The prevalence of human immunodeficiency virus and syphilis among men who have sex with men in China is high, yet the 2 epidemics are largely geographically separate. Characteristics of the overall population surveyed as well as segments within this population are described.
Keywords: HIV, syphilis, MSM, China
Abstract
Background. Human immunodeficiency virus (HIV) has rapidly spread among men who have sex with men (MSM) in China in recent years; the magnitude of the epidemic is unclear. We sought to test 3 hypotheses: (1) The prevalence of both HIV and syphilis among MSM in China is high, (2) the 2 epidemics each have unique geographical distributions, and (3) demographic and sexual behavior characteristics are different among segments of the MSM population in China.
Methods. A total of 47 231 MSM from 61 cities in China participated in a cross-sectional survey conducted from February 2008 to September 2009. Demographic and behavioral data were collected and analyzed and blood samples tested for HIV and syphilis. Three subgroups among the broader MSM sample were described. Main outcome measures were HIV and syphilis prevalence.
Results. An overall prevalence of 4.9% (2314/47 231; 95% confidence interval [CI], 4.7%–5.1%) for HIV and 11.8% (5552/47 231; 95% CI, 11.5%–12.0%) for syphilis was found. Syphilis-positive MSM had the highest HIV prevalence, 12.5% (693/5552; 95% CI, 11.6%–13.4%). However, correlations between HIV and syphilis prevalence were found in only 3 of 6 geographical regions (Northwest: r = 0.82, P = .0253; East: r = 0.78, P = .0004; and South-central: r = 0.63, P = .0276). Three subgroups—nonlocal MSM, Internet-using MSM, and female-partnering MSM—were found to have different profiles of characteristics and behaviors.
Conclusions. HIV and syphilis prevalences among MSM in China are high and the 2 epidemics are largely separate geographically. Three segments of the Chinese MSM population each have different demographic and sexual risk “profiles” that suggest high potential for bridging infection across geographies, generations, and sexes.
(See the Editorial Commentary by Muessig and Cohen on pages 310–3.)
Prevalence estimates of human immunodeficiency virus (HIV) among men who have sex with men (MSM) in developing Asian countries are high: 7.8% in Cambodia, 9.0% in Indonesia, 14.7% in India, and 24.6% in Thailand [1]. In India, prevalence varies geographically from 7.5% to as high as 20.9% [2], and in Thailand, HIV prevalence has increased rapidly—17.3% in 2003, 28.3% in 2005, and 30.8% in 2007 [3]. As HIV susceptibility and/or infectiousness is associated with the presence of other sexually transmitted infections such as syphilis [4], it is not surprising that syphilis is also a major public health issue among MSM in developing Asian nations—4.3% in Indonesia [5], 8.4%–14% in India [2], and 33% among those newly diagnosed with HIV in Thailand [6].
In China, several meta-analyses of HIV and syphilis prevalence among Chinese MSM have been published [7–10]. In 2009, Gao et al reported a pooled HIV prevalence of 2.5% and a pooled syphilis prevalence of 9.1% for studies conducted during 2001–2008 [7]. In 2011, Li et al reported a range of 3.2%–15.8% for HIV prevalence for studies conducted during 2005–2008 [8]. Also in 2011, Chow et al reported HIV prevalence of 5.3% for 2007–2009 [9] and 4.7% for 2007–2008, and syphilis prevalence of 13.5% for the same time period [10]. However, it is unclear how generalizable these study findings are owing to relatively small sample sizes or few study sites. Additionally, we find only 2 studies describing the nationwide geographical distributions of HIV and syphilis prevalence, one reporting that HIV prevalence among MSM is significantly higher over time in the Southwest region only and another finding that HIV and syphilis prevalence is correlated in the Northeast and East regions only [9, 10]. Furthermore, a few studies have suggested that there are different segments within the Chinese MSM community (one ethnographic study identifying as many as 20), which have very little overlap in their behavioral characteristics and social circles [11, 12].
It is in this context that we have undertaken the largest study of HIV and syphilis prevalence among MSM in the world, surveying and testing a total of 47 231 MSM. Our primary aim was to directly obtain a reliable measure of the current magnitude and geography of the HIV and syphilis epidemics among MSM in China, testing the hypothesis that HIV and syphilis prevalences are high, but with unique geographical distributions. We also hypothesized that there are several segments within the MSM population that have different characteristics; thus, our secondary aim was to identify and describe a few of these subgroups.
METHODS
Study Design and Participant Eligibility
A nationwide cross-sectional survey was conducted in 61 cities in China from February 2008 to September 2009. To meet eligibility criteria, subjects needed to be men 18–69 years of age who reported engaging in sex with men in the previous year, and who were willing to be tested for HIV and syphilis.
City Selection and Sampling Methods
For each province or autonomous region, 1–4 cities at the prefecture level including the capital city were selected. Cities were selected on the basis of population size and estimated number of MSM. The desired minimum sample size was 600 for municipalities (Beijing, Chongqing, Shanghai, and Tianjin) and 200–450 for other cities. The original protocol required 10 cities (Beijing, Chongqing, Changchun, Harbin, Nanjing, Jinan, Qingdao, Wuhan, Guangzhou, and Urumqi) to be sampled by a respondent-driven sampling (RDS) method [13], and the remaining 51 cities to be sampled by stratified snowball sampling methods [14]. However, very early in the study, all sampling was changed to the snowball method because investigators were unable to obtain large enough sample sizes using RDS. Overall, 92.0% of subjects were recruited by the snowball method and 8.0% by the RDS method. For more detailed information, see Supplementary Data describing estimation of the numbers of MSM in cities (Supplementary Methods 1), city selection (Supplementary Methods 2), and use of seeds for sampling (Supplementary Methods 3).
Survey
The survey questionnaire was based on that used in the national sentinel surveillance program since 1995, with modifications based on Chinese MSM community feedback. A pilot survey was conducted in 4 cities from January to February 2008. Subjects included in the pilot study were not included in the final data analysis. Local Centers for Disease Control and Prevention (CDC) staff who conducted the surveys by interview were given intensive training and a detailed protocol. Interview settings had at least 1 private interview/counseling room, a testing room, and a waiting room, and were usually located within a hospital or local CDC facility.
HIV and Syphilis Testing
Blood samples were collected from each subject and tested immediately on-site for HIV and current, active syphilis infection (not lifetime exposure), and waiting subjects were notified of their serostatus. Counseling was provided before and after testing. Participants who tested positive were referred to the National AIDS Program and/or a local hospital or clinic. Samples yielding inconclusive HIV results from rapid, on-site tests were subjected to confirmatory testing and subjects were asked to return to receive their results. More information on testing methods can be found in Supplementary Methods 4.
Statistical Analysis
HIV and syphilis prevalence was calculated by dividing the sum of all confirmed cases by the total number of subjects who participated. Sensitivity analysis for prevalence was also conducted, and methods and results of weighted prevalence calculations are available in Supplementary Methods 5 and Supplementary Tables 1 and 2. Confidence intervals (CIs) of prevalence were calculated by approximating the binomial distribution with a normal distribution. To account for nonindependency, multilevel (city and individual) logistic regression models (SAS/GLIMMIX) were used to calculate both unadjusted and adjusted odds ratios (ORs) and CIs for predictor variables. The Supplementary Data contain more information on our mixed sampling method design (Supplementary Methods 6) and our multivariate model (Supplementary Methods 7). Missing values were treated as separate categories for clarity, but otherwise received no special treatment; rather, all regression models were run using complete cases. Pearson correlation coefficients at the regional level between HIV and syphilis prevalence were generated using an SAS Corr procedure and Gplot procedure with a linear regression line. All P values are 2-sided. Data analysis was performed using SAS version 9.2 for Windows x64 (SAS Institute).
Ethical Approval
This study was reviewed and approved by the Institutional Review Board of the National Center for AIDS/STD Control and Prevention, China CDC. Subjects provided signed informed consent and were assigned unique identification numbers so that anonymity could be maintained yet double-testing prevented. Participants were provided not more than CNY55 (approximately US$8) as compensation for transportation costs.
RESULTS
Study Population Characteristics
A total of 47 231 MSM participated in the survey. As shown in Tables 1 and 2, most participants were young (29 831/47 231 aged 18–29 years), never married (34 784/47 231), Han Chinese (43 635/47 231), highly educated (20 592/47 231 had a college education or greater) and nonlocal (20 601/47 231 not registered as local residents in the city where they were surveyed).
Table 1.
Demographic Characteristics, HIV Prevalence, and Risk Factors for Men Who Have Sex With Men in 61 Cities in China
| Characteristics | Subjects, No. (%) | HIV Cases, No. (%) | Prevalence (CI)a | Unadjusted ORb (CI) | Adjusted OR (CI) | Adjusted P Valueb,c |
|---|---|---|---|---|---|---|
| Demographics | ||||||
| Age, y | ||||||
| 18–24 | 20 454 (43.3) | 774 (33.4) | 3.8 (3.5–4.0) | 1.0 | 1.0 | |
| 25–29 | 9377 (19.9) | 478 (20.7) | 5.1 (4.7–5.5) | 1.4 (1.2–1.6) | 1.4 (1.2–1.6) | <.0001 |
| 30–34 | 6574 (13.9) | 404 (17.5) | 6.1 (5.6–6.7) | 1.8 (1.6–2.1) | 1.7 (1.5–2.0) | <.0001 |
| 35–39 | 4419 (9.4) | 247 (10.7) | 5.6 (4.9–6.3) | 1.6 (1.4–1.9) | 1.4 (1.2–1.7) | .0003 |
| 40–49 | 4654 (9.9) | 293 (12.7) | 6.3 (5.6–7.0) | 1.9 (1.7–2.2) | 1.6 (1.3–2.0) | <.0001 |
| 50–69 | 1182 (2.5) | 90 (3.9) | 7.6 (6.1–9.1) | 2.3 (1.8–2.8) | 1.9 (1.5–2.5) | <.0001 |
| Refused/missing | 571 (1.2) | 28 (1.2) | … | … | … | … |
| Marital status | ||||||
| Never married | 34 784 (73.6) | 1588 (68.6) | 4.6 (4.3–4.8) | 1.0 | 1.0 | |
| Married | 9592 (20.3) | 507 (21.9) | 5.3 (4.8–5.7) | 1.3 (1.2–1.5) | .93 (.79–1.1) | .3758 |
| Live with a partner (male/female) | 645 (1.4) | 31 (1.3) | 4.8 (3.2–6.5) | 1.1 (.76–1.6) | .84 (.55–1.3) | .4246 |
| Divorced/widowed | 2200 (4.7) | 188 (8.1) | 8.5 (7.4–9.7) | 2.0 (1.7–2.4) | 1.3 (1.04–1.6) | .0156 |
| Refused/missing | 10 (0.02) | 0 (0) | … | … | … | … |
| Ethnicity | ||||||
| Han Chinese | 43 635 (92.4) | 2148 (92.8) | 4.9 (4.7–5.1) | 1.0 | 1.0 | |
| Other | 355 (7.5) | 165 (7.1) | 4.6 (4.0–5.3) | 1.1 (.94–1.3) | 1.1 (.88–1.3) | .5449 |
| Refused/missing | 42 (0.09) | 1 (0.04) | … | … | … | … |
| Highest education | ||||||
| Junior high | 9959 (21.1) | 593 (25.6) | 6.0 (5.5–6.4) | 1 | 1 | |
| Senior high | 16 666 (35.2) | 852 (36.8) | 5.1 (4.8–5.4) | .84 (.75–.94) | .98 (.87–1.1) | .7301 |
| College or higher | 20 592 (43.6) | 868 (37.5) | 4.2 (3.9–4.5) | .60 (.54–.67) | .77 (.68–.88) | <.0001 |
| Refused/missing | 14 (0.03) | 1 (0.04) | … | … | … | … |
| Household registration | ||||||
| Local resident | 26 607 (56.3) | 1060 (45.8) | 4.0 (3.7–4.2) | 1.0 | 1.0 | |
| Non–local resident | 20 601 (43.6) | 1253 (54.1) | 6.1 (5.8–6.4) | 1.4 (1.3–1.5) | 1.4 (1.3–1.5) | <.0001 |
| Refused/missing | 23 (0.05) | 1 (0.04) | … | … | … | … |
| Syphilis infection status | ||||||
| Negative | 41 679 (88.2) | 1621 (70.1) | 3.9 (3.7–4.1) | 1.0 | 1.0 | |
| Positive | 5552 (11.8) | 693 (29.9) | 12.5 (11.6–13.4) | 3.6 (3.3–4.0) | 3.3 (3.0–3.7) | <.0001 |
| Sexual behavior in the past 6 mo | ||||||
| Venues for finding sex partners | ||||||
| Bars/tea houses/dance halls | 10 380 (22.0) | 443 (19.1) | 4.3 (3.9–4.7) | 1.0 | 1.0 | |
| Public bathhouses/saunas | 6436 (13.6) | 475 (20.5) | 7.4 (6.7–8.0) | 1.7 (1.5–2.0) | 1.4 (1.2–1.6) | <.0001 |
| Parks | 5461 (11.6) | 214 (9.2) | 3.9 (3.4–4.4) | 1.1 (.89–1.3) | .86 (.71–1.04) | .1269 |
| Internet sites | 21 444 (45.4) | 973 (42.0) | 4.5 (4.3–4.8) | .9 (.8–1.1) | 1.0 (.87–1.1) | .9753 |
| Other | 2681 (5.7) | 173 (7.5) | 6.7 (5.7–7.4) | 1.1 (.91–1.3) | 1.2 (1.00–1.5) | .04466 |
| Refused/missing | 829 (1.7) | 36 (1.6) | … | … | … | … |
| Buy male sex | ||||||
| No | 44 541 (94.3) | 2185 (94.4) | 4.9 (4.7–5.1) | 1.0 | 1.0 | |
| Yes | 2543 (5.4) | 117 (5.1) | 4.6 (3.8–5.4) | 1.1 (.90–1.3) | 1.4 (1.1–1.7) | .0082 |
| Refused/missing | 147 (0.31) | 12 (0.52) | … | … | … | … |
| Sell sex to a male | ||||||
| No | 42 732 (90.5) | 2102 (90.8) | 4.9 (4.7–5.1) | 1.0 | 1.0 | |
| Yes | 4358 (9.2) | 203 (8.8) | 4.7 (4.0–5.3) | 1.1 (.92–1.2) | 1.4 (1.1–1.7) | .0012 |
| Refused/missing | 141 (0.30) | 9 (0.39) | … | … | … | … |
| No. of male sex partners | ||||||
| 0 | 5886 (12.5) | 215 (9.3) | 3.7 (3.2–4.1) | 1.0 | 1.0 | |
| 1 | 13 421 (28.4) | 502 (21.7) | 3.7 (3.4–4.1) | 1.0 (.88–1.2) | 1.1 (.90–1.3) | .3781 |
| 2–10 | 22 370 (47.4) | 1274 (55.1) | 5.7 (5.4–6.0) | 1.6 (1.4–1.9) | 1.5 (1.3–1.8) | <.0001 |
| >10 | 2372 (5.0) | 155 (6.7) | 6.5 (5.5–7.5) | 1.8 (1.5–2.3) | 1.6 (1.3–2.0) | .0001 |
| Refused/missing | 3182 (6.7) | 168 (7.3) | … | … | … | … |
| Consistent condom use with male partners | ||||||
| No | 24 107 (51.0) | 1402 (60.6) | 5.8 (5.5–6.1) | 1.0 | 1.0 | |
| Yes | 16 720 (35.4) | 669 (28.9) | 4.0 (3.7–4.3) | .66 (.60–.72) | .71 (.64–.79) | <.0001 |
| No sex in past 6 mo | 5886 (12.5) | 215 (9.3) | 3.7 (3.2–4.1) | .60 (.51–.70) | .65 (.55–.76) | <.0001 |
| Refused/missing | 518 (1.1) | 28 (1.2) | … | … | … | … |
| No. of female sex partners | ||||||
| 0 | 35 495 (75.2) | 1800 (77.8) | 5.3 (5.1–5.6) | 1.0 | 1.0 | |
| 1 | 8401 (17.8) | 383 (16.6) | 4.8 (4.3–5.2) | 1.0 (.86–1.1) | .86 (.75–.98) | .0415 |
| ≥2 | 2699 (5.7) | 106 (4.6) | 4.1 (3.3–4.9) | .74 (.61–.91) | .70 (.56–.88) | .0022 |
| Refused/missing | 636 (1.3) | 25 (1.1) | … | … | … | … |
| Study design | ||||||
| Sampling method | ||||||
| Snowball | 43 437 (92.0) | 2047 (88.5) | 4.7 (4.5–4.9) | 1.0 | 1.0 | |
| RDS | 3794 (8.0) | 267 (11.5) | 7.0 (6.2–7.8) | 1.1 (.97–1.4) | 1.1 (.94–1.4) | .2192 |
| City-level characteristics | ||||||
| Administrative level | ||||||
| Directly under central government | 6051 (12.8) | 562 (24.3) | 9.3 (8.6–10.0) | 3.3 (1.5–7.3) | 3.0 (1.3–6.7) | .0092 |
| Province capital | 23 422 (49.6) | 1167 (50.4) | 5.0 (4.7–5.3) | 1.6 (1.1–2.4) | 1.4 (.9–2.2) | .1198 |
| Other cities | 17 758 (37.6) | 585 (25.3) | 3.3 (3.0–3.6) | 1.0 | ||
| Overall | 47 231 (100) | 2314 (100) | 4.9 (4.7–5.1) | … | … | … |
Abbreviations: CI, confidence interval; HIV, human immunodeficiency virus; OR, odds ratio; RDS, respondent-driven sampling.
a CIs are 95% CIs in all cases and were calculated by approximating the binomial distribution with a normal distribution.
b ORs and P values were calculated by using a multilevel logistic regression model.
c P values are 2-sided in all cases.
Table 2.
Demographic Characteristics, Syphilis Prevalence, and Risk Factors for Men Who Have Sex With Men in 61 Cities in China
| Characteristics | Subjects, No. (%) | Syphilis Cases, No. (%) | Prevalence (CI)a | Unadjusted ORb (CI) | Adjusted OR (CI) | Adjusted P Valueb,c |
|---|---|---|---|---|---|---|
| Demographics | ||||||
| Age, y | ||||||
| 18–24 | 20 454 (43.3) | 1686 (30.4) | 8.2 (7.9–8.6) | 1.0 | 1.0 | |
| 25–29 | 9377 (19.9) | 1121 (20.2) | 12.0 (11.3–12.6) | 1.5 (1.4–1.6) | 1.5 (1.4–1.7) | <.0001 |
| 30–34 | 6574 (13.9) | 826 (14.9) | 12.6 (11.8–13.4) | 1.6 (1.4–1.7) | 1.7 (1.5–1.9) | <.0001 |
| 35–39 | 4419 (9.4) | 658 (11.9) | 14.9 (13.8–15.9) | 1.9 (1.7–2.1) | 2.0 (1.7–2.2) | <.0001 |
| 40–49 | 4654 (9.9) | 935 (16.8) | 20.1 (18.9–21.2) | 2.7 (2.4–2.9) | 2.8 (2.5–3.2) | <.0001 |
| 50–69 | 1182 (2.5) | 274 (4.9) | 23.2 (20.8–25.6) | 3.1 (2.7–3.6) | 3.2 (2.7–3.8) | <.0001 |
| Refused/missing | 571 (1.2) | 52 (0.94) | … | … | … | … |
| Marital status | ||||||
| Never married | 34 784 (73.6) | 3617 (65.1) | 10.4 (10.1–10.7) | 1.0 | 1.0 | |
| Married | 9592 (20.3) | 1452 (26.2) | 15.1 (14.4–15.9) | 1.5 (1.4–1.6) | .86 (.78–.96) | .0047 |
| Live with a partner (male/female) | 645 (1.4) | 72 (1.3) | 11.2 (8.7–13.6) | 1.2 (.96–1.6) | .98 (.75–1.3) | .9062 |
| Divorced/widowed | 2200 (4.7) | 410 (7.4) | 18.6 (17.0–20.3) | 2.0 (1.8–2.3) | .95 (.83–1.1) | .4967 |
| Refused/missing | 10 (0.02) | 1 (0.02) | … | … | … | … |
| Ethnicity | ||||||
| Han Chinese | 43 635 (92.4) | 5124 (92.3) | 11.7 (11.4–12.0) | 1.0 | 1.0 | |
| Other | 355 (7.5) | 426 (7.7) | 12.0 (10.9–13.1) | 1.2 (1.1–1.3) | 1.2 (1.0–1.3) | .0076 |
| Refused/missing | 42 (0.09) | 2 (0.04) | … | … | … | … |
| Highest education | ||||||
| Junior high | 9959 (21.1) | 1479 (26.6) | 14.9 (14.2–15.5) | 1.0 | 1.0 | |
| Senior high | 16 666 (35.2) | 2181 (39.3) | 13.1 (12.6–13.6) | .84 (.78–.90) | .97 (.90–1.1) | .4579 |
| College or above | 20 592 (43.6) | 1891 (34.1) | 9.2 (8.8–9.6) | .55 (.51–.59) | .70 (.64–.77) | <.0001 |
| Refused/missing | 14 (0.03) | 1 (0.02) | … | … | … | … |
| Household registration | ||||||
| Local resident | 26 607 (56.3) | 2921 (52.6) | 11.0 (10.6–11.4) | 1.0 | 1.0 | |
| Non–local resident | 20 601 (43.6) | 2626 (47.3) | 12.7 (12.3–13.2) | 1.1 (1.05–1.2) | 1.2 (1.1–1.3) | <.0001 |
| Refused/missing | 23 (0.05) | 5 (0.09) | … | … | … | … |
| Sexual behavior in the past 6 mo | ||||||
| Venues for finding sex partners | ||||||
| Bars/tea houses/dance halls | 10 380 (22.0) | 1186 (21.4) | 11.4 (10.8–12.0) | 1.0 | 1.0 | |
| Public bathhouses/saunas | 6436 (13.6) | 1197 (21.6) | 18.6 (17.6–19.5) | 1.7 (1.5–1.8) | 1.4 (1.3–1.5) | <.0001 |
| Parks | 5461 (11.6) | 751 (13.5) | 13.8 (12.9–14.7) | 1.4 (1.3–1.6) | 1.2 (1.1–1.3) | .0024 |
| Internet sites | 21 444 (45.4) | 2033 (36.6) | 9.5 (9.1–9.9) | .85 (.78–.91) | .97 (.89–1.1) | .4801 |
| Other | 2681 (5.7) | 312 (5.6) | 11.6 (10.4–12.9) | 1.0 (.88–1.1) | 1.0 (.90–1.2) | .6048 |
| Refused/missing | 829 (1.7) | 73 (1.3) | … | … | … | … |
| Buy male sex | ||||||
| No | 44 541 (94.3) | 5209 (93.8) | 11.7 (11.4–12.0) | 1.0 | 1.0 | |
| Yes | 2543 (5.4) | 328 (5.9) | 12.9 (11.6–14.2) | .85 (.75–.96) | .94 (.82–1.1) | .3613 |
| Refused/missing | 147 (0.31) | 15 (0.27) | … | … | ||
| Sell sex to a male | ||||||
| No | 42 732 (90.5) | 4991 (89.9) | 11.7 (11.4–12.0) | 1.0 | 1.0 | |
| Yes | 4358 (9.2) | 553 (10.0) | 12.7 (11.7–13.7) | .91 (.83–1.0) | .96 (.89–1.1) | .5458 |
| Refused/missing | 141 (0.30) | 8 (0.14) | … | … | ||
| No. of male sex partners | ||||||
| 0 | 5886 (12.5) | 545 (9.8) | 9.3 (8.5–10.0) | 1.0 | 1.0 | |
| 1 | 13 421 (28.4) | 1279 (23.0) | 9.5 (9.0–10.0) | 1.0 (.92–1.1) | 1.1 (1.0–1.3) | .0267 |
| 2–10 | 22 370 (47.4) | 2958 (53.3) | 13.2 (12.8–13.7) | 1.4 (1.3–1.6) | 1.5 (1.3–1.7) | <.0001 |
| >10 | 2372 (5.0) | 368 (6.6) | 15.5 (14.1–17.0) | 1.7 (1.5–1.9) | 1.7 (1.4–1.9) | <.0001 |
| Refused/missing | 3182 (6.7) | 402 (7.2) | … | … | … | … |
| Consistent condom use with male partners | ||||||
| No | 24 107 (51.0) | 3085 (55.6) | 12.8 (12.4–13.2) | 1.0 | 1.0 | |
| Yes | 16 720 (35.4) | 1862 (33.5) | 11.1 (10.7–11.6) | .81 (.76–.86) | .71 (.64–.79) | <.0001 |
| No sex in past 6 mo | 5886 (12.5) | 545 (9.8) | 9.3 (8.5–10.0) | .69 (.63–.76) | .65 (.55–.76) | <.0001 |
| Refused/missing | 518 (1.1) | 60 (1.0) | … | … | … | … |
| No. of female sex partners | ||||||
| 0 | 35 495 (75.2) | 4196 (75.6) | 11.8 (11.5–12.2) | 1.0 | 1.0 | |
| 1 | 8401 (17.8) | 1040 (18.7) | 12.4 (11.7–13.1) | 1.0 (.96–1.1) | .86 (.75–.98) | <.0001 |
| ≥2 | 2699 (5.7) | 261 (4.7) | 9.7 (8.6–10.8) | .81 (.71–.93) | .67 (.54–.84) | <.0001 |
| Refused/missing | 636 (1.3) | 55 (1.0) | … | … | … | … |
| Study design | ||||||
| Sampling method | ||||||
| Snowball | 43 437 (92.0) | 5024 (90.5) | 11.6 (11.3–11.9) | 1.0 | 1.0 | |
| RDS | 3794 (8.0) | 528 (9.5) | 13.9 (12.8–15.0) | 1.4 (1.2–1.6) | 1.4 (1.2–1.5) | <.0001 |
| City-level characteristics | ||||||
| Administrative level | ||||||
| Directly under central government | 6051 (12.8) | 776 (14.0) | 12.8 (12.0–13.7) | 1.6 (.90–2.9) | 1.5 (.87–2.6) | .1384 |
| Province capitals | 23 422 (49.6) | 2913 (52.5) | 12.4 (12.0–12.9) | 1.5 (1.1–2.0) | 1.4 (1.04–1.8) | .0257 |
| Other cities | 17 758 (37.6) | 1863 (33.6) | 10.5 (10.0–10.9) | 1.0 | 1.0 | |
| Overall | 47 231 (100) | 5552 (100) | 11.8 (11.5–12.0) | … | … | … |
Abbreviations: CI, confidence interval; OR, odds ratio; RDS, respondent-driven sampling.
a CIs are 95% CIs in all cases and were calculated by approximating the binomial distribution with a normal distribution.
b ORs and P values were calculated by using a multilevel logistic regression model.
c P values are 2-sided in all cases.
Prevalence and Risk Factors
The overall prevalence of HIV was 4.9% (95% CI, 4.7%–5.1%; 2314/47 231), and 92% of confirmed HIV-positive participants were notified of their serostatus. As shown in Table 1, syphilis-positive MSM had the highest HIV prevalence, 12.5% (95% CI, 11.6%–13.4%; 693/5552). Being >24 years of age (P < .0001), being divorced or widowed (P = .0156), being a non–local resident (P < .0001), having an active syphilis infection (P < .0001), finding sex partners in public bathhouses/saunas (P < .0001), buying sex from men (P = .0082), selling sex to men (P = .0012), and having >1 male sex partner (2–10 partners: P < .0001; >10 partners: P = .0001) were all associated with a higher probability of having an HIV infection. Having a college education (P < .0001), using condoms consistently when having sex with men (P < .0001), having at least 1 female sex partner (P = .0415), and having ≥2 partners (P = .0022) were all protective factors.
The overall prevalence of syphilis was 11.8% (95% CI, 11.5%–12.0%; 5552/47 231). As shown in Table 2, MSM aged 50–69 years had the highest syphilis prevalence, 23.2% (95% CI, 20.8%–25.6%; 274/1182). Being >24 years of age (P < .0001), being an ethnic minority (P = .0076), being a non–local resident (P < .0001), finding sex partners in public bathhouses/saunas (P < .0001) or parks (P = .0024), and having 1 or more male sex partners (1 partner: P = .0267, 2–10 partners: P < .0001; >10 partners: P < .0001) were all associated with a higher probability of syphilis infection. Having a college education (P < .0001), using condoms consistently when having sex with men (P < .0001), and having at least 1 female sex partner (1 partner: P < .0001; ≥2 partners: P < .0001) were all protective factors.
Sampling method is included as a variable in both Tables 1 and 2. Although we do find this factor to have a statistically significant association with the likelihood of having syphilis (Table 2), we do not find that the inclusion of the 8% of individuals sampled by RDS affected the overall prevalence values for HIV and syphilis significantly (HIV prevalence: 4.7% for snowball data only vs 4.9% overall; syphilis prevalence: 11.6% for snowball data only vs 11.8% overall).
Geographical Distributions
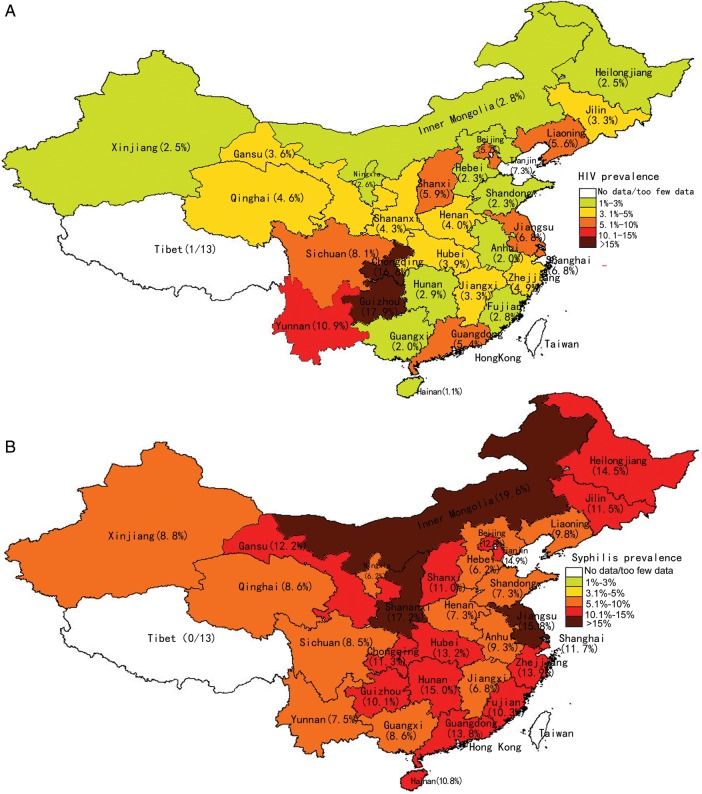
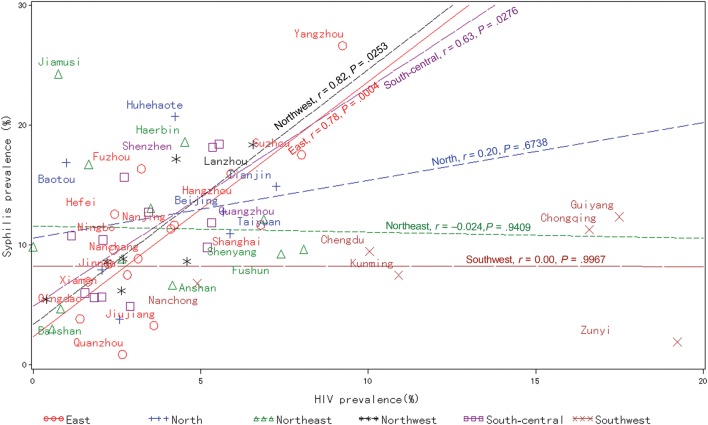
The median HIV prevalence was 3.4% at the city level and 3.8% at the provincial level. For syphilis, median prevalence was 9.7% at the city level and 10.2% at the provincial level. Figure 1 depicts provincial-level maps of both epidemics, color-coded to represent the geographical differences in HIV and syphilis prevalence. Detailed data on HIV and syphilis prevalence at the city, province, autonomous region, and municipality levels are available in Supplementary Table 3. Correlations found between HIV and syphilis prevalence in the 6 regions are shown in Figure 2. No correlation was detected in the North (r = 0.20, P = .6738), Northeast (r = –0.024, P = .9409), and Southwest (r = 0.00, P = .9967) regions, whereas HIV and syphilis prevalence were correlated in the Northwest (r = 0.82, P = .0253), East (r = 0.78, P = .0004), and South-central (r = 0.63, P = .0276) regions.
Figure 1.
Maps of China showing the geographical distribution at the provincial level of human immunodeficiency virus (A) and syphilis (B) prevalence among men who have sex with men. Abbreviation: HIV, human immunodeficiency virus.
Figure 2.
Human immunodeficiency virus prevalence was correlated with syphilis prevalence in the Northwest (r = 0.82, P = .0253), East (r = 0.78, P = .0004), and South-central (r = 0.63, P = .0276) regions. Pearson correlation coefficients are denoted as r and symbols represent individual cities. Lhasa City was treated as an outlier. Abbreviation: HIV, human immunodeficiency virus.
Description of 3 Subgroups
Three subgroups were identified among the broader sample and described: (1) MSM who were not local residents of the city surveyed (20 601/47 231, 43.6%), (2) MSM who used the Internet to find male sex partners (21 444/47 231, 45.4%), and (3) MSM who had at least 1 female sex partner in the past 6 months (11 633/47 231, 24.6%). Table 3 summarizes subgroup demographics, sexual behaviors, and knowledge and prevalence of HIV and syphilis. The profile of Internet-using MSM in our sample is that of young (aged 18–24 years, 11 095/21 444, 51.7%), never-married (18 024/21 444, 84.1%), college-educated (12 732/21 444, 59.4%) students (5781/21 444, 27.0%) and professionals (8553/21 444, 39.9%) who identify themselves as homosexual (13 657/21 444, 63.7%). By contrast, the profile of MSM who have had female partners is that of middle-aged (aged 30–49 years, 5985/11 633, 51.4%), married (5773/11 633, 49.6%), junior or senior high school–educated (8037/11 633, 69.1%) men who self-identify as bisexual (7871/11 633, 67.7%). The profile of nonlocal MSM falls in between these in many respects as they are of a similar age (18–24 years, 9795/20 601, 47.5%), marital status (never married, 15 974/20 601, 77.5%), and sexual orientation (homosexual, 11 404/20 601, 55.4%) profile relative to Internet-using MSM, but, similar to female-partnering MSM, have lesser educations (junior or senior high school, 12 128/20 601, 58.9%). In terms of sexual behavior, a greater proportion of MSM who have female partners reported buying sex from men (1086/11 633, 9.3%), and a similar proportion of female-partnering and nonlocal MSM reported selling sex to men (1550/11 633, 13.3% and 2961/20 601, 14.4%, respectively). The majority of both nonlocal MSM and Internet-using MSM do not have female partners (15 204/20 601, 73.8% and 17 760/21 444, 82.8%, respectively). HIV knowledge was highest among Internet users (17 718/21 444, 82.6%), and HIV and syphilis prevalence was highest among nonlocals (1253/20 601, 6.1% for HIV and 2626/20 601, 12.7% for syphilis).
Table 3.
Demographics, Sexual Behavior, and Knowledge and Prevalence of HIV and Syphilis Among 3 Subgroups of Men Who Have Sex With Men
| Characteristics | Nonlocal MSM, No. (%) | Internet- Using MSM, No. (%) | Female- Partnering MSM, No. (%) |
|---|---|---|---|
| Demographics | |||
| Age group, y | |||
| 18–24 | 9795 (47.5) | 11095 (51.7) | 3334 (28.7) |
| 25–29 | 4270 (20.7) | 5050 (23.5) | 1813 (15.6) |
| 30–34 | 2833 (13.8) | 2745 (12.8) | 2122 (18.2) |
| 35–39 | 1727 (8.4) | 1376 (6.4) | 1797 (15.4) |
| 40–49 | 1380 (6.7) | 1004 (4.7) | 2066 (17.8) |
| 50–69 | 272 (1.3) | 134 (0.6) | 395 (3.4) |
| Refused/ missing | 324 (1.6) | 40 (0.2) | 106 (0.9) |
| Marital status | |||
| Never married | 15 974 (77.5) | 18 024 (84.1) | 5258 (45.2) |
| Married | 3498 (17.0) | 2615 (12.2) | 5773 (49.6) |
| Live with a partnera | 330 (1.6) | 254 (1.2) | 228 (2.0) |
| Divorced/ widowed | 794 (3.9) | 547 (2.6) | 369 (3.2) |
| Refused/ missing | 5 (0.0) | 4 (0.0) | 5 (0.0) |
| Highest education | |||
| Junior high | 5161 (25.1) | 2242 (10.5) | 3523 (30.3) |
| Senior high | 6967 (33.8) | 6468 (30.2) | 4514 (38.8) |
| College or above | 8468 (41.1) | 12 732 (59.4) | 3590 (30.9) |
| Refused/ missing | 5 (0.0) | 2 (0.0) | 6 (0.1) |
| Household registration | |||
| Local resident | 0 (0.0) | 9622 (44.8) | 5357 (46.1) |
| Non–local resident | 20 601 (100.0) | 11 815 (55.1) | 6270 (53.9) |
| Refused/ missing | 0 (0.0) | 7 (0.1) | 6 (0.1) |
| Occupation | |||
| Student | 3232 (15.7) | 5781 (27.0) | 652 (5.6) |
| Professionalb | 9722 (47.2) | 8533 (39.8) | 5863 (50.4) |
| Factory worker | 1938 (9.4) | 1823 (8.5) | 1915 (16.5) |
| Farmerc | 575 (2.8) | 184 (0.9) | 361 (3.1) |
| Migrant worker | 44 (0.2) | 28 (0.1) | 58 (0.5) |
| Other | 3815 (18.5) | 3665 (17.0) | 1937 (16.7) |
| Unemployed | 1275 (6.2) | 1430 (6.7) | 847 (7.3) |
| Sexual orientation | |||
| Homosexual | 11 404 (55.4) | 13 657 (63.7) | 2539 (21.8) |
| Bisexual | 7477 (36.3) | 6422 (29.9) | 7871 (67.7) |
| Heterosexual | 536 (2.6) | 232 (1.1) | 562 (4.8) |
| Not sure | 1058 (5.1) | 1028 (4.8) | 599 (5.1) |
| Refused/ missing | 126 (0.6) | 105 (0.5) | 62 (0.5) |
| Sexual behavior with men in the past 6 mo | |||
| Venues for finding male sex partners | |||
| Bars/tea houses/ dance halls | 4258 (20.7) | 0 (0.0) | 3038 (26.1) |
| Public bathhouses/ saunas | 2969 (14.4) | 0 (0.0) | 2236 (19.2) |
| Parks | 2054 (10.0) | 0 (0.0) | 1882 (16.2) |
| Internet sites | 9622 (46.7) | 21 444 (100.0) | 3646 (31.3) |
| Other | 1231 (6.0) | 0 (0.0) | 682 (5.9) |
| Refused/ missing | 467 (2.3) | 0 (0.0) | 149 (1.3) |
| Noncommercial sex | |||
| No. of male partners | |||
| 0 | 2248 (10.9) | 2444 (11.4) | 1797 (15.4) |
| 1 | 5113 (24.8) | 6903 (32.2) | 2758 (23.7) |
| 2–10 | 10 243 (49.7) | 10 173 (47.4) | 5616 (48.3) |
| >10 | 1537 (7.5) | 660 (3.1) | 729 (6.3) |
| Refused/ missing | 1460 (7.1) | 1264 (5.9) | 733 (6.3) |
| Consistent condom use with male partnersd | |||
| No | 10 364 (56.5) | 10 792 (56.8) | 5601 (56.9) |
| Yes | 7730 (42.1) | 7967 (41.9) | 4130 (42.0) |
| Refused/ missing | 259 (1.4) | 241 (1.3) | 105 (1.1) |
| Commercial sex | |||
| Buying sex from men | |||
| No | 19 331 (93.8) | 20 674 (96.4) | 10 507 (90.3) |
| Yes | 1196 (5.8) | 714 (3.3) | 1086 (9.3) |
| Refused/ missing | 74 (0.4) | 56 (0.3) | 40 (0.3) |
| Consistent condom use when buying sex from mend | |||
| No | 523 (41.2) | 255 (33.1) | 507 (45.0) |
| Yes | 687 (54.1) | 468 (60.8) | 591 (52.5) |
| Refused/ missing | 60 (4.7) | 47 (6.1) | 28 (2.5) |
| Selling sex to men | |||
| No | 17 568 (85.3) | 20 170 (94.1) | 10 043 (86.3) |
| Yes | 2961 (14.4) | 1224 (5.7) | 1550 (13.3) |
| Refused/ missing | 72 (0.3) | 50 (0.2) | 40 (0.3) |
| Consistent condom use when selling sex to mend | |||
| No | 1108 (36.5) | 415 (32.6) | 567 (35.7) |
| Yes | 1849 (61.0) | 810 (63.6) | 994 (62.5) |
| Refused/ missing | 76 (2.5) | 49 (3.8) | 29 (1.8) |
| Sexual behavior with women in the past 6 mo | |||
| No. of female partners | |||
| 0 | 15 204 (73.8) | 17 760 (82.8) | 0 (0.0) |
| 1 | 3522 (17.1) | 2714 (12.7) | 8399 (72.2) |
| ≥2 | 1515 (7.4) | 746 (3.5) | 2690 (23.1) |
| Refused/ missing | 360 (1.7) | 224 (1.0) | 544 (4.7) |
| Consistent condom use with female partnersd | |||
| No | 3495 (64.8) | 2350 (63.8) | 8030 (69.0) |
| Yes | 1705 (31.6) | 1222 (33.2) | 3394 (29.2) |
| Refused/ missing | 197 (3.7) | 112 (3.0) | 209 (1.8) |
| HIV and syphilis knowledge and prevalence | |||
| Accurate HIV knowledgee | |||
| Yes | 15 056 (73.1) | 17 718 (82.6) | 7928 (68.2) |
| No | 5545 (26.9) | 3726 (17.4) | 3705 (31.8) |
| HIV and syphilis infection status | |||
| HIV-positive | 1253 (6.1) | 973 (4.5) | 506 (4.3) |
| Syphilis-positive | 2626 (12.7) | 2033 (9.5) | 1347 (11.6) |
| HIV/syphilis- positive | 375 (1.8) | 241 (1.1) | 155 (1.3) |
| Overall | 20 601 (100.0) | 21 444 (100.0) | 11 633 (100.0) |
Abbreviations: HIV, human immunodeficiency virus; MSM, men who have sex with men.
a Living with a partner, male or female.
b Includes teachers, doctors, nurses, and other service industry professionals.
c Includes farmers, fishermen, and herdsmen.
d Consistent condom use only calculated for those who report having had sex in the past 6 months.
e Accurate knowledge of HIV transmission and prevention determined by correctly answering at least 6 of 8 questions.
DISCUSSION
Two Epidemics: High, but Mostly Separate
Among the 47 231 Chinese MSM in our sample, we find prevalence estimates of 4.9% (2314/47 231) for HIV and 11.8% (5552/47 231) for syphilis, results that are generally consistent with several recent studies [7–10]. Since this study was conducted, the Ministry of Health of the People's Republic of China estimated that HIV prevalence among China's MSM was approximately 6.3% in 2011, which suggests that the HIV epidemic is still expanding among this population [13]. The risk and protective factors identified for having HIV and syphilis infections are not unexpected. We found characteristics such as older age and risky sexual behavior (ie, large numbers of sex partners) to be associated with increased probability of having HIV or syphilis, whereas characteristics including higher education and safer sexual behavior (ie, consistent condom use) were protective factors.
On analysis of correlations between HIV and syphilis prevalence among MSM in China's 6 geographical regions, we find no correlation in the Southwest, North, and Northeast regions, yet we do detect correlations in the Northwest, South-central, and East regions. We believe that the pattern we observed may have emerged as a result of the unique progression of the HIV epidemic and the pattern of resurgence of syphilis in China [14–16]. Historically, transmission via needle sharing by drug users had been the major driver of the early HIV epidemic (1985–2005), which was initially limited to the Southwest. It has only been more recently, as the epidemic has matured, that sexual contact has become the primary transmission route nationwide, a transition that likely bridged infection from the drug user population to the MSM population [14]. Because sexually transmitted infections such as syphilis are thought to increase the sexual transmission efficiency of the HIV virus [4], one could speculate that syphilis had an impact in facilitating the spread of HIV only after sexual transmission became more dominant, and that by that time, the HIV epidemic was already well established in southwestern China. Although syphilis was nearly eradicated in China during the 1960s, it was still present in small pockets in remote areas of northern China [15], and began spreading rapidly beginning in 1993 [16]. The high prevalence of syphilis in the North and Northeast regions suggests that although high-risk sexual behavior among MSM is present, HIV has not yet penetrated this population. We interpret this as a significant opportunity to save lives by increasing public health efforts focused on HIV prevention in these areas.
Three Subgroups: Nonlocal, Internet-Using, and Female-Partnering MSM
We find different profiles of characteristics and behaviors in 3 segments of our MSM sample that suggests they may represent “growth fronts” in the HIV and syphilis epidemics—bridges of infection across geographies (non–local resident MSM), generations (Internet-using MSM), and sexes (female-partnering MSM).
Nonlocal MSM
China's migrant workforce is often characterized as poor, uneducated, rural farmers or laborers who seek work in large cities and who are more likely to engage in high-risk sexual behavior, less likely to have accurate HIV knowledge, and more likely to have sexually transmitted infections [17–22]. By contrast, most nonlocal MSM in our sample are unmarried professionals who do not identify themselves as migrant workers. We find that relatively more engage in commercial sex with men and roughly half consistently use condoms with men across settings, but HIV knowledge is high. In this context, it is not surprising to find high HIV and syphilis prevalence among the nonlocal MSM subgroup.
Internet-Using MSM
Despite the Internet becoming a major venue for Chinese MSM to seek male sex partners [12, 21, 23], we find no association between this venue and HIV or syphilis prevalence; Internet-using MSM show the lowest HIV and syphilis prevalence among all 3 subgroups. Although this has been observed in a few other studies, the reasons have been unclear [24, 25]. However, we find that Internet-using MSM are the youngest, most educated, and most likely to self-identify as homosexual and have the greatest HIV knowledge, lowest engagement in commercial sex, and highest rate of consistent condom use compared to the other subgroups. This young age profile has also been observed in Internet-based sampling studies [21, 26]. This effect of age on prevalence could be due to a lack of sufficient exposures or undetected acute infections.
Female-Partnering MSM
The large number of MSM who report having female partners confirms the high prevalence of bisexuality among Chinese MSM described previously [27, 28]. Compared to the other 2 subgroups, female-partnering MSM tend to be older, married, and less educated. They have higher rates of engagement in commercial sex, the lowest rates of condom use, and display the least HIV knowledge. However, though the results of this study show that having a female partner is protective for MSM, having a bisexual partner is likely dangerous for uninfected women [27–29]. In fact, the lowest rate of consistent condom use found in this study was in the context of MSM having sex with female partners. This is consistent with a previous study that reported a mere 26% of Chinese MSM consistently use condoms with female partners [27]. Alarmingly, another study found that 68% of Chinese MSM who know they are HIV-positive continue to have unprotected sex with female partners [29].
Limitations
Our cross-sectional study is inherently observational and descriptive; thus, we cannot infer causality. Because only large cities were sampled, our results may not be generalizable to small towns and rural areas. Our national prevalence figures result from aggregating prevalence in individual cities; therefore, these data must be interpreted with caution. Because our study relied on self-reported data, risk behaviors may be underestimated. As participants were asked the frequency of risk behaviors over the previous 6 months, misclassification of exposures may have occurred. Although we cannot be certain our sample is representative, we do believe that our large sample size and our use of multiple sampling techniques improve its representativeness. The recruitment process for this study was led by CDC staff, which may have resulted in some selection bias. Because the proportion of missing values was low, no sensitivity analysis or imputation was performed; however, missing values could still cause biases. Finally, because of our large sample size, the power of our statistical analysis may have ascribed significance to differences that were perhaps not meaningful.
CONCLUSIONS
In summary, the results presented here offer an important characterization of the HIV and syphilis epidemics among MSM in China that can advise future national and international evidence-based policy decisions. HIV transmission among MSM must be made a top priority in China's national HIV/AIDS strategy and should be supported by sufficient resources to increase coverage of effective interventions addressing the unique care and prevention needs of MSM.
Supplementary Data
Supplementary materials are available at Clinical Infectious Diseases online (http://cid.oxfordjournals.org/). Supplementary materials consist of data provided by the author that are published to benefit the reader. The posted materials are not copyedited. The contents of all supplementary data are the sole responsibility of the authors. Questions or messages regarding errors should be addressed to the author.
Notes
Acknowledgments. The authors thank men who have sex with men (MSM) community leaders with the MSM & HIV Expert Panel; Beichuan Zhang, Yaqi Guo, Ge Tong, Xiaodong Wang, Ran An, Lin Meng, and Tao Hong, who provided consultancy for development of survey protocol and revision of the survey questionnaire; MSM community organizations for helping in community mobilization prior to the survey; all the subjects who participated in the survey; and Roger Detels and Sheena Sullivan for their valuable comments and suggestions.
The National MSM Survey Group included the following investigators: Steering Committee: Z. Wu, Y. Wang, Y. Hao, X. Sun, N. Wang, J. Sun, J. Xu, Y. Mao, Y. Xiao, Y. Liu, M. Bulterys, and R. Yip. Participating Institutions and Principal Staff: Chinese CDC, National Center for AIDS/STD Control and Prevention. Protocol Group: K. Rou, H. Hu, L. Wang, Y. Jiang, F. Zhang, H. Xing, R. Yip, J. Zhao, Z. Li, K. Zhou, Y. Cui, X. Zhang, Y. Liu, J. Xu, and Y. Xiao. Implementation Monitoring Group: J. Xu, Y. Xiao, Y. Feng, H. Liu, W. Ma, W. Xing, Y. Bao, Z. Dou, H. Tang, J. Xu, H. Zhou, S. Wang, and G. Mi. Laboratory Group: Y. Jiang, W. Xing, and H. Xing. Data Group: Y. Mao, L. Pang, W. Ma, and E Liu. Local Implementation Group: Anhui Provincial CDC: G. Ji, B. Su, X. Chen; Anhui Hefei CDC: Z. Li; Anhui Wuhu CDC: J. He; Beijing CDC: H. Lu, X. Ma; Fujian CDC: L. Lin, W. Pan; Fujian Xiamen CDC: G. Ma; Fujian Quanzhou CDC: C. Gong; Gansu CDC: A. Yu, A. Tu, J. Li; Gansu Lanzhou CDC: Y. Li; Gansu Tianshui CDC: F. Quan; Gangdong CDC: P. Lin, Y. Wang, Q. He; Guangdong Guangzhou CDC: F. Zhong; Guangxi CDC: W. Liu, G. Lan; Guangxi Nanning CDC: S. Chen; Guangxi Liuzhou CDC: Y. Bai; Guizhou CDC: L. Shen, Y. Yao; Guizhou Guiyang CDC: F. Yuan; Guizhou Zunyi CDC: H. Guo; Hainan CDC: Q. He, Z. Wang; Hainan Haikou CDC: F. Feng; Hebei CDC: L. Liang; Hebei Shijiazhuang CDC: S. Li; Hebei Baoding CDC: Y. Hou; Henan CDC: Z. Wang, Q. Liu; Henan Zhengzhou CDC: Z. Liu; Henan Louyang CDC: B. Tang; Heilongjiang CDC: H. Yan; Heilongjiang Haerbin CDC: L. Wang; Heilongjiang Qiqihaer CDC: X. Zhang; Heilongjiang Modanjiang CDC: X. Guo; Heilongjiang Jiamoshi CDC: Z. Zhao; Hubei CDC: F. Zhan, L. Li; Hubei Wuhan CDC: P. Liu; Hubei Xiangfan CDC: A. Xie; Hubei Jinzhou CDC: A. Mao; Hunan CDC: X. Chen, J. Zheng; Hunan Changsha CDC: X. Huang; Hunan Changde CDC: J. Nie; Jilin CDC: W. Guo; Jilin Changchun CDC: J. Yu; Jilin Jilin CDC: Y. Chai; Jilin Baishan CDC: G. Feng; Jilin Yanbian CDC: X. Sun; Jiangsu CDC: H. Yang, H. Xi, H. Yan; Jiangsu Nanjing CDC: M. Zhang; Jiangsu Suzhou CDC: X. Zhao; Jiangsu Yangzhou CDC: D. Zhu; Jiangxi CDC: G. Hu, F. Lu; Jiangxi Nanchang CDC: D. Xu; Jiangxi Jiujiang CDC: Y. Sun; Liaoning CDC: C. Lu, N. Ma; Liaoning Shenyang CDC: Y. Gu; Liaoning Dalian CDC: W. Tong; Liaoning Anshan CDC: L. Zhao; Liaoning Fuxun CDC: X. Wang; Inner Mongolia CDC: B. Tao, J. Yang; Inner Mongolia Huhehaote CDC: Z. Yun; Inner Mongolia Baotou CDC: J. Wang; Ninxia CDC: J. Zhao; Ninxia Yinchuan CDC: Z. Miao; Qinghai CDC: Y. Ma, M. Fan; Qinghai Xining CDC: C. Zhao; Shandong CDC: J. Fu, Y. Qian; Shandong Jinan CDC: S. Ruan; Shandong Qingdao CDC: Z. Jiang; Shanxi CDC: S. Yuan, X. Qiao; Shanxi Taiyuan CDC: L. Mei; Shannxi CDC: W. Chang, A. Xing, Y. Lu; Shanghai CDC: Q. Pan, Z. Ning; Sichuan CDC: N. Zhang, T. Li, W. Huang; Sichuan Chengdu CDC: X. Liang; Sichuan Nancong CDC: D. Tan; Tianjing CDC: M. Yu; Tibet CDC: L. Yuzhen; Xinjiang CDC: F. Li, M. Xiao; Xinjiang Wulumuqi CDC: X. Wang; Xinjiang Akesu CDC: J. Zhang; Yunnan CDC: X. Ming, Y. Wang, H. Lou; Zhejiang CDC: X. Pan; Zhejiang Hangzhou CDC: S. Chen; Zhejiang Ninbo CDC: D. Zhang; Zhejiang Shaoxin CDC: L. Fu; Chongqing CDC: L. Feng, X. Ding, J. Xu.
Author contributions. Z. W., J. X., E. L., Y. M., Y. X., and Y. W. designed the study. X. S. and Y. L. coordinated the study. J. X., Y. M., Y. X., Y. L., Y. J., Z. D., G. M., N. W., J. S., Z. L., L. W., K. R., L. P., W. X., J. X., S. W., Y. C., Z. L., M. B., and J. Z. collected the data. E. L. did primary data analysis and W. L. and Y. W. contributed to part of the analysis. Z. W., E. L., and J. M. M. drafted the paper. Z. W. had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Financial support. This study was supported by the Chinese Government AIDS Program; the Bill & Melinda Gates Foundation (grant number 49277); the Global Fund Against AIDS, Tuberculosis and Malaria (CHN-405-G05-H and CHN-506-G06-H); the Global AIDS Program of the US Centers for Disease Control and Prevention (1U2GPS001188-01); and the China Multidisciplinary AIDS Prevention Training Program with the US National Institutes of Health (grant number U2RTW06918, funded by the Fogarty International Center, National Institute on Drug Abuse, and National Institute of Mental Health).
Disclaimer. The opinions expressed herein reflect the collective views of the coauthors and do not necessarily represent the official position of the Chinese Ministry of Health, National Center for AIDS/STD Control and Prevention, Chinese CDC, US Centers for Disease Control and Prevention, US National Institutes of Health, Bill & Melinda Gates Foundation, or Global Fund Against AIDS, Tuberculosis and Malaria. The funding organizations had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript.
Potential conflicts of interest. All authors: No reported conflicts.
All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
References
- 1.Baral S, Sifakis F, Cleghorn F, Beyrer C. Elevated risk for HIV infection among men who have sex with men in low- and middle-income countries 2000–2006: a systematic review. PLoS Med. 2007;4:e339. doi: 10.1371/journal.pmed.0040339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Brahmam GN, Kodavalla V, Rajkumar H, et al. Sexual practices, HIV and sexually transmitted infections among self-identified men who have sex with men in four high HIV prevalence states of India. AIDS. 2008;22(suppl 5):S45–57. doi: 10.1097/01.aids.0000343763.54831.15. [DOI] [PubMed] [Google Scholar]
- 3.van Griensven F, Varangrat A, Wimonsate W, et al. Trends in HIV prevalence, estimated HIV incidence, and risk behavior among men who have sex with men in Bangkok, Thailand, 2003–2007. J Acquir Immune Defic Syndr. 2010;53:234–9. doi: 10.1097/QAI.0b013e3181c2fc86. [DOI] [PubMed] [Google Scholar]
- 4.Galvin SR, Cohen MS. The role of sexually transmitted diseases in HIV transmission. Nat Rev Microbiol. 2004;2:33–42. doi: 10.1038/nrmicro794. [DOI] [PubMed] [Google Scholar]
- 5.Morineau G, Nugrahini N, Riono P, et al. Sexual risk taking, STI and HIV prevalence among men who have sex with men in six Indonesian cities. AIDS Behav. 2011;15:1033–44. doi: 10.1007/s10461-009-9590-6. [DOI] [PubMed] [Google Scholar]
- 6.Sirivongrangson P, Lolekha R, Charoenwatanachokchai A, et al. HIV risk behavior among HIV-infected men who have sex with men in Bangkok, Thailand. AIDS Behav. 2012;16:618–25. doi: 10.1007/s10461-011-9884-3. [DOI] [PubMed] [Google Scholar]
- 7.Gao L, Zhang L, Jin Q. Meta-analysis: prevalence of HIV infection and syphilis among MSM in China. Sex Transm Infect. 2009;85:354–8. doi: 10.1136/sti.2008.034702. [DOI] [PubMed] [Google Scholar]
- 8.Li HM, Peng RR, Li J, et al. HIV incidence among men who have sex with men in China: a meta-analysis of published studies. PLoS One. 2011;6:e23431. doi: 10.1371/journal.pone.0023431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chow EP, Wilson DP, Zhang J, Jing J, Zhang L. Human immunodeficiency virus prevalence is increasing among men who have sex with men in China: findings from a review and meta-analysis. Sex Transm Dis. 2011;38:845–57. doi: 10.1097/OLQ.0b013e31821a4f43. [DOI] [PubMed] [Google Scholar]
- 10.Chow EP, Wilson DP, Zhang L. HIV and syphilis co-infection increasing among men who have sex with men in China: a systematic review and meta-analysis. PLoS One. 2011;6:e22768. doi: 10.1371/journal.pone.0022768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Choi KH, Diehl E, Guo Y, Qu S, Mandel J. High HIV risk but inadequate prevention services for men in China who have sex with men: an ethnographic study. AIDS Behav. 2002;6:255–66. [Google Scholar]
- 12.Guo Y, Li X, Fang X, et al. A comparison of four sampling methods among men having sex with men in China: implications for HIV/STD surveillance and prevention. AIDS Care. 2011;23:1400–9. doi: 10.1080/09540121.2011.565029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ministry of Health, People's Republic of China. Beijing, China: Ministry of Health; 2012. 2012 China AIDS response progress report. [Google Scholar]
- 14.Ministry of Health, People's Republic of China. Beijing, China: Ministry of Health: 2011. 2011 estimates for the HIV/AIDS epidemic in China. [Google Scholar]
- 15.Chen X. Epidemic updates and control strategies of syphilis in China. Inter J Epidemiol Infect Dis. 2008;35:73–6. [Google Scholar]
- 16.Chen ZQ, Zhang GC, Gong XD, et al. Syphilis in China: results of a national surveillance programme. Lancet. 2007;369:132–8. doi: 10.1016/S0140-6736(07)60074-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chen XS, Peeling RW, Yin YP, Mabey DC. The epidemic of sexually transmitted infections in China: implications for control and future perspectives. BMC Med. 2011;9:111. doi: 10.1186/1741-7015-9-111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Guo Y, Li X, Song Y, Liu Y. Bisexual behavior among Chinese young migrant men who have sex with men: implications for HIV prevention and intervention. AIDS Care. 2012;24:451–8. doi: 10.1080/09540121.2011.613914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hu Z, Liu H, Li X, Stanton B, Chen X. HIV-related sexual behaviour among migrants and non-migrants in a rural area of China: role of rural-to-urban migration. Public Health. 2006;120:339–45. doi: 10.1016/j.puhe.2005.10.016. [DOI] [PubMed] [Google Scholar]
- 20.Rou K, Sullivan SG, Liu P, Wu Z. Scaling up prevention programmes to reduce the sexual transmission of HIV in China. Int J Epidemiol. 2010;39(suppl 2):ii38–46. doi: 10.1093/ije/dyq211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Guo Y, Li X, Stanton B. HIV-related behavioral studies of men who have sex with men in China: a systematic review and recommendations for future research. AIDS Behav. 2011;15:521–34. doi: 10.1007/s10461-010-9808-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Shi TX, Zhang BC, Li XF. Study on HIV/AIDS related high risk behaviors among unmarried men who have sex with women [in Chinese] Zhonghua Liu Xing Bing Xue Za Zhi. 2009;30:10–3. [PubMed] [Google Scholar]
- 23.Hong FC, Zhou H, Cai YM, et al. Prevalence of syphilis and HIV infections among men who have sex with men from different settings in Shenzhen, China: implications for HIV/STD surveillance. Sex Transm Infect. 2009;85:42–4. doi: 10.1136/sti.2008.031682. [DOI] [PubMed] [Google Scholar]
- 24.Lau JT, Lau M, Cheung A, Tsui HY. A randomized controlled study to evaluate the efficacy of an Internet-based intervention in reducing HIV risk behaviors among men who have sex with men in Hong Kong. AIDS Care. 2008;20:820–8. doi: 10.1080/09540120701694048. [DOI] [PubMed] [Google Scholar]
- 25.Tsui HY, Lau JT. Comparison of risk behaviors and socio-cultural profile of men who have sex with men survey respondents recruited via venues and the internet. BMC Public Health. 2010;10:232. doi: 10.1186/1471-2458-10-232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lee SS, Tam DK, Mak DW, Wong KH. Use of the Internet for sex partnership in men who have sex with men before HIV infection. Public Health. 2011;125:433–5. doi: 10.1016/j.puhe.2011.03.010. [DOI] [PubMed] [Google Scholar]
- 27.Chow EP, Wilson DP, Zhang L. What is the potential for bisexual men in China to act as a bridge of HIV transmission to the female population? Behavioural evidence from a systematic review and meta-analysis. BMC Infect Dis. 2011;11:242. doi: 10.1186/1471-2334-11-242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Yun K, Xu JJ, Reilly KH, et al. Prevalence of bisexual behaviour among bridge population of men who have sex with men in China: a meta-analysis of observational studies. Sex Transm Infect. 2011;87:563–70. doi: 10.1136/sextrans-2011-050079. [DOI] [PubMed] [Google Scholar]
- 29.He Q, Peng WJ, Zhang JQ, Wang BX, Wang J. Prevalence of unprotected anal intercourse and unprotected vaginal intercourse among HIV-positive men who have sex with men in China: a meta-analysis. Sex Transm Infect. 2012;88:229–33. doi: 10.1136/sextrans-2011-050230. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.