Abstract
The Army Physical Evaluation Board results for wounded warriors from a previously described cohort were reviewed to identify permanently disabling conditions and whether the conditions were preexisting or caused by battlefield injury. Arthritis was the most common unfitting condition in this cohort, with 94.4% of cases attributed to combat injury and only 5.6% attributed to preexisting conditions or documented in the health records prior to battle injury. The most common causes of injury that resulted in arthritis were intra-articular fractures secondary to explosions, traumatic arthrotomies resulting from fragment projectiles, and gunshot wounds. Arthritis was recognized as a disabling condition an average of 19 ± 10 months after injury. Research is needed to enhance prevention and management of joint injuries in order to minimize the disabling effects of joint degeneration in this young patient population.
Osteoarthritis (OA) consumes a tremendous amount of medical resources and causes considerable disability. OA is the most common cause of disability in adults, affecting nearly 27 million people in the United States and accounting for an estimated $2,600 to $7,500 in out-of-pocket expense per person per year.1-3 In 2004, primary OA accounted for 22.3% of the 50.3 million non-injury ambulatory care visits and 70% of nonfederal short stay hospital admissions.2
In the United States, financial losses resulting from disability and cost of total joint arthroplasties total at least $21 billion each year.4,5 According to the World Health Organization, OA has the fourth greatest impact of all diseases on years of life lost due to disability.6 The prevalence of OA is highest in persons aged ≥65 years, and the burden of OA as a global health concern is rising with the increasingly aging population.2 In 2004 dollars, the cost of arthritis rose from $184.3 billion in 1996 to $281.5 billion in 2004.2
The causes of OA are seldom delineated in reports of prevalence, cost, and resource utilization. Many studies report on heterogeneous populations, which makes it difficult to infer the impact of OA on a definite patient population. Specifically, no one has yet fully differentiated the burden of degenerative OA in older persons versus OA resulting from traumatic injury, which is more common in younger persons.7 Thus, the impact of OA on morbidity in terms of injury and days of work lost in young and middle-aged populations is likely to be underestimated.8 Brown et al9 estimated that 12% of symptomatic OA is attributable to posttraumatic osteoarthritis (PTOA) of the hip, knee, or ankle, with an aggregate financial burden of $3.06 billion annually, or 0.15% of the total direct healthcare costs in the United States.
OA is the most common cause of disability among service members who are medically separated from active duty.10 It affects a spectrum of service members, from the young enlisted person (the most commonly injured demographic in combat) to the older, senior ranking person with degenerative OA following a career of military service.11
The current Overseas Contingency Operations—primarily in Iraq and Afghanistan—have placed a large number of young service members at risk of traumatic injury.12 Military healthcare providers are seeing younger combat-wounded patients with joint injuries, and it is important to determine whether OA in younger combat-wounded warriors is caused by traumatic injury or is a preexisting degenerative condition.
METHODS
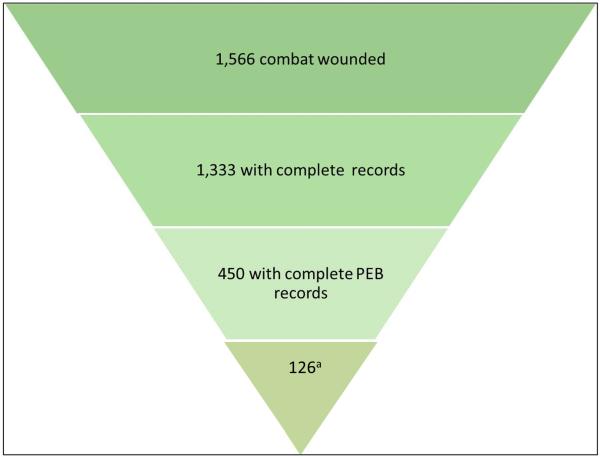
The study population, which consists of 1,566 combat-injured warriors who could not return to duty, has been characterized elsewhere.11 A previous study carefully reviewed the results of the US Army Physical Evaluation Board (PEB) and available medical documentation on 450 battlefield-wounded warriors10 (Figure 1). Each warrior was evaluated by the PEB to determine which conditions caused by combat injuries resulted in permanent disability (Figure 2). In the 126 patients with OA as an unfitting condition, the patients and conditions were fully characterized using the PEB medical records. The records were carefully reviewed to determine affected anatomic region, cause of arthritis (ie, battle injury, preexisting), and average disability rating. The anatomic regions injured in the study population were reviewed, and the rate of OA following injury to the specific regions was determined.
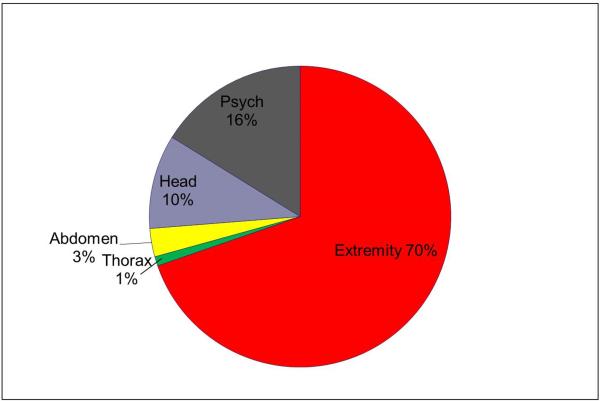
Figure 1.
Pie charts demonstrating that, of 450 patients who underwent a US Army Physical Examination Board evaluation to determine fitness for duty or retention in military service, 70% were found to have an unfitting condition that involved at least one extremity. These soldiers are presumed to be otherwise fit for duty.10 Psych = psychiatric condition.
Figure 2.
Of 1,566 combat-wounded warriors from a previously published cohort, complete records with US Army Physical Evaluation Board (PEB) findings of 450 warriors were available for review and analysis.10
a Warriors with osteoarthritis as an unfitting condition (out of 450).
RESULTS
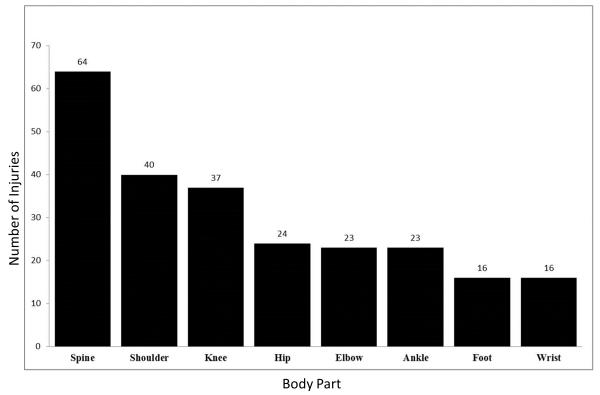
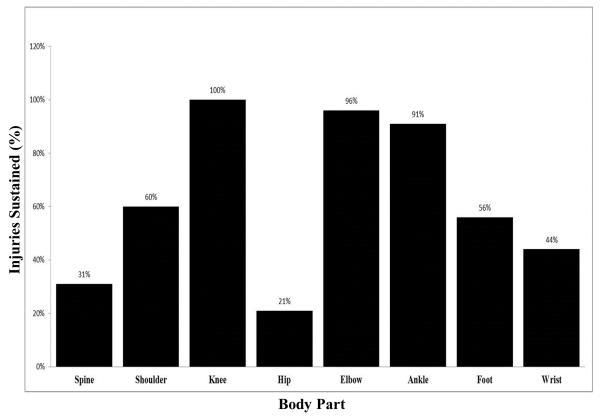
Among those with OA as an unfitting condition, injuries to the spine and shoulder occurred most commonly (Figure 3). The rate of arthritis by injured anatomic region varied considerably. Injuries to the knee resulted in OA in all cases, and the elbow and ankle joints became arthritic following injury in >90% of cases (Figure 4). In contrast, the hip became arthritic following injury in only 21% of cases.
Figure 3.
Graphic representation of the number of injuries per body part in our cohort. Injuries to the spine and shoulder were the most common.
Figure 4.
Graphic representation of the rate of occurrence of osteoarthritis (OA) by injured anatomic region. Although the knee was the third most commonly injured anatomic region in the cohort, injuries to the knee resulted in OA 100% of the time. In contrast, injuries to the spine, the most commonly injured anatomic region, resulted in OA only 31% of the time.
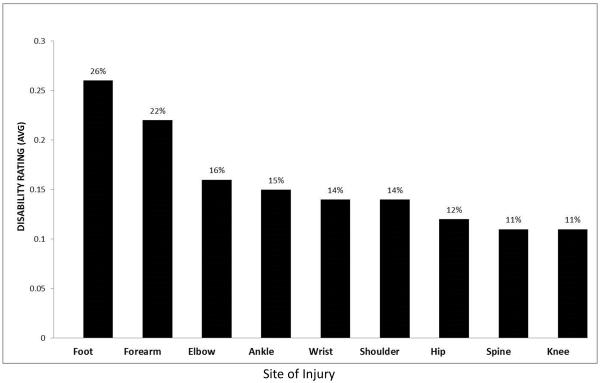
Our study included 125 cases of joint OA, 7 of which were the result of predeployment conditions and 118 of which were the result of war-related injury. Of the 20 cases of spine OA, 5 were the result of predeployment conditions and 15 were the result of war-related injury. Thus, traumatic injury was the cause of 94.4% of all cases of joint OA and 75% of cases of spine OA (Table 1). Fractures and arthrotomies resulting from explosive devices caused 75% of these OA conditions. Average disability rating varied greatly. The foot had the highest rating, and the knee and spine had the lowest (26% and 11%, respectively) (Figure 5). Arthritis was diagnosed, recognized as a disabling condition, and documented in the medical records at an average of 19 ± 10 months after injury.
Table 1.
Mechanisms of Injury Attributed to All 145 Unfitting conditionsa
| Injuries | ||
|---|---|---|
| Mechanism | Number | Percentage |
| Fracture from explosion | 92 | 63 |
| Arthrotomy due to projectiles resulting from an explosion |
17 | 12 |
| Soft-tissue injury from explosion |
9 | 6 |
| Gunshot wound | 14 | 10 |
| Fall | 1 | <1 |
| Condition prior to deployment | 12 | 8 |
| TOTAL | 145 | 100 |
145 unique injuries resulted in osteoarthritis in 126 individuals.
Figure 5.
Graphic representation of the average disability rating per site of injury. The average disability rating varied greatly by affected body region, with the foot receiving the highest rating and the knee and spine the lowest.
DISCUSSION
PTOA is a common and disabling condition in combat-wounded warriors. The prevalence of OA was 28% in our study population, compared with 12% in the civilian trauma population.9 In our patients, PTOA was directly attributable to combat injury in 92% of cases and to a preexisting condition in 8%. The permanent disability resulting from combat-related traumatic arthritis is substantial. The diagnosis of arthritis is accelerated in this group, with an average time of <2 years from injury to determination of disability as a result of arthritis. PTOA affects not only the appendicular joints but is disabling following injury to the spine, as well.
Reports in the civilian trauma literature confirm that intra-articular injuries often result in poor outcomes and that tolerance to joint injury varies by anatomic site. Acetabular fracture is associated with fair to poor postoperative outcomes in 24% to 43% of patients.13-15 Short-term studies indicate that the tibial plateau is more tolerant of joint injury than is the acetabulum; however, poor intra-articular reduction, joint instability, meniscus pathology, and malalignment can contribute to poor outcomes in the knee.16-19 Furthermore, fixation of the tibial plateau does not prevent the need for early total joint arthroplasty.20 Twelve percent to 36% of total knee replacements are performed to address traumatic arthritis. 9,21 Fractures of the tibial plafond result in a 74% rate of PTOA and notably increased pain, decreased quality of life measures, and decreased recreational activity function compared with noninjured ankles.22-24 Intra-articular injury is common in war wounds. In a large series of combat-wounded subjects, 77.1% of limb injuries included an intra-articular bony injury.25 Serious fragment injuries affect not only the articular surface of the joint but also the surrounding soft-tissue and neurovascular structures, thereby contributing to a poorer outcome.25
In our cohort, injuries were most commonly caused by explosion, resulting in multiple injuries per casualty with a high frequency of open fractures and soft-tissue wounds. These high-energy injuries cause all of the reported predictors of poor outcome following intra-articular injury: primary high-energy insult to the articular cartilage, comminuted joint surface, articular bone loss, soft-tissue damage that can lead to instability, and open and contaminated wounds that are susceptible to infectious complications.8
PTOA is anticipated to be a significant burden on those directly affected by it and on the healthcare system. The current generation of wounded warriors will require significant expenditures for lifelong care of this progressively degenerative condition. Dominick et al26 reported that US veterans experience a higher frequency of OA, chronic joint symptoms, and activity limitations than do persons in the general population. Reports of arthritis requiring joint arthroplasty following combat injury indicate good outcomes at 2- to 3-year follow-up.27,28 However, the average age of these wounded warriors is much lower than that of the general arthroplasty population with degenerative OA.28 Wounded warriors who require arthroplasty at a young age to manage joint injury are likely to need revision procedures and to face more years than their older counterparts of joint-related symptoms, activity limitations, and risks associated with revision arthroplasty.
One weakness of this study is the retrospective nature of the data collection. We did not have access to the subjects’ full medical records, which may have provided greater detail on the injuries, treatments, degree of comminution at the joint surfaces, and the surgical methods and results of management of intraarticular injuries. Radiographs were not available for assessment of comminution, articular step-off, or radiographic evidence of arthritis. Therefore, the definition of arthritis for the purposes of this article likely is not comparable to that of other investigations. However, the heterogeneity of diagnostic criteria has been noted in previous studies of OA and PTOA. Idiopathic OA is defined as symptomatic limitation of the affected joint with documented structural changes. PTOA is defined as symptomatic limitation of joint function with structural changes in a patient with a documented history of joint injury.9 However, debate exists with regard to the minimum amount of energy transfer required to qualify as PTOA as well as with regard to chronicity of symptoms, magnitude of symptoms, and the temporal relationship between injury and presentation of symptoms. For the purposes of our study, PTOA was defined as symptoms presenting in a patient who sustained battlefield or wartime injuries with symptoms significant enough to limit his or her military duties.
SUMMARY
This study is the first to report that PTOA is common in the battlefield-injured population and that PTOA can be directly related to combat injury. War injuries about the joints lead to arthritis following 60% of injuries, with the highest rate (100%) following knee injury. Providers who manage acute injuries in the military population need to understand how best to minimize the impact of high-energy joint injuries in terms of future risk of PTOA. Research that leads to better management of joint injuries is warranted to minimize the disabling effects of joint degeneration in this population. Areas of focus could include: (1) delineation of the requisite trauma and the signaling process that initiates chondrocyte necrosis versus autophagy versus apoptosis, (2) identification of nonsurgical methods to assess cartilage injury (ie, noncontrast MRI, biomarkers, nuclear medicine), (3) identification of clear patient-related factors that contribute to the development of OA (eg, sex, age, body mass index, smoking), (4) identification of clear injury-related factors that contribute to the development of OA (eg, mechanism of injury; extent of cartilage damage; injury to meniscus, ligament, synovium, vascular tissues; bone involvement), and (5) identification of clear treatment-related factors that contribute to the development of OA (ie, possible therapeutic and chondrotoxic effects of intra-articularly applied medications, timing of surgery for intra-articular injuries, optimum rehabilitation strategies for postoperative and nonsurgical management of articular injuries).
Acknowledgments
Dr. Wenke or an immediate family member has received research or institutional support from BIOnova Medical. Dr. Buckwalter or an immediate family member serves as a paid consultant to ISTO Technologies, Carbylan BioSurgery, and the Musculoskeletal Transplant Foundation and serves as a board member, owner, officer, or committee member of the American Orthopaedic Association. Dr. Ficke or an immediate family member serves as a board member, owner, officer, or committee member of the American Orthopaedic Foot and Ankle Society, American Academy of Orthopaedic Surgeons, Society of Military Orthopaedic Surgeons, and Airlift Research Foundation. Dr. Johnson or an immediate family member is a member of a speakers’ bureau or has made paid presentations on behalf of Pfizer, serves as a paid consultant to the US Food and Drug Administration, has stock or stock options held in Pfizer, and serves as a board member, owner, officer, or committee member of the Society of Military Orthopaedic Surgeons. Neither Dr. Rivera nor any immediate family member has received anything of value from or has stock or stock options held in a commercial company or institution related directly or indirectly to the subject of this article. Dr. Buckwalter’s research is supported by National Institutes of Health Award P50 AR055533.
This study was conducted under a protocol reviewed and approved by the San Antonio Military Medical Center Institutional Review Board, and in accordance with the approved protocol.
The opinions or assertions contained herein are the private views of the authors and are not to be construed as official or as reflecting the views of the Department of the Army or the Department of Defense.
References
- 1.Gabriel SE, Crowson CS, Campion ME, O’Fallon WM. Direct medical costs unique to people with arthritis. J Rheumatol. 1997;24(4):719–725. [PubMed] [Google Scholar]
- 2.American Academy of Orthopaedic Surgeons . The Burden of Musculoskeletal Diseases in the United States: Prevalence, Societal and Economic Cost. American Academy of Orthopaedic Surgeons; Rosemont, IL: 2008. [Google Scholar]
- 3.Lawrence RC, Felson DT, Helmick CG, et al. National Arthritis Data Workgroup: Estimates of the prevalence of arthritis and other rheumatic conditions in the United States: Part II. Arthritis Rheum. 2008;58(1):26–35. doi: 10.1002/art.23176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Buckwalter JA, Saltzman C, Brown T. The impact of osteoarthritis: Implications for research. Clin Orthop Relat Res. 2004;(427 suppl):S6–S15. doi: 10.1097/01.blo.0000143938.30681.9d. [DOI] [PubMed] [Google Scholar]
- 5.Lethbridge-Cejku M, Helmick CG, Popovic JR. Hospitalizations for arthritis and other rheumatic conditions: Data from the 1997 National Hospital Discharge Survey. Med Care. 2003;41(12):1367–1373. doi: 10.1097/01.MLR.0000100582.52451.AC. [DOI] [PubMed] [Google Scholar]
- 6.Reginster JY, Khaltaev NG. Introduction and WHO perspective on the global burden of musculoskeletal conditions. Rheumatology (Oxford) 2002;41(suppl 1):1–2. [PubMed] [Google Scholar]
- 7.Buckwalter JA, Brown TD. Joint injury, repair, and remodeling: Roles in posttraumatic osteoarthritis. Clin Orthop Relat Res. 2004;(423):7–16. [PubMed] [Google Scholar]
- 8.Bureau of Labor Statistics [Accessed June 25, 2012];Nonfatal Occupational Injuries and Illness Requiring Days Away From Work. 2010 [news release]. Available at: http://www.bls.gov/news.release/archives/osh2_11092011.pdf.
- 9.Brown TD, Johnston RC, Saltzman CL, Marsh JL, Buckwalter JA. Posttraumatic osteoarthritis: A first estimate of incidence, prevalence, and burden of disease. J Orthop Trauma. 2006;20(10):739–744. doi: 10.1097/01.bot.0000246468.80635.ef. [DOI] [PubMed] [Google Scholar]
- 10.Cross JD, Ficke JR, Hsu JR, Masini BD, Wenke JC. Battlefield orthopaedic injuries cause the majority of long-term disabilities. J Am Acad Orthop Surg. 2011;19(suppl 1):S1–S7. doi: 10.5435/00124635-201102001-00002. [DOI] [PubMed] [Google Scholar]
- 11.Owens BD, Kragh JF, Jr, Macaitis J, Svoboda SJ, Wenke JC. Characterization of extremity wounds in Operation Iraqi Freedom and Operation Enduring Freedom. J Orthop Trauma. 2007;21(4):254–257. doi: 10.1097/BOT.0b013e31802f78fb. [DOI] [PubMed] [Google Scholar]
- 12.Defense Casualty Analysis System [Accessed May 1, 2012];Global war on terrorism: Casualties by military service component, active, guard and reserve, October 7, 2001 through April 23, 2012. Available at: http://siadapp.dmdc.osd.mil/personnel/CASUALTY/gwot_component.pdf.
- 13.Matta JM. Fractures of the acetabulum: Accuracy of reduction and clinical results in patients managed operatively within three weeks after the injury. J Bone Joint Surg Am. 1996;78(11):1632–1645. [PubMed] [Google Scholar]
- 14.Mayo KA. Open reduction and internal fixation of fractures of the acetabulum: Results in 163 fractures. Clin Orthop Relat Res. 1994;(305):31–37. [PubMed] [Google Scholar]
- 15.Wright R, Barrett K, Christie MJ, Johnson KD. Acetabular fractures: Longterm follow-up of open reduction and internal fixation. J Orthop Trauma. 1994;8(5):397–403. doi: 10.1097/00005131-199410000-00005. [DOI] [PubMed] [Google Scholar]
- 16.Canadian Orthopaedic Trauma Society Open reduction and internal fixation compared with circular fixator application for bicondylar tibial plateau fractures: Results of a multicenter, prospective, randomized clinical trial. J Bone Joint Surg Am. 2006;88(12):2613–2623. doi: 10.2106/JBJS.E.01416. [DOI] [PubMed] [Google Scholar]
- 17.Giannoudis PV, Tzioupis C, Papathanassopoulos A, Obakponovwe O, Roberts C. Articular step-off and risk of post-traumatic osteoarthritis: Evidence today. Injury. 2010;41(10):986–995. doi: 10.1016/j.injury.2010.08.003. [DOI] [PubMed] [Google Scholar]
- 18.Stevens DG, Beharry R, McKee MD, Waddell JP, Schemitsch EH. The longterm functional outcome of operatively treated tibial plateau fractures. J Orthop Trauma. 2001;15(5):312–320. doi: 10.1097/00005131-200106000-00002. [DOI] [PubMed] [Google Scholar]
- 19.Weigel DP, Marsh JL. High-energy fractures of the tibial plateau: Knee function after longer follow-up. J Bone Joint Surg Am. 2002;84(9):1541–1551. doi: 10.2106/00004623-200209000-00006. [DOI] [PubMed] [Google Scholar]
- 20.Diduch DR, Insall JN, Scott WN, Scuderi GR, Font-Rodriguez D. Total knee replacement in young, active patients: Long-term follow-up and functional outcome. J Bone Joint Surg Am. 1997;79(4):575–582. doi: 10.2106/00004623-199704000-00015. [DOI] [PubMed] [Google Scholar]
- 21.Saleh KJ, Sherman P, Katkin P, et al. Total knee arthroplasty after open reduction and internal fixation of fractures of the tibial plateau: A minimum five-year follow-up study. J Bone Joint Surg Am. 2001;83(8):1144–1148. doi: 10.2106/00004623-200108000-00002. [DOI] [PubMed] [Google Scholar]
- 22.Anderson DD, Van Hofwegen C, Marsh JL, Brown TD. Is elevated contact stress predictive of post-traumatic osteoarthritis for imprecisely reduced tibial plafond fractures? J Orthop Res. 2011;29(1):33–39. doi: 10.1002/jor.21202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Marsh JL, Weigel DP, Dirschl DR. Tibial plafond fractures: How do these ankles function over time? J Bone Joint Surg Am. 2003;85(2):287–295. [PubMed] [Google Scholar]
- 24.Marsh JL, McKinley T, Dirschl D, et al. The sequential recovery of health status after tibial plafond fractures. J Orthop Trauma. 2010;24(8):499–504. doi: 10.1097/BOT.0b013e3181c8ad52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Nikolić D, Jovanović Z, Popović Z, Vulović R, Mladenović M. Primary surgical treatment of war injuries of major joints of the limbs. Injury. 1999;30(2):129–134. doi: 10.1016/s0020-1383(98)00239-3. [DOI] [PubMed] [Google Scholar]
- 26.Dominick KL, Golightly YM, Jackson GL. Arthritis prevalence and symptoms among US non-veterans, veterans, and veterans receiving Department of Veterans Affairs Healthcare. J Rheumatol. 2006;33(2):348–354. [PubMed] [Google Scholar]
- 27.Haspl M, Pećina M, Orlić D, Cicak N. Arthroplasty after war injuries to major joints. Mil Med. 1999;164(5):353–357. [PubMed] [Google Scholar]
- 28.Kuklo TR, Heekin RD, Temple HT, Islinger RB, Horan PJ. A review of total joint replacement in active duty soldiers. Mil Med. 1997;162(3):201–204. [PubMed] [Google Scholar]