Abstract
This review extends a prior meta-analysis of acupuncture’s utility for treating opioid detoxification, addressing the efficacy of acupuncture when combined with allopathic therapies. Both English and Chinese databases were searched for randomized trials comparing acupuncture combined with opioid agonist treatment versus opioid agonists alone for treating symptoms of opioid withdrawal. The methodological quality of each study was assessed with Jadad’s scale (1–2 = low; 3–5 = high). Meta-analysis was performed with fixed- or random-effect models in RevMan software; the outcome measures assessed were withdrawal-symptoms score, relapse rate, side effects, and medication dosage. Withdrawal-symptom scores were lower in combined treatment trials than in agonist-alone trials on withdrawal days 1, 7, 9, and 10. Combined treatment also produced lower reported rates of side effects and appeared to lower the required dose of opioid agonist. There was no significant difference on relapse rate after 6 months. This meta-analysis suggests that acupuncture combined with opioid agonists can effectively be used to manage the withdrawal symptoms. One limitation of this meta-analysis is the poor quality of the methodology of some included trials. High-quality studies are needed to confirm findings regarding the side effects and medication dosage.
Keywords: Acupuncture, Opioid, Detoxification, Meta-analysis
Introduction
Acupuncture is a traditional Chinese medical treatment developed over 2,000 years ago, in which needles are inserted into the skin to stimulate specific points. Related, needle-free techniques provide stimulation through manual application of pressure (acupressure), electrical charge, or a laser beam (Linde et al. 2001). For at least the past 30 years, acupuncture has been used internationally to treat drug-abuse and dependence (Wen and Teo 1975; Wen 1977). For instance, auricular acupuncture treatment is available at over 400 substance-abuse clinics in the United States and Europe.
However, acupuncture’s efficacy as a drug-abuse treatment has been the subject of conflicting findings in clinical trials; some findings have been promising (Margolin et al. 2002), but others showed no difference between auricular and sham acupuncture (Avants et al. 2000). A recent systematic review has indicated that there is no evidence for the effectiveness of auricular acupuncture in treating cocaine dependence (Gates et al. 2006). We know of no published systematic review of acupuncture’s effectiveness in treating opioid dependence, possibly because most of the encouraging results have come from nonrandomized trials (Ter Riet et al. 1990; Linde et al. 2001; Jordan 2006).
However, Chinese researchers have begun studying acupuncture as an adjuvant treatment—augmenting rather than replacing allopathic medications during opioid detoxification. Some studies have indicated that acupuncture, in this ancillary role, can significantly decrease the dosage of buprenorphine or methadone needed to allay the withdrawal symptoms. Further, some of these studies suggest that the combined treatment may lead to lower relapse rates (Wu et al. 1999, 2001). These studies have not been widely cited, partly because most have been published in Chinese journals. To remedy this situation, Min (2007) published a review of relevant trials completed through 2005 and argued that both acupuncture alone and acupuncture combined with medication were more effective than medication alone in relieving heroin-withdrawal symptoms. In that review, both randomized controlled trials and quasi-randomized controlled trials were included, and trials were included without regard to medications co-administered in combined treatments. These factors may have affected the conclusions.
Here, using meta-analytic techniques, we replicate and extend Min’s systematic review, focusing exclusively on the effectiveness and safety of acupuncture as an adjuvant treatment during opioid detoxification.
Methods
Literature Search
After a preparatory literature search, we found that the studies in which acupuncture was used as an adjuvant treatment had usually been carried out in China. No RCTs meeting our criteria were found in English language journals. The relevant body of research in China began in the early 1990s. Therefore, the time span of our final literature search was January 1990 to February 2008. To locate all the reports of relevant clinical trials, we searched English language databases (EMBASE, PUBMED, and the Cochrane Central Register of Controlled Trials) as well as Chinese databases (Chinese Biomedical Literatures, China National Knowledge Infrastructure, Wanfang, and VIP). Our search strategy was to focus on the keywords “heroin” and “acupuncture,” also searching for their synonyms and closely related words such as “opioid, opiate, morphine,” “acupressure, auricular acupuncture, electroacupuncture, ear acupuncture, needle,” and “detoxification, dependence, withdrawal,” and for combinations of these words. We searched for the Chinese counterparts of these words in the Chinese databases. We identified relevant reports by reading the titles and abstracts of the search results. We also inspected the reference list from each relevant article. Finally, we contacted experts in the field to gather information on the ongoing and unpublished studies.
Inclusion and Exclusion Criteria
We included studies that met the following criteria: (1) randomized controlled trial focusing on opioid detoxification, using a double-blind, single-blind, and nonblind design; (2) participants met criteria for opioid–heroin dependence (by DSM-IIIR, or DSM-IV criteria, with opioid-abuse history, documented abstinence syndrome, and positive urine test), and were in the acute stage of the abstinence syndrome (lachrymation, yawning, sweating, diarrhea, insomnia, fatigue, etc.); (3) the trial compared an experimental group receiving acupuncture combined with opioid receptor agonists (AT plus ORA) versus a control group receiving any opioid receptor agonists (ORA) or partial opioid receptor agonists (pORA); (4) the trial included at least one of the following outcome measures: total score for opioid-withdrawal symptoms, relapse rate, side effects, or medicine dosage needed to allay withdrawal; and (5) there were at least 15 participants in each group.
Exclusion criteria included: (1) nonnumeric data and (2) re-publication.
Data Extraction and Quality Assessment
Two reviewers read the titles and abstracts of search hits to assess each article suitability for inclusion. Uncertainties were resolved through discussion. The following key information was extracted from each study: first author, publication year, study design, sample size, patients’ demographic characteristics and drug-use history, detailed description of the intervention, and their outcomes.
The methodological quality of the included trials was assessed using the Jadad scale (Jadad et al. 1996), which rates studies for: (1) randomization, (2) double-blinding, (3) description of withdrawal, (4) description of randomization, and (5) description of blinding. Trials scoring 1 or 2 points are considered low-quality, while trials scoring 3–5 points are considered as high-quality.
Data Synthesis and Analysis
Demographic information for all participants in the included studies was summarized and analyzed using RevMan software (Cochrane Collaboration 2004). Continuous outcomes (such as scores on rating scales) were assessed in terms of the weighed mean difference (WMD) between two groups. Dichotomous outcomes (such as relapse rate) were assessed in terms of relative risk (RR). For both types of outcome, 95% confidence intervals (CIs) were calculated. Random-effect models were used to analyze pooled effects when heterogeneity was significant; otherwise, fixed-effect models were used. Differences were taken to be statistically significant when 95% CIs did not overlap (a more stringent criterion than a significance test at P < 0.05) (Wolfe and Hanley 2002). Fail-safe numbers were assessed to estimate the number of unpublished negative studies that would be needed to offset the observed results (Rosenthal 1979).
Results
Characteristics of Studies
We identified 21 reports of RCTs of acupuncture therapy combined with opioid receptor agonists for heroin detoxification; of these studies, 11 (with a total of 1,105 participants) were eligible for inclusion in the meta-analysis (see Table 1 for study details). The average age of participants in the included studies ranged from 24.0 to 34.2 years, and most participants were males (82.0%). The drug abused in these studies was heroin, with no mention of other classes of drugs. The average amount of daily heroin use was 0.45–1.80 g, with an average duration of use for 38.9–98.4 months. Intravenous injection and insufflation were the most commonly reported routes of administration in the included studies. The most commonly used specific acupoints were neiguan, zusanli, shenmen, hegu, and sanyinjiao (Jin 2007). The average duration of needling or electrical stimulation time was 20–50 min, with a frequency of once or twice per day. All of the included trials scored 2 points on the Jadad scale and were thus characterized as low-quality studies. The two points were for randomization and description of withdrawal. The included trials received no points for details of randomization or for double-blind design.
Table 1.
Characteristics of included studies
| Author and Year | Jadad score | Participants | Intervention | Duration (days) | Outcomes | ||||
|---|---|---|---|---|---|---|---|---|---|
| N AT + ORA/ORA | AT + ORA | ORA | AT + ORA/ORA | ||||||
| Age-year | Male% | Age-year | Male% | ||||||
| (He and Li 2005a) | 2 | 70/70 | 24.00 | – | 23.00 | – | AT + methadone/methadone | 15 | 2;3 |
| (He and Li 2005b) | 2 | 35/35 | 28.12 | 85.71 | 28.30 | 82.86 | AT + methadone/methadone | 15 | 1;3 |
| (Li et al. 2004) | 2 | 40/40 | 30.16 | 77.50 | 28.45 | 82.50 | AT + buprenorphine/buprenorphine | 10 | 1;4 |
| (Liu et al. 2005a) | 2 | 74/74 | 28.25 | 91.89 | 27.20 | 89.19 | AT + methadone/methadone | 10 | 1;4 |
| (Rong et al. 2005) | 2 | 33/31/30 | 31.80/31.90 | 84.85/87.10 | 29.20 | 83.33 | Scalp AT + methadone/body AT+methadone/methadone | 10 | 1 |
| (Wang et al. 1999a) | 2 | 60/60 | – | – | – | – | AT + methadone/methadone | 10 | 2;3 |
| (Wang et al. 1999b) | 2 | 100/100 | – | 86.00 | – | 87.00 | AT + methadone/methadone | 10 | 2;3 |
| (Wang et al. 2005) | 2 | 60/60 | – | 81.67 | – | 85.00 | AT + methadone/methadone | 10 | 2;3 |
| (Wu et al. 2003) | 2 | 30/30 | – | – | – | – | AT + opiate/opiate + buprenorphine | 10 | 1;4 |
| (Zeng et al. 2004) | 2 | 31/26 | 33.16 | 83.87 | 34.23 | 80.77 | AT + methadone/methadone | 10 | 1 |
| (Zhang et al. 2004) | 2 | 43/43 | 26.52 | 85.00 | 28.11 | 93.02 | AT+methadone/methadone | 10 | 1;4 |
Note: 1: total score of WSS; 2: relapse rate; 3: number of patients detoxified; 4: frequency of side effects
Efficacy of Combined Treatment (AT plus ORA)
Total Withdrawal Symptom Score (WSS)
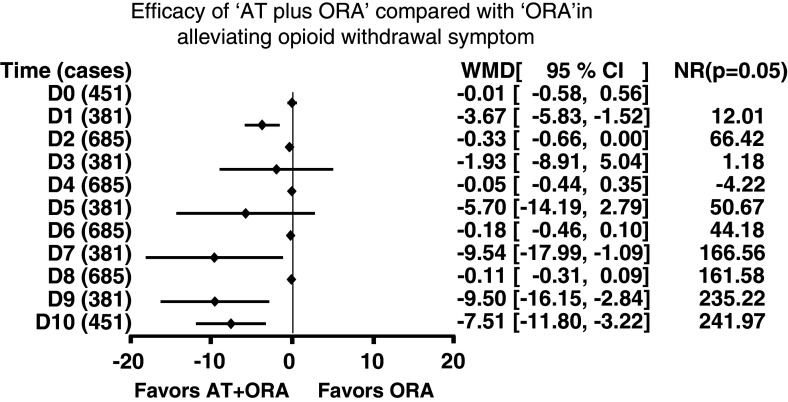
Seven trials assessed the severity of withdrawal symptoms using the withdrawal symptom scale (Himmeisbach and Andrews 1943). We analyzed the combined data from these studies (Fig. 1). Pretreatment baseline scores (D0) were similar across the treatments. For the first (D1), seventh (D7), and the final 2 days (D9, D10), combined treatment was significantly more effective than the agonist treatment alone. The WMDs and 95% CIs were: D1, 3.67 [−5.83, −1.52]; D7, 9.54 [−17.99, −1.09]; D9, 9.50 [−16.15, −2.84]; D10, 7.51 [−11.80, −3.22]. There were no significant differences between the groups at other time points, but when nonsignificant differences were apparent, they favored combined treatment.
Fig. 1.
Efficacy of acupuncture therapy plus opioid receptor agonists (AT ± ORA) versus ORA in alleviating opioid withdrawal symptoms. Summary estimates of the weighed mean differences (WMDs) and their 95% CIs are given day by day. D0 indicates pretreatment baseline. D0 and D1 were analyzed with fixed-effect models. The other time points were analyzed with random-effect models. N R indicates the failsafe number, i.e., the number of unpublished negative studies that would be required to negate each significant finding at an alpha level of 0.05
Relapse Rate
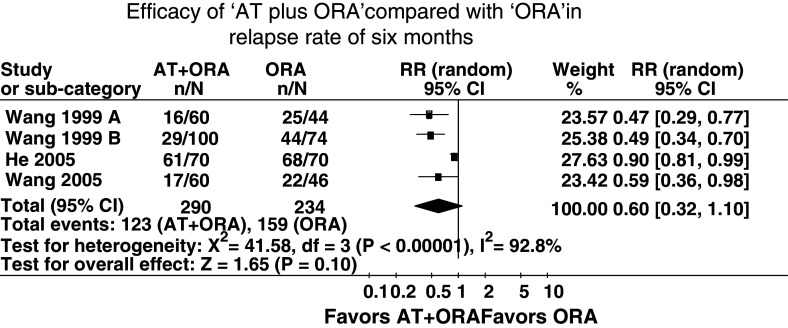
Four trials, involving a total of 524 participants, included 6-month follow-up evaluations to assess relapse rate after discontinuation of acupuncture. The 6-month relapse rates in combined groups and control groups were: 87% vs. 97% (He and Li 2005a); 26.6% vs. 56.8% (Wang et al. 1999a); 29.0% vs. 59.5% (Wang et al. 1999b); and 28.3% vs. 47.8% (Wang et al. 2005). Pooled analysis showed no significant effect of acupuncture (Fig. 2). The RR and 95% CI were 0.60 [0.32, 1.10], P = 0.10.
Fig. 2.
Efficacy of acupuncture therapy plus opioid receptor agonists (AT ± ORA) versus ORA in reducing rate of relapse at 6 months. Summary estimates of the relative risk (RR) and its 95% CI were analyzed with random-effect models
Safety of Combined Treatment (AT plus ORA): Side Effects
Insufficient data were available to perform pooled analysis on side-effect incidence; only four trials mentioned side effects during the treatment. The most common side effects reported were nausea, vomiting, dry mouth, blurred vision, and headache. While one study showed no significant differences in side effects between the groups (Wu et al. 2003), another found that the incidence of side effects was significantly less in the AT + ORA group than in the ORA group (Li et al. 2004). The two other studies found that the most common complaint in AT + ORA recipients was muscle twitching from electroacupuncture, which was well tolerated after explanation and intensity adjustment (Zhang et al. 2004; Liu et al. 2005a).
Other Comparison: Medicine Dosage Used
In three of the included trials, the investigators attempted to reduce the dose of opioid agonist for the AT + ORA group (using half the dose given to the ORA group) (Li et al. 2004, 2005a; Zhang et al. 2004) and withdrawal syndromes were managed smoothly in both the groups. In the other eight trials, the doses were equal across the groups. The dosage of opioid agonist was determined in accordance with the amount of heroin abused, and decreased gradually across 10 or 15 days. The starting doses were less than 60 mg/day for methadone, 0.8–1.6 mg/day for buprenorphine, and 300 mg/day for morphine.
File-Drawer Effect
To address the “file-drawer problem” (the possibility that unpublished negative findings would negate the findings of the published studies), we calculated the fail-safe number N R (Rosenthal 1979), representing the number of studies with null results that would render each of our findings nonsignificant at P = 0.05. N Rs are shown in the right-hand column of Fig. 1. Note that N R is calculated in terms of significant differences at P = 0.05, which sometimes emerge even in instances when 95% CIs overlap (Wolfe and Hanley 2002).
Discussion
Our meta-analysis revealed that individuals receiving acupuncture therapy combined with opioid agonist treatment showed lower scores for opioid-withdrawal symptoms than individuals receiving only opioid agonists, on the first day and three of the last days of a 10-day taper. There was no significant difference between the two groups in terms of relapse rate at 6 months.
Our present findings differed somewhat from those of the earlier meta-analysis that we sought to replicate and extend (Min 2007). That study concluded that acupuncture combined with medication was more efficacious than medication alone from days 1 to 10, and that subsequent relapse rates were lower after the combination treatment. This difference may be due to different inclusion criteria between the two meta-analyses; unlike Min (2007), we included only RCTs and restricted the control group treatment to opioid agonists.
Theoretically, acupuncture as applied by qualified practitioners in the traditional way should have no side effects (Lu et al. 2004; Min 2007). The side effects that were reported in a few of the included trials seem to have resulted from improper application of electrical impulses in electroacupuncture, and these side effects were remedied by adjustment of the electroacupuncture intensity. In the included trials, acupuncture not only rarely caused side effects but also diminished the side effects caused by the opioid agonists. One included trial showed that its combined-therapy group had fewer side effects than the group receiving agonist medication alone (Li et al. 2004). Also, in three included trials, doses of opioid agonists half those used in the medication alone groups were used in conjunction with acupuncture, and combined group participants’ withdrawal syndromes were managed effectively. Because acupuncture is inexpensive, simple, and essentially free of side effects, further research on its application as a complementary therapy should be performed to facilitate dosage reduction of conventional medicine.
The styles of acupuncture in the meta-analyzed trials included traditional needle puncturing, auricular acupuncture, and electroacupuncture. According to the theory of acupuncture, bodily functions are controlled by systems of “Jingluo” and “Qi-xue,” and pressure applied through needles improves the functioning of these systems (Shi et al. 2006). In rats, acupuncture at acupoint HT7 significantly decreases both dopamine release in the nucleus accumbens and behavioral hyperactivity induced by a systemic morphine challenge (Kim et al. 2005). Peripheral electric stimulation in rats inhibits morphine-induced place preference (Wang et al. 2000) and attenuates the signs of morphine withdrawal (Liu et al. 2005b). Some of the effects of electroacupuncture may be mediated by release of endogenous peptides such as enkephalins and dynorphin (Han et al. 1991; Chen and Han 1992).
The existing evidence indicates that acupuncture combined with an opioid agonist is efficacious for treatment of opioid withdrawal and may have the potential to decrease the agonist dosage needed and alleviate the side effects of the agonist. However, there is no strong evidence that the combination is otherwise superior to treatment with an opioid-agonist alone, and the question is still open. A major limitation of this meta-analysis is the poor methodological quality of the included trials. Unfortunately, none of the included trials used a double-blind design: the control groups did not receive sham acupuncture. The published results also lacked adequate details about randomization. Also, because all the included trials were conducted in China, their results may not be generalizable to other regions. Thus, high-quality research is essential for more definitive conclusions.
Acknowledgments
This work was supported in part by the National Basic Research Program of China (973 Program, 2003CB515400), the National High Technology Research and Development Program of China (863 Program, 2006AA02Z4D1), and the China-Canada Joint Health Research Program (No: 30611120528).
Contributor Information
Jie Shi, FAX: +86-10-62032624, Email: shijie@bjmu.edu.cn.
Lin Lu, Email: linlu@bjmu.edu.cn.
References
- Avants SK, Margolin A, Holford TR, Kosten TR (2000) A randomized controlled trial of auricular acupuncture for cocaine dependence. Arch Intern Med 160:2305–2312. doi:10.1001/archinte.160.15.2305 [DOI] [PubMed] [Google Scholar]
- Chen XH, Han JS (1992) Analgesia induced by electroacupuncture of different frequencies is mediated by different types of opioid receptors: another cross-tolerance study. Behav Brain Res 47:143–149. doi:10.1016/S0166-4328(05)80120-2 [DOI] [PubMed] [Google Scholar]
- Cochrane Collaboration (2004) RevMan user guide. http://www.cc-ims.net/download/revman/Documentation/User%20guide.pdf. Accessed 21 Dec 2007
- Gates S, Smith LA, Foxcroft DR (2006) Auricular acupuncture for cocaine dependence. Cochrane Database Syst Rev (Online), CD005192, 25 Jan 2006 [DOI] [PMC free article] [PubMed]
- Han JS, Chen XH, Sun SL, Xu XJ, Yuan Y, Yan SC, Hao JX, Terenius L (1991) Effect of low- and high-frequency TENS on Met–enkephalin–Arg–Phe and dynorphin A immunoreactivity in human lumbar CSF. Pain 47:295–298. doi:10.1016/0304-3959(91)90218-M [DOI] [PubMed] [Google Scholar]
- He JL, Li YZ (2005a) A comparative clinical study of the effect of electro-acupuncture compared with medicine treatment on treatment of opiate addicts. Chin J Clin Rehabil 9:215 [Google Scholar]
- He JL, Li YL (2005b) Application of electro-acupuncture in drug detoxification treatment. Chin J Drug Abuse Prev Treat 6:42–43 [Google Scholar]
- Himmeisbach CK, Andrews HL (1943) Studies on the modification of the morphine abstinence syndrome by drugs. J Pharmacol Exp Ther 77:17–23 [Google Scholar]
- Jadad AR, Moore RA, Carroll D, Jenkinson C, Reynolds DJ, Gavaghan DJ, McQuay HJ (1996) Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials 17:1–12. doi:10.1016/0197-2456(95)00134-4 [DOI] [PubMed] [Google Scholar]
- Jin GY (2007) Contemporary medical acupuncture—a systems approach. Springer and HEP, Berlin March [Google Scholar]
- Jordan JB (2006) Acupuncture treatment for opiate addiction: a systematic review. J Subst Abuse Treat 30:309–314. doi:10.1016/j.jsat.2006.02.005 [DOI] [PubMed] [Google Scholar]
- Kim MR, Kim SJ, Lyu YS, Kim SH, Lee Y, Kim TH, Shim I, Zhao R, Golden GT, Yang CH (2005) Effect of acupuncture on behavioral hyperactivity and dopamine release in the nucleus accumbens in rats sensitized to morphine. Neurosci Lett 387:17–21. doi:10.1016/j.neulet.2005.07.007 [DOI] [PubMed] [Google Scholar]
- Li CC, Lin WP, Zhang JM (2004) A comparative clinical study of the effect of buprenorphine or combined with acupuncture on withdrawal symptom of heroin addicts. J Guangdong Med Coll 124:515–516 [Google Scholar]
- Linde K, Vickers A, Hondras M, ter Riet G, Thormahlen J, Berman B, Melchart D (2001) Systematic reviews of complementary therapies—an annotated bibliography. Part 1: acupuncture. BMC Complement Altern Med 1:3. doi:10.1186/1472-6882-1-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu Q, Zhou YP, Zhang PG, Guo XY (2005a) Efficacy of electro-acupuncture combined with methadone on heroin withdrawal symptom. J Clin Med Pract 6:42–43 [Google Scholar]
- Liu S, Zhou W, Liu H, Yang G, Zhao W (2005b) Electroacupuncture attenuates morphine withdrawal signs and c-Fos expression in the central nucleus of the amygdala in freely moving rats. Brain Res 1044:155–163. doi:10.1016/j.brainres.2005.02.075 [DOI] [PubMed] [Google Scholar]
- Lu PK, Lu GP, Lu DP, Lu DP, Lu WI (2004) Managing acute withdrawal syndrome on patients with heroin and morphine addiction by acupuncture therapy. Acupunct Electrother Res 29:187–195 [DOI] [PubMed] [Google Scholar]
- Margolin A, Kleber HD, Avants SK, Konefal J, Gawin F, Stark E, Sorensen J, Midkiff E, Wells E, Jackson TR, Bullock M, Culliton PD, Boles S, Vaughan R (2002) Acupuncture for the treatment of cocaine addiction: a randomized controlled trial. JAMA 287:55–63. doi:10.1001/jama.287.1.55 [DOI] [PubMed] [Google Scholar]
- Min X (2007) Acupuncture in treatment of heroin withdrawal syndrome: a systematic review and meta-analysis. http://www.nd.gov.hk/Syndrome_Executive_summary_Eng.pdf. Accessed 21 Jan 2008
- Rong J, Chen JY, Liu ZY (2005) Clinical research of scalp acupuncture treatment for withdrawal symptoms of heroin addicts. J Xinjiang Med Univ 28:615–617 [Google Scholar]
- Rosenthal R (1979) The “file drawer problem” and tolerance for null results. Psychol Bull 86:638–641. doi:10.1037/0033-2909.86.3.638 [Google Scholar]
- Shi J, Liu YL, Fang YX, Xu GZ, Zhai HF, Lu L (2006) Traditional Chinese medicine in treatment of opiate addiction. Acta Pharmacol Sin 27:1303–1308. doi:10.1111/j.1745-7254.2006.00431.x [DOI] [PubMed] [Google Scholar]
- Ter Riet G, Kleijnen J, Knipschild P (1990) A meta-analysis of studies into the effect of acupuncture on addiction. Br J Gen Pract 40:379–382 [PMC free article] [PubMed] [Google Scholar]
- Wang B, Luo F, Xia YQ, Han JS (2000) Peripheral electric stimulation inhibits morphine-induced place preference in rats. NeuroReport 11:1017–1020 [DOI] [PubMed] [Google Scholar]
- Wang ZT, Yuan YQ, Wang J, Luo JK (1999a) Observations on the efficacy of electro-acupuncture therapy plus medicine for treating heroin addiction. Chin J Inform Tradit Chin Med 6:35 [Google Scholar]
- Wang ZT, Yuan YQ, Wang J, Luo JK (1999b) Observations on the efficacy of electro-acupuncture therapy plus medicine for treating heroin addiction. Zhongguo Zhen Jiu 18:657–658 [Google Scholar]
- Wang ZT, Yuan YQ, Wang J, Luo JK (2005) Observations on the efficacy of auricular-plaster therapy plus medicine for treating heroin addiction. Shanghai Zhen Jiu Za Zhi 24:6–7 [Google Scholar]
- Wen HL (1977) Fast detoxification of heroin addicts by acupuncture and electrical stimulation (AES) in combination with naloxone. Comp Med East West 5:257–263. doi:10.1142/S0147291777000362 [DOI] [PubMed] [Google Scholar]
- Wen HL, Teo SW (1975) Experience in the treatment of drug addiction by electro-acupuncture. Xianggang Hu Li Za Zhi 19:33–35 [PubMed] [Google Scholar]
- Wolfe R, Hanley J (2002) If we’re so different, why do we keep overlapping? When 1 plus 1 doesn’t make 2. CMAJ 166:65–66 [PMC free article] [PubMed] [Google Scholar]
- Wu JM, Wei DY, Luo YF, Xiang XY (2003) Clinic research on heroin de-addiction effects of acupuncture and its potentiality of preventing relapse. Zhong Xi Yi Jie He Xue Bao 1:268–272. doi:10.3736/jcim20030412 [DOI] [PubMed] [Google Scholar]
- Wu LZ, Cui CL, Han JS (1999) Treatment on heroin addicts by four channel Han’s acupoint nerve stimulator (HANS). J Beijing Med Univ 31:239–242 [Google Scholar]
- Wu LZ, Cui CL, Han JS (2001) Reduction of methadone dosage and relief of depression and anxiety by 2/100 Hz tens for heroin detoxification. Chin J Drug Depend 10:124–126 [Google Scholar]
- Zeng XL, Lei LM, Lu YH, Wang ZT (2004) Clinically controlled study on deintoxication of heroin dependence by acupuncture on points of the governor vessel. Zhongguo Zhen Jiu 24:385–387 [Google Scholar]
- Zhang PG, Kang B, Zhong Q (2004) Studies on the synergic effect of electroacupuncture and methadone on heroin withdrawal symptoms. Shanghai Zhen Jiu Za Zhi 23:5–6 [Google Scholar]