Abstract
Skeletal muscle injuries often leave lasting functional damage or pain. Muscle injuries are routinely treated conservatively, but the most effective treatment to promote the repair of injured muscles has not yet been established. Our previous report demonstrated that human peripheral blood-derived CD133+ cell transplantation to rat skeletal muscle injury models inhibited fibrosis and enhanced myogenesis after injury. However, the acquisition of a sufficient number of cells remains the limitation for clinical application, as the CD133+ population is rare in human blood. In this study, we applied a magnetic cell targeting system to accumulate transplanted cells in the muscle injury site and to enhance the regenerative effects of CD133+ cell transplantation, focusing on the fact that CD133+ cells are labeled with a magnetic bead for isolation. For the magnetic cell targeting, the magnet field generator was set up to adjust the peak of the magnetic gradient to the injury site of the tibialis anterior muscle, and 1×104 human peripheral blood CD133+ cells were locally injected into the injury site. This cell number is 10% of that used in the previous study. In another group, the same number of CD133+ cells was injected without magnetic force. The CD133+ cells transplanted with the magnetic force were more accumulated in the muscle injury site compared with the CD133+ cells transplanted without the magnetic force. In addition, the transplantation of CD133+ cells under the magnetic control inhibited fibrous scar formation and promoted angiogenesis and myogenesis, and also upregulated the mRNA expression of myogenic transcription factors, including Pax7, MyoD1 and Myogenin. However, the transplantation of CD133+ cells without the magnetic force failed to demonstrate these effects. Thus, our magnetic cell targeting system enables transplantation of a limited number of CD133+ cells to promote the repair of skeletal muscle injury.
Introduction
Skeletal muscle injuries occur frequently, especially in those that participate in sports. Myofibers are considered to have regenerative capacity, therefore, muscle injuries are routinely treated conservatively. However, fibrosis can progress, leading to incomplete muscle healing.1 Previous studies have examined the use of drugs, cytokines, cells, and gene therapy attempted to improve muscle recovery.2–10 Recently, we showed that transplantation of human peripheral blood CD133-expressing cells (CD133+ cells) inhibits fibrosis and improves muscle regeneration after skeletal muscle laceration.11 Human blood CD133+ cells are well-suited for clinical applications, because collecting these cells is safe, with limited ethical problems. However, obtaining a sufficient number of cells is the most important factor limiting clinical application, as the proportion of CD133+ cells to mononuclear cells (MNCs) in human blood is small.12
In this study, we used a magnetic cell targeting system to obtain a sufficient regenerative effect with a small number of CD133+ cells. In our magnetic cell targeting system, labeled cells can be guided into the desired region by a magnetic force from the extracorporeal device.13,14 The CD133+ cells were labeled with a magnetic bead, and isolated from human peripheral blood using a magnetic cell separation instrument.15 We hypothesized that immunomagnetic CD133+ cells administrated into muscle injury models could be targeted to a specific region of the body by a magnetic force, and that even a small number of these targeted CD133+ cells could promote skeletal muscle regeneration. Here we report that our magnetic cell targeting system promotes the regeneration of injured skeletal muscle by a limited number of CD133+ cells.
Materials and Methods
The Institutional Animal Care and Use Committees Of University of Hiroshima approved all animal procedures, including human cell transplantation.
Preparation of CD133+ cells for transplantation
CD133+ cells, isolated from granulocyte colony stimulating factor (G-CSF)-mobilized human peripheral blood-derived-MNCs by using a direct immunomagnetic CD133 MicroBeads labeling and a magnetic cell sorting system, were purchased from AllCells(Lot Number: PCA1521B, Purity tested by flow cytometry: 136%). CD133 MicroBeads is a highly specific CD133 monoclonal antibody conjugated to superparamagnetic particle with a diameter of ∼50 nm (20–100 nm). The superparamagnetic particle is nontoxic and biodegradable. When needed, frozen CD133+ cells were thawed, and resuspended in phosphate buffered saline (PBS).
External magnetic device
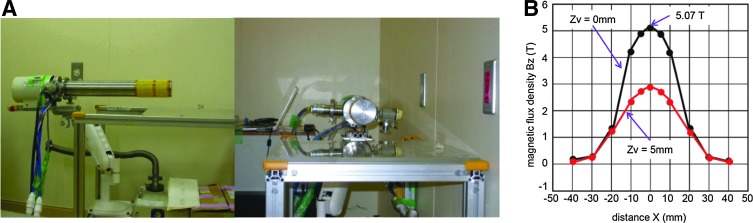
In the present study, to generate an external magnetic force (EMF), a portable superconducting bulk magnet system (Hitachi, Ltd., Mechanical Engineering Research Laboratory) was used as a magnetic field generator (Fig. 1A). The cylindrical shaped EMF system yields a large magnetic force, with the magnetic flux density at the surface of the vacuum chambers that contain the bulk magnets reaching 5.07 T under the static fields of 6 T. The magnet force tapers as the distance from the center of the device increases. The magnetic flux density at 5 mm from the surface of the vacuum chambers (position used in this study) was decreased to ∼3.0 T (Fig. 1B).16
FIG. 1.
(A) The portable superconducting bulk magnet system (Hitachi, Ltd., Mechanical Engineering Research Laboratory). (B) A graph of the magnetic flux density associated with the distance from the center of the magnetic device. The magnetic flux density at the surface of the vacuum chambers that contain the bulk magnets reached 5.07 T (black line). The magnet force tapers as the distance from the center of this device increases. The magnetic flux density used for this study at 5 mm from the surface of the vacuum chambers decreased to ∼3.0 T (red line).
Skeletal muscle injury model
The rat skeletal muscle injury model was generated as reported previously.11 Briefly, female F344/NJcl-rnu/rnu athymic nude rats (9 weeks old, n=39) were anesthetized using intraperitoneal pentobarbital sodium (50 mg/kg). The muscle belly of tibialis anterior muscle was lacerated transversely using a scalpel. The injury to the muscle was wedge-shaped, at 4 mm in width and 5 mm in depth. To examine the regenerative potential of a small number of CD133+ cells, we used one-tenth the number of transplanted CD133+ cells used in our previous study.11 The external magnetic device was set to direct the peak of the magnetic gradient to the injury site of the muscle, and 1×104 CD133+ cells resuspended with 30 μL of PBS were injected into the injury site after closure of the fascia. The rats were left under the EMF (3.0 T) for 10 min (CD133M group). As controls, the same number of CD133+ cells were transplanted in other injured rats without application of the EMF (CD133 group), or injured rats were administered 30 μL of PBS without CD133+ cells and were subjected to the same EMF as the experimental rats for 10 min (PBSM group).
Every evaluation was performed based on our previous report.11 The lacerated sites of all rats were observed macroscopically at 1 and 4 weeks after injury and evaluated electromechanically. After evaluation, the moist weight of the tibialis anterior muscles of both legs were measured, and these muscles were used for histological assessment (n=5 for each time point and group). For real-time reverse transcription–polymerase chain reaction (RT-PCR) analysis, the injured muscle tissues were collected at day 3 and 7 after injury, and were analyzed as described below. In this experiment, no animals showed infectious findings at any time.
Macroscopic assessment
Rats with muscle injuries were assessed macroscopically for repair at 1 and 4 weeks after injury. The occupying tissue that bridged lacerated sites were observed and photographed. The muscles were then subjected to electromechanical evaluation.
Functional assessment of injured muscle
We evaluated functional repair of the tibialis anterior muscles at 1 and 4 weeks after injury. The common peroneal nerve was stimulated, and isometric tensile strength was measured and recorded using transducer load cells (LVS-1KA; Kyowa Electronic Instruments), a sensor interface (PCD-300A; Kyowa Electronic Instruments), and a software program (PCD-30A; Kyowa Electronic Instruments), as described previously.6,7,11 Under anesthesia, common peroneal nerves were stimulated at 1 Hz (fast twitch) and 50 Hz (tetanus) using an electrostimulator (SEN-2201; Nihon Koden). To determine the optimal stimulation voltage, the minimum voltage that visibly contracted the tibialis anterior muscle was identified as the threshold. The common peroneal nerves were stimulated by a 10-fold threshold voltage, and the maximum isometric tensile strengths produced by the tibialis anterior muscles were measured. Data were normalized to nontreated controls (contralateral legs), to minimize inter-animal variation. The strength ratio (lacerated side to the contralateral side) was calculated for both fast twitch and tetanus stimulation.
Histological assessment
The regenerated tissues at 1 and 4 weeks after injury were frozen and sectioned at 6 μm on a cryostat. For evaluation of fibrosis and muscle regeneration, Masson trichrome staining was performed on sections from each sample. The average area of fibrosis in sagittal sections was digitized and analyzed using ImageJ software (National Institutes of Health).
Immunohistochemistry
Frozen sections from each sample at 1 week after injury were immunostained with the following primary antibodies: desmin (1:50; Santa Cruz Biotechnology), and von Willebrand factor protein (vWF, 1:1000; Abcam) to examine muscle regeneration and angiogenesis.9,11,17–20 To detect transplanted human cells, frozen sections were immunostained with a human mitochondrial antibody (hMit, 1:100; Millipore) just after injection, 1 day after injection and 1 week after injection. Secondary antibodies (1:500) were Alexa Fluor 568-conjugated goat anti-mouse IgG1 (Molecular Probes) for hMit, and Alexa Fluor 488 or 568-conjugated goat anti-rabbit IgG (Molecular Probes) for desmin and vWF protein. The sections were incubated in a 4,6-diamidino-2-phenylindole (DAPI) solution for 5 min to stain nuclei.
Real-time RT-PCR analysis
Analysis of mRNA levels of transcription factors promoting myogenesis (Pax7, MyoD1 and Myogenin) was performed in each group using real-time RT-PCR. Inflammatory cytokine production, such as tumor necrosis factor-α1 (TNF-α1), interleukin (IL)-6, IL-1β and transforming growth factor-β1 (TGF-β1), in transplanted muscle was also analyzed. Total RNA (12.3–48.2 μg) was obtained from regenerated tissues at day 3 and 7 after injury (n=6 in each group). An analysis of gene expression related to the inflammatory response at day 3 after the magnetic beads alone were applied at relevant quantities was also performed. For these experiments, the superparamagnetic MicroBeads conjugated with monoclonal mouse anti-human CD133 antibodies (Miltenyi Biotec) were resuspended in 30 μL of PBS, and injected at the injured site (Beads+ group). The administered dose of the MicroBeads per rat was equal to the quantity needed for the isolation of 1×105 CD133+ cells. Thereafter, the same volume of PBS alone was injected at the injured site as a control (Bead− group). First-strand cDNA was synthesized using the RNA LA PCR Kit version 3.0 (TaKaRa). Real-time PCR was performed using the MiniOpticon™ System (Biorad Laboratories) and QuantiTect™ SYBR green (Qiagen KK), according to the manufacturer's instructions. The mRNA expression levels were normalized to β-actin (ACTB). The ΔΔCt method was used for analysis of real-time RT-PCR data. The primer sequences are shown in Table 1.
Table 1.
The Characteristics of Primers Utilized for Real-Time Polymerase Chain Reaction
| Gene | Primer pair sequence for real-time PCR |
|---|---|
| rPax7 | F: 5′-GCCCTCAGTGAGTTCGATTAGC-3′ |
| R: 5′-TCCTTCCTCATCGTCCTCTTTC-3′ | |
| rMyoD1 | F: 5′-GCGACAGCCGATGACTTCTAT-3′ |
| R: 5′-GGTCCAGGTCCTCAAAAAAGC-3′ | |
| rMyogenin | F: 5′-GACCCTACAGGTGCCCACAA-3′ |
| R: 5′-ACATATCCTCCACCGTGATGCT-3′ | |
| rACTB | F: 5′-GATCATTGCTCCTCCTGAGCG-3′ |
| R: 5′-TGCTGATCCACATCTGCTGGA-3′ | |
| rTGF-β1 | F: 5′-CCACGTGGAAATCAATGGGA-3′ |
| R: 5′-GGCCATGAGGAGCAGGAAG-3′ | |
| rIL-1β | F: 5′-CACCTCTCAAGCAGACACAG-3′ |
| R: 5′-GGGTTCCATGGTGAAGTCAAC-3′ | |
| rIL-6 | F: 5′-TCCTACCCCAACTTCCAATGCTC-3′ |
| R: 5′-TTGGATGTCTTGGTCCTTACTCC-3′ | |
| rTNF-α1 | F: 5′-GTAGCCCACGTCGTAGCAAA-3′ |
| R: 5′-CCCTTCTCCAGCTGGAAGAC-3′ |
PCR, polymerase chain reaction.
Statistical analysis
The results are expressed as the means±standard deviation. Statistical analysis was performed by a one-way analysis of variance and subsequent Tukey's post hoc test. p-Values<0.05 were considered to be statistically significant.
Results
Experimental group
The external magnetic device directed the maximum value of the magnetic gradient to the injury site. A total of 1×104 CD133+ cells in 30 μL of PBS were injected into the muscle at the injury site after the fascia was closed, and rats were left under the EMF (3.0 T) for 10 min (CD133M group). In the control animals, the same number of CD133+ cells were transplanted without application of the EMF (CD133 group) or PBS alone was injected with application of EMF for 10 min (PBSM group). In these experiments, the number of transplanted CD133+ cells was one-tenth the number used in our previous study.11
Gross pathology of the lacerated muscle
The gross appearance of the lacerated muscles was assessed initially at 1 and 4 weeks after injury. Concavity was present in lacerated regions in all groups at 1 week after injury. At 4 weeks after injury, although flat bridging tissue was present at the injury site in all of the rats in the CD133M group, the lacerated regions showed significant concavity or protrusion in the PBSM and CD133 groups (Fig. 2A). These findings suggest that the transplantation of CD133+ cells and the application of magnetic force enhanced the bridging of muscle defects.
FIG. 2.
Assessment of the macroscopic and functional improvement. (A) Representative macroscopic pictures of the lacerated sites of the tibialis anterior muscles (arrows) at weeks 1 and 4 after injury. All pictures taken at 1 week after injury show concavity in the lacerated regions. At 4 weeks after injury, the lacerated region is smooth and filled with well-formed tissue only in the CD133M group. (B, C) Electromechanical assessments of injured muscles. The fast twitch strength ratio in the CD133M group was significantly greater than that in the PBSM group and CD133 group at 1 week after injury. At 4 weeks after injury, although there were no significant differences between the CD133 and PBSM groups in the fast twitch strength ratio, the fast twitch strength ratio in the CD133M group was significantly higher compared with the PBSM group (B). The tetanus strength ratio in the CD133M group was significantly higher than that in the CD133 and PBSM groups both at 1 week and 4 weeks after injury. The tetanus strength ratio in the CD133 group was significantly higher compared with the PBSM group only at 1 week after injury (C). (B, C) *p<0.05. **p<0.01.
Functional recovery of injured muscle
Tibialis anterior muscle tensile strength was examined to evaluate functional recovery at 1 week and 4 weeks after injury, by comparing the fast twitch and tetanus strength ratios of the three groups, as reported previously.11 No significant difference in the fast twitch strength ratio was observed between the CD133 and PBSM groups at either 1 or 4 weeks after injury. However, the fast twitch strength ratio of the CD133M group was significantly higher than that in either the CD133 or PBSM group at 1 week after injury and that of the PBSM group at 4 weeks after injury (Fig. 2B) (Table 2). The tetanus strength ratio of the CD133M group was significantly higher than that in the CD133 and the PBSM groups both at 1 week and 4 weeks after injury. The tetanus strength ratio in the CD133 group was significantly higher compared with the PBSM group at 1 week after injury, but there was no significant difference between the CD133 and PBSM groups at 4 weeks after injury (Fig. 2C). These results indicate that the transplantation of CD133+ cells with application of the magnetic force for 10 min promoted significant functional recovery of injured muscles compared to CD133+ cell transplantation without the magnetic force.
Table 2.
Summary of Histological and Functional Evaluations
| Evaluation headings | PBSM | CD133 | CD133M |
|---|---|---|---|
| Fast-twitch strength ratio (Lt/Rt) | |||
| 1 week | 0.53±0.03 | 0.56±0.05 | 0.75±0.04a,b |
| 4 week | 0.59±0.10 | 0.65±0.06 | 0.86±0.03a |
| Tetanus strength ratio (Lt/Rt) | |||
| 1 week | 0.33±0.07 | 0.57±0.04 | 0.80±0.03a,b |
| 4 week | 0.60±0.08 | 0.60±0.05 | 0.85±0.05a,b |
| Area of fibrosis (mm2) | |||
| 1 week | 8.90±1.93 | 5.86±0.78 | 1.37±0.16a,b |
| 4 week | 3.44±0.50 | 3.11±0.50 | 0.37±0.16a,b |
| % Regenerated area (%) | |||
| 1 week | 0.84±0.14 | 3.17±0.61 | 6.02±0.35a,b |
| Capillary density (n per mm2) | |||
| 1 week | 41.00±6.91 | 64.00±7.76 | 251.50±16.69a,b |
| hMit (n per mm2) | |||
| Right after injection | — | 261.14±52.32 | 599.48±74.41b |
| 1 day | — | 125.39±12.25 | 558.55±75.22b |
| 1 week | — | 13.33±3.74 | 164.00±14.70b |
| Gene expression (fold) at day 3 | |||
| Pax7 | 1.00±0.09 | 0.87±0.21 | 2.03±0.31a,b |
| MyoD1 | 1.00±0.08 | 0.83±0.14 | 2.29±0.19a,b |
| Myogenin | 1.00±0.22 | 0.80±0.17 | 3.27±0.60a,b |
| IL-1β | 3.37±0.35 | 3.68±0.66 | 3.50±0.22 |
| IL-6 | 11.72±2.37 | 10.54±2.16 | 10.25±0.75 |
| TNF-α1 | 2.41±0.46 | 1.59±0.22 | 2.50±0.46 |
| TGF-β1 | 12.48±0.97 | 14.69±2.38 | 5.69±0.32a,b |
| Gene expression (fold) at 1 week | |||
| Pax7 | 1.00±0.05 | 1.18±0.19 | 1.05±0.06 |
| MyoD1 | 1.00±0.12 | 1.23±0.25 | 1.23±0.15 |
| Myogenin | 1.00±0.07 | 1.08±0.16 | 2.66±0.06a,b |
| Bead− | Bead+ | ||
|---|---|---|---|
| Gene expression (fold) at day 3 | |||
| IL-1β | 1.00±0.30 | 0.86±0.16 | |
| IL-6 | 1.00±0.16 | 1.04±0.28 | |
| TNF-α1 | 1.00±0.15 | 1.02±0.14 | |
| TGF-β1 | 1.00±0.32 | 1.05±0.18 | |
p<0.05 versus PBSM.
p<0.05 versus CD133.
hMit, human mitochondrial antibody; Lt, left; Rt, right.
Morphological evaluation of muscle fibrosis
Masson trichrome staining was used to evaluate fibrosis histologically. The area of fibrosis in the CD133M group was significantly smaller compared with both the CD133 and PBSM groups at 1 week and 4 weeks after injury. However, the CD133 and PBSM groups at 1 week or 4 weeks after injury showed no significant difference with regard to the area of fibrosis (Fig. 3A, B) (Table 2).
FIG. 3.
Histological evaluation of injured skeletal muscles. (A, B) Assessments of fibrosis. In the examination of Masson trichrome staining, the area of fibrosis in the CD133M group was significantly smaller compared with both the CD133 and PBSM groups at 1 week and 4 weeks after injury. In contrast, the area of fibrosis in the CD133 group was not significantly different from that in the PBSM group at both 1 week and 4 weeks after injury. Scale bars: (A) 500 μm. (B) *p<0.05. **p<0.01.
Immunohistological assessment of muscle regeneration after cell transplantation
Immunofluorescent assessments were performed on axial sections of the injured sites at 1 week after injury. Desmin is widely used to distinguish individual cell types within the regenerating and central zone of a muscle injury. Desmin-positive myofibers were dispersed uniformly throughout the lacerated area in both the superficial and deep regions of the muscle. The desmin-positive area in the CD133 group was greater than that in the PBSM group, and that in the CD133M group was significantly greater compared to that of the other groups (Fig. 4A, B). To evaluate the extent of angiogenesis, vascular endothelial cells were stained for vWF. Neovascularization was enhanced significantly in the CD133M group compared with that in both the CD133 and PBSM groups (Fig. 5A–C) (Table 2).
FIG. 4.
Evaluation of myogenesis by immunohistochemistry. The desmin positive area, indicating myogenesis, in the CD133 group was greater than that in the PBSM group, and that in the CD133M group was significantly greater compared with the other groups (A, B). Green: Desmin, Blue: 4,6-diamidino-2-phenylindole (DAPI), Scale bars: 100 μm. Data were calculated as the means±standard error (SE). **p<0.01.
FIG. 5.
Immunohistochemical evaluation of angiogenesis and transplanted cells at 1 week after the injury (A–C). The von Willebrand factor protein (vWF) positive area indicates capillary vessels (A). The number of capillaries and the capillary density in the CD133 group were greater than in the PBSM and CD133 groups, although there were no significant differences between the CD133 and PBSM groups (B, C). (A) Green: vWF, Scale bars: 100 μm. (B, C) Data were calculated as the means±SE. **p<0.01. An immunohistochemical evaluation of human mitochondrial antibody (hMit) right after the injury and 1 day after the injury (D, E). The number of hMit+ cells calculated at the deep area in the CD133M-group was significantly higher compared with the CD133-group both right after and 1 day after the injury (D, E). Data were calculated as the means±SE. *p<0.05. At 1 week after injury, hMit+ cells could be detected in the lacerated area of the skeletal muscles in the CD133 and CD133M groups, although no hMit+ cells could be observed in the PBSM group (F). In addition, some hMit+ cells were located along the vWF+ vessels or incorporated into the vWF+ vessels at 1 week after the injury (F). The number of hMit+ cells in the CD133M group was significantly higher than that in the CD133 group (G). (F) Red: hMit, Green: wVF, Blue: DAPI, Scale bars: 100 μm. (G) Data were calculated as the means±SE. **p<0.01.
Accumulation of transplanted CD133+ cells
Tissue samples were immunostained with a human-specific antibody against mitochondria (hMit) transplanted CD133+ cells. hMit+ cells were observed in the injury site in both the CD133 and CD133M groups at just after the injection, at 1 day after injection, and at 1 week after injection. However, no hMit+ cells were detected in the PBSM group (Fig. 5D, F). The number of hMit+ cells at the bottom of the V-shaped injury site of muscles in the CD133M group was significantly higher than that in the CD133 group in each time period (Fig. 5E, 5G) (Table 2). In addition, a portion of hMit+ cells were located along the vWF+ vessels or incorporated into the vWF+ vessels (Fig. 5F).
Gene expression levels in recipient animals after CD133+ cell injection with EMF
To further evaluate skeletal myogenesis, mRNA expression levels of transcription factors promoting myogenesis, including Pax7, MyoD1, and Myogenin, were assessed by RT-PCR, using rat-specific primers. The expression levels of Pax7, MyoD1, and Myogenin were significantly higher in the CD133M group compared with the CD133 and PBSM groups at day 3 after injury. At day 7 after the injury, no significant differences between the three groups with regard to the expression of these factors were observed, except that Myogenin levels were significantly higher in the CD133M group compared to those in the CD133 and PBSM groups. However, there were no significant differences between the CD133 group and PBSM group with regard to the expression of these factors at either day 3 or 7 after the injury (Fig. 6A, B). The production of inflammatory cytokines, such as TNF-α1, IL-6, IL-1β and TGF-β1, in transplanted muscle was also evaluated at day 3 after injury. The levels of all these cytokines were increased in all groups after injury compared with uninjured muscle. There were no significant differences between groups with regard to gene expression, except for TGF-β1 expression. TGF-β1 expression in the CD133M group was significantly lower than that in the CD133 and PBSM groups (Fig. 6C). There were no significant differences between the Bead− and Beads+ groups with regard to the expression levels of TNF-α1, IL-6, IL-1β or TGF-β1 (Table 2) (Supplementary Fig. S1; Supplementary Data are available online at www.liebertpub.com/tec).
FIG. 6.
The mRNA expression levels of the transcription factors promoting myogenesis, including Pax7, MyoD1 and Myogenin on day 3 and 1 week after injury (A, B). The expression levels of Pax7, MyoD1, and Myogenin on day 3 were the highest in the CD133M group. However, there were no significant differences between the CD133 group and the PBSM group in the expression levels of these factors on day 3. The expression levels of Myogenin on 1 week were the highest in the CD133M group. However, there were no significant differences between three groups in the expression levels of Pax7 and MyoD1 on 1 week. The data were calculated as the means±SE. **p<0.01. The mRNA expression levels of the inflammatory cytokine production, including tumor necrosis factor-α1 (TNF-α1), interleukin (IL)-6, IL-1β and transforming growth factor-β1 (TGF-β1) on day 3 after injury (C). All of these factors in all groups were increased after injury compared with uninjured muscle. There were no significant differences between groups in the expression levels of TNF-α1, IL-6, and IL-1β. The expression level of TGF-β1 in CD133M group was significantly higher than other groups. The data were calculated as the means±SE. *p<0.05.
Discussion
Transplantation of CD133+ cells under external magnetic control enhances the accumulation of transplanted cells to the muscle injury site and promotes the regenerative process of the injured skeletal muscle, as indicated by the reduction of fibrosis and the acceleration of myogenesis. The magnetic cell targeting system enables the transplantation of a small number of CD133+ cells that is sufficient to promote the regeneration of injured skeletal muscle.
CD133+ cells formed cell colonies that generated cells of endothelial lineage and with endothelial properties in vitro.21 The transplantation of CD133+ cells has been reported to enhance neovascularization and tissue repair in animal models of a number of disorders in various tissues, including myocardium, peripheral nerve, nonvascularized fasciocutaneous free graft, spinal cord, axonal growth, and skeletal muscle.11,22–27 Our previous study showed that CD133+ cell transplantation enhances angiogenesis and inhibits fibrous scar formation through the upregulation of vascular endothelial growth factor expression and the downregulation of TGF-β1 expression. In that study, myofibers derived from the injected CD133+ cells were identified by double staining for MyoD1 and hMit. However, the number of differentiated cells was limited.11 Thus, the injection of CD133+ cells may simply stimulate muscle regeneration. In the present study, even though transplanted cells were observed at the muscle injury site and a portion of these cells were incorporated into blood vessels; these cells were too few to constitute a substantial portion of the vasculature or regenerating muscles. However, the administration of CD133+ cells with application of the magnetic force upregulated the mRNA expression of Pax7, MyoD1, and Myogenin, indicating increased myogenesis. These findings suggest that CD133+ cell transplantation accelerates endogenous angiogenesis and myogenesis after injury.
CD133+ cells are isolated from peripheral blood easily, and there are no major ethical or technical problems with their use. Kawamoto et al. demonstrated the efficacy and safety of intramuscular transplantation of magnetic bead-labeled CD34+ cells in patients with critical limb ischemia.28 The magnetic beads used in the separation of the CD34+ cells in their study were similar to those used for the CD133+ cells in our study. Magnetically-labeled CD133+ cells have minimal toxicity, and they should be applicable for clinical use. Indeed, this cell fraction is a possible candidate autologous therapeutic agent, but the small number of CD133+ cells in peripheral blood is an important factor limiting their clinical application.11 To obtain a sufficient CD133+ cell fraction, the administration of growth factors, such as G-CSF, is required.28 However, mobilization and economic issues should be considered if such treatment is necessary to obtain a sufficient number of these cells. In this study, we applied a magnetic cell targeting system to concentrate the CD133+ cells at the target site. In present study, the transplantation of CD133+ cells with EMF control was observed to enhance skeletal muscle regeneration. Although the transplantation of CD133+ cells without EMF failed to demonstrate these effects, a limited number of CD133+ cells accumulate around the injury site without EMF. The findings of immunostaining for human mitochondria showed that the accumulation of injected CD133+ cells at the injury site was enhanced by EMF, as indicated by immunopositive staining for human mitochondria. Additionally, our previous in vitro study demonstrated that EMF enhanced the adhesion of magnetically labeled mesenchymal stem cells through the upregulation of several cell adhesion molecules in the cells.29 Therefore, we suggest that EMF may prevent the diffusion of the injected cells from the injury site and enhance the adhesion of the CD133+ cells to the injury site. The increased accumulation and adhesion of transplanted cells in the injury site may contribute to the promotion of the regenerative process of the injured skeletal muscle, as indicated by the reduction in fibrosis and the acceleration of both angiogenesis and myogenesis. Our magnetic cell targeting system enabled the transplantation of a small number of CD133+ cells to promote functional and histological regeneration of injured muscles.
In this study, the magnetic force applied from outside the body enhanced the accumulation of transplanted cells in the muscle injury site. Previous studies have reported that cultured bone marrow stromal cells labeled with magnetic particles could be guided and gathered into a desired region by a magnetic force.13,14 However, the present study is the first report of magnetic cell targeting of freshly isolated cells in a muscle injury model without requiring their in vitro culture. These findings have important implications, especially for the treatment of skeletal muscle injury. One week after injury, which is the necrosis and inflammation phase, is the most critical phase for enhancing muscle regeneration.6 Autologous transplantation of cultured cells, which require a substantial time for establishment, is difficult to apply for the treatment of muscle injury, and may be ineffective for inducing recovery. Therefore, the ability to use the CD133+ cells immediately after isolation makes it possible to treat the injury much sooner.
In previous studies, the maximum magnetic flux density of the magnetic targeting system was ∼0.6 T.13 However, since magnetic beads combined with CD133 antibodies are smaller than the magnetic particles (ferumoxides) used for the labeling of cells in the previous study, the flux magnetic density may need to be larger to control the transplanted CD133+ cells. Therefore, we used a portable superconducting bulk magnet system, a more powerful magnetic field generator, for the present study. The bulk magnet system achieves a relatively higher magnetic density than permanent magnets or coil magnets. Moreover, since it has a high magnetic field gradient, the magnetic effect rapidly decreases with distance from the source. The magnetic flux density at 50 mm from the center of the surface of the vacuum chambers is 0.22 T.
Exposure to a magnetic field induced modifications of the cell shape, surface and cytoskeleton.30 The effects depended on the conditions, such as the duration of the exposure, magnetic density, and type of cell. In a previous report, in which these conditions were similar to those in our present study, an exposure of 4.75 T for up to 48 h had no proliferative, activating, or proinflammatory effects on peripheral blood MNCs.31
There are possible limitations to this study. First, in this study, the effect of EMF itself on the repair process of injured muscle was not examined. However, the degree of muscle repair in the PBSM group was approximately equal to that in the control group (PBS injection only in the same models) in our previous study,11 which suggests that the magnetic force does not directly affect the repair process of the injured muscle. Second, it was necessary to use athymic rats as experimental animals to use human-derived cells. However, inflammatory reactions are important for the healing process during the first week after muscle injury. Therefore, we assessed the gene expression of inflammatory cytokines, such as TNF-α1, IL-6, IL-1β and TGF-β1. In those experiments, the levels of these genes expressed from injured muscle were significantly increased compared with uninjured muscle. Therefore, an inflammatory reaction after muscle injury occurred even in the athymic immunosuppressed rats.
Conclusion
CD133+ cells transplanted into muscle injury models can be controlled by an external magnetic force, and even a small number of CD133+ cells can promote skeletal muscle regeneration when used in combination with our magnetic cell targeting system.
Supplementary Material
Acknowledgments
This work was partly supported by a grant-in-aid for scientific research from the Ministry of Education, Culture, Sports, Science and Technology-Japan (No. 21249079 to M.O.) and a grant from the General Insurance Association of Japan.
Disclosure Statement
The authors have declared no conflict of interest.
References
- 1.Moyer A.L. Wagner K.R. Regeneration versus fibrosis in skeletal muscle. Curr Opin Rheumatol. 2011;23:568. doi: 10.1097/BOR.0b013e32834bac92. [DOI] [PubMed] [Google Scholar]
- 2.Bacou F. el Andalousi R.B. Daussin P.A. Micallef J.P. Levin J.M. Chammas M. Casteilla L. Reyne Y. Nougues J. Transplantation of adipose tissue-derived stromal cells increases mass and functional capacity of damaged skeletal muscle. Cell Transplant. 2004;13:103. doi: 10.3727/000000004773301771. [DOI] [PubMed] [Google Scholar]
- 3.Chan Y.S. Li Y. Foster W. Fu F.H. Huard J. The use of suramin, an antifibrotic agent, to improve muscle recovery after strain injury. Am J Sports Med. 2005;33:43. doi: 10.1177/0363546504265190. [DOI] [PubMed] [Google Scholar]
- 4.Menetrey J. Kasemkijwattana C. Day C.S. Bosch P. Vogt M. Fu F.H. Moreland M.S. Huard J. Growth factors improve muscle healing in vivo. J Bone Joint Surg Br. 2000;82:131. doi: 10.1302/0301-620x.82b1.8954. [DOI] [PubMed] [Google Scholar]
- 5.Messina S. Mazzeo A. Bitto A. Aguennouz M. Migliorato A. De Pasquale M.G. Minutoli L. Altavilla D. Zentilin L. Giacca M. Squadrito F. Vita G. VEGF overexpression via adeno-associated virus gene transfer promotes skeletal muscle regeneration and enhances muscle function in mdx mice. FASEB J. 2007;21:3737. doi: 10.1096/fj.07-8459com. [DOI] [PubMed] [Google Scholar]
- 6.Nakasa T. Ishikawa M. Shi M. Shibuya H. Adachi N. Ochi M. Acceleration of muscle regeneration by local injection of muscle-specific microRNAs in rat skeletal muscle injury model. J Cell Mol Med. 2010;14:2495. doi: 10.1111/j.1582-4934.2009.00898.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Natsu K. Ochi M. Mochizuki Y. Hachisuka H. Yanada S. Yasunaga Y. Allogeneic bone marrow-derived mesenchymal stromal cells promote the regeneration of injured skeletal muscle without differentiation into myofibers. Tissue Eng. 2004;10:1093. doi: 10.1089/ten.2004.10.1093. [DOI] [PubMed] [Google Scholar]
- 8.Sheehan S.M. Tatsumi R. Temm-Grove C.J. Allen R.E. HGF is an autocrine growth factor for skeletal muscle satellite cells in vitro. Muscle Nerve. 2000;23:239. doi: 10.1002/(sici)1097-4598(200002)23:2<239::aid-mus15>3.0.co;2-u. [DOI] [PubMed] [Google Scholar]
- 9.Stratos I. Rotter R. Eipel C. Mittlmeier T. Vollmar B. Granulocyte-colony stimulating factor enhances muscle proliferation and strength following skeletal muscle injury in rats. J Appl Physiol. 2007;103:1857. doi: 10.1152/japplphysiol.00066.2007. [DOI] [PubMed] [Google Scholar]
- 10.Usas A. Huard J. Muscle-derived stem cells for tissue engineering and regenerative therapy. Biomaterials. 2007;28:5401. doi: 10.1016/j.biomaterials.2007.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Shi M. Ishikawa M. Kamei N. Nakasa T. Adachi N. Deie M. Asahara T. Ochi M. Acceleration of skeletal muscle regeneration in a rat skeletal muscle injury model by local injection of human peripheral blood-derived CD133-positive cells. Stem Cells. 2009;27:949. doi: 10.1002/stem.4. [DOI] [PubMed] [Google Scholar]
- 12.Yin A.H. Miraglia S. Zanjani E.D. Almeida-Porada G. Ogawa M. Leary A.G. Olweus J. Kearney J. Buck D.W. AC133, a novel marker for human hematopoietic stem and progenitor cells. Blood. 1997;90:5002. [PubMed] [Google Scholar]
- 13.Kobayashi T. Ochi M. Yanada S. Ishikawa M. Adachi N. Deie M. Arihiro K. A novel cell delivery system using magnetically labeled mesenchymal stem cells and an external magnetic device for clinical cartilage repair. Arthroscopy. 2008;24:69. doi: 10.1016/j.arthro.2007.08.017. [DOI] [PubMed] [Google Scholar]
- 14.Kobayashi T. Ochi M. Yanada S. Ishikawa M. Adachi N. Deie M. Arihiro K. Augmentation of degenerated human cartilage in vitro using magnetically labeled mesenchymal stem cells and an external magnetic device. Arthroscopy. 2009;25:1435. doi: 10.1016/j.arthro.2009.06.009. [DOI] [PubMed] [Google Scholar]
- 15.Yamamoto R. Ishikawa M. Tanaka N. Kamei N. Nakanishi K. Sasaki H. Nakamae T. Mochizuki Y. Asahara T. Ochi M. CD133+ cells from human peripheral blood promote corticospinal axon regeneration. Neuroreport. 2008;19:799. doi: 10.1097/WNR.0b013e3282ff6396. [DOI] [PubMed] [Google Scholar]
- 16.Saho N. Nishijima N. Tanaka H. Sasaki A. Development of portable superconducting bulk magnet system. Physica C. 2009;469:1286. [Google Scholar]
- 17.Foster W. Li Y. Usas A. Somogyi G. Huard J. Gamma interferon as an antifibrosis agent in skeletal muscle. J Orthop Res. 2003;21:798. doi: 10.1016/S0736-0266(03)00059-7. [DOI] [PubMed] [Google Scholar]
- 18.Fukushima K. Badiani N. Usas A. Usas A. Riano F. Fu F.H. Huard J. The use of an antifibrosis agent to improve muscle recovery after laceration. Am J Sports Med. 2001;29:394. doi: 10.1177/03635465010290040201. [DOI] [PubMed] [Google Scholar]
- 19.Li Y. Foster W. Deasy B.M. Chan Y. Prisk V. Tang Y. Cummins J. Huard J. Transforming growth factor-beta1 induces the differentiation of myogenic cells into fibrotic cells in injured skeletal muscle, a key event in muscle fibrogenesis. Am J Pathol. 2004;164:895. doi: 10.1016/s0002-9440(10)63188-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sato K. Li Y. Foster W. Fukushima K. Badlani N. Adachi N. Usas A. Fu F.H. Huard J. Improvement of muscle healing through enhancement of muscle regeneration and prevention of fibrosis. Muscle Nerve. 2003;28:365. doi: 10.1002/mus.10436. [DOI] [PubMed] [Google Scholar]
- 21.Masuda H. Alev C. Akimaru H. Ito R. Shizuno T. Kobori M. Horii M. Ishihara T. Isobe K. Isozaki M. Itoh J. Itoh Y. Okada Y. McIntyre B.A. Kato S. Asahara T. Methodological development of a clonogenic assay to determine endothelial progenitor cell potential. Circ Res. 2011;24:20. doi: 10.1161/CIRCRESAHA.110.231837. [DOI] [PubMed] [Google Scholar]
- 22.Bartunek J. Vanderheyden M. Vandekerckhove B. Mansour S. De Bruyne B. De Bondt P. Van Haute I. Lootens N. Heyndrickx G. Wijns W. Intracoronary injection of CD133-positive enriched bone marrow progenitor cells promotes cardiac recovery after recent myocardial infarction, feasibility and safety. Circulation. 2005;112(9 Suppl):I178. doi: 10.1161/CIRCULATIONAHA.104.522292. [DOI] [PubMed] [Google Scholar]
- 23.Kijima Y. Ishikawa M. Sunagawa T. Nakanishi K. Kamei N. Yamada K. Tanaka N. Kawamata S. Asahara T. Ochi M. Regeneration of peripheral nerve after transplantation of CD133+ cells derived from human peripheral blood. J Neurosurg. 2009;110:758. doi: 10.3171/2008.3.17571. [DOI] [PubMed] [Google Scholar]
- 24.Nakanishi M. Ishikawa M. Sunagawa T. Yokota K. Asahara T. Ochi M. The effects of CD133-positive cells to a nonvascularized fasciocutaneous free graft in the rat model. Ann Plast Surg. 2009;63:331. doi: 10.1097/SAP.0b013e3181934951. [DOI] [PubMed] [Google Scholar]
- 25.Sasaki H. Ishikawa M. Tanaka N. Nakanishi K. Kamei N. Asahara T. Ochi M. Administration of human peripheral blood-derived CD133+ cells accelerates functional recovery in a rat spinal cord injury model. Spine. 2009;34:249. doi: 10.1097/BRS.0b013e3181913cde. [DOI] [PubMed] [Google Scholar]
- 26.Tanaka N. Kamei N. Nakamae T. Yamamoto R. Ishikawa M. Fujiwara H. Miyoshi H. Asahara T. Ochi M. Kudo Y. CD133+ cells from human umbilical cord blood reduce cortical damage and promote axonal growth in neonatal rat organ co-cultures exposed to hypoxia. Int J Dev Neurosci. 2010;28:581. doi: 10.1016/j.ijdevneu.2010.07.232. [DOI] [PubMed] [Google Scholar]
- 27.Yang C. Zhang Z.H. Li Z.J. Yang R.C. Qian G.Q. Han Z.C. Enhancement of neovascularization with cord blood CD133+ cell-derived endothelial progenitor cell transplantation. Thromb Haemost. 2004;91:1202. doi: 10.1160/TH03-06-0378. [DOI] [PubMed] [Google Scholar]
- 28.Kawamoto A. Katayama M. Handa N. Kinoshita M. Takano H. Horii M. Sadamoto K. Yokoyama A. Yamanaka T. Onodera R. Kuroda A. Baba R. Kaneko Y. Tsukie T. Kurimoto Y. Okada Y. Kihara Y. Morioka S. Fukushima M. Asahara T. Intramuscular transplantation of G-CSF-mobilized CD34(+) cells in patients with critical limb ischemia, a phase I/IIa, multicenter, single-blinded, dose-escalation clinical trial. Stem Cells. 2009;27:2857. doi: 10.1002/stem.207. [DOI] [PubMed] [Google Scholar]
- 29.Nakamae T. Adachi N. Kobayashi T. Nagata Y. Nakasa T. Tanaka N. Ochi M. The effect of an external magnetic force on cell adhesion and proliferation of magnetically labeled mesenchymal stem cells. Sports Med Arthrosc Rehabil Ther Technol. 2010;2:5. doi: 10.1186/1758-2555-2-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Dini L. Abbro L. Bioeffects of moderate-intensity static magnetic fields on cell cultures. Micron. 2005;36:195. doi: 10.1016/j.micron.2004.12.009. [DOI] [PubMed] [Google Scholar]
- 31.Aldinucci C. Garcia J.B. Palmi M. Sgaragli G. Benocci A. Meini A. Pessina F. Rossi C. Bonechi C. Pessina G.P. The effect of strong static magnetic field on lymphocytes. Bioelectromagnetics. 2003;24:109. doi: 10.1002/bem.10071. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.