring Hickman catheter care and dressing changes at home, using a chest mannequin the PI showed the proper way to (a) inspect the site for signs and symptoms of infection, (b) remove the old dressing, (c) clean the site, (d) place a new dressing, and (e) flush the catheter lines with normal saline and low-dose heparin. The caregiver was then requested to demonstrate the procedure on the mannequin or on the actual patient, if feasible. Adequate time was given for questions and the caregiver repeated the demonstrations on the mannequin until successful completion.
Measures
A Caregiver Demographic Questionnaire included gender, age, ethnicity, race, marital status, educational status, work status, relationship to patient, and years of caregiving experience.
The Cancer Caregiver Self-Efficacy (Confidence) Questionnaire in Symptom Management (CCSE) was comprised of a 23-item measure that was modified from a version utilized by Porter and colleagues for cancer caregivers (Porter, Keefe, Garst, McBride, & Baucom, 2008). Each item in the CCSE is stated as a specific behavioral task or targeted to a particular skill. For example, for central catheter care, caregivers are asked: “How confident are you that you can clean and dress the central catheter using the proper technique?”. For nausea, caregivers are asked: “If your loved one is nauseated, how confident are you that you can help in decreasing his/her nausea?”. All items are phrased in terms of can rather than will, since can is a judgment of capability while will is a statement of intention. The CCSE uses ratings on a scale of 0 (not very confident) to 10 (very confident). Higher scores indicate greater perceived self-efficacy for symptom management.
Data Collection Procedure
Data were collected before and after training, and at 1 week after hospital discharge of cancer patients. The post-training CCSE was collected within 24 hours of the training to assess accurately the changes associated with the training and minimize the effect of recall bias. Caregivers completed the post-training CCSE instrument after the PI had left the room and the instrument was then collected by a study staff the following day. The CCSE was also collected at 1 week after hospital discharge to allow a preliminary look at the trajectory of self-efficacy of family caregivers. Despite our efforts to only include those who were not pojected to die soon, four (20%) cancer patients expired within a week of hospital discharge thus accounting for only 16 CCSE datasets at 1-week follow-up.
Statistical Analysis
Categorical data were summarized as frequencies and percentages, and continuous data were summarized as means and standard deviations. Repeated-measures, mixed-effects models (Cnaan, Laird, & Slasor, 1997) were used to examine changes in self-efficacy. Two-sided p-values of < 0.05 were regarded as statistically significant. All data analyzed were done using STATA version 9.1 (STATA Press, 2005).
Results
The caregiver subjects had a mean age of 62 (range of 44 – 80 years), approximately the same age group as the cancer patients (mean age of 66, range 51 – 81 years) (see Table 3). A large majority were White, female, and spouses of cancer patients. Approximately near half of the caregivers had at least an Associate’s degree in college. Majority are currently unemployed. There was a wide variation in caregiving years from less than 1 month for a newly diagnosed husband to almost 24 years for a chronically ill mother with cancer.
Table 3.
Demographic characteristics of caregiver subjects (N=20)
| Demographic Characteristics | ||
|---|---|---|
|
| ||
| Age | 44–80 (mean age: 62) | |
|
| ||
| Gender | Female | 17 (85%) |
| Male | 3 (15%) | |
|
| ||
| Race | White | 17 (85%) |
| AA | 2 (10%) | |
| A-Indian | 1 (5%) | |
|
| ||
| Relationship with patient | Spouse | 13 (65%) |
| Children | 3 (15%) | |
| Sibling | 2 (10%) | |
| In-law | 1 (5%) | |
| Fiance | 1 (5%) | |
|
| ||
| Educational Degree | Less than high school | 2 (10%) |
| HS or GED | 9 (45%) | |
| Assoc degree | 5 (25%) | |
| Bachelor’s or higher | 4 (20%) | |
|
| ||
| Years of caregiving | 1 month – 24 years | |
The CCSE displayed good psychometric qualities. The CCSE has high internal consistency with a Cronbach’s alpha of 0.94 for this pilot study. The CCSE also exhibited construct validity: correlation between total CCSE scores and total scores of shortened version of Caregiving Preparedness Scale (Archbold & Stewart, 1990) using datasets in the authors’ ongoing caregiving study (N=70) was 0.77 (p <0.0001).
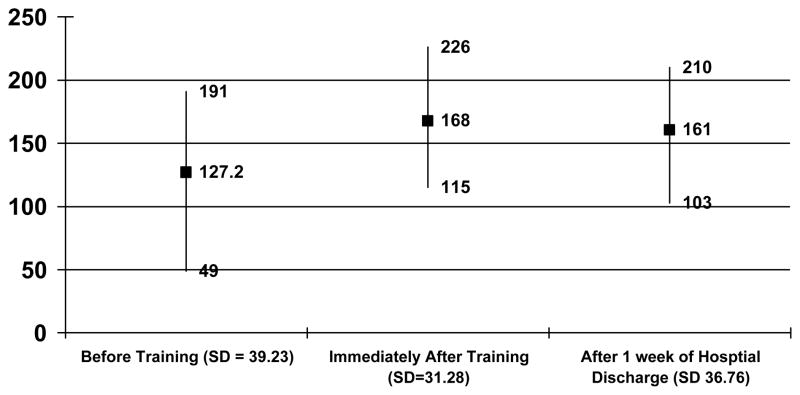
Total scores in self-efficacy (CCSE) of caregivers were significantly higher immediately post-training (z = 4.49, p < 0.001) and at 1 week post-hospital discharge of cancer patients (z = 3.22, p < 0.001). Immediately after receiving the individualized experiential training, all 20 appraised themselves as confident to highly confident as reflected by their total CCSE scores ranging from 115 to 226 (baseline total scores were between 49 – 191) (Figure 1). This level of confidence seemed to be sustained, although a bit lower, at 1 week of hospital discharge with total CCSE scores ranging from 103 to 207.
Figure 1.
CCSE Mean Scores, Range, and Standard Deviation
Discussion
Similar to the results of the authors’ feasibility study (Hendrix & Ray, 2006), this pilot study confirmed that individualized experiential training in home care and symptom management prior to hospital discharge was well received by both family caregivers and older patients with cancer. A significant number of older patients have family caregivers who stay with them or visit them almost daily throughout their hospital stay thus accessibility of family members to have bedside caregiver training was never a problematic issue. Most of the sessions ended with compliments from caregivers about the individualized approach to training since this allowed the training to be tailored to their particular needs, unlike the group approach in which caregivers are often left to decide on their own on how to apply the information learned to their particular situation (Schumacher et al., 2002). To date, many researchers have sought to develop completely structured interventions to facilitate reproducibility. While the domains or areas of needs can be predicted, the exact nature of the problems encountered require unique problem-solving for each caregiver and patient scenario. In this study, our caregivers affirmed the added-value of individualized attention. Our approach of a tailored intervention grounded in predefined areas of teaching provides requisite balance between reproducibility and patient/caregiver-centeredness.
The individualized experiential training was associated with significant improvements in self-efficacy as measured by the CCSE among family caregivers in symptom management and home care. The training may have been especially helpful since it was timed during a transition of care - from hospital to home, an event replete with confusion for patients and family caregivers (Coleman, 2003). Caregivers’ self-efficacy was most improved when measured immediately after the conduct of training. After 1 week of hospital discharge, the mean levels of self-efficacy trended down. This suggests that in addition to caregiver training prior to hospital discharge, follow-up support and training perhaps by home care nurses may be needed to ensure that the dyad’s needs are met at home (Jansma, Schure, & de Jong, 2005: Northouse 2005). Consequently, prompt and accurate communication between hospital nurses and home care nurses about patient and caregiver needs is necessary to support the patients and their family in the hospital to home transition. Home care nurses are well-positioned to further enhance self-efficacy among family caregivers and promote continuity of care by conducting formalized caregiver training at home during home visits.
Limitations
The generalizability of this pilot study is especially limited by a small sample size and without a control group. Further, the study results should be interpreted with caution since the Cancer Caregiver Self-Efficacy Scale in Cancer Symptom Management (CCSE), a modified version of Porter and colleagues self-efficacy measure for cancer caregivers (Porter et al., 2008) has not been tested on a large sample. In addition, the authors acknowledge that issues such as patients’ functional status can influence levels of self-efficacy among caregivers but these attributes were not measured. Also, no data were collected on whether patients received home care services after hospital discharge. However, the results of this study had been crucial as they provided the authors the needed foundation and direction for their ongoing funded study that rigorously evaluates the effects of individualized experiential training on caregiver’s self-efficacy in home care and symptom management. The long-term goal is to look into the cost-effectiveness of incorporating an individualized family caregiver training program as part of the standard hospital teaching given by nurses before patients are discharged from the hospital
Relevance to Clinical Practice
Caregiving education and support are largely under the purview of nurses and therefore nurses must find ways to improve the preparation of family members for home caregiving. The findings of this study suggest that one-to-one experiential training for family caregivers may be effective in increasing self-efficacy in cancer symptom management and home care. Additionally, offering the training prior to hospital discharge of their loved one may be an optimal time since hospital to home transition is often replete with problems (Coleman 2003). Having similar training immediately after hospital discharge by home care nurses may also show the same benefit as transition of care offers excellent teachable moments for both patients and their family caregivers. In the authors’ ongoing study, the hospital to home transition period is being further investigated as a key moment of training and support for patients and their family caregivers.
In this study, patient participation was encouraged as this allows both patients and caregivers to receive first-hand information and direct support to their specific needs (Northouse, 2005). In addition, involving both patients and caregivers in the training legitimizes the caregiving role of the family member. When caregivers’ involvement in cancer care is properly recognized and legitimized, it will be easier for them to attend to their own needs along with those of the patients (Morris & Thomas, 2001).
Most hospitals follow the principle that discharge planning should begin at the time of admission. However, in reality, because of demands placed on nurses in acute care settings, planning for home discharge frequently happens late and around the time of actual discharge date, and consists of teaching family caregivers in spurts as dictated by nurses’ time and workloads as well as caregivers’ accessibility. Although many caregiver studies are available in the empirical literature (see Cameron et al. 2004; Given & Sherwood 2006), to the authors’ knowledge, none has systematically looked at structured training for family caregivers prior to hospital discharge using an individualized and experiential approach similar to what was investigated in this study. As family caregivers become the bedrock of chronic care in the United States, including cancer care, nurses must keep testing ways to effectively prepare family members for home care of their loved ones. By helping family members, favorable patient outcomes may be achieved, enabling older patients with cancer to stay longer in the comfort of their homes.
Acknowledgments
The authors would like to acknowledge Linda Folsom, BSN, RN for her support in the conduct of this pilot study.
Source of Support:
This pilot study was funded by the NINR P20 NR007795 Trajectory of Aging and Care Center at Duke University School of Nursing
Contributor Information
Cristina C. Hendrix, Email: Hendr024@mc.duke.edu, Duke University School of Nursing, Nurse Investigator/Practitioner - Durham VAMC GRECC, DUMC 3322 Durham NC 27710, (919) 684- 9358 office, (919) 681-8899 fax.
Amy Abernethy, Email: Abern003@mc.duke.edu, Duke University School of Medicine.
Rick Sloane, Email: sloane@geri.duke.edu, Duke University School of Nursing.
Joey Misuraca, Email: Misur001@mc.duke.edu, Duke University Medical Center.
Joseph Moore, Email: Moore035@mc.duke.edu, Duke University School of Medicine.
References
- American Cancer Society. Cancer Facts and Figures 2007. Atlanta: American Cancer Society; 2007. [Google Scholar]
- Archbold PG, Stewart BJ. Mutuality and preparedness as predictors of caregiver role strain. Research in Nursing and Health. 1990;13(6):375–84. doi: 10.1002/nur.4770130605. [DOI] [PubMed] [Google Scholar]
- Bandura A. Self-efficacy: The exercise of control. New York: W.H. Freeman and Company; 1997. [Google Scholar]
- Bandura A. Social foundations of thought and action: a social cognitive theory. Englewood Cliffs, NJ: Prentice-Hall, Inc; 1986. [Google Scholar]
- Cameron JI, Shin JL, Williams D, Stewart DE. A brief problem-solving intervention for family caregivers to individuals with advanced cancer. Journal of Psychosomatic Research. 2004;57:137–143. doi: 10.1016/S0022-3999(03)00609-3. [DOI] [PubMed] [Google Scholar]
- Cnaan A, Laird NM, Slasor P. Using the general linear mixed model to analyse unbalanced repeated measures and longitudinal data. Statistics in Medicine. 1997;16:2349–2380. doi: 10.1002/(sici)1097-0258(19971030)16:20<2349::aid-sim667>3.0.co;2-e. [DOI] [PubMed] [Google Scholar]
- Coleman EA. Falling through the cracks: challenges and opportunities for improving transitional care for persons with continuous complex care needs. Journal of the American Geriatrics Society. 2003;51:549–555. doi: 10.1046/j.1532-5415.2003.51185.x. [DOI] [PubMed] [Google Scholar]
- Donelan K, Hill CA, Hoffman C, Scoles K, Feldman PH, Levine C, et al. Challenged to care: informal caregivers in a changing health system. Health Affairs. 2002;21(4):222–231. doi: 10.1377/hlthaff.21.4.222. [DOI] [PubMed] [Google Scholar]
- Given B, Sherwood PR. Family care for the older person with cancer. Seminar in Oncology Nursing. 2006;22(1):43–50. doi: 10.1016/j.soncn.2005.10.006. [DOI] [PubMed] [Google Scholar]
- Glajchen M. The merging role and needs of family caregivers in cancer care. The Journal of Supportive Oncology. 2004;2(2):145–155. [PubMed] [Google Scholar]
- Hendrix CC. A manual for informal caregivers on cancer symptom management. 2004. (Unpublished Manual) [Google Scholar]
- Hendrix CC, Ray S. Informal caregiver training on home care and cancer symptom management prior to hospital discharge: a feasibility study. Oncology Nursing Forum. 2006;33(4):793–797. doi: 10.1188/06.ONF.793-798. [DOI] [PubMed] [Google Scholar]
- Hwang SS, Chang VT, Alejandro Y, Osenenko O, Davis C, Cogswell J, et al. Caregiver unmet needs, burden, satisfaction in symptomatic advanced cancer patients at a Veterans Affairs Medical Center. Palliative & Supportive Care. 2003;1(4):319–329. doi: 10.1017/s1478951503030475. [DOI] [PubMed] [Google Scholar]
- Jansma FF, Schure LM, de Jong BM. Support requirements for caregivers of patients with palliative cancer. Patient Education & Counselling. 2005;58(2):182–186. doi: 10.1016/j.pec.2004.08.008. [DOI] [PubMed] [Google Scholar]
- Laizner AM, Yost LMS, Barg FK, McCorkle R. Needs of family caregivers if persons with cancer: a review. Seminar in Oncology Nursing. 1993;9:114–120. doi: 10.1016/s0749-2081(05)80107-x. [DOI] [PubMed] [Google Scholar]
- Morris SM, Thomas C. The carer’s place in the cancer situation: where does the carer stand in the medical setting. European Journal of Cancer Care. 2001;10:87–95. doi: 10.1046/j.1365-2354.2001.00249.x. [DOI] [PubMed] [Google Scholar]
- Northouse L. Helping families of patients with cancer. Oncology Nursing Forum. 2005;32(4):743–750. doi: 10.1188/05.onf.743-750. [DOI] [PubMed] [Google Scholar]
- Osse BH, Vernooij-Dassen MJ, Schade E, Grol RP. Problems experienced by the informal caregivers of cancer patients and their needs for support. Cancer Nursing. 2006;29(5):378–388. doi: 10.1097/00002820-200609000-00005. [DOI] [PubMed] [Google Scholar]
- Porter LS, Keefe FJ, Garst J, McBride CM, Baucom D. Self-efficacy for managing pain, symptoms, and function in patients with lung cancer and their informal caregivers: Associations with symptoms and distress. Pain. 2008;137(2):306–15. doi: 10.1016/j.pain.2007.09.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schumacher KL, Koresawa S, West C, Hawkins C, Johnson C, Wais E, et al. Putting cancer pain management regiments into practice at home. Journal of Pain and Symptom Management. 2002;23(5):369–382. doi: 10.1016/s0885-3924(02)00385-8. [DOI] [PubMed] [Google Scholar]
- STATA Press. STATA Reference Manual Release 9. College Station, TX: STATA Press; 2005. [Google Scholar]
- Sutton LM, Demark-Wahnefried W, Clipp EC. Management of terminal cancer in elderly patients. Lancet Oncology. 2003;4(3):149–157. doi: 10.1016/s1470-2045(03)01019-2. [DOI] [PubMed] [Google Scholar]
- Weitzner MA, Jacobsen PB, Wagner H, Friedland J, Cox C. The Caregiver Quality of Life Index – Cancer (CQOLC) scale: development and validation of an instrument to measure quality of life of the family caregiver of patients with cancer. Quality of Life Research. 1999;9:55–63. doi: 10.1023/a:1026407010614. [DOI] [PubMed] [Google Scholar]