Abstract
We examined whether people who tend to catastrophize about pain and who also attempt to regulate negative thoughts and feelings through suppression may represent a distinct subgroup of individuals highly susceptible to pain and distress. Ninety-seven healthy normal participants underwent a 4-min ischemic pain task followed by a 2-min recovery period. Self-reported pain and distress was recorded during the task and every 20 s during recovery. Participants completed the Pain Catastrophizing Scale and the White Bear Suppression Inventory. Repeated measures multiple regression analysis (using General Linear Model procedures) revealed significant 3-way interactions such that participants scoring high on the rumination and/or helplessness subscales of the Pain Catastrophizing Scale and who scored high on the predisposition to suppress unwanted thoughts and feelings reported the greatest pain and distress during recovery. Results suggest that pain catastrophizers who attempt to regulate their substantial pain intensity and distress with maladaptive emotion regulation strategies, such as suppression, may be especially prone to experience prolonged recovery from episodes of acute pain. Thus, emotion regulation factors may represent critical variables needed to understand the full impact of catastrophic appraisals on long-term adjustment to pain.
Keywords: Pain catastrophizing, Suppression, Emotion regulation, Acute pain
Introduction
Pain catastrophizing is consistently related to acute pain intensity among healthy people (Severeijns et al. 2005; Sullivan et al. 1995), and to pain severity, emotional distress and poor adjustment among chronic pain patients (Severeijns et al. 2001, 2004; Sullivan et al. 2001). Pain catastrophizing is defined as a predisposition to ruminate, magnify and feel helpless about pain (Sullivan et al. 1995). People who tend to catastrophize about pain may believe that pain signals harm and is generally awful, and such pain schemas may in turn bias attention toward the worst and most negative affectively-charged information presented by a painful stimulus, and direct attention away from more innocuous sensory information (Michael and Burns 2004; Sullivan et al. 2001). Thus, pain catastrophizers may be vigilant for, and selectively attend to the most threatening aspects of a painful experience (Crombez et al. 2004; Goubert et al. 2004). Elevated pain perception and negative emotions are the results of such a process (Bartley and Rhudy 2008; Smeets et al. 2006; Turner et al. 2004). Although a schema-activation model appears to be a useful theoretical framework by which to conceptualize the catastrophizing-pain relationship, there is debate about whether catastrophizing should be viewed as a cognitive set, a coping strategy or a personality trait. Indeed, one alternative conceptualization argues that pain catastrophizing represents a coping response by which an individual utilizes exaggerated pain expression as a way of eliciting assistance or empathic responses from others (Sullivan et al. 2001). Too, catastrophizing has been conceptualized as a personality trait engendered by early learning history with experiences of pain (Whitehead et al.1994; Muris et al. 2007).
Research has begun to support these kinds of cognitive and trait conceptualizations of pain catastrophizing, but what is less well-known are the emotion regulation strategies that catastrophizers bring to bear to cope with the high levels of emotional distress and perceived pain intensity inspired by catastrophic appraisals. Depending on how distress is regulated, negative outcomes may be ameliorated or exacerbated. Research indicates that various regulation or coping strategies used primarily to avoid information about, or feelings engendered by a noxious event are not adaptive in the long term. Suppression is one such tactic.
Suppression has been characterized as a “response-focused” emotion regulation strategy that people use to reduce the impact of a negative emotional experience (Gross and John 2003). Suppression, according to Gross and colleagues (Gross 1998; Gross and John 2003; Gross and Levenson 1993) is attempted only after an emotion is activated, and has the effect of reducing the behavioral expression of emotion (e.g., facial expressions of disgust) but not the subjective awareness and physiological arousal that may accompany it. Indeed, subjective experience and physiological activation may be magnified during efforts to suppress (Gross 1998; Gross and Levenson 1993, 1997). Alternatively, Wegner’s ironic process model of thought suppression (Wegner et al. 1987) focuses on delayed effects. Attempts to suppress unwanted thoughts, including those regarding pain and distress, may paradoxically increase awareness and salience of the thoughts and feelings an individual desires to avoid. Cioffi and Holloway (1993) and Sulllivan et al. (1997) demonstrated that efforts to suppress pain-related thoughts either during or prior to painful stimulation had the unintended effect of increasing reports of pain severity relative to reports of individuals who did not attempt to suppress. Further, Burns (2006) showed that attempts to suppress during pain may also affect physiological arousal during a subsequent but non-painful stressor. In sum, both views of suppression suggest that attempts to avoid, inhibit or suppress thoughts and feelings inspired by pain may have the unintended and paradoxical consequence of magnifying awareness of pain intensity, heightening fear and anxiety, and sustaining physiological arousal.
To improve understanding of how catastrophizing impacts pain perception in the short and long term, we believe that a cognitive conceptualization of pain catastrophizing must be integrated with models of emotion regulation. We examined the potential effects of pain catastrophizing and thought suppression taken together (i.e., additively or in interaction), rather than testing effects of each factor considered individually. Evidence suggests that high catastrophizers become emotionally overwhelmed by the experience of pain due to a narrow focus on the most threatening information posed by painful stimulation (Michael and Burns 2004; Sullivan et al. 2001). Catastrophizers are therefore faced with having to regulate rather intense negative emotional responses to pain. A certain subgroup of them may attempt to mitigate this distress by suppressing awareness of both thoughts and feelings surrounding the painful event. As shown in previous research, however, suppression typically does not work as intended. Thus, a high pain catastrophizer who also tends to regulate perceptions of pain and distress by attempting to suppress awareness may ironically experience exaggerated negative pain responses and a prolonged recovery. Although a high catastrophizer who does not routinely use suppression to regulate pain and distress may suffer to a greater degree than a low catastrophizer, the former’s experience would probably still be less agonizing than the catastrophizer who also attempts to suppress.
The purpose of this study was to test whether the pain and distress experienced during and following acute pain-induction is affected by the interactive effects of the tendency to catastrophize about pain and the tendency to suppress negative thoughts and feelings. We used trait measures to tap these constructs—the Pain Catastrophizing Scale (PCS: Sullivan et al. 1995) and the White Bear Suppression Inventory (WBSI; Wegner and Zanakos 1994). Given the detrimental effects of making catastrophic appraisals about noxious stimuli and attempting to regulate the negative thoughts and feelings that accompany such stimuli through suppression, we expected that participants characterized by relatively high pain catastrophizing scores and high thought suppression scores to report the highest pain intensity during pain-induction and to reveal the slowest recovery following pain. Because findings suggest that suppression appears to exert primarily delayed effects on pain and physiological reactivity (Burns 2006; Burns et al. 2008a, 2008b; Cioffi and Holloway 1993), we expected the most pronounced interactive relationships to emerge during recovery following pain-induction.
In addition, recent factor analyses of the PCS identified a three-component model of this phenomenon: rumination, magnification, and helplessness (Severeijns et al. 2002; Van Damme et al. 2002). It could be the case that catastrophizers who are especially elevated on the tendency to magnify the awfulness of the pain experience may produce the greatest level of negative emotion that they then must regulate. If so, then we expected people high on the magnification subscale of the PCS who are also high on the WBSI to be particularly vulnerable to pain and distress.
Methods
Participants
Ninety-seven healthy normal participants (men; n = 41) were recruited through email postings at a university, and were paid $25. Participants were excluded if (a) they ingested any analgesic medication, alcohol or caffeine within 3 h prior to the study; (b) they had a history of anxiety or depressive disorders; (c) they had any current alcohol or substance abuse problems; (d) they had chronic pain (pain lasting greater than 4 months) from any source within the past year. The mean age was 25 years (SD = 2.83). Sample characteristics appear in Table 1.
Table 1.
Sample characteristics (N = 97)
| Gender (male) | 42% male |
|---|---|
| Age (years) | M = 25.0 (SD = 2.83) |
| Race/ethnicity | 63.0% Caucasian, 23.0% Asian, 9.2% African Americans, 2.0% Native Hawaiian/Pacific Islander, 2.0% Indian/Alaskian, 1.0% Hispanic/Latino |
| WBSI | M = 41.84 (SD = 10.8) |
| RS | M = 7.78 (SD = 5.3) |
| HS | M = 7.73 (SD = 6.3) |
| MS | M = 4.00 (SD = 3.0) |
WBSI White Bear Thought Suppression Inventory; PCS Pain Catastrophizing Scale; RS Rumination subscale score of PCS; HS Helplessness subscale score of PCS; MS Magnification subscale score of PCS
Apparatus
The Jamar Hydraulic Hand Dynamometer was used to induce pain through an ischemic pain procedure (see below). This task used a hand dynamometer in order to exercise dominant forearm muscles prior to inflation of a standard manual sphygmomanometer cuff to create temporary forearm ischemia.
Measures
Pain Catastrophizing Scale
The PCS (Sullivan et al. 1995) is a 13-item scale that measures rumination (e.g., “I can’t seem to keep it out of my mind”), magnification (e.g., “I wonder whether something serious may happen”), and helplessness (e.g., “I feel I can’t go on”) regarding pain. Sullivan et al. reported a high degree of stability across a 6-week period (r = .75, P < .001) and adequate internal consistency (coefficient alpha for entire scale of .87). Coefficient alphas were .87, .60 and .79 for the rumination, magnification and helplessness subscales, respectively. Osman et al. (2000) provided support for the validity of the PCS subscale scores by reporting significant correlations with measures of pain severity, interference and negative affectivity.
White Bear Suppression Inventory
The WBSI (Wegner and Zanakos 1994) is a 15-item questionnaire measuring the tendency to suppress thoughts. Participants rate, on a 5-point Likert scale, the extent to which they agree (1 = strongly disagree; 5 = strongly agree) with statements such as; “I have thoughts that I cannot stop” and “There are things I prefer not to think about.” Wegner and Zanakos report good test–retest reliabilities (r = .69 to r = .92), and an internal consistency coefficient (alpha) for the entire scale of .88. Additionally, Wegner and Zanakos, provided support for the validity of the WBSI by reporting significant correlations with self-report measures of obsessive thinking, anxiety and depression (r’s > .39).
Self-reported pain and distress
To assess pain intensity and distress, participants recorded their perceived pain intensity and distress on numerical rating scales (NRS; “0” = none; “5” = extreme). Pain and distress were reported prior to the start of the ischemic pain task, immediately after, and every 20 s following the pain task for 120 s. Participants were instructed to rate the degree to which they felt physical pain (pain intensity ratings), and the degree to which the pain was upsetting and distressing (distress ratings).
Pain-induction
Pain was induced with an ischemic pain procedure based on procedures described by Maurset et al. 1992. This task used a hand dynamometer in order to exercise dominant forearm muscles during inflation of a standard manual sphygmomanometer cuff to create temporary forearm ischemia. Participants were asked to apply his or her maximum grip of the nondominant hand to the hand dynamometer to determine maximum grip. The blood pressure cuff was then inflated on the participant’s nondominant bicep up to 200 mmHg depending on participant gender. Participants were then told to grip the dynamometer again at a level determined by the experimenter to be 25% of their maximum grip, and to maintain this grip during the duration of the task. Unbeknownst to participants, they were not allowed to exceed 4 min. At 4-min, participants were told to release their grip and the blood pressure cuff was removed.
Procedure
Prior to the laboratory session, participants completed the PCS and WBSI. Upon completion of informed consent, participants were seated upright in a chair facing a desk. The shape of the desk allowed the participant to rest his or her arm used for the pain induction task on the desk. Participants completed a pain and distress NRS, and were then instructed to apply their maximum grip to the dynamometer in order to establish their maximum grip in pounds. Instructions for the experiment and the blood pressure cuff were given. The cuff was inflated to 185 mmHg for females and to 200 mmHg for males. Participants were then told to maintain 25% of their maximum grip for the duration of the task. Throughout the study, the experimenter monitored the dynamometer gauge to assure that appropriate grip pressure was maintained.
The participant then gripped the dynamometer at 25% of his/her previously established maximum grip for a period of 4 min. They were told to maintain their grip until asked to release it. After 4-min, the dynamometer was released, the blood pressure cuff deflated and participants were again given the pain rating measure. Then, the participants were asked to rate how much physical pain and distress they were experiencing every 20 s for a total of 120 s. Upon completion of the procedure, participants were thoroughly debriefed and paid for their participation.
Data reduction and analysis
Within-subject ANOVAs were used to examine changes in pain and distress ratings over time. Because Rumination, Helplessness and Magnification subscale scores were significantly, albeit modestly, correlated with WBSI scores (r’s = .34, .44, and .23, respectively), variables were centered on respective means for use in multiple regressions. Repeated measures multiple regression analyses (using General Linear Model procedures) were conducted to determine whether the subscales of the PCS scale (rumination, magnification, helplessness) interacted with WBSI scores to impact self-reported pain and distress over eight assessment points (i.e., baseline, post-task, 20, 40, 60, 80, 100, 120 s into recovery). Significant interaction effects were examined in detail in two ways. First, simple Pain Catastrophizing Subscale scores × WBSI interaction effects on pain and/or distress were tested at each period. For significant interactions, beta weights were generated describing the relationship between Pain Catastrophizing Scale subscale scores and pain or distress at hypothetical levels of WBSI scores (+1 SD and −1 SD from the WBSI mean). These beta weights were tested for significance following procedures described in Cohen et al. (2003). Second, results were displayed graphically by solving regression equations for hypothetical Pain Catastrophizing Scale subscale and WBSI scores (again, +1 SD and −1 SD from the respective means) at each assessment point (Cohen et al. 2003).
Results
Change from baseline to task to recovery
Within-subject ANOVAs were conducted to determine whether the ischemic pain task resulted in significant changes from baseline to task and into recovery for pain intensity and emotional distress. Means and SDs for these variables are presented in Table 2. The ischemic pain task resulted in significant changes over time [F’s (7, 651) > 103; P’s > .01] for both pain and distress. Simple comparisons showed that both pain and distress increased significantly from baseline to post-task [F’s > 225; P’s < .01]. While pain and distress ratings decreased throughout the recovery period, pain ratings remained significantly elevated above baseline by the end of the 2 min recovery period, t (96) = 14.04, P < .001. Post-recovery distress ratings were also elevated relative to baseline, but the difference was nonsignificant, t (96) = 1.62, P < .10.
Table 2.
Means and standard deviations for pain intensity and emotional distress from baseline to recovery
| Pain Intensity |
Emotional distress |
|||
|---|---|---|---|---|
| Mean | (SD) | Mean | (SD) | |
| Baseline | .06 | (.03) | .38 | (.08) |
| Post-PT | 4.25 | (.09) | 3.01 | (.17) |
| 20-s | 2.92 | (.11) | 1.63 | (.15) |
| 40-s | 2.68 | (.11) | 1.33 | (.15) |
| 60-s | 2.36 | (.11) | .98 | (.13) |
| 80-s | 2.02 | (.12) | .77 | (.12) |
| 100-s | 1.78 | (.12) | .67 | (.11) |
| 120-s | 1.70 | (.11) | .59 | (.10) |
Post-PT = immediately following pain task; 20-s = 20 s into recovery; 40-s = 40 s into recovery; 60-s = 60 s into recovery; 80- s = 80 s into recovery; 100-s = 100 s into recovery; 120-s = 120 s into recovery
Rumination subscale of PCS × WBSI × period for pain
A significant Rumination × WBSI × Period interaction was found for pain ratings, F(7, 630) = 2.16, P < .04, suggesting that the nature of the Rumination × WBS Iinteraction changed over time. To dissect this complex interaction, Rumination × WBSI interactions were tested at each time point. These interactions were significant at the 20-, 40-, 60-, and 80-s points. Separate slopes were then generated describing the relationship between Rumination subscale scores and pain ratings for each of these periods for hypothetical WBSI scores (+1 SD and −1 SD from the sample mean). See Cohen et al. (2003) for a detailed account of this procedure. Results showed that for low WBSI scores, beta weights for Rumination subscale scores ranged from −.03 to .08, and were all nonsignificant (P’s > .10). For high WBSI scores, the beta weights for Rumination subscale scores at 20-, 40-, 60-, and 80-s were significant (betas > .34; P’s < .05). For the 100- and 120-s periods, only the main effects for Rumination (betas > .24; P’s < .05), and WBSI scores (betas > .22; P’s < .05). To further illustrate the nature of these effects, the regression equations describing the relationships between Rumination subscale scores and WBSI scores were solved for four hypothetical values (−1 SD and +1 SD from the sample means of the scales, following procedures described by Cohen et al. 2003) at each period. See Fig. 1. Results of the slope tests coupled with the pattern of values shown in Fig. 1 suggest that all participants seemed to report similar pain levels at the end of the pain task, but participants described by both high rumination and high trait suppression reported greater elevations in pain intensity, relative to all other groups, beginning early in recovery. This distinction for high rumination/high suppression participants was attenuated, however, late in recovery, when participants with high rumination or high trait suppression reported elevated pain.
Fig. 1.
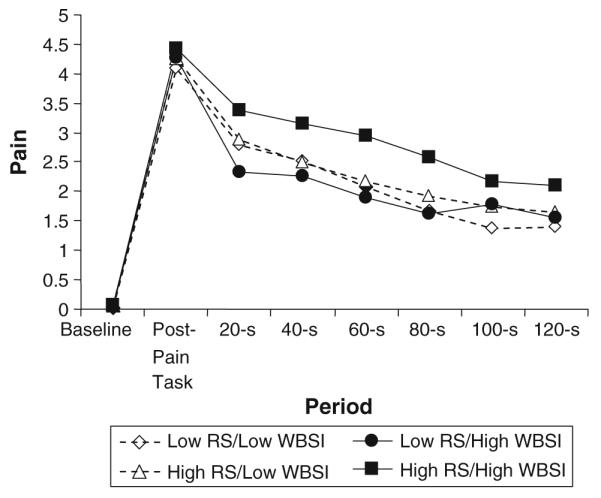
Rumination subscale × White Bear Suppression Inventory × Period effects for pain intensity ratings. Rumination subscale (RS) and White Bear Suppression Inventory (WBSI) predicted values = ±1 SD from sample means
Helplessness subscale of PCS × WBSI × period for pain
A significant Helplessness × WBSI × Period interaction was also found for pain ratings, F(7, 630) = 2.28, P < .03, suggesting, as with rumination, that the nature of the Helplessness × WBSI interaction changed over time. To dissect this complex interaction, Helplessness × WBSI interactions were tested at each period. These interactions were significant at the 20-, 40-, 60-, and 80-s points. Slopes were generated for the Helplessness subscale scores and pain ratings at each period for hypothetical WBSI scores (+1 SD and −1 SD). Results showed that for low WBSI scores, beta weights for Helplessness subscale scores ranged from −.11 to .02, and were all nonsignificant (P’s > .10). For high WBSI scores, the beta weights for 20-, 40-, 60-, and 80-s were significant (betas > .31; P’s < .05). For the 100- and 120-s periods, only the main effects for Helplessness (betas > .26; P’s < .05) and WBSI scores (betas > .22; P’s < .05) were significant. The regression equations describing the relationships between Helplessness subscale scores and WBSI scores were then solved for four hypothetical values (−1 SD and +1 SD from the sample means of the scales) at each period. See Fig. 2. Similar to rumination, results of the slope tests and the pattern of values shown in Fig. 2, taken together, suggest that all participants reported similar pain levels at the end of the pain task, but participants described by both high helplessness and high trait suppression showed greater elevations in pain intensity, relative to all other groups, beginning early in recovery. Again, this distinction for these participants eroded late in recovery began to converge, when participants with high helplessness or high suppression reported prolonged pain.
Fig. 2.
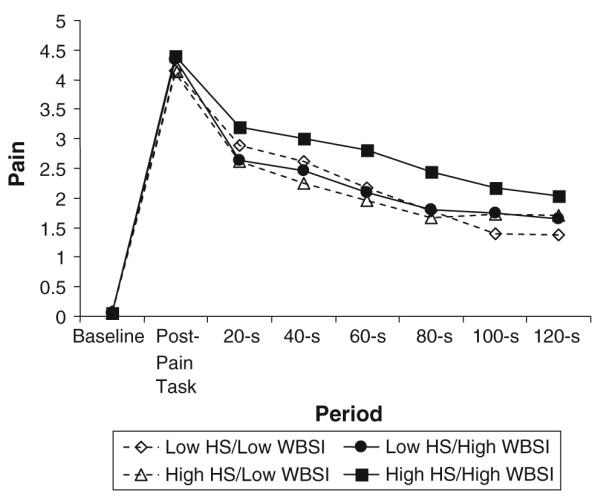
Helplessness subscale × White Bear Suppression Inventory × Period effects for pain intensity ratings. Helplessness subscale (HS) and White Bear Suppression Inventory (WBSI) predicted values = ±1 SD from sample means
Magnification subscale of PCS × WBSI × period for pain
The Magnification × WBSI × Period interaction for pain ratings was nonsignificant F(7, 630) < 1, as was the Magnification × Period interaction F(7, 644) < 1. The main effect for Magnification, collapsed across Period, was also nonsignificant [F(1, 90) < 1]. Results suggest that pain intensity experienced during and following acute pain-induction was not affected significantly by the interactive effects of the tendency to suppress negative thoughts and feelings and the tendency to magnify painful experiences, nor by the main effects of magnification.
Rumination subscale of PCS × WBSI × period for distress
The Rumination × WBSI × Period interaction was nonsignificant F(7, 623) = 1.31, P = .242 for distress ratings. However, the Rumination × Period 2-way interaction was significant F(7, 637) = 4.67, P < .001, suggesting that the relationship between rumination and distress changed over time. To dissect this significant interaction, regression equations describing the relationship between Rumination subscale scores and distress were computed at each period. Beta weights at post-task, 20-, 40-, 60-, 80-, 100-, and 120-s were .25, .31, .34, .33, .31, .26 and .14, respectively, with all significant (P’s < .02) except the beta weight for 120-s (P > .10). Results implied that the strongest association between rumination and distress emerged during early recovery, but that the relationship decreased in magnitude late in recovery.
Helplessness subscale of PCS × WBSI × period for distress
A significant Helplessness × WBSI × Period interaction was found for distress ratings, F(7, 623) = 2.28, P < .03, telling that the nature of the Helplessness subscale × WBSI interaction changed over time. Again, Helplessness × WBSI interactions were tested at each period. These interactions were significant at the 20-, 40-, 60-, 80-, and 100-s points. Slopes were generated for the Helplessness subscale scores and pain ratings at each period for hypothetical WBSI scores (+1 SD and −1 SD). Results showed that for low WBSI scores, beta weights for Helplessness subscale scores ranged from −.08 to −.01, and were all nonsignificant (P’s > .10). For high WBSI scores, the beta weights for 20-, 40-, 60-, 80-, and 100-s were significant (betas > .32; P’s < .05). No other main effects for Helplessness and WBSI scores were significant. To further illustrate the nature of this significant 3-way interaction, the regression equations describing the relationships between Rumination subscale scores and WBSI scores were solved for four hypothetical values (−1 SD and +1 SD from the sample means of the scales, following procedures described by Cohen et al. 2003) at each period. See Fig. 3. Results of the slope tests coupled with the pattern of values shown in Fig. 3 suggest that all participants seemed to report similar pain levels at the end of the pain task, but participants described by both high rumination and high trait suppression reported greater elevations in pain intensity, relative to all other groups, beginning early in recovery. This difference was attenuated only very late in recovery.
Fig. 3.
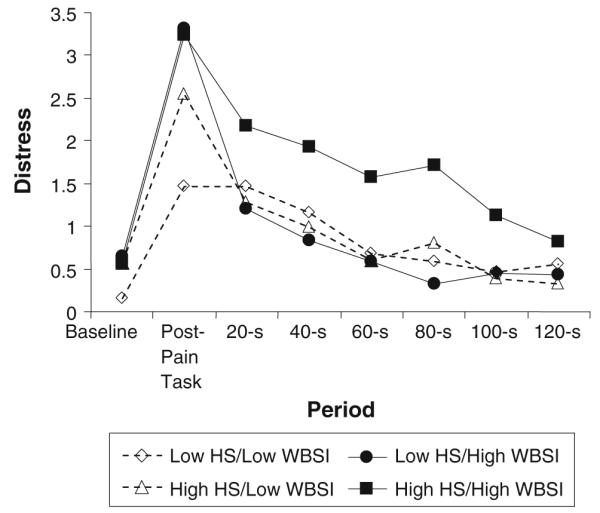
Helplessness subscale × White Bear Suppression Inventory × Period effects for distress ratings. Helplessness subscale (HS) and White Bear Suppression Inventory (WBSI) predicted values = ±1 SD from sample means
Magnification subscale of PCS × WBSI × period for distress
All interactions featuring the Magnification subscale were nonsignificant F’s < 1, as was the main effect (collapsed across Period) [F < 1]. Similar to results for pain, distress experienced during and following acute pain-induction was not affected by the interactive effects of the tendency to suppress negative thoughts and feelings and the tendency to magnify painful experiences, nor by the main effects of magnification.
Discussion
The tendency to catastrophize about pain may be rooted in stable pain schemas formulated around the belief that pain is harmful and unmanageable, which leads to selective focus on negative information attending painful stimulation. Consequently, catastrophizers experience heightened pain intensity and emotional distress. We submit that high catastrophizers must also regulate thoughts and feelings during and following acute pain, and some may do so through attempts to suppress. Suppression, however, may paradoxically result in heightened awareness of pain and suffering. If this is the case, then catastrophizers who also tend to suppress unwanted thoughts and emotions would represent a distinct subgroup of individuals who are highly susceptible to pain and distress. We tested these propositions by examining the interactive effects of PCS subscales and WBSI scores on pain and distress during and following acute pain-induction.
Two components of pain catastrophizing—the tendencies to ruminate about pain and to feel helpless in the face of pain—were related most strongly to pain and distress among those participants who also reported a predisposition to suppress unwanted thoughts and feelings.
Although the interactive effects of rumination by suppression and helplessness by suppression were not apparent during acute pain induction, the patterns of ratings reported following pain (i.e., during recovery) suggested that participants characterized by a combination of both high rumination and/or helplessness and high suppression may constitute a distinct subset of catastrophizers who are especially susceptible to experiencing prolonged pain and distress after enduring a painful event. Although participants with elevated scores on rumination/helplessness and suppression appeared to experience the most detrimental effects, our findings also revealed that participants characterized by high catastrophizing components but low suppression were indistinguishable from low catastrophizers in terms of pain and distress during recovery.
On one level, findings support our notion that the full range and extent of the detrimental effects of catastrophic appraisals may be better understood through theoretical conceptualizations that integrate multiple constructs. In this case, individual differences in how pain is appraised were combined with individual differences in how pain and distress may be regulated or managed. High catastrophizers may not necessarily use suppression to regulate negative emotions, as the correlations between castrophizing subscales and the WBSI indicate. Results imply, however, that for those who do routinely try to suppress awareness of pain and suffering, they may ironically render pain-related thoughts and feelings highly accessible to consciousness and thereby delay recovery. Findings that suppression, in concert with catastrophizing, primarily affected pain recovery is consistent with results of previous studies showing a variety of delayed effects following attempts to suppress (Cioffi and Holloway 1993; Sulllivan et al. 1997; Burns 2006). In short, the routine use of emotion regulation tactics or coping strategies that serve not to reduce or resolve the emotional turmoil attending catastrophic appraisals—such as suppression—may instead aggravate or make more salient the overwhelming aspects of pain and so prolong pain and suffering. The final impact of a painful event, then, may not solely be the result of catastrophizing, but may also be a result of the tactics used to respond to these appraisals and their emotional concomitants.
On another level, these results run counter to the notion implicit in past research that all high catastrophizers tend to experience greater negative emotion and pain sensitivity than low catastrophizers, and do so during pain-induction (Bartley and Rhudy 2008; France et al. 2002 Smeets et al.2006; Turner et al. 2004). Our results imply that only one subgroup of high catastrophizers are actually at increased risk for elevated pain and distress—those also characterized by maladaptive emotion regulation. Thus, the significant main effects for catastrophizing, that were the targets of previous studies, may have concealed important distinctions among high catastrophizers. Those high catastrophizers who do not routinely use detrimental emotion regulation strategies may suffer less extreme pain and distress. However, the high catastrophizing/high suppression group was clearly distinguished from the other groups only as recovery unfolded and not immediately following acute pain-induction. It may be the case that the tendency to catastrophize about pain may be necessary but not sufficient to produce protracted recovery. The additional consideration of emotional regulation may provide the needed ingredient to discriminate catastrophizers who experience extended periods of pain and distress following the original noxious stimulus from catastrophizers who do not. Thus, this kind of profile approach may be one method to help capture the dual and potentiating effects of appraisals and emotion regulation strategies in order to identify people who truly have the worst prognosis for dealing with, and adjusting to painful events.
Of note, the interactive effect of magnification by suppression was nonsignificant. Indeed, even the magnification main effect was miniscule (F < 1). These findings were surprising in that the tendency to magnify and exaggerate the negative aspects of a stimulus seems to lie at the heart of the pain catastrophizing construct (Severeijns et al.2001; Tan et al. 2001; Turner et al. 2001), and so we expected this component to produce the bulk of effects. Instead, the tendency to perseverate about pain and to feel helpless showed significant effects. It may be that, for instance, perceptions that pain is uncontrollable or even unpredictable make pain an even more awful and overwhelming experience than simply magnifying its impact. These exaggerated appraisals of uncontrollability in concert with attempts to suppress could further exacerbate negative responses. Teasing apart the relative contributions of catastrophizing components, and the conditions under which one component may exert greater deleterious effects over other components awaits future research.
It should be emphasized that we took a trait approach to assessing the effects of catastrophizing and suppression on acute pain. Our explicit goal was to investigate how predispositions to think about, and regulate emotional responses to noxious stimuli may coalesce to form distinct trait profiles. To our knowledge, this is indeed the first study to examine trait thought suppression in the context of acute pain-induction. Still, it must also be considered that the effects of state catastrophizing (Edwards et al. 2008) and state suppression (Quartana and Burns 2007) on acute pain, have been examined, albeit separately, with results indicating that these states also significantly affect pain sensitivity.
A conceptual model that combines appraisal and emotion regulation styles may have important clinical implications. Chronic pain patients who catastrophize about pain and are distinguished by excessive suppression of negative thoughts and emotions may appear in the short term to successfully control or reduce negative emotions surrounding pain. However, in the long term, suppression leads to ironic increases in awareness of pain, does little to rectify the circumstances precipitating the pain and distress, and may lead to a vicious cycle where more suppression efforts are needed to regulate both old and new distress. Our results hint that the application of interventions that focus only on the maladaptive beliefs and appraisals of high catastrophizer pain patients may fail to effectively address a crucial element that may magnify the negative effects of catastrophizing; namely, maladaptive emotion regulation tactics such as suppression. Acquisition of new emotion regulation skills could help chronic pain patients who tend to appraise pain in a catastrophic fashion learn to accept or at least tolerate the distress associated with chronic pain in a more adaptive fashion (McCracken et al. 2005; Thorn and Boothby 2002).
It is important to note some limitations of this study. First, the sample was comprised of healthy people who underwent a laboratory pain-induction procedure. Thus, it is unclear how the findings of this study would generalize to a population of chronic pain patients who suffer from clinical pain. The appraisal and emotion regulation model will need to be evaluated among clinical samples in future research. Second, our method used self-report trait measures of pain catastrophizing and thought suppression as, essentially, proxy measures of what people actually do when confronted with pain. Because participants were not randomly assigned to conditions in which they were instructed to suppress or not, or to catastrophize or not, we are left to infer that catastrophizers catastrophized and suppressors suppressed. That is, we assume that the trait measures used in this study accurately reflected what participants’ actually did during pain-induction and recovery. As we have argued (Burns et al. 2008a, 2008b), the study of the effects of actual efforts to suppress during arousing situations (in controlled laboratory settings) must augment the use of trait suppression and inhibition measures in pain research.
In summary, our results support the notion that pain catastrophizing is rooted in cognitive distortions of pain (Sullivan et al. 2001), but expand this conceptualization by showing that the ways in which catastrophizers attempt to regulate emotional responses to pain may also be important in understanding how catastrophic appraisals affect eventual recovery from pain. Results suggest that for catastrophizers elevated on rumination and helplessness, the use of suppression may represent an especially maladaptive approach to regulating the negative emotional experiences provoked by painful stimuli. Conversely, high catastrophizers who do not regulate via suppression may be protected to some extent from the worst effects of prolonged recovery from pain. Taken together, results point to the possibility that appropriate assessment and treatment of those individuals revealing the most toxic profiles of pain appraisal and regulation traits would have the advantage of helping pinpoint intervention targets or tailoring treatment efforts for a wide variety of patients afflicted with painful medical conditions.
Acknowledgments
This research was supported in part by Grant MH071260 from the National Institute of Mental Health.
Contributor Information
Wesley Gilliam, Rosalind Franklin University of Medicine and Science, North Chicago, IL, USA.
John W. Burns, Department of Behavioral Sciences, Rush University Medical Center, 1653 W. Congress Parkway, 310 Rawson, Chicago, IL 60612, USA
Phillip Quartana, Johns Hopkins University School of Medicine, Baltimore, MD, USA.
Justin Matsuura, Rosalind Franklin University of Medicine and Science, North Chicago, IL, USA.
Carla Nappi, San Diego Veteran Affairs Hospital, San Diego, CA, USA.
Brandy Wolff, Rosalind Franklin University of Medicine and Science, North Chicago, IL, USA.
References
- Bartley EJ, Rhudy JL. The influence of pain catastrophizing on experimentally induced emotion and emotional modulation of nociception. The Journal of Pain. 2008;9:388–396. doi: 10.1016/j.jpain.2007.11.015. [DOI] [PubMed] [Google Scholar]
- Burns JW. Arousal of negative emotions and symptom-specific reactivity in chronic low back pain patients. Emotion. 2006;6:309–319. doi: 10.1037/1528-3542.6.2.309. [DOI] [PubMed] [Google Scholar]
- Burns JW, Quartana P, Bruehl S. Anger inhibition and pain: Conceptualizations, evidence and new directions. Journal of Behavioral Medicine. 2008a;31:259–279. doi: 10.1007/s10865-008-9154-7. [DOI] [PubMed] [Google Scholar]
- Burns JW, Quartana PJ, Gilliam W, Gray E, Matsuura J, Nappi C, et al. Effects of anger suppression on pain severity and pain behaviors among chronic pain patients: Evaluation of an ironic process model. Health Psychology. 2008b;27:645–652. doi: 10.1037/a0013044. [DOI] [PubMed] [Google Scholar]
- Cioffi D, Holloway J. Delayed costs of suppressed pain. Journal of Personality and Social Psychology. 1993;64:274–282. doi: 10.1037//0022-3514.64.2.274. [DOI] [PubMed] [Google Scholar]
- Cohen J, Cohen P, West SG, Aiken LS. Applied Multiple Regression/Correlation Analysis for the Behavioral Sciences. 3rd ed Lawrence Erlbaum Associates, Inc.; New Jersey: 2003. p. 201. [Google Scholar]
- Crombez G, Eccleston C, Van den Broeck A, Goubert L, Van Houdenhove B. Hypervigilance to pain in Fibromyalgia: The mediating role of pain intensity and catastrophic thinking about pain. Clinical Journal of Pain. 2004;20:98–102. doi: 10.1097/00002508-200403000-00006. [DOI] [PubMed] [Google Scholar]
- Edwards RR, Kronfli T, Haythornthwaite JA, Smith MT, McGuire L, Page GG. Association of catastrophizing with interleukin-6 responses to acute pain. Pain. 2008;140:135–144. doi: 10.1016/j.pain.2008.07.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- France CR, France JL, al’Absi M, Ring C, McIntyre D. Catastrophizing is related to pain, but not nociceptive flexion reflex threshold. Pain. 2002;99:459–463. doi: 10.1016/s0304-3959(02)00235-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goubert L, Crombez G, Van Damme S. The role of neuroticism, pain catastrophizing, and pain-related fear in vigilance to pain: A structural equations approach. Pain. 2004;107:234–241. doi: 10.1016/j.pain.2003.11.005. [DOI] [PubMed] [Google Scholar]
- Gross JJ. Antecedent- and response-focused emotion regulation: Divergent consequences for experience, expression, and physiology. Journal of Personality and Social Psychology. 1998;74:224–237. doi: 10.1037//0022-3514.74.1.224. [DOI] [PubMed] [Google Scholar]
- Gross JJ, John OP. Individual differences in two emotion regulation processes: Implications for affect, relationships, and well-being. Journal of Personality and Social Psychology. 2003;85:348–362. doi: 10.1037/0022-3514.85.2.348. [DOI] [PubMed] [Google Scholar]
- Gross JJ, Levenson RW. Emotional suppression: Physiology, self-report, and expressive behavior. Journal of Personality and Social Psychology. 1993;64:970–986. doi: 10.1037//0022-3514.64.6.970. [DOI] [PubMed] [Google Scholar]
- Gross JJ, Levenson RW. Hiding feelings: The acute effects of inhibiting negative and positive emotion. Journal of Abnormal Psychology. 1997;106:95–103. doi: 10.1037//0021-843x.106.1.95. [DOI] [PubMed] [Google Scholar]
- Maurset A, Skoglung LA, Hustveit O, Klepstad P, Oye I. A new version of the ischemic tourniquet pain test. Methods and Findings in Experimental Clinical Pharmacology. 1992;13:643–647. [PubMed] [Google Scholar]
- McCracken LM, Vowles KE, Eccleston C. Acceptance-based treatment for persons with complex, long-standing pain: A preliminary analysis of treatment outcome in comparison to a waiting phase. Behaviour Research and Therapy. 2005;28:271–284. doi: 10.1016/j.brat.2004.10.003. [DOI] [PubMed] [Google Scholar]
- Michael ES, Burns JW. Catastrophizing and pain sensitivity among chronic pain patients: Moderating effects of sensory and affect focus. Annals of Behavioral Medicine. 2004;27:185–194. doi: 10.1207/s15324796abm2703_6. [DOI] [PubMed] [Google Scholar]
- Muris P, Meesters C, van den Hout A, Wessels S, Franken I, Rassin E. Personality and temperament correlates of pain catastrophizing in young adolescents. Child Psychiatry and Human Development. 2007;38:171–181. doi: 10.1007/s10578-007-0054-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Osman A, Francisco FX, Gutierrez BAK, Merrifield T, Grittmann L. The pain catastrophizing scale: Further psychometric evaluation with adult samples. Journal of Behavioral Medicine. 2000;23:351–365. doi: 10.1023/a:1005548801037. [DOI] [PubMed] [Google Scholar]
- Quartana P, Burns JW. The painful consequences of anger suppression. Emotion. 2007;7:400–414. doi: 10.1037/1528-3542.7.2.400. [DOI] [PubMed] [Google Scholar]
- Severeijns R, van den Hout MA, Vlaeyen JWS. The causal status of pain catastrophizing: An experimental test with healthy participants. European Journal of Pain. 2005;9:257–265. doi: 10.1016/j.ejpain.2004.07.005. [DOI] [PubMed] [Google Scholar]
- Severeijns R, van den Hout MA, Vlaeyen JW, Picavet HS. Pain catastrophizing and general health status in a large dutch community sample. Pain. 2002;99:367–376. doi: 10.1016/s0304-3959(02)00219-1. [DOI] [PubMed] [Google Scholar]
- Severeijns R, Vlaeyen JWS, van den Hout MA, Picavet SJH. Pain catastrophizing is associated with health indices in musculoskeletal pain: A cross-sectional study in the dutch community. Health Psychology. 2004;23:49–57. doi: 10.1037/0278-6133.23.1.49. [DOI] [PubMed] [Google Scholar]
- Severeijns RM, Vlaeyen JWS, van den Hout MA, Weber WEJ. Pain catastrophizing predicts pain intensity, disability and psychological distress independent of level of physical impairment. The Clinical Journal of Pain. 2001;17:165–172. doi: 10.1097/00002508-200106000-00009. [DOI] [PubMed] [Google Scholar]
- Smeets RJEM, Vlaeyen JWS, Kester ADM, Knottnerus JA. Reduction of pain catastrophizing mediates the outcome of both physical and cognitive-behavioral treatment in chronic low back pain. The Journal of Pain. 2006;74:261–271. doi: 10.1016/j.jpain.2005.10.011. [DOI] [PubMed] [Google Scholar]
- Sullivan MJL, Bishop SR, Pivik J. The pain catastrophizing scale: Development and validation. Psychological Assessment. 1995;7:524–532. [Google Scholar]
- Sullivan MJL, Thorn B, Haythornthwaite JA, Keefe F, Martin M, Bradley LA, et al. Theoretical perspectives on the relation between catastrophizing and pain. The Clinical Journal of Pain. 2001;58:52–64. doi: 10.1097/00002508-200103000-00008. [DOI] [PubMed] [Google Scholar]
- Sulllivan MJL, Rouse D, Bishop S, Johnston S. Thought suppression, catastrophizing and pain. Cognitive Therapy and Research. 1997;21:555–568. [Google Scholar]
- Tan G, Jensen MP, Robinson-Whelen S, Thornby JI, Monga TN. Coping with chronic pain: A comparison of two measures. Pain. 2001;90:127–133. doi: 10.1016/s0304-3959(00)00395-x. [DOI] [PubMed] [Google Scholar]
- Thorn BE, Boothby JL. Targeted treatment of catastrophizing for the management of chronic pain. Cognitive and Behavioral Practice. 2002;9:127–138. [Google Scholar]
- Turner JA, Dworkin SF, Mancl L, Huggins KH, Truelove EL. The roles of beliefs, catastrophizing, and coping in the functioning of patients with temporomandibular disorders. Pain. 2001;92:41–51. doi: 10.1016/s0304-3959(00)00469-3. [DOI] [PubMed] [Google Scholar]
- Turner JA, Mancl L, Aaron LA. Pain-related catastrophizing: A daily process study. Pain. 2004;110:103–111. doi: 10.1016/j.pain.2004.03.014. [DOI] [PubMed] [Google Scholar]
- Van Damme S, Crombez G, Bijttebier P, Goubert L, van Houdenhove B. A confirmatory factor analysis of the pain catastrophizing scale: Invariant factor structure across clinical and non-clinical populations. Pain. 2002;96:319–324. doi: 10.1016/S0304-3959(01)00463-8. [DOI] [PubMed] [Google Scholar]
- Wegner DM, Schneider DJ, Carter SR, White TL. Paradoxical effects of thought suppression. Journal of Personality and Social Psychology. 1987;53:5–13. doi: 10.1037//0022-3514.53.1.5. [DOI] [PubMed] [Google Scholar]
- Wegner DM, Zanakos S. Chronic thought suppression. Journal of Personality. 1994;62:615–640. doi: 10.1111/j.1467-6494.1994.tb00311.x. [DOI] [PubMed] [Google Scholar]
- Whitehead WE, Crowell MD, Heller BR, et al. Modeling and reinforcement of the sick role during childhood predicts adult illness behavior. Psychosomatic Medicine. 1994;56:541–550. doi: 10.1097/00006842-199411000-00010. [DOI] [PubMed] [Google Scholar]


