Abstract
Regular physical activity is important for promoting health and well-being; however, physical activity behaviors in children with autism spectrum disorders (ASD) have received little attention. We compared physical activity levels among 53 children with ASD and 58 typically developing children ages 3–11 years who participated in the Children's Activity and Meal Patterns Study (CHAMPS). After adjustment for age and sex the amount of time spent daily in moderate and vigorous activity (MVPA) was similar in children with ASD (50.0 minutes/day, and typically developing children 57.1 minutes/day). However, parents reported that children with ASD participated in significantly fewer types of physical activities than did typically developing children (6.9vs.9.6, p < .001) and spent less time annually participating in these activities compared to typically developing children (158 vs. 225 hr/yr, p < 0.0001) after adjusting for age and sex. Although both groups of children engaged in similar levels of moderate and vigorous activity (MVPA) as measured by accelerometry, children with ASD engaged in fewer physical activities and for less time according to parental report, suggesting that some of the activity in children with ASD is not captured by standard questionnaire-based measures.
Keywords: accelerometry, children, physical activity, autism spectrum disorders
Introduction
Previous studies of children have shown that moderate and vigorous physical activity (MVPA) improves both physiological and psychological health (Janssen and Leblanc, 2010; Schmalz et al., 2007). The Centers for Disease Control and Prevention (CDC, 2011) recommends that children engage in 60 minutes of MVPA each day. A recent national study suggested that less than half of children ages 6–11 years meet these recommendations (Troiano et al., 2008). Parents and clinicians frequently report that the social, physical, cognitive, and behavioral limitations that children with autism spectrum disorder (ASD) experience often prevent them from participating in team sports and other physical activities. For example, in a sub-sample of the population-based Special Needs and Autism Project (SNAP), 79% of children with autism exhibited movement impairments (Green et al., 2009). In the 2003 National Survey of Children's Health children with ASD were less likely to participate in sports (41% vs. 27%, p < 0.005) or extracurricular activities (45% vs. 34%, p < 0.05) compared to children with other developmental disabilities (Blanchard et al., 2006).
The extant literature on physical activity levels in children with ASD is sparse; most studies are limited by small sample sizes (Rosser Sandt and Frey, 2005), lack of a comparison group (Pan and Frey, 2005, 2006; Venkatesan, 2005), or have focused on a particular part of the day only (Pan, 2008).
Because children with ASD often have impairments in movement, communication, social skills, and behavior, we hypothesized that they would spend less time engaged in physical activities and would have lower physical activity levels than typically developing (TD) children. We also hypothesized that less physically active TD children as well as less active children with ASD would have a higher BMI z-score.
Methods
The Children's Activity and Meal Patterns Study (CHAMPS) was a cross-sectional study conducted in 2007–2008 that included children with ASD and TD children ages 3–11 years. Participants were recruited via outreach to local schools and community recreation programs, existing participant databases at the UMMS-Shriver Center, autism support organizations and networks, public listings on the Internet, and the assistance of the Interactive Autism Network (IAN) Project at the Kennedy Krieger Institute, Baltimore, MD. Inclusion criteria required that the child be in good health and free from diseases or disorders that could affect dietary and/or physical activity habits (e.g., diabetes, cystic fibrosis, chronic gastrointestinal illness, cerebral palsy, etc.). In addition, we excluded participants taking medications known to impact appetite, such as steroids, atypical antipsychotics, mood stabilizers, tricyclic antidepressants, anticonvulsants, and stimulants. The study was approved by the Institutional Review Board at the University of Massachusetts Medical School. Parents were compensated for their participation, and children were given a gift certificate to a book store.
The diagnosis of ASD was verified via the Autism Diagnostic Interview-Revised (ADI-R) (Rutter et al., 2003), which was administered to the parents of children who had indicated their child had ASD. The Vineland Adaptive Behavior Scales (Sparrow et al., 2005) was used to characterize adaptive skills, and we used the Differential Abilities Scale (Elliott, 1990) to assess the cognitive abilities of the children with ASD.
All children were weighed and measured in light clothing without shoes using a Seca™ portable scale and wall-mounted stadiometer. Body mass index (BMI) was calculated from measures of height and weight (kg/m2) and referenced against the sex- and age-specific CDC childhood growth reference (Kuczmarski et al., 2002). Overweight was defined as a BMI-for-age at or above the 85th percentile respectively, and underweight was defined as a BMI-for-age at or below the 5th percentile, as recommended by the CDC (Division of Nutrition, Physical Activity, and Obesity, 2011).
Assessment of Physical Activity
Accelerometry
Physical activity level was measured with the Actical® accelerometer. The Actical® utilizes a “piezoelectric accelerometer,” or motion sensor, that integrates the degree and intensity of motion and produces a voltage output signal whose magnitude is recorded as activity counts. Counts were recorded over 30-second epochs. The device is fastened via Velcro closures to an elastic belt that the child wears around his/her waist over either the left or right hip. Parents were provided a calendar which indicated the days on which they should have their child wear the accelerometer. Parents were instructed to assist their child to put on the accelerometer upon awakening in the morning and to remove it at night just before bed. They were asked to have the child wear the accelerometer on five weekdays and two weekend days. Wearing the device for seven consecutive days was encouraged, but due to holidays and individual considerations (forgetting to put it on, device malfunction, family vacation, etc.) this could not always be accomplished. Parents were given a daily activity log on which they were asked to indicate the times the accelerometer was put on and removed, and to indicate if there was anything unusual about the day (e.g., the child was sick, missed school, or did not wear the device for substantial parts of the day). At the end of the monitoring period parents were asked to return the device by mail in a pre-paid envelope.
Activity counts via accelerometry were used to estimate minutes and percentage of total time spent in light, moderate, and vigorous activity based on cut-off points established by Puyau et al. (Puyau et al., 2004). Cut-off points for light, moderate, and vigorous activity were 100–1499, 1500–6499 and ≥ 6500 counts per minute, respectively. To be included in our accelerometry analyses, children had to meet the following criteria for at least three weekdays and one weekend day: 1) the accelerometer was worn for a minimum of 600 minutes per day; 2) the day had to be considered to be a “typical” weekday or weekend day, meaning that no illness was reported and the child attended school on weekdays (if they were in school at the time); and 3) there was no report that the child removed the device for extended periods of time. If a child had more than the minimum of three weekdays and one weekend day of useable data, we included all their useable days in our analyses. We evaluated moderate and vigorous activity separately and as a composite variable.
We examined activity counts, minutes of participation in MVPA per day, the percentage of the day spent in light, moderate, and vigorous activity for both weekdays and weekend days, and total daily activity. We computed total daily activity from a weighted average of weekday and weekend activity data [(5*weekday average + 2* weekend average)/7] expressed as time and as percentage time spent in light, moderate, and vigorous activity.
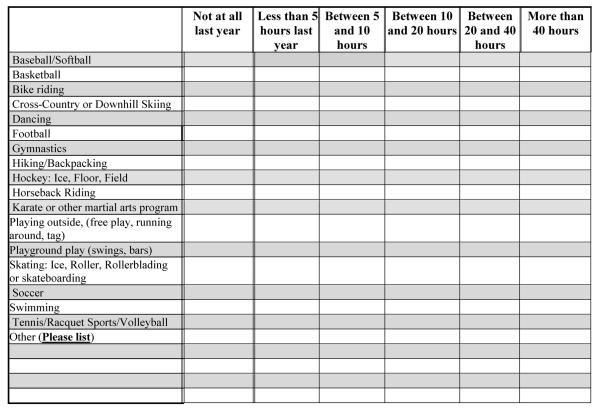
To determine the child's participation in organized and unstructured physical activities, parents completed a questionnaire developed by our research team. The questionnaire contained a checklist (see Figure 1) that asked parents to indicate the types and frequency of physical activities their children engaged in over the prior 12 months (17 activities total, including playground play, baseball/softball, swimming, etc.). The checklist included six possible response categories: 1) not at all; 2) less than 5 hours per year; 3) between 5 and 10 hours per year; 4) between 10 and 20 hours per year; 5) between 20 and 40 hours per year; and 6) over 40 hours per year. Parents were also given the opportunity to write in physical activities their child participated in that were not on the questionnaire. We aggregated activity time by using the midpoint for each frequency category to calculate the annual hours for all physical activities on the checklist and summing across all activities. We used 40 hours per year for the highest category. In addition, we asked parents to report how many days over the past 7 days they and their spouse/partner participated in activity of at least 20 minutes duration that made them breathe hard and/or sweat. The question was adapted from items used in the National Survey of Children's Health (Centers for Disease Control [CDC], National Center for Health Statistics [NCHS], State and Local Telephone Survey, 2003) and the National Health and Nutrition Examination Surveys (CDC, NCHS, 2003–2004). We repeated the questionnaires within 10–30 days with 44 parents (13 parents of children with ASD and 31 parents of TD children). The estimates for hours of physical activity on the two questionnaires were highly correlated (Pearson r= 0.98 ASD, 0.93 TD) as were the number of activities (Pearson r= 0.78 ASD, 0.90 TD). Furthermore, the mean error did not differ between the two groups for either measure before or after adjustment for age and sex.
Figure 1.
Physical Activity Checklist
Statistical Analyses
All analyses were conducted in SAS Version 9.2 (SAS Institute, Cary, NC), with the alpha level set at .05. Using t-tests for continuous variables and chi-square or Fisher exact tests for categorical variables, we determined whether TD children and children with ASD differed relative to the following covariates: age, sex, race (white, non-white), parental education (earned a college degree or not), parent reported activity (days per week), siblings (0 vs. ≥ 1), and child weight status (underweight, normal weight, or overweight).
Children who did not meet criteria for wearing the accelerometer were dropped from all analyses using accelerometry but were included in the analyses of physical activity participation. We conducted a series of linear regression analyses for physical activity outcome variables based on accelerometry and derived from questionnaires. Covariates that differed for children with ASD and TD children were considered as potentially confounding variables in these regression analyses. We also assessed the need to control for potential confounding variables by determining their correlation with any aspect of physical activity. The only variable to differ between groups was that TD children were more likely to be an only child, but there was no relationship observed between only child status and any of the physical activity measures by accelerometry or by questionnaire. We retained age and gender in the regression analyses to aid in comparison with other studies. To establish whether the influence of age on our physical activity measures differed by autism status we evaluated the statistical significance of the interaction (i.e., cross product term) between age and group (ASD or TD) in multiple linear regression models with each of the aggregate physical activity variables as the outcome variable. In a secondary analysis, we repeated these analyses for the accelerometry-based physical activity on weekdays and weekend days. We used a similar approach to determine whether associations between physical activity measured by accelerometry and questionnaire-based activity measures (number of activities, hours of activities) differed by group based on the statistical significance of the interaction term between group and hours spent in physical activity or variety of physical activity. Finally, in separate models for ASD and TD, we used multiple linear regression analyses to evaluate the association between accelerometry-measured activity and BMI z-score.
Results
Fifty-three children with ASD and 58 TD children completed the study. None of the demographic variables differed between children with ASD and typically developing children, except that TD children were more likely to be only children (Table 1).
Table 1.
Demographic characteristics in TD children and children with ASD
| TD children (n = 58) | Children with ASD (n = 53) | p a | |
|---|---|---|---|
| Age, years: M (SD) | 6.7 (2.4) | 6.6 (2.1) | .75 |
| VABS Score: M (SD) | N/A | 71.1 (12.4) | |
| DAS General Conceptual Ability Score: M (SD) | N/A | 85.8 (22.1)b | |
| Sex, male (%) | 78% | 83% | .47 |
| Race, white (%) | 76% | 83% | .35 |
| Maternal education, ≥college degree (%) | 72% | 74% | .89 |
| Paternal education, ≥college degree (%) | 67% | 54%c | .15 |
| Days a week mother exercises: M (SD) | 2.6 (2.1) | 2.1 (2.1) | .30 |
| Days a week father exercises: M (SD) | 3.1 (2.9) | 2.2 (2.7) | .13 |
| Child is an only child (%) | 26% | 11% | .05 |
| Overweight, ≥ 85th percentile BMI (%) | 22% | 26% | .62 |
| Underweight, BMI < 5th percentile BMI (%) | 0% | 1.9% | .48 |
Note. ASD: autism spectrum disorder; TD: typically developing
p values for differences in autism status groups,
n = 48,
n = 52
Accelerometry
Physical activity level was measured directly by accelerometry. Overall, 46 (87%) children with ASD and 54 (93%) TD children wore the accelerometers. Of these, thirty-five (66%) children with ASD and forty-seven (81%) TD children met our minimum criteria for inclusion of at least 600 minutes per day on three weekdays and one weekend day. Neither the proportion of children who wore the devices or the proportion of those wearing them who met criteria for inclusion differed by group (each p>0.05, chi-square test).
Total activity counts, the absolute amount of time (in minutes), and the percentage of time that children spent in light, moderate, and vigorous physical activity, adjusted for age and sex, are presented in Table 2. We did not observe any differences in total activity counts or time spent in light, moderate, vigorous, or MVPA combined between the two groups based on the weighted seven-day average. Percentage of time spent in light, moderate, vigorous and MVPA was also similar in the two groups. However, in a secondary analysis after controlling for age and sex, total activity counts for moderate activity during weekdays were significantly higher in TD children than in children with ASD (adjusted M 156,384 vs. 122,446, respectively, p < .05). Time spent in moderate activity was also significantly higher in TD children than children with ASD on weekdays (57.6 min/d vs. 46.5 min/d, respectively; p < .05). Percentage of time spent in moderate activity on the weekdays was higher in TD children than children with ASD, but the results were of borderline statistical significance (7.4% vs. 6.1%, p < .07), as was percentage of weekday time spent in MVPA (7.6% typically developing vs. 6.3% ASD, p < .08). Light, moderate, and vigorous activity on the weekends did not differ significantly by autism status. Overall, 43% of TD children participated in 60 minutes of MVPA a day compared to 23% of children with ASD (p < .06).
Table 2.
Estimates of physical activity from accelerometry for children with autism spectrum disorders and typically developing children
| Daily Weighted Average-7da | Daily Weighted Average-Weekdaysa | Daily Weighted Average-Weekend daysa | |||||||
|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||
| TD children (n = 47) | Children with ASD (n = 35) | p | TD children (n = 47) | Children with ASD (n = 35) | p | TD children (n = 47) | Children with ASD (n = 35) | p | |
| ACTIVITY COUNTS | |||||||||
| Light activity | 131,174 | 128,928 | .72 | 128,863 | 127,461 | .83 | 136,952 | 132,595 | .56 |
| Moderate activity | 150,060 | 127,475 | .19 | 156,384 | 122,446 | .05 | 134,248 | 140,047 | .79 |
| Vigorous activity | 11,794 | 12,965 | .75 | 13,375 | 12,744 | .89 | 7,844 | 13,518 | .14 |
| MVPA | 161,842 | 140,724 | .28 | 169,759 | 135,190 | .08 | 142,051 | 154,558 | .60 |
| Total Activity counts | 299,771 | 276,203 | .29 | 305,437 | 269,831 | .11 | 285,606 | 292,132 | .81 |
| TIME (minutes) PER DAY | |||||||||
| Light activity | 264 | 266 | .82 | 261 | 266 | .70 | 271 | 268 | .81 |
| Moderate activity | 55.7 | 48.0 | .17 | 57.6 | 46.5 | .05 | 51.1 | 51.7 | .93 |
| Vigorous activity | 1.4 | 1.6 | .76 | 1.6 | 1.5 | .88 | 1.0 | 1.7 | .17 |
| MVPA | 57.1 | 50.0 | .19 | 59.2 | 48.0 | .06 | 52.1 | 53.5 | .86 |
| PERCENTAGE of TOTAL TIME b | |||||||||
| Light activity | 34.6 | 35.3 | .64 | 33.9 | 34.7 | .62 | 36.1 | 36.6 | .79 |
| Moderate activity | 7.3 | 6.4 | .24 | 7.4 | 6.1 | .07 | 6.8 | 7.1 | .76 |
| Vigorous activity | 0.2 | 0.2 | .70 | 0.2 | 0.2 | .90 | 0.1 | 0.2 | .14 |
| MVPA | 7.5 | 6.6 | .28 | 7.6 | 6.3 | .08 | 7.0 | 7.4 | .69 |
Note. ASD: autism spectrum disorder; TD: typically developing; MVPA: moderate and vigorous physical activity
Least square means from linear regression, adjusted for age and sex.
Percentages do not total to 100% – remaining time is sedentary time.
Parent report of activity variety and time spent in activities (via questionnaire)
Parental reports of the time spent in and the variety of physical activities were correlated in the overall sample (r = .79, p < .0001). In multivariable analyses, adjusting for age and sex, we compared the number of types of physical activity the child engaged in (e.g., basketball, swimming, bicycling, etc.) and the total reported time spent in these activities between children with ASD and TD children (Table 3). Parents of children with ASD reported that their children participated in significantly fewer types of activities than did TD children (6.9 vs. 9.6 per year, respectively, p < .0001), and that children with ASD spent significantly less time in these activities annually than did TD children (158 hours ASD vs. 225 hours TD, p < .0001). The association between age and hours per year spent in activity differed by autism status (p-value for interaction = 0.01). Whereas age was not significantly associated with hours spent in physical activity for children with ASD (p = .93), there was a significant positive association between age and number of hours spent in physical activity for TD children (p < .01). The association between age and the number of activities children participated in did not differ significantly by autism status (p for interaction = .09). For both children with ASD and TD children, parents reported that younger children engaged in more activities than did older children (p = 0.03).
Table 3.
Reported number and time spent in physical activities per year, for children with autism spectrum disorders and typically developing children as measured by parent questionnairea
| TD children (n = 58) | Children with ASD (n = 53) | p | |
|---|---|---|---|
| Number of different activities | 9.6 | 6.9 | <.0001 |
| Hours per year | 225 | 158 | <.0001 |
Note. ASD: autism spectrum disorder; TD: typically developing
Least square means, adjusted for age and sex.
Comparison of accelerometer to questionnaire data
Among the 82 participants who had valid accelerometry data (47 TD, 35 ASD), we compared total activity counts and time spent in MVPA as measured by accelerometry with the number of physical activities and hours spent in physical activity, as reported by questionnaire. We assessed whether these associations differed by autism status, adjusted for age and sex. We did not find a significant relationship between reported activity (variety and time) and percentage time spent in MVPA measured by accelerometry. We also did not observe a significant interaction between autism status and reported time spent in physical activities or variety of activities, suggesting that the association between questionnaire-based measures and objectively measured physical activity by accelerometry did not differ by autism status.
Relationship to weight status
In both groups, BMI-z score was not significantly related to total activity counts or time, or percent time spent in MVPA.
Discussion
We sought to understand how physical activity measured objectively via accelerometry or by parent report would differ between children with ASD and TD children.
Our hypothesis that children with ASD would spend less time engaged in physical activity than TD children was only partially supported. Based on accelerometry measures, the two groups of children had similar levels of physical activity over the week. The only difference observed was seen on weekdays. Children with ASD spent less time in moderate activity than TD. The explanation for this is not clear, but one could speculate that children with ASD may engage in fewer activities after school than TD children. In contrast, based on parent report children with ASD spent significantly less time in physical activities and participated in a narrower variety of activities than did TD children.
The finding that time spent in MVPA overall as measured by accelerometry is similar between children with ASD and TD children but that children with ASD engaged annually in fewer parent-reported hours of physical activity and in a narrower variety of physical activities was unexpected. The lack of observed differences may be because some of the physical activity engaged in by children with ASD was not captured by our questionnaires. Children with ASD may engage in physical activity by pacing, roaming, or engaging in highly repetitive or self-stimulating types of physical behavior that characterize these disorders. For example, during television watching children with ASD may engage in more movement than typically developing children. These behaviors would be captured by accelerometry but might not be reported as physical activity by parents or may be reported as sedentary behavior (TV watching).
The lack of observed differences in physical activity levels based on accelerometry between children with ASD and TD children is similar to results reported by Rosser, Sandt and Frey (2005). In a second study, Pan and Frey (2006) measured time spent in MPVA in 30 children with ASD in elementary (n = 9), middle (n = 9) and high school (n = 12). Seventy-eight percent (78%) of the elementary school children, 67% of the middle school children, and 8% of the high school children accumulated 60 minutes of daily MVPA. Only twenty-three percent (23%) of the participants with ASD in our study met the criteria for MVPA.
We did not observe any association of physical activity level measured by accelerometry for either total counts or time in MVPA with BMI-z score. In contrast, this association has been previously identified in studies of TD children using both cross-sectional and prospective study designs (Must & Tybor, 2005).
Several limitations in this study are noteworthy. First, we used the cut-off points determined from equations by Puyau et al. (2004) to calculate MVPA based on activity counts. These cutoff points categorize time spent as sedentary, light, moderate, and vigorous activity. A single set of calculations is used for all children up to age 18 years based on laboratory analysis of accelerometry data during performance of a specified set of activities, even though it is known that the energy cost may be different with age. Unfortunately, we were unable to find a set of equations for children aged 3–11 years of age. The Puyau equations most closely match the age range of our study participants and were developed in a cohort of children aged 7–18 years. Although the application of a single equation across the age range may have introduced error, we expect this would have affected both groups similarly.
A second limitation relates to our approach to estimating annual hours of physical activity, based on parents' recall of annual time spent in specific activities. We were unable to identify a suitable validated questionnaire for children with ASD and TD children to determine types of activities and frequencies of activities that they participated in and therefore we developed a questionnaire tailored to our research questions. We acknowledge that this questionnaire has not been tested for validity in TD children or children with ASD; we did confirm its reliability. We did not observe a positive association between accelerometry and annual time spent in activities as reported by the parent, but the extent to which this reflects a lack of validity in the questionnaire is uncertain. The objective of the questionnaire was to determine whether children with ASD participated in fewer physical activities than TD children or if the time spent in a variety of physical activities differed among children with ASD and TD children. Many movements that the accelerometer would record as MVPA might be engaged in intermittently by the child and not considered physical activities by the parent. For example, some children with ASD engage in frequent roaming and pacing, and this activity was not captured on the physical activity checklist; this may also be true for young typically developing children whose activity might be intermittent jumping, running, or playing in the house. Some specific limitations of our grid to estimate time spent in various activities are noteworthy. The highest response option was 40 hours or more per year, and so children who engaged in, for example, 80 hours per year of an activity would not be differentiated from children who engaged in 40 hours and their time spent in activity would be underestimated. Our measurements of reported physical activity for both children with ASD and TD children may also be subject to recall bias and/or reporting error.
Another limitation of our study is that we were not able to account for potential differences in physical activity during the school year versus summer vacation that could affect how active a child was during the week that they wore the accelerometer. However, we observed similar numbers for children in each group who wore the accelerometer in the summer (TD n = 5 and ASD n = 7). With respect to the number of activities children engaged in, our questionnaire did not account for the intensity of activities, only the number of distinct activities.
A strength of our study was in the use of accelerometers to measure directly children's physical activity levels. This allowed us to compare an objective measure of physical activity with parent responses to questions about the types of activities in which their child participated over the past year. Our study was also substantially larger than previous investigations. Although we were initially concerned that children with ASD would have difficulty wearing the accelerometer, their compliance was quite good; 46 of the 53 children with ASD in the study wore the device for some time and two-thirds met our criteria of wearing the accelerometer for at least 600 minutes on four days.
Our findings using accelerometers suggest that young children with ASD have similar overall physical activity levels as TD children. We did observe a significant difference of 11 minutes per day in moderate activity on weekdays by accelerometer, with TD children being more active than children with ASD. However, because of the large number of statistical comparisons, we cannot exclude the possibility that this was due to chance.
Previous work (Troiano et al., 2008) has shown that physical activity levels decline with age in TD children. One cross-sectional study in youth with ASD (Pan and Frey 2005) also suggests that MVPA declines with age in children with ASD. This represents an important area of inquiry given our finding that parent-reported time spent in specific physical activities and the variety of physical activities children with ASD engage in were lower than those of TD children. Further studies in adolescents with ASD are needed to establish that they are getting adequate amounts of daily physical activity to meet overall health recommendations.
Acknowledgments
This study was supported by NIH grant R21 HD048989, NIH grant 2P30HD004147-33A2, and Clinical and Community Research Methods Core of the Boston Nutrition Obesity Research Center grant 5P30DK046200. The study sponsors had no role in 1) study design; 2) collection, analysis, and interpretation of data; 3) the writing of the report; or 4) the decision to submit the manuscript for publication.
Footnotes
The authors report no conflicts of interest.
References
- Blanchard LT, Gurka MJ, Blackman JA. Emotional, developmental, and behavioral health of American children and their families: a report from the 2003 National Survey of Children's Health. Pediatrics. 2006;117(6):e1202–1212. doi: 10.1542/peds.2005-2606. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (CDC) National Center for Health Statistics (NCHS) National Survey of Children's Health. U.S. Department of Health and Human Services, Centers for Disease Control and Prevention; Hyattsville, MD: 2003. State and Local Area Integrated Telephone Survey. Available at: http://www.cdc.gov/nchs/data/slaits/NSCH_Questionnaire.pdf. [Google Scholar]
- CDC. NCHS . National Health and Nutrition Examination Survey Questionnaire, Physical Activity. U.S. Department of Health and Human Services, Centers for Disease Control and Prevention; Hyattsville, MD: 2003–2004. Available at: http://www.cdc.gov/nchs/nhanes/nhanes2003–2004/quex03_04.htm. [Google Scholar]
- CDC Physical Activity for Everyone: Children. 2011 Available at: http://www.cdc.gov/physicalactivity/everyone/guidelines/children.html.
- CDC Division of Nutrition, Physical Activity and Obesity. Healthy Weight: Assessing Your Weight: About BMI for Children and Teens. 2011 Available at: http://www.cdc.gov/healthyweight/assessing/bmi/childrens_bmi/about_childrens_bmi.html.
- Elliott CD. Differential Ability Scales. The Psychological Corporation; San Antonio, TX: 1990. [Google Scholar]
- Green D, Charman T, Pickles A, Chandler S, Loucas T, Simonoff E, et al. Impairment in movement skills of children with autistic spectrum disorders. Developmental Medicine & Child Neurology. 2009;51(4):311–316. doi: 10.1111/j.1469-8749.2008.03242.x. [DOI] [PubMed] [Google Scholar]
- Janssen I, Leblanc AG. Systematic review of the health benefits of physical activity and fitness in school-aged children and youth. International Journal of Behavioral Nutrition and Physical Activity. 2010;7:40. doi: 10.1186/1479-5868-7-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuczmarski RJ, Ogden CL, Guo SS, Grummer-Strawn LM, Flegal KM, Mei Z, et al. 2000 CDC Growth Charts for the United States: methods and development. Vital Health Statistics. 2002;11(246):1–190. [PubMed] [Google Scholar]
- Must A, Tybor DJ. Physical activity and sedentary behavior: a review of longitudinal studies of weight and adiposity in youth. International Journal of Obesity. 2005;(Suppl 2):S84–96. doi: 10.1038/sj.ijo.0803064. [DOI] [PubMed] [Google Scholar]
- Pan CY. Objectively measured physical activity between children with Autism Spectrum Disorders and children without disabilities during inclusive recess settings in Taiwan. Journal of Autism and Developmental Disorders. 2008;38:1292–1301. doi: 10.1007/s10803-007-0518-6. [DOI] [PubMed] [Google Scholar]
- Pan CY, Frey GC. Identifying physical activity determinants in youth with Autistic Spectrum Disorders. Journal of Physical Activity and Health. 2005;2:412–422. [Google Scholar]
- Pan CY, Frey GC. Physical activity patterns in youth with Autism Spectrum Disorders. Journal of Autism and Developmental Disorders. 2006;36:597–606. doi: 10.1007/s10803-006-0101-6. [DOI] [PubMed] [Google Scholar]
- Puyau M, Adolph A, Vohra F, Zakeri I, Butte N. Prediction of activity energy expenditure using accelerometers in children. Medicine & Science in Sports and Exercise. 2004;36(9):1625–1631. [PubMed] [Google Scholar]
- Rosser Sandt DD, Frey GC. Comparison of physical activity levels between children with and without Autistic Spectrum Disorders Adapted Physical Activity Quarterly. 2005;22:146–159. [Google Scholar]
- Rutter M, Le Couteur AL, Lord C. Autism Diagnostic Interview-Revised. Western Psychological Services; Los Angeles: 2003. [Google Scholar]
- Schmalz DL, Deane GD, Birch LL, Davison K. A longitudinal assessment of the links between physical activity and self-esteem in early adolescent non-Hispanic females. Journal of Adolescent Health. 2007;41(6):559–565. doi: 10.1016/j.jadohealth.2007.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spadano JL, Must A, Bandini LG, Dallal GE, Dietz WH. Energy cost of physical activities in 12-y-old girls: MET values and the influence of body weight. International Journal of Obesity. 2003;27(12):1528–33. doi: 10.1038/sj.ijo.0802440. [DOI] [PubMed] [Google Scholar]
- Sparrow SS, Cicchetti DV, Balla DA. Vineland Adaptive Behavior Scales. 2nd ed. AGS Publishing; Circle Pines, MN: 2005. [Google Scholar]
- Troiano R, Berrigan D, Dodd K, Masse L, Tilert T, McDowell M. Physical activity in the United States measured by accelerometer. Medicine & Science in Sports and Exercise. 2008;40(1):181–188. doi: 10.1249/mss.0b013e31815a51b3. [DOI] [PubMed] [Google Scholar]
- Venkatesan S. Activity log of preschool children with developmental disabilities and Autism Spectrum Disorders. Asia Pacific Disability Rehabilitation Journal. 2005;16(1):68–76. [Google Scholar]