Abstract
Objective
The purpose of this study was to test a newly developed DXA method for abdominal fat depot quantification in subjects with AN, normal weight, and obesity using CT as a gold standard.
Design and Methods
135 premenopausal women (overweight/obese: n=89, normal-weight: n=27, AN: n=19); abdominal visceral adipose tissue (VAT), subcutaneous adipose tissue (SAT), and total adipose tissue (TAT) areas determined on CT and DXA.
Results
There were strong correlations between DXA and CT measurements of abdominal fat compartments in all groups with the strongest correlation coefficients in the normal-weight and overweight/obese groups. Correlations of DXA and CT VAT measurements were strongest in the obese group and weakest in the AN group. DXA abdominal fat depots were higher in all groups compared to CT, with the largest % mean difference in the AN group and smallest in the obese group.
Conclusions
A new DXA technique is able to assess abdominal fat compartments including VAT in premenopausal women across a large weight spectrum However, DXA measurements of abdominal fat were higher than CT, and this percent bias was most pronounced in the AN subjects and decreased with increasing weight, suggesting that this technique may be more useful in obese individuals.
Introduction
Visceral adiposity is a major risk factor for the development of the metabolic syndrome and is associated with insulin resistance, dyslipidemia, and a proinflammatory and prothrombotic state (1-3). In contrast, lower body obesity (subcutaneous adipose tissue stored in the gluteofemoral region) is associated with a lower risk of metabolic complications (4, 5). The increased cardiometabolic risk of visceral fat has been attributed in part to its higher expression of inflammatory cytokines and elevated portal vein free fatty acid (FFA) levels (6, 7). Given the increased cardiometabolic risk associated with visceral adiposity, it is important to accurately determine the amount of visceral fat to identify individuals at risk for cardiometabolic disease. Several methods exist for the assessment of body composition, with CT and MRI being considered the gold standard for detailed assessment of abdominal fat compartments (8, 9). However, cost, radiation exposure and availability make these methods impractical in the clinical setting or for large research studies. Dual energy X-ray absorptiometry (DXA) is a technique that can determine whole body and regional distribution of fat and lean mass (10-12). DXA is widely available, associated with only a minimal radiation dose, and relatively inexpensive. However, the ability of DXA to determine abdominal fat compartments is limited. A new DXA method for assessment of visceral adipose tissue (VAT) has recently been reported and was shown to perform as well as a clinical read of VAT from a CT scan (13). However, body composition extremes of obesity and anorexia nervosa (AN) may impact DXA accuracy. Subjects with AN have a paucity of abdominal fat which can alter the validity of DXA-derived estimates of abdominal fat, and we have previously shown an increasing bias of DXA in abdominal fat assessment with increasing weight (14). The purpose of this study was to test a newly developed DXA method for abdominal fat depot quantification in subjects across a weight spectrum ranging from obese to AN using CT as a gold standard.
Methods and Procedures
The study was approved by the Partners Healthcare Inc. Institutional Review Board and was Health Insurance Portability and Accountability Act compliant. Written informed consent was obtained from all subjects prior to the study.
Subjects
We studied a total of 135 premenopausal women. Of those, 89 were overweight or obese, 27 were of normal weight, and 19 had AN. Obese and normal weight subjects were recruited from the community through advertisements. AN subjects were referred by eating disorders care providers or recruited through advertisements. Inclusion criteria for all groups were: ages 18-45 years and female gender. Exclusion criteria included pregnancy, lactation and chronic disease, including diabetes mellitus. AN subjects fulfilled all psychiatric Diagnostic and Statistical Manual IV (DSM-IV) criteria for AN.
Overweight/obese subjects had a BMI of ≥ 25 kg/m2 and normal weight subjects had a BMI ≥ 19 and < 25 kg/m2. Clinical characteristics and CT data have been previously reported on a subset of the obese and normal weight subjects (14-20).
Anthropometry
Body weight was measured with a calibrated digital scale to the nearest 0.1 kg. Height was measured with a wall mounted stadiometer to the nearest 0.1cm in triplicate and averaged. Body mass index (BMI) was calculated as weight divided by height squared (kg/m2).
Dual-energy X-ray Absorptiometry
Whole body DXA measurements of body composition were performed in all patients using a Hologic Discovery A (Hologic Inc., Bedford, MA).
Analysis of DXA scans was performed as previously described (13). Briefly, DXA fat depots were measured in a 5 cm wide region placed across the abdomen just above the iliac crest at a level that approximately coincided with the 4th lumbar vertebrae, the region of abdominal fat depot measurements by CT. The software automatically locates the outer and inner margins of the abdominal wall on both sides of projected DXA image based on fat and lean mass profiles across the abdomen at the level of the fourth lumbar vertebra. The software then measures the total fat mass within the abdominal walls, i.e. the visceral region, a region which contains both subcutaneous and visceral fat. The amount of subcutaneous adipose tissue (SAT) above and below the visceral region is estimated by measuring the subcutaneous fat between the skin line and outer abdominal wall on both sides of the image, and this estimate is subtracted from the total abdominal fat mass (TAT) measured within the visceral region to yield DXA visceral adipose tissue (VAT) (21, 22).
Computed Tomography
Each subject underwent a single-slice CT scan of the abdomen at the level of the 4th lumbar vertebrae. Subjects were placed supine in the CT scanner and a lateral and frontal scout image was obtained to identify the level of L4, which served as landmarks for the single slice image. Scan parameters were standardized: 144 table height, 80kV, 70 mA, scan time 2 seconds, 1 cm slice thickness, 48 cm field of view.
Images were analyzed by a single trained analyst under the direction and supervision of an expert reader (MP). Quantification of abdominal fat depots was performed using image analysis software (SliceOmatic V4.2, TomoVision, Montreal, Quebec, Canada) as previously described (13). Briefly, thresholding methods were applied to identify adipose tissue, using a threshold set for −30 to −190 Hounsfield units (HU), then manual delineation, using tools provided by the software, was used to separate SAT, VAT, and intermuscular adipose tissue (IMAT). Pixels within the threshold that were not anatomically one of the two adipose tissue depots were removed. The total abdominal fat area was then calculated as the sum of abdominal SAT, VAT, and IMAT areas (cm2). The sum of VAT and IMAT was used to determine CT-VAT for comparison with DXA-VAT. The coefficient of variation for repeated measurements of the same scan on consecutive days by the same analyst is 1.7% for SAT, 2.3% for VAT, and 5.9% for IMAT(13) .
Statistical Analysis
Statistical analysis was performed using JMP (version 5.0.1a, SAS Institute, Cary, NC) and MedCalc (version 9.2.1.0, MedCalc, Mariakerke, Belgium) software. Variables were compared using the Student’s t-test. The Tukey-Kramer test was used to adjust for multiple comparisons. Correlation analysis between VAT, abdominal SAT and TAT determined by DXA and CT was performed in obese, normal weight, and AN subjects. Correlation analysis between BMI and abdominal fat compartments was also performed. In order to determine agreement between the two methods, VAT, abdominal SAT and TAT areas from CT and DXA were compared using Bland Altman analysis (23).
Results
Clinical characteristics and body composition of study subjects
Subject characteristics and body composition by CT and DXA of the three groups are shown in Table 1. Study participants ranged from 19 to 45 years, mean age: 32.4±7.7 years and in BMI from 15.6 to 47.5 kg/m2, mean BMI 29.4±7.9 kg/m2. AN subjects were younger and obese subjects were older compared to normal weight subjects. As expected, there was a significant difference in weight, BMI, and abdominal fat depots between the groups, with BMI, weight, and abdominal fat being the lowest in AN and the highest in the obese group.
Table 1.
Clinical characteristics and abdominal fat body composition of study subjects (values are means ± SD and range)
| AN (n=19) | Normal weight (n=27) |
Overweight/obese (n=89) |
|
|---|---|---|---|
| Age (years) | 24.8±3.6*,** (19.0 to 33.0) |
30.1±6.9 (19.0 to 45.0) |
34.8±7.4* (19.0 to 45.0) |
| Weight (kg) | 49.7±5.1*,** (40.3 to 60.2) |
61.4±7.7 (45.8 to 76.8) |
90.7±14.8* (62.7 to 128.8) |
| BMI (kg/m2) | 17.9±1.4*,** (15.6 to 20.3) |
22.0±2.0 (18.1 to 24.8) |
34.0±5.2* (25.1 to 47.5) |
| CT VAT (cm2) | 14.0±8.7** (2.7 to 36.3) |
31.8±17.3 (12.3 to 79.3) |
107.8±53.7* (16.9 to 247.6) |
| DXA VAT (cm2) | 20.9±11.2** (9.8 to 58.5) |
43.4±19.0 (18.6 to 88.6) |
128.2±47.4* (39.8 to 250.5) |
| CT SAT (cm2) | 76.9±37.6*,** (44.2 to 193.8) |
189.7±86.5 (72.5 to 474.6) |
447.3±135.6* (199.4 to 790.3) |
| DXA SAT (cm2) | 136.3±32.5*,** (102.3 to 231.3) |
265.7±83.4 (149.2 to 519.0) |
523.4±126.0* (276.2 to 828.6) |
| CT TAT (cm2) | 90.9±43.7*,** (47.1 to 230.1) |
221.5±94.3 (97.3 to 507.0) |
555.1±169.4* (240.5 to 980.0) |
| DXA TAT (cm2) | 157.2±41.8*,** (113.0 to 289.8) |
309.1±96.2 (176.3 to 585.2) |
651.6±157.4* (321.6 to 980.9) |
p<0.05, compared to normal weight group (BMI ≥ 19 and < 25 kg/m2)
p<0.05, compared to obese group (BMI ≥ 25 kg/m2)
p-values are adjusted for multiple comparisons using the Tukey-Kramer test
AN: anorexia nervosa
VAT: visceral adipose tissue
SAT: subcutaneous adipose tissue
TAT: total adipose tissue
Correlation between DXA and CT body composition parameters
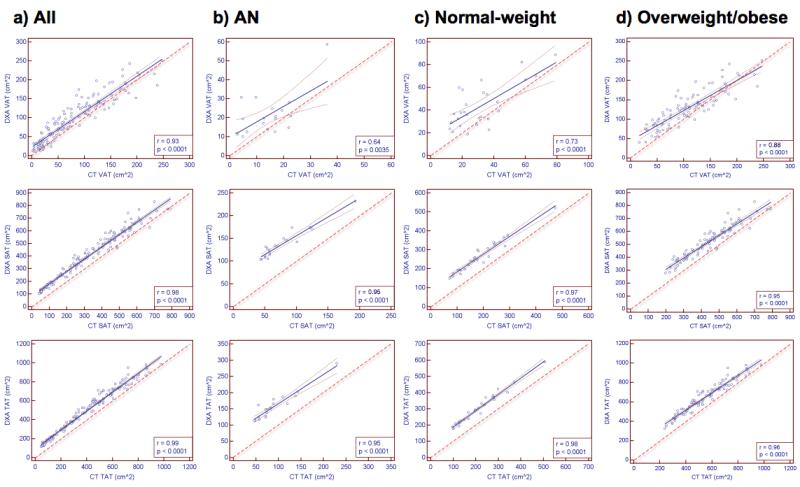
There were strong correlations between DXA and CT measurements of abdominal fat compartments in the group as a whole and in all three groups separately (Table 2). When evaluating AN, normal weight, and obese groups, the strongest correlation coefficients were found in the normal weight and obese groups (Figure 1). Correlations of DXA and CT VAT measurements were strongest in the obese group (Figure 1).
Table 2.
Regression analysis of abdominal fat compartments derived from CT and DXA
| All (n=135) | AN (n=19) | Normal weight (n=27) |
Overweight/obese (n=89) |
|
|---|---|---|---|---|
| VAT | r=0.93 (p<0.0001) RMSE: 22.2 cm2 95% CI: 0.90 to 0.95 |
r=0.64 (p=0.0035) RMSE: 6.9 cm2 95% CI: 0.25 to 0.85 |
r=0.73 (p<0.0001) RMSE: 12.0 cm2 95% CI: 0.49 to 0.87 |
r=0.88 (p<0.0001) RMSE: 26.0 cm2 95% CI: 0.82 to 0.92 |
| SAT | r=0.98 (p<0.0001) RMSE: 37.9 cm2 95% CI: 0.97 to 0.99 |
r=0.95 (p<0.0001) RMSE: 11.6 cm2 95% CI: 0.88 to 0.98 |
r=0.97 (p<0.0001) RMSE: 21.4 cm2 95% CI: 0.93 to 0.99 |
r=0.95 (p<0.0001) RMSE: 44.6 cm2 95% CI:0.92 to 0.96 |
| TAT | r=0.99 (p<0.0001) RMSE: 39.6 cm2 95% CI: 0.98 to 0.99 |
r=0.95 (p<0.0001) RMSE: 14.7 cm2 95% CI: 0.86 to 0.98 |
r=0.98 (p<0.0001) RMSE: 17.4 cm2 95% CI: 0.96 to 0.99 |
r=0.96 (p<0.0001) RMSE: 46.0 cm2 95% CI:0.94 to 0.98 |
AN: anorexia nervosa
VAT: visceral adipose tissue
SAT: subcutaneous adipose tissue
TAT: total adipose tissue
RMSE: root mean square error
CI: confidence interval
Figure 1.
Correlation analysis between CT and DXA measures of visceral adipose tissue (VAT), subcutaneous adipose tissue (SAT), and total adipose tissue (TAT) in all subjects (a), anorexia nervosa (AN) subjects (b), normal weight subjects (c), and overweight/obese subjects (d). Correlations were strongest in the normal weight and overweight/obese groups. Thin dashed lines indicate 95% confidence interval. Thick dashed line indicates line of identity.
There were strong correlations between BMI and DXA and CT measurements of abdominal fat depots in all subjects combined and the overweight/ obese group, whereas there were no associations between BMI and abdominal fat compartments in the AN group (Table 3).
Table 3.
Regression analysis of BMI and abdominal fat compartments derived from CT and DXA
| All (n=135) | AN (n=19) | Normal weight (n=27) |
Overweight/obese (n=89) |
|
|---|---|---|---|---|
| CT-VAT | r=0.80 (p<0.0001) | r= −0.04 (p=0.88) | r=0.27 (p=0.18) | r=0.60 (p<0.0001) |
| DXA-VAT | r=0.86 (p<0.0001) | r= 0.04 (p=0.86) | r=0.48 (p=0.01) | r=0.64 (p<0.0001) |
| CT-SAT | r=0.94 (p<0.0001) | r=0.27 (p=0.26) | r=0.65 (p=0.0002) | r=0.86 (p<0.0001) |
| DXA-SAT | r=0.94 (P<0.0001) | r=0.12 (p=0.60) | r=0.68 (p<0.0001) | r=0.85 (p<0.0001) |
| CT-TAT | r=0.99 (p<0.0001) | r=0.23 (p=0.35) | r=0.65 (p=0.0003) | r=0.88 (p<0.0001) |
| DXA-TAT | r=0.95 (p<0.0001) | r=0.10 (p=0.67) | r=0.69 (p<0.0001) | r=0.87 (p<0.0001) |
AN: anorexia nervosa
VAT: visceral adipose tissue
SAT: subcutaneous adipose tissue
TAT: total adipose tissue
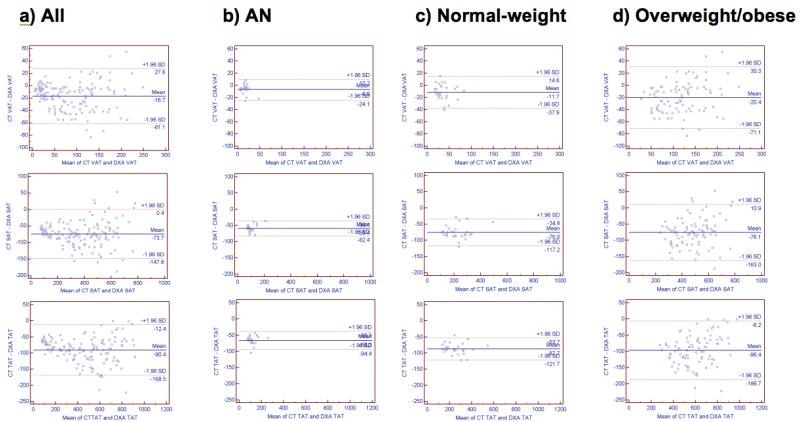
Agreement between DXA and CT body composition parameters
Agreement between DXA and CT measurements of abdominal fat depots are shown in Table 4 and Figure 2. DXA abdominal fat depots were higher in all three groups. The % mean difference between CT and DXA measurements of abdominal fat depots was largest in the AN group and smallest in the obese group. However, the mean difference in cm2 was largest in the obese group and smallest in the AN group due to larger fat areas in the obese group. Within the AN group, DXA overestimated VAT compared with CT by 46.8%, SAT by 60.9%, and TAT by 58.2%, while in the overweight/obese group DXA overestimated VAT by 23.5%, abdominal SAT by 17.4% and abdominal TAT by 17.7%. However, the mean difference in cm2 between DXA and CT was smallest in the AN group and became larger with increasing weight (Table 4). In the group as a whole, the %difference between CT and DXA measurements became smaller with increasing weight. This was also seen within groups, where there was decreased bias with increasing weight (Figure 2).
Table 4.
Agreement between abdominal fat compartments determined by DXA and CT using Bland Altman analysis. Values are expressed in % mean difference (95% confidence interval) and in absolute values (cm2) mean difference (95% confidence interval).
| All (n=135) | AN (n=19) | Normal weight (n=27) |
Overweight/obese (n=89) |
|
|---|---|---|---|---|
| VAT | −28.7 (−98.2 to 40.7) % −16.7 (−61.1 to 27.6) cm2 |
−46.8 (−153.6 to 60.1) % −6.9 (−24.1 to 10.2) cm2 |
−33.5 (−108.9 to 42.0) % −11.7 (−37.9 to 14.6) cm2 |
−23.5 (−77.5 to 30.6) % −20.4 (−71.1 to 30.3) cm2 |
| SAT | −27.7 (−68.3 to 13.0) % −73.7 (−147.8 to 0.4) cm2 |
−60.9 (−98.8 to −23.1) % −59.4 (−82.4 to −36.4) cm2 |
−37.9 (−69.4 to −6.3) % −76.0 (−117.2 to −34.8) cm2 |
−17.4 (−39.4 to 4.5) % −76.1 (−163.0 to 10.9) cm2 |
| TAT | −27.2 (−64.2 to 9.8) % −90.4 (−168.5 to −12.4) cm2 |
−58.2 (−95.4 to −20.9) % −66.3 (−94.4 to −38.3) cm2 |
−36.7 (−62.1 to −11.3) % −87.7 (−121.7 to −53.7) cm2 |
−17.7 (−36.8 to 1.3) % −96.4 (−186.7 to −6.2) cm2 |
AN: anorexia nervosa
VAT: visceral adipose tissue
SAT: subcutaneous adipose tissue
TAT: total adipose tissue
Figure 2.
Bland Altman analysis of CT and DXA derived visceral adipose tissue (VAT), subcutaneous adipose tissue (SAT), and total adipose tissue (TAT) in all subjects (a), anorexia nervosa (AN) subjects (b), normal weight subjects (c), and overweight/obese subjects (d). DXA overestimates VAT in all three groups compared to CT with the error becoming smaller with increasing weight. This trend is also visible within the groups.
Discussion
Our study showed that a new DXA technique based on changes in gray scale values and special modeling techniques is able to assess abdominal fat compartments including VAT in premenopausal women across a weight spectrum ranging from obese to AN, using CT as the gold standard. We found strong correlations between abdominal fat depots measured by CT and DXA. Our Bland-Altman agreement analyses showed that DXA abdominal fat depots were higher in all three groups compared with CT, and this bias was most pronounced in the AN subjects and decreased with increasing weight. Therefore, this technique may be a useful research or clinical technique, particularly for overweight and obese individuals, in whom body composition research is particularly important.
With the increased incidence of obesity and the increased awareness of eating disorders, simple and reliable methods for assessing body composition are needed. This is particularly true for overweight and obese populations. Visceral adiposity is a strong risk factor for cardiovascular disease, insulin resistance, and type 2 diabetes (3, 24). Visceral fat is morphologically and functionally distinct from subcutaneous fat in that cellularity and FFA turnover are higher per unit adipose tissue (25, 26). Also, venous output of visceral fat drains directly into the portal system of the liver, while FFA from subcutaneous fat enter the systemic circulation (6). In visceral obesity the delivery of FFA to the liver is increased contributing to hepatic fat accumulation (27), which is strongly associated with insulin resistance, type 2 diabetes, and hypertriglyceridemia (28). Therefore, simple, non-invasive methods to accurately determine VAT are important for detection of individuals at risk for cardiometabolic disease. CT and MRI are considered the gold standard to assess VAT and have been validated against cadavers (8, 9); however, these techniques are expensive, often not readily available, and CT involves radiation exposure. DXA is a technique that is widely available, requires only a minimal radiation dose, and is relatively inexpensive. In a prior study, we have shown strong correlations between VAT determined by CT and trunk fat determined by DXA, as a surrogate for VAT. However, in that study, DXA underestimated trunk fat – a bias that increased with increasing weight (14), suggesting that DXA trunk fat may not be used as a surrogate for VAT in subjects with obesity. A recent study has described a fully automated DXA method for quantification of VAT (29). In that study of men and women over a large age and BMI range, there were strong correlations between DXA and CT VAT, similar to our study. DXA overestimated VAT by an average of 56 cm3. In our study, the average difference between DXA and CT VAT in the entire cohort was much less, at 16.7 cm2.
Several studies have used manually defined subregions on whole body DXA images to estimate VAT (30-32). In these studies DXA did not perform better than waist circumference in estimating VAT. As DXA is a two-dimensional technique, defining subregions on DXA images integrates both VAT and SAT. Therefore, a more sophisticated technique was developed that uses changes in grey scale levels and specific modeling techniques to estimate abdominal SAT which can then be subtracted from abdominal TAT measured directly by DXA to yield VAT. This technique has been shown to perform as well as a clinical CT for VAT measurement in a large cohort of premenopausal women (13). However, this technique has not been tested in cohorts of women with AN and obesity, at the extremes of the weight and fat mass spectrum. Therefore, we studied a cohort of premenopausal women with AN, obesity and normal weight to test this new technique in these populations. Although there were strong correlations between CT and DXA measurements of all abdominal fat compartment in all groups, DXA abdominal fat depots were higher in all three groups compared to CT and this bias increased with decreasing weight by as much as 60.9% for SAT in the AN group. However, when measuring the mean difference in cm2, there was an increase in mean difference between the DXA and CT measurements with increasing weight. The smallest mean difference was found in the AN group, where the mean difference of VAT between CT and DXA was only −6.9cm2. This represented a -46.8% difference, as the mean VAT area in the AN group was 14.0±8.7cm2. Therefore, although the mean difference in absolute numbers was smallest in the AN group, caution should be used when interpreting these data as AN subjects have a paucity of abdominal fat and these small numbers represented a relatively large % mean difference. In addition, the RSME for VAT was largest in the AN group, especially below 40 cm2, which may limit the ability of DXA to monitor changes in VAT in this population. Although the mean difference in cm2 was larger in the obese group, the % mean difference decreased with increasing weight, which makes this technique more useful in the clinical or research setting, for estimation of cardiometabolic complications from VAT.
A potential reason for the discrepancy between DXA and CT measurements include partial volume errors on the CT, especially in the AN population with a paucity of visceral fat. In addition, although the region of interest on the DXA was chosen to correspond closely to the single slice CT, the DXA region of interest might have included a slightly different area than the single slice CT.
We found that DXA correlated strong with CT abdominal fat compartments and BMI in the group as a whole and the overweight/obese group. However, there were no associations between BMI and abdominal fat in the AN group and only moderately strong correlations in the normal-weight group. This confirms the inability of BMI to discriminate between different fat compartments.
Our study had several limitations. First, we only studied premenopausal women. There are sex and age related differences in DXA measurements, and studies in men, children or the elderly might yield different results. Second, we studied a smaller number of AN and normal weight women than obese women. Third, we used single slice CT for evaluating abdominal fat compartment, which may not correspond to the exact region used by the DXA technique. However, DXA analysis was performed in a region coinciding with abdominal CT. Fourth, CT might be an imperfect standard of reference and the accuracy of fat quantification has not been studied in AN and severely obese subjects. Fifth, we only used single-slice CT of the abdomen for estimation of abdominal fat compartments, not total abdominal fat. However, several studies have shown strong correlations between single-slice and whole body abdominal fat compartments (33, 34).
In conclusion, a new DXA technique is able to determine abdominal fat depots including VAT in premenopausal women with obesity and AN. It should be noted that the percent mean difference between CT and DXA decreased with increasing weight, which is important as obese women are at highest risk for cardiometabolic complications associated with VAT. Our data suggest that DXA can be used to assess body composition in individuals of different weights but may be less accurate when used in extremely low-weight premenopausal women -- and more accurate in overweight and obese women, in whom body composition assessment and research are important, given the established link between visceral adiposity and cardiovascular risk.
What is already known about this subject?
Dual energy X-ray absorptiometry (DXA) is a widely available and relatively inexpensive technique that can determine whole body and regional distribution of fat and lean mass using only a minimal radiation dose.
Visceral adipose tissue (VAT) is a major risk factor for the development of the metabolic syndrome and cardiovascular disease.
A new DXA method for assessment of VAT has recently been reported and was shown to perform as well as a clinical read of VAT from a CT scan .
What does this study add?
This study tests the new DXA method for quantification of abdominal fat in subjects with anorexia nervosa (AN) and obesity.
The new DXA method can be used to quantify abdominal fat depots in women ranging from AN to morbidly obese.
The new DXA method is more useful in quantifying abdominal fat depots in overweight/obese women than in subjects with AN.
Acknowledgments
This work was supported in part by the following grants: R01 HL-077674, UL1 RR025758, R01 MH083657 and K23 RR-23090
Footnotes
Disclosures TLK and KEW are employees of Hologic Inc, the DXA manufacturer used in this study and own stock in the company. After unblinding the data, all authors had access to all results and analyses. The other authors declared no conflict of interest.
References
- 1.Despres JP, Lemieux I. Abdominal obesity and metabolic syndrome. Nature. 2006;444:881–887. doi: 10.1038/nature05488. [DOI] [PubMed] [Google Scholar]
- 2.Grundy SM. Obesity, metabolic syndrome, and coronary atherosclerosis. Circulation. 2002;105:2696–2698. doi: 10.1161/01.cir.0000020650.86137.84. [DOI] [PubMed] [Google Scholar]
- 3.Rexrode KM, Carey VJ, Hennekens CH, et al. Abdominal adiposity and coronary heart disease in women. Jama. 1998;280:1843–1848. doi: 10.1001/jama.280.21.1843. [DOI] [PubMed] [Google Scholar]
- 4.Snijder MB, Henry RM, Visser M, et al. Regional body composition as a determinant of arterial stiffness in the elderly: The Hoorn Study. J Hypertens. 2004;22:2339–2347. doi: 10.1097/00004872-200412000-00016. [DOI] [PubMed] [Google Scholar]
- 5.Snijder MB, Visser M, Dekker JM, et al. Low subcutaneous thigh fat is a risk factor for unfavourable glucose and lipid levels, independently of high abdominal fat. The Health ABC Study. Diabetologia. 2005;48:301–308. doi: 10.1007/s00125-004-1637-7. [DOI] [PubMed] [Google Scholar]
- 6.Bjorntorp P. “Portal” adipose tissue as a generator of risk factors for cardiovascular disease and diabetes. Arteriosclerosis. 1990;10:493–496. [PubMed] [Google Scholar]
- 7.Poulain-Godefroy O, Lecoeur C, Pattou F, Fruhbeck G, Froguel P. Inflammation is associated with a decrease of lipogenic factors in omental fat in women. Am J Physiol Regul Integr Comp Physiol. 2008;295:R1–7. doi: 10.1152/ajpregu.00926.2007. [DOI] [PubMed] [Google Scholar]
- 8.Abate N, Burns D, Peshock RM, Garg A, Grundy SM. Estimation of adipose tissue mass by magnetic resonance imaging: validation against dissection in human cadavers. J Lipid Res. 1994;35:1490–1496. [PubMed] [Google Scholar]
- 9.Rossner S, Bo WJ, Hiltbrandt E, et al. Adipose tissue determinations in cadavers--a comparison between cross-sectional planimetry and computed tomography. Int J Obes. 1990;14:893–902. [PubMed] [Google Scholar]
- 10.Fuller NJ, Hardingham CR, Graves M, et al. Assessment of limb muscle and adipose tissue by dual-energy X-ray absorptiometry using magnetic resonance imaging for comparison. International Journal of Obesity and Related Metabolic Disorders: Journal of the International Association for the Study of Obesity. 1999;23:1295–1302. doi: 10.1038/sj.ijo.0801070. [DOI] [PubMed] [Google Scholar]
- 11.Glickman SG, Marn CS, Supiano MA, Dengel DR. Validity and reliability of dual-energy X-ray absorptiometry for the assessment of abdominal adiposity. Journal of Applied Physiology (Bethesda, Md.: 1985) 2004;97:509–514. doi: 10.1152/japplphysiol.01234.2003. [DOI] [PubMed] [Google Scholar]
- 12.Levine JA, Abboud L, Barry M, Reed JE, Sheedy PF, Jensen MD. Measuring leg muscle and fat mass in humans: comparison of CT and dual-energy X-ray absorptiometry. Journal of Applied Physiology (Bethesda, Md.: 1985) 2000;88:452–456. doi: 10.1152/jappl.2000.88.2.452. [DOI] [PubMed] [Google Scholar]
- 13.Micklesfield LK, Goedecke JH, Punyanitya M, Wilson KE, Kelly TL. Dual-energy X-ray performs as well as clinical computed tomography for the measurement of visceral fat. Obesity (Silver Spring) 2012;20:1109–1114. doi: 10.1038/oby.2011.367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bredella MA, Ghomi RH, Thomas BJ, et al. Comparison of DXA and CT in the assessment of body composition in premenopausal women with obesity and anorexia nervosa. Obesity (Silver Spring) 2010;18:2227–2233. doi: 10.1038/oby.2010.5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bredella MA, Ghomi RH, Thomas BJ, Miller KK, Torriani M. Comparison of 3.0 T proton magnetic resonance spectroscopy short and long echo-time measures of intramyocellular lipids in obese and normal-weight women. J Magn Reson Imaging. 2010;32:388–393. doi: 10.1002/jmri.22226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bredella MA, Ghomi RH, Thomas BJ, et al. Breath-hold 1H-magnetic resonance spectroscopy for intrahepatic lipid quantification at 3 Tesla. J Comput Assist Tomogr. 2010;34:372–376. doi: 10.1097/RCT.0b013e3181cefb89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bredella MA, Lin E, Brick DJ, et al. Effects of GH in women with abdominal adiposity: a 6-month randomized, double-blind, placebo-controlled trial. Eur J Endocrinol. 2012;166:601–611. doi: 10.1530/EJE-11-1068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bredella MA, Torriani M, Ghomi RH, et al. Adiponectin is inversely associated with intramyocellular and intrahepatic lipids in obese premenopausal women. Obesity (Silver Spring) 2011;19:911–916. doi: 10.1038/oby.2010.296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bredella MA, Torriani M, Ghomi RH, et al. Vertebral bone marrow fat is positively associated with visceral fat and inversely associated with IGF-1 in obese women. Obesity (Silver Spring) 2011;19:49–53. doi: 10.1038/oby.2010.106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bredella MA, Utz AL, Torriani M, Thomas B, Schoenfeld DA, Miller KK. Anthropometry, CT, and DXA as predictors of GH deficiency in premenopausal women: ROC curve analysis. J Appl Physiol. 2009;106:418–422. doi: 10.1152/japplphysiol.90998.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kelly T, Wilson K, Ruth C. Hologic I, editor. Estimating visceral fat by dual-energy X-ray absorptiometry. 2010.
- 22.Kelly T, Wilson K, Ruth C. Holigic I, editor. Visceral fat measurement. 2011.
- 23.Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet. 1986;1:307–310. [PubMed] [Google Scholar]
- 24.Zhang C, Rexrode KM, van Dam RM, Li TY, Hu FB. Abdominal obesity and the risk of all-cause, cardiovascular, and cancer mortality: sixteen years of follow-up in US women. Circulation. 2008;117:1658–1667. doi: 10.1161/CIRCULATIONAHA.107.739714. [DOI] [PubMed] [Google Scholar]
- 25.Jensen MD, Johnson CM. Contribution of leg and splanchnic free fatty acid (FFA) kinetics to postabsorptive FFA flux in men and women. Metabolism. 1996;45:662–666. doi: 10.1016/s0026-0495(96)90040-2. [DOI] [PubMed] [Google Scholar]
- 26.Tchkonia T, Giorgadze N, Pirtskhalava T, et al. Fat depot origin affects adipogenesis in primary cultured and cloned human preadipocytes. Am J Physiol Regul Integr Comp Physiol. 2002;282:R1286–1296. doi: 10.1152/ajpregu.00653.2001. [DOI] [PubMed] [Google Scholar]
- 27.Goto T, Onuma T, Takebe K, Kral JG. The influence of fatty liver on insulin clearance and insulin resistance in non-diabetic Japanese subjects. Int J Obes Relat Metab Disord. 1995;19:841–845. [PubMed] [Google Scholar]
- 28.Yu AS, Keeffe EB. Nonalcoholic fatty liver disease. Rev Gastroenterol Disord. 2002;2:11–19. [PubMed] [Google Scholar]
- 29.Kaul S, Rothney MP, Peters DM, et al. Dual-energy X-ray absorptiometry for quantification of visceral fat. Obesity (Silver Spring) 2012;20:1313–1318. doi: 10.1038/oby.2011.393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Gradmark AM, Rydh A, Renstrom F, et al. Computed tomography-based validation of abdominal adiposity measurements from ultrasonography, dual-energy X-ray absorptiometry and anthropometry. Br J Nutr. 2010;104:582–588. doi: 10.1017/S0007114510000796. [DOI] [PubMed] [Google Scholar]
- 31.Lee K, Lee S, Kim YJ, Kim YJ. Waist circumference, dual-energy X-ray absortiometrically measured abdominal adiposity, and computed tomographically derived intra-abdominal fat area on detecting metabolic risk factors in obese women. Nutrition. 2008;24:625–631. doi: 10.1016/j.nut.2008.03.004. [DOI] [PubMed] [Google Scholar]
- 32.Micklesfield LK, Evans J, Norris SA, et al. Dual-energy X-ray absorptiometry and anthropometric estimates of visceral fat in Black and White South African Women. Obesity (Silver Spring) 2010;18:619–624. doi: 10.1038/oby.2009.292. [DOI] [PubMed] [Google Scholar]
- 33.Irlbeck T, Massaro JM, Bamberg F, O’Donnell CJ, Hoffmann U, Fox CS. Association between single-slice measurements of visceral and abdominal subcutaneous adipose tissue with volumetric measurements: the Framingham Heart Study. Int J Obes (Lond) 2010;34:781–787. doi: 10.1038/ijo.2009.279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Siegel MJ, Hildebolt CF, Bae KT, Hong C, White NH. Total and intraabdominal fat distribution in preadolescents and adolescents: measurement with MR imaging. Radiology. 2007;242:846–856. doi: 10.1148/radiol.2423060111. [DOI] [PubMed] [Google Scholar]