Abstract
Objective
To determine whether a brief individual motivational interview (IMI) plus a family motivational interview (Family Check-Up [FCU]) would reduce alcohol use in adolescents treated in an emergency department after an alcohol-related event more effectively than would an IMI only.
Design
Two-group randomized design with 3 follow-up time points.
Setting
An urban regional level I trauma center.
Participants
Adolescents aged 13 to 17 years (N=125) with a positive blood alcohol concentration as tested using blood, breath, or saliva.
Interventions
Either IMI or IMI plus FCU.
Main Outcome Measures
Drinking frequency (days per month), quantity (drinks per occasion), and frequency of high-volume drinking (≥5 drinks per occasion).
Results
Both conditions resulted in a reduction in all drinking outcomes at all follow-up points (P < .001 for all), with the strongest effects at 3 and 6 months. Adding the FCU to the IMI resulted in a somewhat better outcome than did the IMI only on high-volume drinking days at 3-month follow-up (14.6% vs 32.1%, P =.048; odds ratio, 2.76; 95% confidence interval, 0.99–7.75).
Conclusions
Motivational interventions have a positive effect on drinking outcomes in the short term after an alcohol-related emergency department visit. Adding the FCU to an IMI resulted in somewhat better effects on high-volume drinking at short-term follow-up than did an IMI only. The cost of extra sessions necessary to complete the FCU should be weighed against the potential benefit of reducing high-volume drinking when considering adding the FCU to an IMI for this population.
Primary health care settings have been the site of several efforts to reduce substance use among at-risk adolescent patients.1,2 Studies have also targeted alcohol-abusing teenagers who present to the emergency department (ED), reasoning that the salience of an alcohol-related event may increase the adolescent’s sense of vulnerability and, thereby, increase receptivity to an intervention by capitalizing on a teachable moment. Indeed, 1 study3 found that an individual motivational interview (IMI),4 which uses a nonconfrontational empathic therapeutic style, offers personalized feedback, and develops a discrepancy between current drinking behavior and current and long-term goals, to be effective in reducing alcohol-related problems in 18- to 19-year-old adolescents. Another study5 of 13- to 17-year-olds found a greater reduction in average number of drinking days per month and frequency of high-volume drinking in adolescents who reported a history of problematic alcohol use at baseline if they received an IMI compared with standard care.
One potential weakness of an IMI for adolescents is that it does not address the role of the parent(s) in managing adolescents’ substance use. The Family Check-Up (FCU)6 is an assessment and feedback intervention, consistent with a motivational approach, designed to enhance parental recognition of child/adolescent risk behaviors and increase motivation for reducing these problem behaviors and associated risk factors. The intervention targets specific family risk and protective factors linked to alcohol and other drug use, including parental supervision, monitoring, and parent-child relationship quality. In 1 study,7 an FCU conducted with sixth graders was found to have a protective effect on subsequent alcohol use in ninth grade, with parental monitoring found to be the mechanism of efficacy.
The purpose of this study was to conduct a 2-group, parallel, randomized design trial to test the hypothesis that the addition of the FCU to an IMI would result in significantly better adolescent alcohol use outcomes at 3-, 6-, and 12-month follow-up compared with an IMI only for adolescents treated in the ED after an alcohol-related incident.
METHODS
BASELINE RECRUITMENT
Between January 1, 2003, and January 31, 2008, 13- to 17-year-old patients treated at an urban level I trauma center in the Northeast United States were eligible for this 5-year National Institutes of Health–funded study if they had a positive blood alcohol concentration as tested using blood, breath, or saliva or self-reported drinking of alcohol in the 6 hours before the ED visit. Alcohol-positive patients who were suicidal (n=17), did not speak English or Spanish as their primary language (n=4), or had experienced serious traumatic injury (n=21) were not approached to participate. Of 239 alcohol-positive eligible patients and families, 110 (46.0%) agreed to participate; of 25 who self-reported alcohol use, 15 (60.0%) agreed to participate, resulting in a total sample of 125 participants. The most common reasons for refusing to participate included discharge from the ED before completion of recruitment, lack of interest, being too tired, or being in too much pain.
PROCEDURE
Interventionists with master’s degrees in counseling and psychology conducted all aspects of the baseline contact, including obtaining written informed consent from the parents and assent from the adolescents, administering the assessment, and conducting the intervention. The consent/assent procedure included assurances that parents would not be informed of any of the adolescent’s responses. Patients were then randomly assigned to the IMI or the IMI + FCU condition by the interventionists based on condition assignments contained in sealed envelopes. Patients in both conditions received the IMI first. Adolescents were not approached until their blood alcohol concentration was below 0.1%, and they had to pass a mental status examination and be able to describe the essential elements of the study to assent to participation. All procedures were approved by the Brown University and Rhode Island Hospital institutional review boards. Owing to high blood alcohol concentrations and time of night in the ED, most patients in both conditions were scheduled to return to the hospital within a few days to complete their interventions.
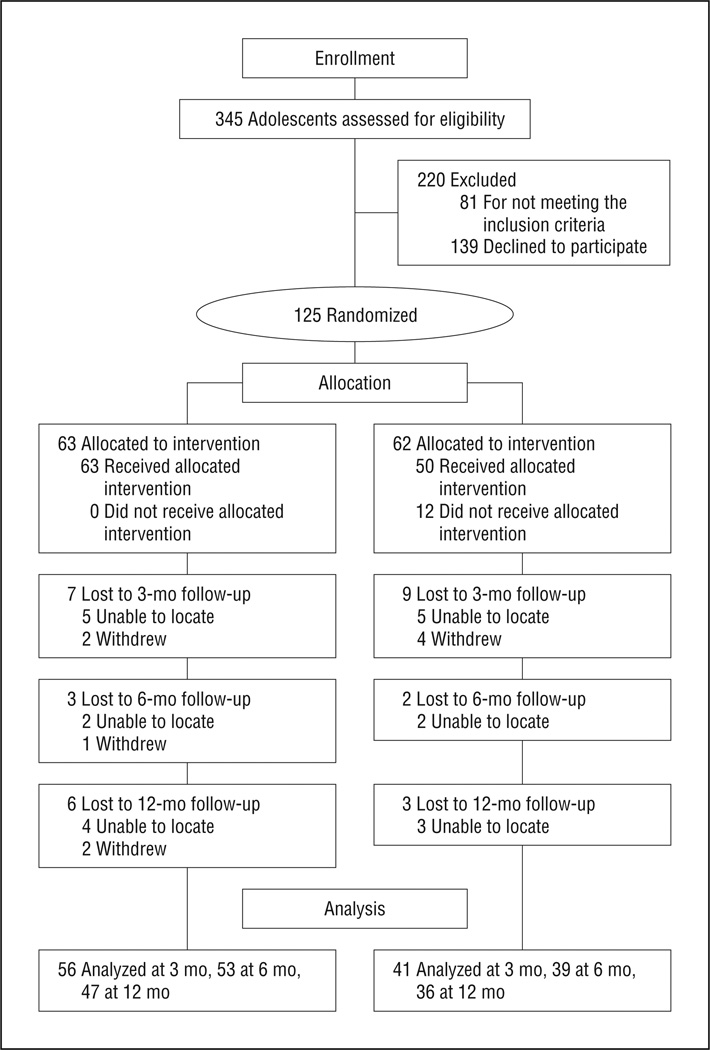
The IMI, identical in both groups, was completed in 45 to 60 minutes before randomization. On completion of the IMI, adolescents were given a $20 gift certificate, and parents were compensated $50 on completion of the FCU. Families in the IMI + FCU condition then returned for a 1-hour videorecorded assessment session (described in the “The FCU” subsection), and parents received feedback in a second 1-hour session. Parents in both conditions were given follow-up information regarding substance use treatment services and received 5 monthly booster brochures on parenting before the 6-month follow-up visit. Follow-up interviews were conducted at 3 months by telephone and at 6 and 12 months in person by research assistants who were masked to treatment group assignment (Figure 1).
Figure 1.
Consolidated Standards of Reporting Trials (CONSORT) flow diagram.
THE IMI
The IMI was an approximately 45-minute counseling session that included an emphasis on personal responsibility, exploration of motivation for drinking and review of potential negative consequences, personalized normative assessment feedback, establishing goals regarding drinking, and anticipating barriers to accomplishing goals, such as peer pressure to drink. In addition to being empathic and avoiding argumentation, the interventionists made an effort to develop a discrepancy between the adolescent’s current drinking and longer-term goals and to support the adolescent’s sense of self-efficacy.4 Independent raters coded the sessions. Fidelity to the intervention protocol and competency in delivering the intervention were rated by independent coders and averaged 83% for fidelity and ranged from 83.0% to 97.0% for competence (available on request from the authors).
THE FCU
Families in the IMI + FCU condition returned for a 1-hour videotaped family assessment task (FAsTask6), which consists of the parent(s) and the adolescent discussing family beliefs regarding alcohol, marijuana, cigarette, and other drug use and other topics, such as curfew. All FAsTask videos were coded separately by the treatment provider and a second rater to provide information to be used in the feedback session. A week after the family completed the FAsTask, parents received feedback derived from the FAsTask and from self-report measures that assessed family stress, parent substance use, and beliefs regarding substance use.6 There were 4 specific phases of feedback: self-assessment, support and clarification, feedback, and development of a plan for change. Parent motivation for change, change options, and specific steps for making positive changes in family relationships and parenting were discussed, including potential barriers to change. Fidelity to the components of the FCU ranged from 79% to 100%. Competency scores were all acceptable, with ratings ranging from 75% to 100% (available on request from the authors).
PRIMARY OUTCOME MEASURES
At baseline, families were asked to report on adolescent behavior and parenting. Only results on alcohol measures are reported herein, which were collected using the Adolescent Drinking Questionnaire.8 This questionnaire is scored on an 8-point scale and taps into drinking frequency (days per month), quantity (drinks per occasion), frequency of high-volume drinking (≥5 drinks per occasion), and frequency of intoxication (feeling “drunk” or “very, very high”) in the previous 3 months.
STATISTICAL ANALYSES
The 2 intervention groups were compared for equivalency using t tests and χ2 analyses of baseline variables. Follow-up completion was investigated by group using χ2 tests. A series of dependent t tests were used to examine whether there were significant changes from baseline to the 3-, 6-, and 12-month follow-up points in continuous alcohol scores. The generalized estimating equations (GEE) method9 was then used for dichotomous variables to examine whether alcohol use changed during follow-up and differed at follow-up based on treatment condition. The respective continuous baseline values were covaried in the GEE analyses. The GEE provides an extension of regression analyses to repeated or correlated data, allows inclusion of participants with some missing data, and is flexible in its ability to handle a range of distributions. A Poisson model was used to examine differences in count data, that is, quantity per drinking occasion. χ2 Analyses were used to examine intervention effects on dichotomous outcomes at each follow-up time point separately.
RESULTS
PRELIMINARY ANALYSES
Table 1 indicates that there was little difference between groups in demographic or substance use variables at baseline. The Adolescent Drinking Questionnaire item “high-volume (≥5 drinks) drinking days” was highly correlated with the item “drunk” (r = 0.67, P < .001). Consequently, “drunk” data are not reported herein, leaving 3 conceptually distinct alcohol variables reported: drinking frequency, drinking quantity, and high-volume drinking frequency. There were no differences between groups on any alcohol measures at baseline.
Table 1.
Demographic Information Across Intervention Conditionsa
| Variable | IMI Only (n=63) |
IMI + FCU (n=62) |
|---|---|---|
| Sex, No. (%) | ||
| Male | 30 (47.6) | 28 (45.2) |
| Female | 33 (52.4) | 34 (54.8) |
| Race, No. (%) | ||
| Non-Hispanic white | 45 (71.4) | 38 (61.3) |
| Black | 1 (1.6) | 1 (1.6) |
| Asian American/East Indian | 0 | 3 (4.8) |
| Hispanic | 17 (27.0) | 17 (27.4) |
| Mixed race | 0 | 3 (4.8) |
| Reason for ED visit, No. (%) | ||
| Intoxication with injury or medical concern | 18 (28.6) | 14 (22.6) |
| Intoxication only | 45 (71.4) | 48 (77.4) |
| Age, mean (SD), y | 15.48 (1.24) | 15.42 (1.16) |
Abbreviations: ED, emergency department; FCU, Family Check-Up; IMI, individual motivational interview.
Percentages may not total 100 because of rounding.
The IMI session was completed by 100% of the adolescents in both treatment conditions. The IMI + FCU condition entailed 2 additional family sessions, and 50 of the 62 families (79.4%) completed the assessment and the FCU feedback sessions (P <.001). Of the families that completed the IMI session, 85.7% completed the 3-month, 81.4% completed the 6-month, and 72.6% completed the 12-month follow-ups. One patient in the sample died in a house fire. There were no significant differences in follow-up rates between conditions.
ALCOHOL USE OUTCOMES
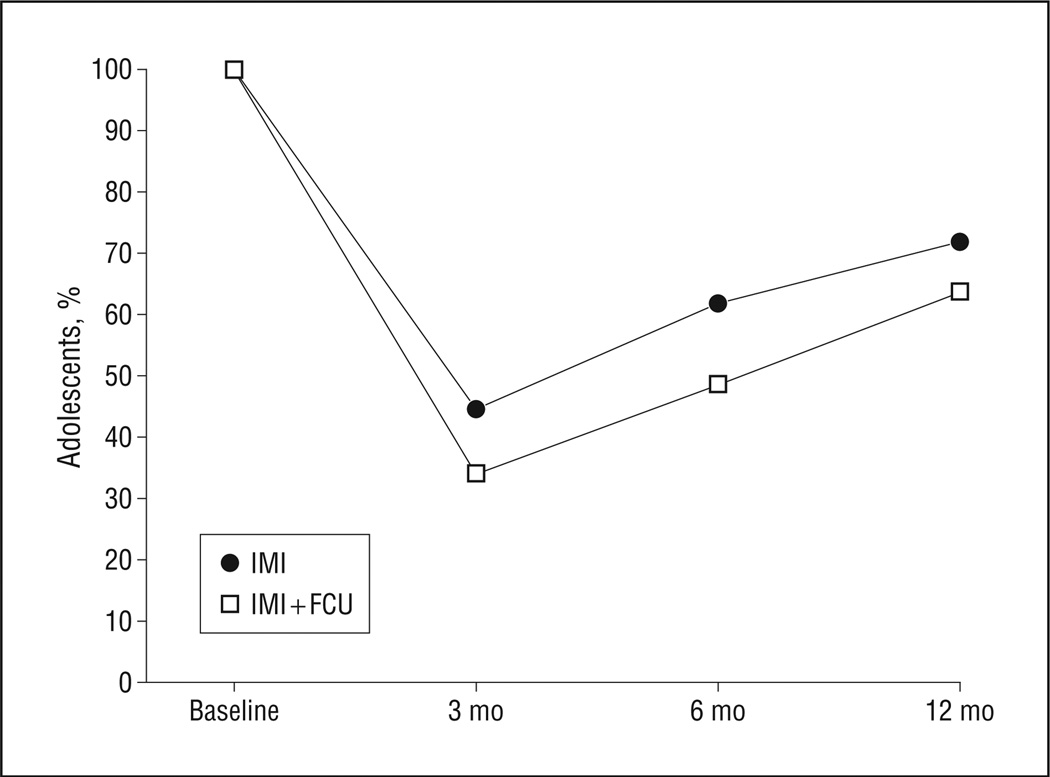
For the sample as a whole, the pattern for the variable “any drinking in the previous month” indicated a decrease from 100% at baseline to 39.3% at 3 months; however, this value rose to 55.2% at 6 months and to 67.9% at 12 months (Figure 2). Table 2 provides the mean values of all the alcohol use variables at baseline and at the 3 follow-up points. A series of t tests indicated that for the sample as a whole, although number of drinking days rose from 3 to 12 months, the average number of drinking days per month at each follow-up point was significantly lower than at baseline: baseline to 3 months, t96 = 6.82; baseline to 6 months, t91 = 6.09; and baseline to 12 months, t82 = 4.18 (P < .001 for all).
Figure 2.
Percentage of the sample that reported any drinking in the previous 3 months by condition. FCU indicates Family Check-Up; IMI, individual motivational interview.
Table 2.
Alcohol Use Variables at All Time Points for the IMI and IMI + FCU Conditions
| Follow-up |
|||||||||
|---|---|---|---|---|---|---|---|---|---|
| Baseline |
3 mo |
6 mo |
12 mo |
||||||
| ADQ Variable | Group | Mean (SD) | No. | Mean (SD) | No. | Mean (SD) | No. | Mean (SD) | No. |
| Frequency, d/moa | IMI | 3.4 (1.6) | 63 | 2.2 (1.7) | 56 | 2.4 (1.8) | 53 | 2.5 (1.7) | 47 |
| IMI + FCU | 3.4 (1.7) | 62 | 1.8 (1.5) | 41 | 2.1 (1.5) | 39 | 2.6 (2.1) | 36 | |
| Total sample | 3.4 (1.6) | 125 | 2.1 (1.6) | 97 | 2.3 (1.7) | 92 | 2.6 (1.9) | 83 | |
| Quantity, per occasiona | IMI | 5.2 (1.6) | 63 | 2.7 (2.3) | 56 | 3.0 (2.3) | 53 | 3.4 (2.4) | 47 |
| IMI + FCU | 5.4 (1.8) | 62 | 2.1 (1.9) | 41 | 2.4 (2.0) | 39 | 3.1 (2.5) | 36 | |
| Total sample | 5.3 (1.8) | 125 | 2.5 (2.2) | 97 | 2.7 (2.2) | 92 | 3.3 (2.4) | 83 | |
| High-volume drinking, d/moa | IMI | 2.7 (1.5) | 63 | 1.9 (1.6) | 56 | 2.0 (1.7) | 53 | 2.0 (1.4) | 47 |
| IMI + FCU | 2.5 (1.6) | 62 | 1.6 (1.6) | 41 | 1.7 (1.6) | 39 | 2.4 (2.1) | 36 | |
| Total sample | 2.6 (1.5) | 125 | 1.8 (1.6) | 97 | 1.9 (1.7) | 92 | 2.1 (1.7) | 83 | |
Abbreviations: ADQ, Adolescent Drinking Questionnaire; FCU, Family Check-Up; IMI, individual motivational interview.
Alcohol use was lower at all 3 follow-up points than at baseline but did not differ by group.
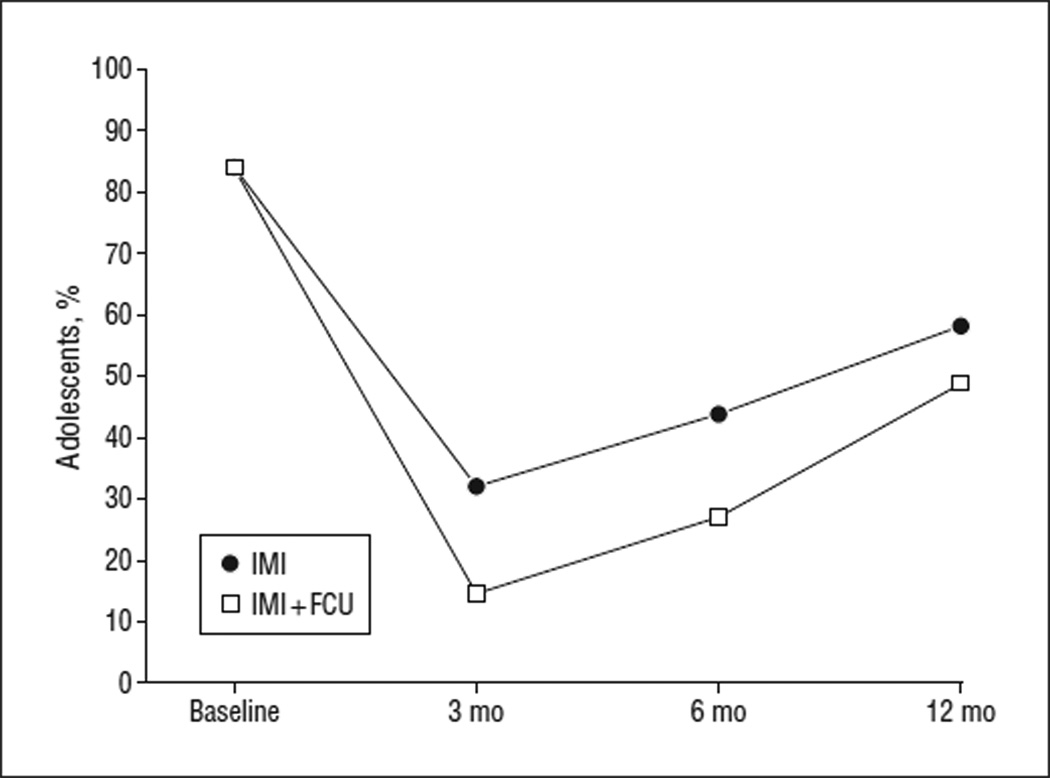
Table 3 displays the percentages of the sample by condition that reported having engaged in high-volume drinking. The GEE analyses indicated an odds ratio (OR) of 1.37 (95% confidence interval [CI], 0.91–2.07) for any drinking by time, ie, from 3 to 12 months. The OR for treatment condition was 1.61 (95% CI, 0.72–3.63). The OR for the treatment condition × time interaction was 1.14 (95% CI, 0.60–2.15) (Figure 3).
Table 3.
Adolescents Who Reported High-Volume Alcohol Use at Each Follow-up Point by Condition, With ORs and 95% CIsa
| Adolescents, No. % |
||||||
|---|---|---|---|---|---|---|
| 3 mo |
6 mo Cumulative |
12 mo Cumulative |
||||
| Condition | Yes | No | Yes | No | Yes | No |
| IMI + FCU | 6 (14.6) | 35 (85.4) | 10 (27.0) | 27 (73.0) | 17 (48.6) | 18 (51.4) |
| IMI | 18 (32.1) | 38 (67.9) | 24 (43.6) | 31 (56.4) | 29 (58.0) | 21 (42.0) |
Abbreviations: CI, confidence interval; FCU, Family Check-Up; IMI, individual motivational interview; OR, odds ratio.
At 3 months; OR, 2.76 (95% CI, 0.99–7.75); 6 months; 2.09 (0.85–5.14); and 12 months; 1.46 (0.61–3.49).
Figure 3.
Percentage of the sample who reported any high-volume drinking (≥5 drinks) in the previous 3 months by condition. FCU indicates Family Check-Up; IMI, individual motivational interview.
A series of t tests conducted with the entire sample indicated that quantity per drinking occasion decreased significantly from baseline to the 3-month (t96 = 9.74), 6-month (t91 = 8.44), and 12-month (t82 = 6.75) follow-up points (P < .001 for all) (see Table 2 for means and standard deviations at each point). Poisson analyses indicated that the OR for quantity per drinking occasion for time from 3 to 12 months was 0.94 (95% CI, 0.87–1.02). Poisson analyses also indicated an OR of 1.10 (95% CI, 0.95–1.27) by treatment condition and an OR of 0.99 (0.88–1.11) for the treatment condition × time interaction.
The occurrence of high-volume drinking days for the entire sample dropped from 84.0% at baseline to 24.0% at 3-month follow-up and then gradually increased to 35.3% at 6 months and 53.3% at 12 months. A series of t tests with the entire sample indicated that the number of high-volume drinking days decreased significantly from baseline to the 3-month (t96 = 6.81), 6-month (t91 = 6.21), and 12-month (t82 = 4.48) follow-up points (P < .001 for all) (see Table 2 for means and standard deviations). The GEE analysis of high-volume drinking revealed an OR of 1.39 (95% CI, 0.90–2.13) for time from 3 to 12 months. For treatment condition, the OR was 2.66 (95% CI, 0.99–7.17); the average likelihood of high-volume drinking across follow-up was 30.1% for the IMI + FCU condition and 44.6% for the IMI condition. The condition × time interaction OR was 1.51 (95% CI, 0.73–3.11) (Figure 2).
SUPPLEMENTARY ANALYSES
Because the OR for treatment condition in the GEE analyses of high-volume drinking was close to 1.00, we also examined high-volume drinking at each follow-up point (Figure 3 and Table 3). There was 1 statistically significant finding, consistent with the GEE analyses, for treatment condition on high-volume drinking days at 3 months. The IMI + FCU group reported a lower prevalence of high-volume drinking (14.6%; 95% CI, 3.8%–25.5%) compared with the IMI group (32.1%; 95% CI, 19.9%–44.4%) at the 3-month follow-up (, P = .048).A similar pattern was found for high-volume drinking at 6 months favoring the IMI + FCU group (27.0%; 95% CI, 12.7%–41.3%) over the IMI group (43.6%; 30.5%–56.8%) (, P=.10). The difference at 12 months was not statistically significant.
COMMENT
The results of this study indicate that for adolescents treated in an ED after an alcohol-related event, an IMI and an IMI plus a family MI resulted in a statistically and clinically significant decrease in alcohol use, quantity of use per drinking occasion, and high-volume drinking at each follow-up point compared with baseline. The largest effects were at 3-month follow-up, with a gradual increase by 6 months and then a sharper increase between 6 and 12 months. The positive effects of both of these brief interventions are consistent with the recent review of the literature10 that found that brief interventions are among the most effective treatments for adolescent alcohol abuse. Because this study did not have a standard care condition, we cannot comment on whether the same pattern of results might have occurred with regular care only in the ED. However, a previous study5 found that an IMI did convey an added advantage above and beyond standard care for adolescents with a history of problematic drinking before their alcohol-related incident. The trends across time indicated that motivational interventions have their greatest effect in the short term, with some effects extending to the 6-month time frame after an alcohol-related ED visit. This finding suggests that booster sessions might be useful in enhancing the effects of both interventions.
When the differences between treatment conditions across the entire follow-up period (3–12 months) were examined, the ORs did not indicate a statistically significant advantage for outcomes by adding the FCU. However, the pattern of results (Figures 2 and 3) raises the possibility that the results might have reached statistical significance if the sample size were larger. Indeed, when each follow-up point was examined individually, the significance level for high-volume drinking reached P = .048 at the 3-month follow-up point (and the lower bound of the CI was close to 1.00, ie, 0.99), suggesting that the addition of the FCU to the IMI may have resulted in a lower percentage of adolescents reporting 5 or more drinks per drinking occasion compared with the IMI condition. There were no effects on number of drinking days or quantity per drinking occasion. This finding fits with a harm reduction model that places an emphasis on lowering negative consequences of drinking rather than abstinence, which is consistent with the MI model.5 Interpretation of the present results is qualified by the fact that our power to detect differences was limited owing to the sample size. We also had fairly wide CIs in the ORs, which may also be a reflection of the small sample size. In addition, the self-report data were not corroborated by a parent or a peer. However, there is no reason to believe that any inaccurate reporting differed as a function of treatment condition. Generalization of these findings is limited to ED samples, and conclusions are also limited by the refusal rate. In this regard, it is important to note that these adolescents were not participating in an alcohol treatment program when we approached them. Indeed, recruitment was different from that of typical treatment outcome studies in that patients were not seeking treatment and, thus, were not necessarily motivated to undergo alcohol treatment. The consenting and baseline assessment procedures made this research protocol much more difficult to conduct than if this intervention were provided as standard practice. Finally, return visits to complete the FCU sessions proved problematic for approximately 20% of the families in this study. This dropout rate may have affected the findings. One way to improve the rate at which parents take part in the intervention might be to conduct future research studies in pediatric practices.
In conclusion, the recent policy statement by the American Academy of Pediatrics11 regarding alcohol use by youth and adolescents notes the need for more research regarding brief interventions. The results reported herein, when combined with previous findings,5 suggest that brief motivational interventions, whether of the individual or individual plus parent type, have the potential for a clinically meaningful short-term effect on high-volume drinking in adolescents. Adolescents who present to the ED with an alcohol-related event might be screened and then asked to complete an IMI in the ED. The assessment battery could be pared down to just a few key measures to provide feedback for the IMI once adolescents are sober and are ready for discharge from the ED. Alternatively, they could be asked to return for an IMI. The results of this study and a previous study5 also suggest that booster sessions at 3 and 6 months would be important to see whether they help sustain the initial positive effects on high-volume drinking.
The addition of the family component is more challenging logistically for these non–treatment-seeking families. The FCU could be recommended as a follow-up to the individual intervention in the ED for selected adolescents, especially those with preexisting alcohol problems, knowing that a portion of those families referred may not follow through with this referral. Physicians must weigh the pros of the family intervention’s likelihood of lowering the rate of such high-risk drinking behavior in the short term, that is, 3 to 6 months, vs the cons of the burden to families of the additional visits to complete the FCU. The potential for harm to befall adolescents engaged in high-volume drinking may make the added burden of additional visits worthwhile.
Acknowledgments
Funding/Support: This study was supported by grant AA013385 from the National Institute on Alcohol Abuse and Alcoholism.
Role of the Sponsor: The study sponsor (the National Institutes of Health) had no role in (1) the study design; (2) the collection, analysis, and interpretation of data; (3) the writing of the report; and (4) the decision to submit the paper for publication.
Footnotes
Author Contributions: Dr Spirito had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. Study concept and design: Spirito, Sindelar-Manning, Colby, Barnett, Lewander, Rohsenow, and Monti. Acquisition of data: Spirito, Sindelar-Manning, and Lewander. Analysis and interpretation of data: Spirito, Colby, and Monti. Drafting of the manuscript: Spirito and Lewander. Critical revision of the manuscript for important intellectual content: Spirito, Sindelar-Manning, Colby, Barnett, Rohsenow, and Monti. Statistical analysis: Colby and Rohsenow. Obtained funding: Spirito, Colby, Barnett, Lewander, Rohsenow, and Monti. Administrative, technical, and material support: Spirito, Colby, Barnett, Lewander, and Monti. Study supervision: Spirito, Sindelar-Manning, and Lewander.
Financial Disclosure: None reported.
Additional Information: Dr Spirito was the principal investigator for this study and Drs Colby, Barnett, Lewander, Rohsenow, and Monti were the coinvestigators.
Additional Contributions: Thomas Dishion, PhD, provided consultation on this study and Cheryl Eaton, MA, assisted in data analyses. We thank the interventionists and the research staff.
REFERENCES
- 1.D’Amico EJ, Miles JN, Stern SA, Meredith LS. Brief motivational interviewing for teens at risk of substance use consequences: a randomized pilot study in a primary care clinic. J Subst Abuse Treat. 2008;35(1):53–61. doi: 10.1016/j.jsat.2007.08.008. [DOI] [PubMed] [Google Scholar]
- 2.Knight JR, Sherritt L, Van Hook S, Gates EC, Levy S, Chang G. Motivational interviewing for adolescent substance use: a pilot study. J Adolesc Health. 2005;37(2):167–169. doi: 10.1016/j.jadohealth.2004.08.020. [DOI] [PubMed] [Google Scholar]
- 3.Monti PM, Colby SM, Barnett NP, et al. Brief intervention for harm reduction with alcohol-positive older adolescents in a hospital emergency department. J Consult Clin Psychol. 1999;67(6):989–994. doi: 10.1037//0022-006x.67.6.989. [DOI] [PubMed] [Google Scholar]
- 4.Miller WR, Rollnick S. Motivational Interviewing: Preparing People to Change Addictive Behavior. New York, NY: Guilford Press; 2001. [Google Scholar]
- 5.Spirito A, Monti PM, Barnett NP, et al. A randomized clinical trial of a brief motivational intervention for alcohol-positive adolescents treated in an emergency department. J Pediatr. 2004;145(3):396–402. doi: 10.1016/j.jpeds.2004.04.057. [DOI] [PubMed] [Google Scholar]
- 6.Dishion TJ, Kavanagh K. Intervening in Adolescent Problem Behavior: A Family-Centered Approach. New York, NY: Guilford Press; 2003. [Google Scholar]
- 7.Dishion TJ, Nelson SE, Kavanagh K. The Family Check-Up with high-risk young adolescents: preventing early-onset substance use by parent monitoring. Behav Ther. 2003;34(4):553–571. [Google Scholar]
- 8.Jessor R, Donovan JE, Costa FM. Health Behavior Questionnaire. Boulder: University of Colorado; 1989. [Google Scholar]
- 9.Liang K-Y, Zeger S. Longitudinal data analysis using generalized linear models. Biometrika. 1986;73(1):13–22. [Google Scholar]
- 10.Tripodi SJ, Bender K, Litschge C, Vaughn MG. Interventions for reducing adolescent alcohol abuse: a meta-analytic review. Arch Pediatr Adolesc Med. 2010;164(1):85–91. doi: 10.1001/archpediatrics.2009.235. [DOI] [PubMed] [Google Scholar]
- 11.Kokotailo PK. Committee on Substance Abuse. Alcohol use by youth and adolescents: a pediatric concern. Pediatrics. 2010;125(5):1078–1087. doi: 10.1542/peds.2010-0438. [DOI] [PubMed] [Google Scholar]