Abstract
Objective
The lack of well-described population-level outcome measures for emergency department (ED) HIV testing is one barrier to translation of screening into practice. We demonstrate the impact of an ED diagnostic testing and targeted screening program on the proportion of ED patients ever tested for HIV and explore cumulative effects on testing rates over time.
Methods
Data were extracted from electronic HIV testing program records and administrative hospital databases for January 2003 to December 2008 to obtain the monthly number of ED visits and HIV tests. We calculated the proportions of (1) patients tested in the program who reported a previous HIV test or had been previously tested in the program, and (2) the cumulative number of unique ED patients who were tested in our program.
Results
During the study period, 165,665 unique patients made 491,552 ED visits and the program provided 13,509 tests to 11,503 unique patients. From 2003 to 2008, tested patients who reported a history of an HIV test increased by 0.085% per month (95% confidence interval [CI] 0.037% to 0.133%), from 67.7% to 74.4%; the percentage of tested patients who had previous testing in the program increased by 0.277% per month (95% CI 0.245% to 0.308%), from 3.2% to 21.2%; and the percentage of unique ED patients previously tested in the program increased by 0.100% per month (95% CI 0.096% to 0.105%), reaching a cumulative proportion of 6.9%.
Conclusion
Our HIV testing program increased the proportion of ED patients who have been tested for HIV at least once and repeatedly tested a subset of individuals. HIV screening, even during a minority of ED visits, can have important cumulative effects over time.
INTRODUCTION
Background
Emergency departments (EDs) may offer ready access to a population at high risk for HIV infection,1 but the feasibility of universal screening of all eligible patients has been questioned and no ED has yet achieved this goal.2–7 Several EDs have partially succeeded at offering nontargeted screening to patients for a sizeable proportion of ED visits,8,9 but the sustainability and the ability to generalize such experiences to other EDs remains unclear.
Importance
Demonstrating the relative capacity of EDs to contribute to the goal of screening the US population for HIV is an important step in justifying the expansion of HIV testing in ED settings. If a policy recommendation is judged unfeasible, it might be discarded entirely rather than adopted incrementally as resources allow.2–5,8–11 Thus, the inability to test all eligible patients might inadvertently result in a failure to expand testing to the degree that it is feasible. Because many patients present to EDs repeatedly, the cumulative effect of modest testing efforts could result in more complete screening levels over time than might be assumed according to a single cross-sectional sample and motivate adoption of screening to the extent possible.
Goals of This Investigation
The HIV diagnostic testing and targeted screening program based in our ED provides testing during less than 2% of annual visits. The effect over time from this level of screening is unknown. The number of visits at which testing is offered does not relate directly to the proportion of the patient population tested because many patients make multiple visits. We hypothesized that among patients tested by our program, both the proportion of patients who report any previous HIV test and the proportion of all ED patients previously tested in our program increase over time.
METHODS
Study Design
This study is a secondary analysis of HIV testing data obtained from the electronic medical record of an HIV counseling and testing program and ED visit data obtained from the hospital administrative database. Use of these data for research purposes was approved by the institutional review board.
Setting
Data were obtained for patients visiting the ED of a Midwestern urban teaching hospital serving many disadvantaged and minority patients, with an annual ED census of more than 85,000. Of the 2.1 million individuals in the Metropolitan Statistical Area, the local county has a population of more than 800,000 that is approximately 25% black, 72% white, and 1.5% Hispanic.12 The ED census is 57% black, 39% white, and 0.5% Hispanic. Almost all patients are older than 18 years; an ED dedicated to the care of children is located several blocks away. Health department surveillance data for the county indicate that the regional prevalence of diagnosed HIV/AIDS is 229 per 100,000 individuals, or approximately 0.2%.13
The HIV counseling and testing program has been described elsewhere.14–16 Briefly, it is an adjunct clinical program of the ED, working closely with an academic HIV treatment center. Testing was performed with conventional HIV enzyme-linked immunosorbent assay, with a confirmatory Western blot. Trained counselors obtained consent and provided testing and comprehensive prevention counseling. When counselors were not available, the medical staff could still conduct testing through the program, with result notification by counselors at a later time. From 2003 through 2005, counselors were available 7 days a week, from 8 am to 12 pm. Beginning in 2006, counselors were scheduled 24 hours per day. Counselors targeted patients for screening according to review of triage notations or medical records. They also accepted referrals from ED staff for both diagnostic testing and screening and provided testing to patients who requested an HIV test. Patients who consented to testing underwent a detailed risk assessment in conjunction with prevention counseling and were asked whether they had ever been tested for HIV. Patients with known or self-reported HIV infection were excluded from testing. Recent testing was not an exclusion criterion, but counselors may have been less assertive about testing or even discouraged testing if the last test was less than 3 months before.
Outcome Measures
Primary outcome measures were the proportion of patients tested who reported a previous test, the proportion of patients tested who had a previous test within the program, and the cumulative proportion of ED patients tested in the program.
Data Analysis
Analyses performed were primarily descriptive. The proportion of patients tested in the program who had previous testing was calculated for each month as the number of tested patients with previous tests divided by the number of tests conducted within that month. The cumulative proportion of ED patients ever tested in the program was computed as the ratio of the cumulative sum of unique patients tested in the program to the cumulative sum of unique patients treated in the ED. The rate of change in the proportion of patients with previous testing was estimated with linear regression. Analyses were conducted with SPSS (version 17.0; SPSS, Inc., Chicago, IL).
RESULTS
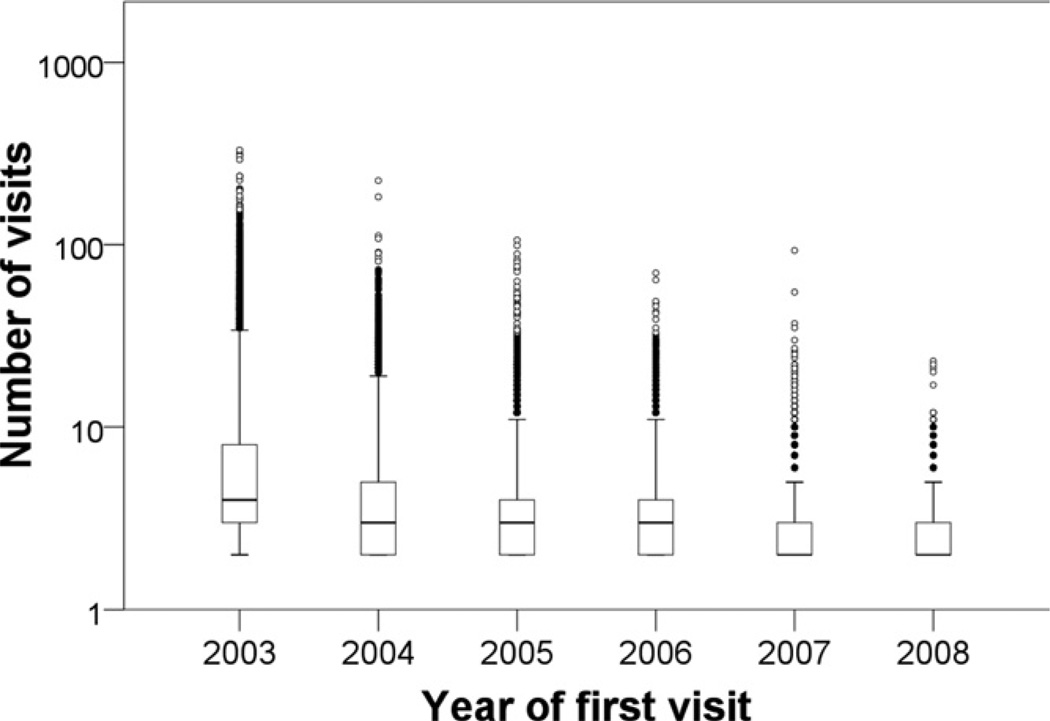
Between January 2003 and December 2008, there were 491,552 ED visits by patients aged 13 to 64 years, who were not known to have HIV infection at their visit. Of the 165,665 unique patients accounting for these visits, 90,508 presented only once during the study period and 75,157 patients (45.4%) presented up to 331 times (Figure 1). The number of patients who presented to the ED each month with no previous visit decreased from a mean of 3,820 per month in the first year of the study to a mean of 1,672 per month in the last year.
Figure 1.
Box-and-whisker plot showing the number of ED visits during the study period for the 75,157 patients with multiple visits. Data are grouped by the year of first presentation.
Overall, the testing program conducted 13,509 HIV tests for 11,503 unique patients, of which 115 of 13,509 (0.9%) test results were positive. The mean number of HIV tests conducted increased from 103 per month in 2003 to 322 per month in 2008. During the study period, 1,457 patients (12.6% of all tested patients) had 1 or more repeated tests within the program.
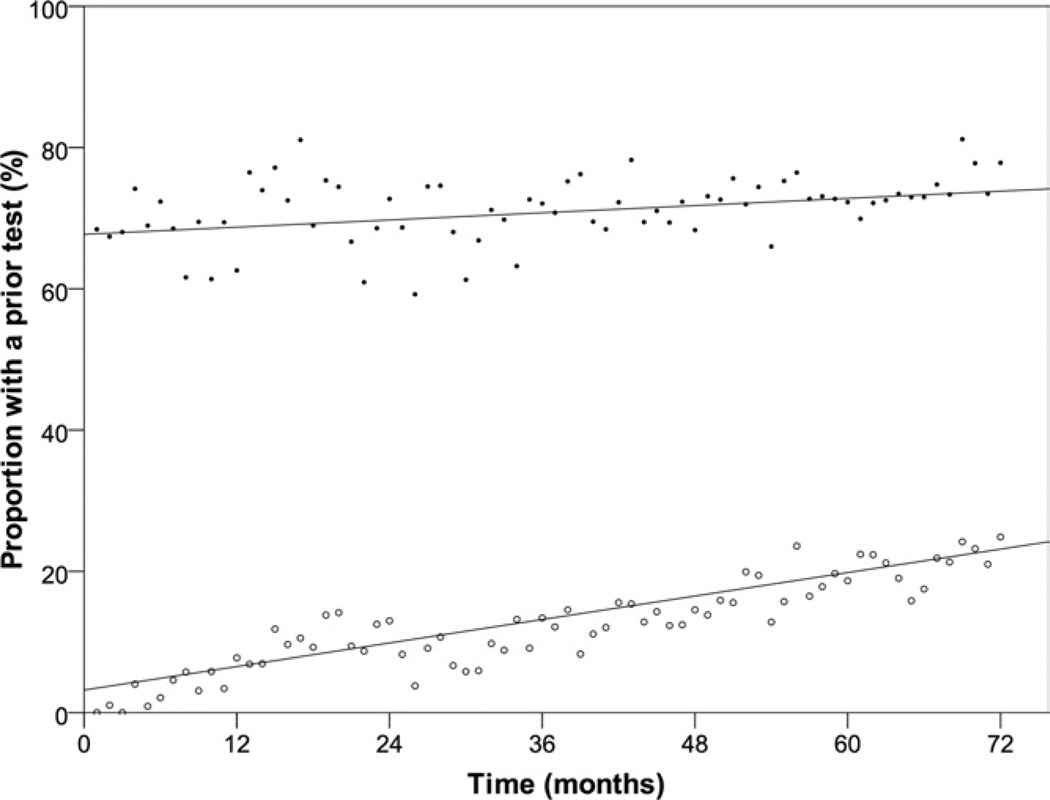
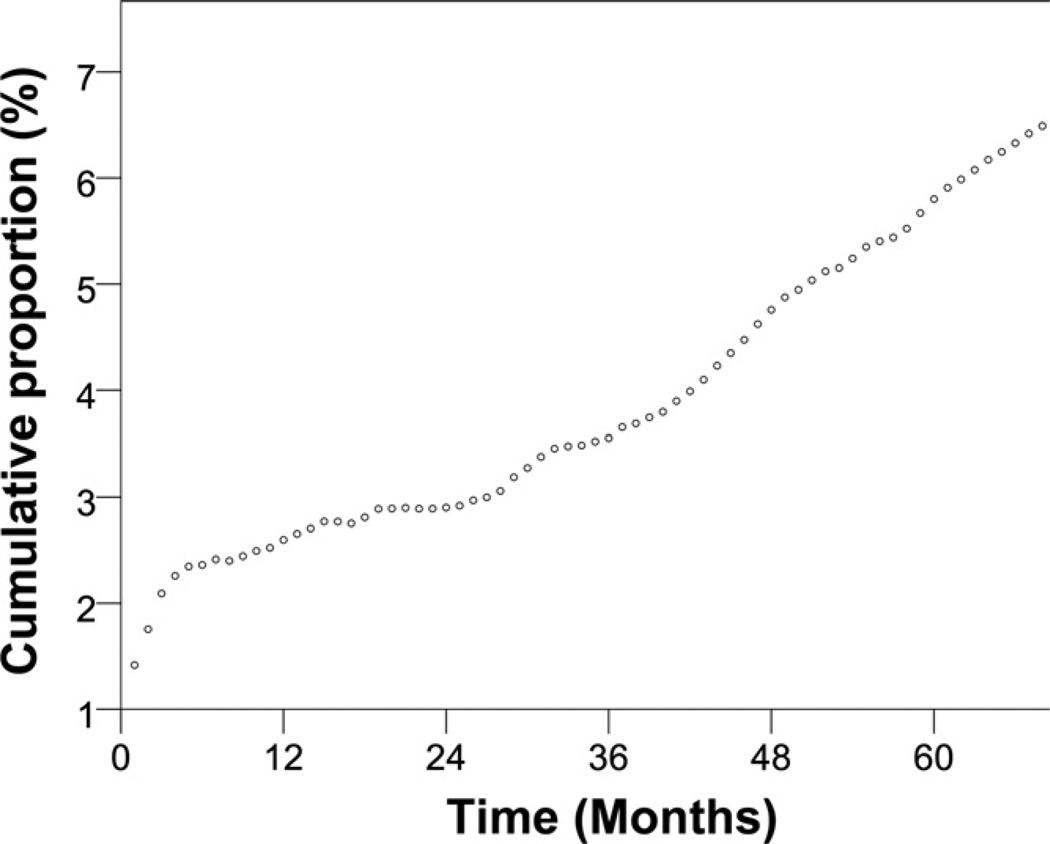
The proportion of tested patients with any previous test increased from 67.7% in 2003 to 74.4% in 2008 at a rate of 0.085% per month (95% confidence interval [CI] 0.037% to 0.133%), or about 1% per year (Figure 2). The proportion of ED patients known to have been tested in the program increased from 3.2% in 2003 to 21.2% in 2008 at a rate of 0.277% per month (95% CI 0.245% to 0.308%), or about 3.3% per year. By the end of the study period, 6.9% of all patients aged 13 to 64 years who were treated in the ED had received HIV testing within the program, an increase of 0.100% per month (95% CI 0.096% to 0.105%) (Figure 3).
Figure 2.
Proportion of HIV tests performed each month at which the patient either self-reported a previous test or had been previously tested by the program. Proportion of HIV tests performed each month at which the patient either self-reported a previous test (●) or was previously tested by the program (○).
Figure 3.
Cumulative proportion of ED patients aged 13 to 64 years with at least 1 HIV test conducted by the HIV testing program.
LIMITATIONS
The results of our study are subject to several limitations. Our numbers of ED patients were obtained from administrative data, and it is possible we were not able to fully exclude patients known to have HIV at their visit. Our HIV testing program collects information about patients in a prospective fashion, but it remains a clinical record without the usual rigor of a research study. Thus, it is possible that repeated visits or patient self-reports were incorrect. We believe this error is likely random, with minimal effect on study results. We also did not have testing history for ED patients who were not assessed in the testing program. We were able to estimate the number of ED patients within the age ranges recommended by the Centers for Disease Control and Prevention (CDC) for universal screening; however, we had no way to estimate the number of patients who might have met criteria for targeted screening or diagnostic testing. Therefore, the denominator used in our calculations to assess the overall cumulative effect includes individuals who might not be eligible for testing according to our current patient selection criteria.
Our findings might not be generalizable to other institutions. Our ED functions as the region’s primary provider of emergency care for indigent and minority patients. This patient population might be more static than that of community EDs. The frequency of previous testing might also differ significantly in other programs.
DISCUSSION
Our study demonstrates that ED screening programs can have important cumulative effects on the overall proportion of patients who have ever been tested for HIV, even when testing is provided during only a fraction of annual visits. This occurred because a sizeable proportion of patients visited the ED more than once, providing more than 1 opportunity to test those patients who had not been tested previously. For the years of this study, our program provided testing during only 2.6% of visits but tested 6.9% of patients aged 13 to 64 years. Studies of cumulative outcomes can be used to motivate translation and changes in health policy. Our finding of cumulative effect should further motivate EDs to engage in screening to whatever extent possible, even if those efforts are modest. Our results also further demonstrate the growing need to consider outcomes from epidemiologic studies in EDs using patients as a unit of analysis.
Until now, the extent of service provided by our program has been underestimated by our use of visits as the sole unit of analysis. Before our investigation, we observed only that the absolute number of HIV tests performed by our program each month was a fraction of the number of ED visits. We have recently explored the degree to which our program tested patients who reported no previous testing17 and the degree to which use of patients or visits as the unit of analysis affects our program-level statistics.18 The relationship between the number of ED patients and number of ED visits at our center was unknown. We hypothesized that our ED population is relatively static and that cumulatively, the proportion of the ED population screened by our program increases over time because, for many patients, there were serial opportunities for screening on repeated visits.
Increasing the proportion of people living in the United States who have ever been tested for HIV is a fundamental goal of public health HIV screening efforts. From 2002 through 2006, the number of individuals in the United States who reported having had an HIV test remained static, at approximately 40%,19 and even high-risk populations have not been screened to saturation.20,21 Our findings suggest that imperfect, yet feasible, approaches to HIV screening can contribute to the ultimate goal of population screening. This finding is of importance, given the cost-effectiveness of diagnosing disease in individuals unaware of HIV infection.22,23 However, enthusiasm for this approach should be tempered by at least 3 considerations. First, the metric “ever tested” does not account for the incidence of new infection acquired after a previous negative test result. If screening efforts are to achieve universal coverage over time, the incidence of new infection must remain below the rate of diagnosis. Second, even the limited number of tests provided by our program might not be feasible in many other centers. Finally, our screening of only 7% of eligible patients after 6 years might be judged insignificant relative to the public health crisis constituted by the HIV epidemic.
The optimal allocation of limited resources between screening patients for the first time and repeatedly screening those at high risk remains unknown. By the end of the study period, more than 20% of the patients being tested had been tested within the ED program previously. If the program had tested only patients who had never been tested before, the proportion of ED patients who had been screened over time might have been greater. However, the CDC recommends retesting high-risk patients, and we have previously found that, among patients reporting previously testing, 0.78% are HIV positive.17
CONCLUSION
Significant cumulative effects on the overall proportion of individuals who have ever been tested for HIV are possible, even for programs that provide testing during a relatively small number of ED visits. Documenting that population-level influence can be realized, whether or not universal screening is feasible, should further motivate EDs to engage in screening to whatever extent possible, even if those efforts are modest.
Acknowledgments
Funding and support: The clinical program described in this report was supported by the Ohio Department of Health and the Cincinnati Health Network. The research component was supported in part by National Institute of Allergy and Infectious Disease K23 AI068453.
Publication of this article was supported by Centers for Disease Control and Prevention, Atlanta, GA.
Footnotes
By Annals policy, all authors are required to disclose any and all commercial, financial, and other relationships in any way related to the subject of this article as per ICMJE conflict of interest guidelines (see www.icmje.org).
REFERENCES
- 1.Liddicoat RV, Horton NJ, Urban R, et al. Assessing missed opportunities for HIV testing in medical settings. J Gen Intern Med. 2004;19:349–356. doi: 10.1111/j.1525-1497.2004.21251.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Irvin CB, Flagel BT, Fox JM. The emergency department is not the ideal place for routine HIV testing. Ann Emerg Med. 2007;49:722. doi: 10.1016/j.annemergmed.2007.03.011. [DOI] [PubMed] [Google Scholar]
- 3.Rothman RE, Merchant RC. Commentary. Ann Emerg Med. 2007;49:577–579. doi: 10.1016/j.annemergmed.2007.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lyons MS, Lindsell CJ, Fichtenbaum CJ, et al. Interpreting and implementing the 2006 CDC recommendations for HIV testing in health-care settings. Public Health Rep. 2007;122:579–583. doi: 10.1177/003335490712200504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rotheram-Borus MJ, Klosinski LE, Etzel MA. Differences between proof-of-concept studies and effective implementation: routine, opt-out HIV testing in emergency departments. J Acquir Immune Defic Syndr. 2007;46:381–383. doi: 10.1097/QAI.0b013e3181582da9. [DOI] [PubMed] [Google Scholar]
- 6.Kelen GD. Public health initiatives in the emergency department: not so good for the public health? Acad Emerg Med. 2008;15:194–197. doi: 10.1111/j.1553-2712.2008.00068.x. [DOI] [PubMed] [Google Scholar]
- 7.McKenna M. HIV testing: should the emergency department take part? Ann Emerg Med. 2007;49:190–192. doi: 10.1016/j.annemergmed.2006.12.008. [DOI] [PubMed] [Google Scholar]
- 8.Brown J, Shesser R, Simon G, et al. Routine HIV screening in the emergency department using the new US Centers for Disease Control and Prevention guidelines. J Acquir Immune Defic Syndr. 2007;46:395–401. doi: 10.1097/qai.0b013e3181582d82. [DOI] [PubMed] [Google Scholar]
- 9.Haukoos JS, Hopkins E, Eliopoulos VT. Development and implementation of a model to improve identification of patients infected with HIV using diagnostic rapid testing in the emergency department. Acad Emerg Med. 2007;14:1149–1157. doi: 10.1197/j.aem.2007.07.015. [DOI] [PubMed] [Google Scholar]
- 10.Kelen GD, Rothman RE. Emergency department–based HIV testing: too little, but not too late. Ann Emerg Med. 2009;54:65–71. doi: 10.1016/j.annemergmed.2009.03.027. [DOI] [PubMed] [Google Scholar]
- 11.Lyss SB, Branson BM, Kroc KA, et al. Detecting unsuspected HIV infection with a rapid whole-blood HIV test in an urban emergency department. J Acquir Immune Defic Syndr. 2007;44:435–441. doi: 10.1097/QAI.0b013e31802f83d0. [DOI] [PubMed] [Google Scholar]
- 12.Kelen GD, Fritz S, Qaqish B, et al. Unrecognized human immunodeficiency virus infection in emergency department patients. N Engl J Med. 1988;318:1645–1650. doi: 10.1056/NEJM198806233182503. [DOI] [PubMed] [Google Scholar]
- 13.Ohio Department of Health Bureau of HIV/AIDS. HIV/AIDS statistics reporting by county in Ohio through December 31, 2005. [Accessed June 16, 2008]; Available at: http://www.odh.ohio.gov/healthStats/disease/hivann/hcty1.aspx. Updated April 22, 2010.
- 14.Lyons MS, Lindsell CJ, Hawkins DA, et al. Contributions to early HIV diagnosis among patients linked to care vary by testing venue. BMC Public Health. 2008;8:220. doi: 10.1186/1471-2458-8-220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lyons MS, Lindsell CJ, Ledyard HK, et al. Emergency department HIV testing and counseling: an ongoing experience in a low-prevalence area. Ann Emerg Med. 2005;46:22–28. doi: 10.1016/j.annemergmed.2004.12.022. [DOI] [PubMed] [Google Scholar]
- 16.Lyons MS, Lindsell CJ, Ledyard HK, et al. Health department collaboration with emergency departments as a model for public health programs among at-risk populations. Public Health Rep. 2005;120:259–264. doi: 10.1177/003335490512000307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lyons MS, Lindsell CJ, Ruffner AH, et al. Relationship of self-reported prior testing history to undiagnosed HIV positivity and HIV risk. Curr HIV Res. 2009;7:580–588. doi: 10.2174/157016209789973646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lyons MS, Raab DL, Ruffner AH, et al. Comparison of emergency department HIV testing data with visit or patient as the unit of analysis. J Med Screen. 2009;16:29–32. doi: 10.1258/jms.2009.008086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Duran D, Beltrami J, Stein R, et al. Persons tested for HIV. MMWR Morb Mortal Wkly Rep. 2008;57:845–849. [PubMed] [Google Scholar]
- 20.Centers for Disease Control and Prevention. Late HIV testing—34 states, 1996–2005. MMWR Morb Mortal Wkly Rep. 2009;58:661–665. [PubMed] [Google Scholar]
- 21.Centers for Disease Control and Prevention. HIV prevalence, unrecognized infection, and HIV testing among men who have sex with men—five US cities, June 2004–April 2005. MMWR Morb Mortal Wkly Rep. 2005;54:597–601. [PubMed] [Google Scholar]
- 22.Paltiel AD, Weinstein MC, Kimmel AD, et al. Expanded screening for HIV in the United States—an analysis of cost-effectiveness. N Engl J Med. 2005;352:586–595. doi: 10.1056/NEJMsa042088. [DOI] [PubMed] [Google Scholar]
- 23.Sanders GD, Bayoumi AM, Sundaram V, et al. Cost-effectiveness of screening for HIV in the era of highly active antiretroviral therapy. N Engl J Med. 2005;352:570–585. doi: 10.1056/NEJMsa042657. [DOI] [PubMed] [Google Scholar]